Abstract
OBJECTIVE
Looking to the experience in the United States with managed care and the possible introduction of gatekeeping in the near future in Germany, we performed a population-based survey to examine preferences for future gatekeeping arrangements.
DESIGN
Cross-sectional telephone survey.
SETTING
Four health districts in Thuringia (formerly East Germany) and Lower Saxony (formerly West Germany).
PARTICIPANTS
Out of a random sample of 644 adults in the 4 districts, 415 persons (64.4%) took part in the survey.
MEASUREMENTS AND MAIN RESULTS
Using multiple logistic regression, we analyzed associations between preferences for gatekeeping arrangements and patient satisfaction, insurance status, and sociodemographic characteristics. Seventy-four percent of respondents valued first-contact care, especially older people (odds ratio [OR], 4.3; 95% confidence interval [95% CI], 2.0 to 9.3), people who were very satisfied with the relationship with their family physician (OR, 2.7; 95% CI, 1.6 to 4.8) and members of sickness funds in contrast to privately insured persons (OR, 2.4; 95% CI, 1.2 to 5.2). The family physician's influence in coordinating the use of specialist services was appreciated by 86%, more often by members of sickness funds (OR, 5.9; 95% CI, 2.4 to 14.3), people who were very satisfied with their doctor's professional competence (OR, 3.2; 95% CI, 1.6 to 6.3) and older persons (OR, 2.9; 95% CI, 1.1 to 7.7).
CONCLUSIONS
A vast majority of the German population would accept their family physician as entry point and as coordinator of all other health services. Since patient satisfaction, among other reasons, strongly influenced preferences for gatekeeper arrangements, family physicians themselves may be able to promote primary care health services.
Keywords: Family practice, managed care, doctor-patient relations, health care reform, consumer satisfaction
Since the declaration of Alma Ata in 1978,1 it is widely accepted that health services should be led by primary care physicians.2,3 Many managed care plans rely on primary care providers as “gatekeepers” to control the use of specialty, hospital, and other expensive services.3–5 Gatekeeping is intended to reduce costs while maintaining or improving quality of care by encouraging first-contact care, increasing coordination and continuity of services, and reducing duplicative or inappropriate care.2,4,6–8 Enrollees typically receive financial incentives to use primary care providers or specific service sites.
Although the German health care system faces the same problems as many other industrialized countries (e.g., ever-increasing costs of health care and a worsening of the mix of generalists to specialists), few efforts have been made to reorganize ambulatory care. To better understand this situation, we describe the most important aspects of the German health care system based on the work of Jackson.9 First, most Germans (88%) receive health care through membership in a sickness fund that finances their medical care. The remainder are wealthy enough to purchase private insurance, with premiums based on actuarial risk according to age. Second, patients are free to visit any physician (often a specialist). The ratio of ambulatory generalists to specialists is 41:59. Third, premiums collected by sickness funds are turned over to 19 regional physician associations, which in turn reimburse physicians. All ambulatory physicians are reimbursed on a fee-for-service basis. This system may have stimulated the highest health utilization rates in the world: the average German sees a physician 11 times annually, compared with 5.5 annual visits in the United States. Fourth, the German system is characterized by an almost complete uncoupling of ambulatory and hospital services. Fifth, after reunification in 1990, the health system of the former German Democratic Republic was brought in line with that in the former West Germany. This meant a change from state-controlled public group practices to private individual practices.
Until a new government was elected in September 1998, discussions about strengthening first-line medical care were rather unpopular in Germany.10 Specialists feared a loss of income and argued that limited access to specialist services could result in worse health outcomes,11,12 and sickness fund managers feared that patients would leave their fund if certain elements of managed care were introduced.
However, there is considerable uncertainty about what patients think of new models in ambulatory health care.13 Only one Israeli study assessed patients' opinions about gatekeeping and direct access to specialists.14 We designed a survey to assess patients' opinions and preferences for health care settings in the future. Looking to the experience in the United States with managed care, we focused on the 4 aspects most central to managed care settings and gatekeeping arrangements: (1) encouragement of first-contact care by generalists rather than specialists,2,4(2) acceptance of continuing provision of health services from the same primary care physician for a longer period of time,3(3) access to specialist or hospital services coordinated (i.e., not strictly controlled) by the primary care physician as case manager,7,11 and (4) the role of financial incentives to persuade patients to accept this primary care physician as their gatekeeper.7
We were interested in whether previous experience with family physicians influences the appreciation of gatekeeping models. Moreover, we assumed that patients' opinions and preferences might be influenced by age, insurance status, frequency of consultations, and the degree of medical supply. Especially in Germany, historical experience (i.e., the integration of East Germany into the western health system) may also influence public opinion.
