Abstract
OBJECTIVE
To describe functional deficits among older adults living alone and receiving home nursing following medical hospitalization, and the association of living alone with lack of functional improvement and nursing home utilization 1 month after hospitalization.
DESIGN
Secondary analysis of a prospective cohort study.
PARTICIPANTS
Consecutive sample of patients age 65 and over receiving home nursing following medical hospitalization. Patients were excluded for new diagnosis of myocardial infarction or stroke in the previous 2 months, diagnosis of dementia if living alone, or nonambulatory status. Of 613 patients invited to participate, 312 agreed.
MEASUREMENTS
One week after hospitalization, patients were assessed in the home for demographic information, medications, cognition, and self-report of prehospital and current mobility and function in activities of daily living (ADLs) and independent activities of daily living (IADLs). One month later, patients were asked about current function and nursing home utilization. The outcomes were lack of improvement in ADL function and nursing home utilization 1 month after hospitalization.
RESULTS
One hundred forty-one (45%) patients lived alone. After hospital discharge, 40% of those living alone and 62% of those living with others had at least 1 ADL dependency (P=.0001). Patients who were ADL–dependent and lived alone were 3.3 (95% confidence interval [95% CI], 1.4 to 7.6) times less likely to improve in ADLs and 3.5 (95% CI, 1.0 to 11.9) times more likely to be admitted to a nursing home in the month after hospitalization.
CONCLUSION
Patients who live alone and receive home nursing after hospitalization are less likely to improve in function and more likely to be admitted to a nursing home, compared with those who live with others. More intensive resources may be required to continue community living and maximize independence.
Keywords: hospitalization, risk factors, activities of daily living, socioeconomic factors, support, aged
Older adults may undergo substantial changes in function and living status when hospitalized for acute medical illness. Decline in function in activities of daily living (ADLs) occurs in one third of hospitalized older adults,1–3 and frequently heralds an end to community living. While a number of studies have focused on risk factors for functional decline and nursing home placement at the end of hospitalization,3–10 less is known about outcomes once patients are discharged home. Yet, for many patients, the posthospitalization period is one of dynamic flux. Changes in functional status (both improvement and worsening) commonly occur even after hospitalization, and the risk of nursing home placement may persist.3,10 To best allocate posthospital health care services, it is important to determine who is at risk for lack of improvement in function and for nursing home placement.
One of the primary tasks of the posthospital period is to improve function, with the goal of recovering function that was lost because of acute illness and iatrogenic complications of hospitalization. Improvement is not universal. In a previous study of patients who lost ADL function associated with hospitalization, 41% had not recovered to their prehospital baseline by 3 months after discharge.3
We hypothesized that older adults who lived alone in the community following hospitalization would be less likely to improve in function after discharge, compared with those who lived with others. Lacking encouragement from an in-home caregiver, patients living alone may be reluctant to assume independence in basic tasks, continuing instead to rely on support from outside the home. Such patients may also be more vulnerable to the effects of insufficient rehabilitation and new or continued medical illness. Thus, they may be at high risk for nursing home placement as well.
While little is known about the