METHODS
In contrast to the United Kingdom or the Netherlands, the population in Germany is not registered in family practice lists. Since it is therefore not possible to draw representative samples of patients from practice lists, we decided to perform a telephone survey.
Study Population and Sampling
The selection of subjects comprised 4 stages.
We selected 4 health districts in Lower Saxony (formerly West Germany) and 2 in Thuringia (formerly East Germany). According to statistics of the regional Associations of Sick Fund Physicians, the physician to population ratio in one district in Lower Saxony and one in Thuringia could be regarded as average or above average, and in the other two districts below average (personal communication).
Using the most recent and comprehensive telephone CD-ROM (D3-Info) for Germany, all telephone numbers in each of the 4 districts were copied and numbered in ascending order. Out of these numbers (between 30,000 and 50,000), we chose approximately 260 numbers at random in each district (using the normal procedure of SAS15).
All selected numbers were phoned and one adult was then randomly selected using the “next-birthday method.”16 If the subject selected was not available at the time of the initial contact or was in a hurry, the interviewer made an appointment to complete the interview at a more convenient time. Two trained female interviewers made the telephone calls from a centralized facility between 4 pmand 8 pm, Monday to Friday, between September and December 1997. To minimize nonresponse, a minimum of 5 calls were made before closing a number as a “no answer.”
After completing more than 350 interviews, we analyzed the age and gender of the persons telephoned and compared the sample with the national census data of 1996.17 In the remaining 50 telephone calls, we tried to select only those persons that were underrepresented with regard to age and gender, if available. Telephone numbers that proved to be nonprivate were replaced by the next successive telephone number. The survey format as well as the introductory phrases were standardized. Answers to frequently asked questions were drilled in advance.
The Questionnaire
The questionnaire was pretested with 20 people who were selected by random digit dialing. At the end of the interview, these people were asked about their understanding of the interview and difficulties in answering. In particular, the wording of the questionnaire was improved, 3 questions were omitted, and the answer format was changed from a 10-point to a 5-point scale. During the study, 10 randomly selected calls were repeated 5 days after the first interview to check the questionnaire for reliability.
The questionnaire consisted of three parts with 52 mostly standardized questions. The first section dealt with the consultation behavior and with satisfaction with the family physician. According to Baker,18 three dimensions of patient satisfaction (i.e., general satisfaction, satisfaction with depth of relationship and with professional care) were covered with one question each (e.g., “I feel able to tell my doctor about very personal things.”). One question about the family physician's coordination function was added: “My doctor always refers me to a specialist, if necessary.” Answers ranged from “strongly agree” to “strongly disagree” in a 5-point Likert format. The second part portrayed different options for managed care and gatekeeping arrangements (e.g., “If you always consult your family physician first, you will pay less for your health insurance. Are you interested in this option?” or, “Your doctor decides, in concordance with you, whether you should consult a specialist or be admitted to hospital. Do you like this idea?”). Answers were “yes,”“no,” or “don't know.” The last component of the questionnaire elicited some sociodemographic characteristics of the persons interviewed.
Analysis
Absolute and relative frequencies with 95% confidence intervals (CIs) are reported for the important variables. Several multiple logistic regressions were performed to determine the influence of the following variables, which were dichotomized: gender, age (≥60 years vs <60 years), insurance status (private insurance vs sickness fund member), consultation frequency (>4 times a year vs ≤4 times a year), different aspects of patient satisfaction (very satisfied vs satisfied or less satisfied). Backward elimination was applied to select important variables ( level for elimination: P = .05). We calculated the odds ratios (OR) with the corresponding 95% CIs as measures of effect.19
RESULTS
A total of 1,064 telephone numbers were called, 420 of which could not be completed because of technical problems (e.g., fax), problems of accessibility (5 calls without a connection), or problems of eligibility (severely ill, not German-speaking). Out of the 644 remaining telephone numbers, 229 persons refused to take part in the survey or did not complete the interview, giving a response rate of 64.4%. There was only a slight difference between the eastern part of Germany (response rate: 63.5%) and the western part (response rate: 65.3%). Table 1) compares the age, gender, and the insurance status of the telephone sample with the population in Germany.
Table 1.
Characteristics of the Study Subjects Compared to the National Population
| Former East Germany | Former West Germany | |||
|---|---|---|---|---|
| Characteristics | Sample (n = 202) | Population* | Sample (n = 213) | Population* |
| Age, y | ||||
| 18–39 | 38.1 | 39.1 | 39.0 | 41.1 |
| 40–59 | 34.2 | 34.6 | 32.9 | 32.8 |
| ≥60 | 27.7 | 26.3 | 28.1 | 26.1 |
| Gender | ||||
| Male | 46.5 | 47.8 | 46.0 | 48.1 |
| Female | 53.5 | 52.2 | 54.0 | 51.9 |
| Health insurance | ||||
| Private | 4.0 | 5.0 | 18.3 | 14.8 |
| Sick fund | 96.0 | 95.0 | 81.7 | 85.2 |
Census data17
The 10 persons who were phoned for a second time generally gave the same or nearly the same answers as the first time. A difference could be detected between the first and second interview in 12% of the answers; in nearly all (96%) of these cases, the answers differed by only 1 point on the Likert scale.
Use and Assessment of Ambulatory Care
Three hundred ninety-five (95%) of 415 participants regularly consulted a family physician; 116 (28%) of them consulted him or her more than 4 times a year. About two thirds of respondents having a family physician (n = 395) were highly satisfied (highest score on the 5-point Likert scale) with the different aspects of care from their doctor: general satisfaction (66%; 95% CI; 62 to 71), professional care (71%; 95% CI; 66 to 75), depth of relationship (65%; 95% CI; 61 to 70), and coordination of care (67%; 95% CI; 63 to 72).
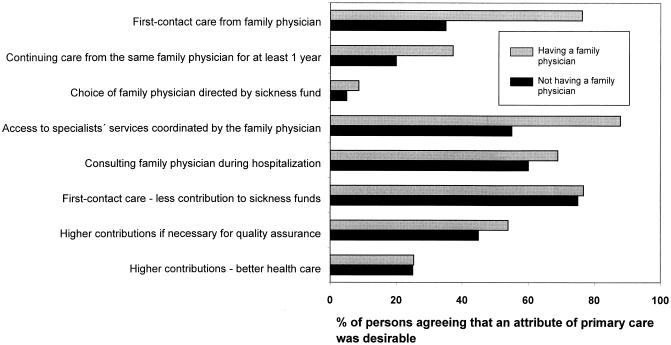
Assessment of Primary Care Modules for the Future
The attributes of primary care people most highly valued are shown in Figure 1. The majority agreed with a strengthening of the family physician's gatekeeping function. First-consult care by the family physician was appreciated by 74% of the participants. If required to consult a specialist, nearly all respondents want to be advised by their doctor and to stay in contact with their family physician during hospitalization. A lower percentage of respondents indicated it was important to consult the same family physician for at least 1 year. Nearly all respondents wanted to choose their doctor by themselves and did not accept a steering function by their sickness fund.
FIGURE 1.
Assessment of primary care modules.
Economic components of different health care concepts for the future were subtly differentiated. Three quarters of the people interviewed would welcome their family physician's gatekeeping function if their premiums to the sickness fund are decreased. But they would tolerate higher premiums if this is the only way to assure the quality of ambulatory care for all members of the society. Most participants did not accept rigid market-models of health care, i.e., a better or worse quality in health care according to the contributions to their sickness fund.
Persons who did not have a family physician as their family doctor (n = 20) were more skeptical about first-contact care and the guiding function of their doctor. Only 35% and 55%, respectively, appreciated these roles for their doctor.
Determinants of the Assessment
In a series of multiple logistic regressions, factors associated with people's preferences were determined. Willingness to first consult a family physician was strongly influenced by age, with older persons more often accepting this option (OR; 4.3; 95% CI; 2.0 to 9.3). Further significant factors were a good relationship with the doctor and his or her competence (assessed by the patient), gender, and membership in a sickness fund (Table 2). Acceptance of being restricted to the same doctor over a period of at least 1 year was significantly associated with a positive assessment of their family physician's professional competence and the depth of the relationship. Type of insurance and the doctor's competence also stimulated acceptance of the gatekeeper model if the sickness funds would lower their premiums.
Table 2.
Factors Associated with Assessment of First-Contact Care*
| Number in Agreement (%) | Adjusted Odds Ratio | 95% Confidence Interval | |
|---|---|---|---|
| Acceptance of first-contact care† | |||
| Age‡ | |||
| <60 | 195 (70) | 1.0 | |
| ≥60 | 106 (91) | 4.3 | 2.0 to 9.3 |
| Relationship with family physician‡ | |||
| Moderate | 83 (61) | 1.0 | |
| Very good | 218 (85) | 2.7 | 1.6 to 4.8 |
| Insurance status‡ | |||
| Private | 24 (59) | 1.0 | |
| Sickness fund | 274 (79) | 2.4 | 1.2 to 5.2 |
| Gender‡ | |||
| Female | 158 (74) | 1.0 | |
| Male | 143 (79) | 2.2 | 1.3 to 3.8 |
| Competence of the family physician‡ | |||
| Moderate | 71 (61) | 1.0 | |
| Very good | 230 (82) | 2.0 | 1.1 to 3.5 |
| Acceptance of first-contact care, if combinedwith financial incentives† | |||
| Insurance status‡ | |||
| Private | 22 (54) | 1.0 | |
| Sickness fund | 277 (80) | 3.1 | 1.6 to 6.1 |
| Family physican's professional competence‡ | |||
| Moderate | 78 (67) | 1.0 | |
| Very good | 225 (81) | 1.9 | 1.2 to 3.2 |
| Acceptance of continuing care from thesame doctor for at least 1 y† | |||
| Relationship with family physician‡ | |||
| Moderate | 31 (23) | 1.0 | |
| Very good | 116 (45) | 2.1 | 1.2 to 3.4 |
| Family physician's professional competence‡ | |||
| Moderate | 26 (22) | 1.0 | |
| Very good | 121 (43) | 2.0 | 1.2 to 3.4 |
| Age‡ | |||
| <60 | 90 (32) | 1.0 | |
| ≥ 60 years | 57 (49) | 1.6 | 1.0 to 2.5 |
The following variables were included: age, sex, children, frequency of consultation, insurance status, satisfaction with the family physician (general satisfaction, competence, relationship, coordination of care), number of inhabitants, physician to population ratio, political region.
Response variables.
Significant covariables.
A positive attitude toward the family physician's advice on consulting a specialist was strongly associated with insurance status. Members of sickness funds frequently valued this option, whereas privately insured subjects were reluctant to restrict their access to specialists. The doctor's competence, as assessed by the persons interviewed, was also important, as well as the physician to population ratio, with a high ratio positively associated with the acceptance of the family physician's advisory function (Table 3). Only one factor (depth of relationship with the doctor) significantly influenced consumer's vote for a potential consultant function of the family physician in hospital care.
Table 3.
Factors Associated with Assessment of the Family Physician's Coordination of Care*
| Number in Agreement n(%) | Adjusted Odds Ratio | 95% Confidence Interval | |
|---|---|---|---|
| Acceptance of controlled accessto specialist services througha gatekeeper† | |||
| Insurance status‡ | |||
| Private | 27 (66) | 1.0 | |
| Sickness fund | 316 (91) | 5.9 | 2.4 to 14.3 |
| Family physician's professionalcompetence‡ | |||
| Moderate | 91 (79) | 1.0 | |
| Very good | 256 (92) | 3.2 | 1.6 to 6.3 |
| Age‡ | |||
| Younger persons (≤60 years) | 237 (85) | 1.0 | |
| Older persons (>60 years) | 110 (95) | 2.9 | 1.0 to 7.7 |
| Region‡ | |||
| Former Eastern Germany | 167 (87) | 1.0 | |
| Former Western Germany | 180 (89) | 2.4 | 1.1 to 5.3 |
| Physician to population ratio‡ | |||
| Low or average | 164 (83) | 1.0 | |
| High | 183 (92) | 2.2 | 1.0 to 4.5 |
| Acceptance with family physician'sconsulting during hospitalization† | |||
| Relationship with family physician‡ | |||
| Moderate | 78 (57) | 1.0 | |
| Very good | 195 (75) | 2.2 | 1.4 to 3.5 |
The following variables were included: age, sex, children, frequency of consultation, insurance status, satisfaction with the family physician (general satisfaction, competence, relationship, coordination of care), number of inhabitants, physician to population ratio, political region.
Response variables.
Significant covariables.
DISCUSSION
Many countries, faced with continually increasing health care costs, are experimenting with reorganization.8,20 Before implementing primary care-led health services, it may be useful to study the public's preferences and views of new models in ambulatory care. This study focused on gatekeeper arrangements. According to a cross-national public opinion survey some years ago,21 Germans, as compared to Americans and Canadians, expressed the strongest opposition to being required to see a family doctor before a specialist as an approach to cost-containment. In the meantime, the German population seems to have become more open-minded toward gatekeeping. Three quarters of the respondents in our telephone survey agreed with a strengthening of the family physician's role in health care delivery and with his or her consulting function in case of hospitalization or of referral to specialist services.
In our survey, nearly all consumers were skeptical about gatekeeping arrangements if they did not feel free to consult a primary care physician of their choice. This finding is similar to 2 recent German surveys in which more than 90% voted against any limitation in choosing one's family doctor.22,23 Although patients in Germany usually do not change their doctor,13 many of them want to be sure that they can choose to go to “the best” doctor available. This is an ideal of Western cultures.11,24
Financial advantages in primary care-led health services played a role for many consumers in the survey, similar to patients in health maintenance organizations in the United States.25 However, many persons in our survey would accept having to pay higher contributions if this would guarantee better health care for the entire nation. This is a plea for a health system based on solidarity.26
Multivariate analyses indicated several independent explanatory variables related to preferences for gatekeeping arrangements. They included age, membership in a sickness fund, satisfaction with one's own doctor, gender, and location.
Age. Older patients may consider their family physician as their representative and advocate in health care. They accept or even prefer that he or she assists them through the maze of health services. Younger people usually have less severe illnesses and, therefore, feel confident in their ability to choose the right specialist.14
Membership in a sickness fund. This may also be true for members of private insurance, most of whom are better educated. They preferred direct access to specialists, as did privately insured and better educated patients in a Dutch study.27
Satisfaction with one's own doctor. Patient satisfaction significantly influenced patient preference for gatekeeping arrangements, as well as for a consulting function of the family physician in hospitals and for referral by him or her. This conclusion is not as trivial as it may seem. Since it is not (or not alone) the media that influence the public perception of health care reforms,28 primary care physicians themselves might be able to promote primary care-led health services.
Gender. We detected a difference in acceptance of first-contact care. Men were more attracted by this option than women. In Germany, women usually consult community specialists in obstetrics and gynecology and might even consider the gynecologist as their family doctor.29 They might be concerned that first-contact care by a family physician might restrict access to their community gynecologist. Similar to recent developments in the United States,30 gatekeeping arrangements in Germany will include community gynecologists as primary care providers.
Location. Since ambulatory physicians in the eastern part assessed cooperation with their hospital colleagues more favorably than doctors in the former West Germany,31 even some years after reunification, it is difficult to explain why fewer consumers in the former East Germany would accept their family physician as future consultant and coordinator of specialist services. Perhaps persons in the eastern part of the country were often more afraid that cooperation between primary and secondary care might hurt confidentiality or reinforce professional dominance that would make up their mind for them as in the past. Further studies are needed to confirm such assumptions.
In the era of managed care, there is some concern that doctors must act as double agents, no longer exclusively fulfilling the Hippocratic oath but serving the interests of both patients and health care corporations.32,33 The gatekeeping role, aimed at restricting access to specialists, has raised much controversy.11,34,35 This may result from a misunderstanding and a misconception of the generalist's role in specialist-dominated health care systems such as Germany's. As Jones35 emphasizes, the generalist has or should have little to do with rationing or checking whether or not the patient qualifies (according to insurance coverage) for an expensive encounter with secondary or tertiary care. On the contrary, the primary care physician may better understand the patient's problem and the options available for dealing with it.
The results of our study suggest that patients opt for gatekeeping if primary care physicians act both as entry point and as integrator of all health services,4 instead of controlling and restricting access to specialists. Another important condition for a successful introduction and public acceptance of gatekeeping arrangements will be that people trust their family physicians and consider them as highly competent professionals,14 and that they may choose—and change—their primary care doctor. Sick fund managers should inform especially younger people and privately insured people about the advantages of first consulting with the family physician and of a long-term relationship.
Some limitations of the study should be considered. Although the age and gender of our sample is similar to the population in Germany and the response rate is satisfactory, we have no further information on the consumers who refused to take part in the survey. Even more important is the fact that many answers were not experience-based. They are anticipations of scenarios which may be entirely unknown to the respondents. Strictly speaking, the survey reflects assumptions, perceptions, and possibly prejudices rather than experience. Sometimes, however, perceptions can be more important than actual experiences since they influence the climate for political decisions.
Acknowledgments
We would like to thank Sabine Häder, PhD, Peter Prüfer, MS (psychologist), and Michael Schneid, MS (sociologist) from the Zentrum für Umfragen, Methoden und Analysen (ZUMA), Mannheim, Germany for their advice in all methodical aspects of telephone interviews. Hans Münchberg, director of a major sick fund (AOK) in the region of Göttingen, cooperated in reviewing the questionnaire. We are very much indebted to Dr. Barbara Starfield for her valuable comments on the manuscript.
REFERENCES
- 1. World Health Organization. Primary Health Care: Alma-Alta 1978. Geneva, Switzerland: WHO, 1978. Health for All; No. 1.
- 2.Coulter A. Why should health care services be primary care-led? J Health Serv Res Policy. 1996;1:122–4. doi: 10.1177/135581969600100212. [DOI] [PubMed] [Google Scholar]
- 3.Starfield B. The future of primary care in a managed care era. Int J Health Serv. 1997;27:687–96. doi: 10.2190/FL2W-ELJX-L54V-TYKH. [DOI] [PubMed] [Google Scholar]
- 4.Starfield B, Cassady C, Nanda J, Forrest CB, Berk R. Consumer experiences and provider perceptions of the quality of primary care: implications for managed care. J Fam Pract. 1998;46:216–26. [PubMed] [Google Scholar]
- 5.Schucht C, Kochen MM. Managed care: a model for outpatient care in Germany? [in German]. Z Ärztl Fortbild Qualitätssich. 1998;92:685–9. [PubMed] [Google Scholar]
- 6.Halm EA, Causino N, Blumenthal D. Is gatekeeping better than traditional care? A survey of physician's attitudes. JAMA. 1997;278:1677–81. [PubMed] [Google Scholar]
- 7.American Medical Association. (AMA). Principles of managed care. Available at www.ama-assn.org/advocacy/principl.htm. Accessed: January.
- 8.Etter JF, Perneger TV. Health care expenditures after introduction of a gatekeeper and a global budget in a Swiss health insurance plan. J Epidemiol Community Health. 1998;52:370–6. doi: 10.1136/jech.52.6.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson JL. The German health system. Lessons for reform in the United States. Arch Intern Med. 1997;157:155–60. [PubMed] [Google Scholar]
- 10.Glöser S. Toward managed care models [in German]. Dtsch Ärztebl. 1999;96:441. [Google Scholar]
- 11.Bodenheimer T, Lo B, Casalino L. Primary care physicians should be coordinators, not gatekeepers. JAMA. 1999;281:2045–9. doi: 10.1001/jama.281.21.2045. [DOI] [PubMed] [Google Scholar]
- 12.Volpp KG, Schwartz JS. Myths and realities surrounding health reform. JAMA. 1994;271:1370–2. doi: 10.1001/jama.271.17.1370. [DOI] [PubMed] [Google Scholar]
- 13.Wasern J, Güther B. The German health system: Attitudes and expectations of the population—a stock-taking [in German] Neuss: Janssen-Cilag; 1998. [Google Scholar]
- 14.Tabenkin H, Gross R, Brammli S, Shvartzman P. Patient's view of direct access to specialists: an Israeli experience. JAMA. 1998;279:1943–8. doi: 10.1001/jama.279.24.1943. [DOI] [PubMed] [Google Scholar]
- 15.SAS Institute Inc. SAS/STAT. User's Guide. Version 6. 4th ed. Cary, NC: SAS Institute Inc; 1989. [Google Scholar]
- 16.Salmon CT, Nichols JS. The next-birthday method of respondent selection. Publ Opinion Quart. 1983;47:277–92. [Google Scholar]
- 17.Federal Statistical Office. Statistical Yearbook 1997 for the Federal Republic of Germany [in German] Stuttgart: Metzler-Poerschel; 1998. [Google Scholar]
- 18.Baker R. Development of a questionnaire to assess patient's satisfaction with consultations in general practice. Br J Gen Pract. 1990;40:487–90. [PMC free article] [PubMed] [Google Scholar]
- 19.Stokes ME, Davis CS, Koch GG. Categorical data analysis using the SAS system. Cary, NC: SAS Institute Inc; 1995. :163ff. [Google Scholar]
- 20.Starfield B. Is primary care essential? Lancet. 1994;344:1129–33. doi: 10.1016/s0140-6736(94)90634-3. [DOI] [PubMed] [Google Scholar]
- 21.Blendon RJ, Benson J, Donelan K, et al. Who has the best health care system? A second look. Health Aff. 1995;14:221–30. doi: 10.1377/hlthaff.14.4.220. [DOI] [PubMed] [Google Scholar]
- 22.EMNID. A survey of doctors and patients [in German] Köln: Capital and Schwarz Pharma; 1997. [Google Scholar]
- 23.Costler D, Klaes L. Free access to doctors—a population based survey [in German] Bonn: Wissenschaftliches Institut der Ärzte Deutschlands (WIAD) e.V; 1999. [Google Scholar]
- 24.Schmittdiel J, Selby JV, Grumbach K, Quesenberry CP., Jr Choice of a personal physician and patient satisfaction in a health maintenance organization. JAMA. 1997;278:1596–9. [PubMed] [Google Scholar]
- 25.Tudor CG, Riley G, Ingber M. Satisfaction with care: do Medicare HMOs make a difference? Health Aff. 1998;17:165–76. doi: 10.1377/hlthaff.17.2.165. [DOI] [PubMed] [Google Scholar]
- 26.Ullrich CG. Solidarity and security. The acceptance of the statutory health insurance [in German]. Z Soziol. 1996;25:171–89. [Google Scholar]
- 27.Kulu-Glasgow I, Delnoij D, de Bakker D. Self-referral in a gatekeeping system: patient's reasons for skipping the general-practitioner. Health Policy. 1998;45:221–38. doi: 10.1016/s0168-8510(98)00045-1. [DOI] [PubMed] [Google Scholar]
- 28.Bernard DB, Shulkin DJ. The media vs managed health care: are we seeing a full court press? Arch Intern Med. 1998;158:2109–11. doi: 10.1001/archinte.158.19.2109. [DOI] [PubMed] [Google Scholar]
- 29.Himmel W, Ittner E, Kron M, Kochen MM. Comparing women's view on family and sexual problems in family and gynecological practices. J Psychosom Obstet Gynecol. 1999;20:127–35. doi: 10.3109/01674829909075586. [DOI] [PubMed] [Google Scholar]
- 30.Frazier JB. Current trends in American managed care: economic, technological, and political factors. Gesundheitsökon Qualitätsmanage. 1999;4:48–54. [Google Scholar]
- 31.Himmel W, Kron M, Hepe S, Kochen MM. Drug prescribing in hospital as experienced by general practitioners. East versus West Germany. Fam Pract. 1996;13:247–53. doi: 10.1093/fampra/13.3.247. [DOI] [PubMed] [Google Scholar]
- 32.Emanuel EJ, Dubler NN. Preserving the physician-patient relationship in the era of managed care. JAMA. 1995;273:323–9. [PubMed] [Google Scholar]
- 33.Shortell SM, Waters TM, Clarke KW, Budetti PP. Physicians as double agents: maintaining trust in an era of multiple accountabilities. JAMA. 1998;280:1102–8. doi: 10.1001/jama.280.12.1102. [DOI] [PubMed] [Google Scholar]
- 34.Kerr EA, Hays RD, Mitchison A, Lee M, Siu AL. The influence of gatekeeping and utilization review on patient satisfaction. J Gen Intern Med. 1999;14:287–95. doi: 10.1046/j.1525-1497.1999.00336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones R. Primary care and the US health care system. J Health Serv Res Policy. 1999;4:2–4. doi: 10.1177/135581969900400102. [DOI] [PubMed] [Google Scholar]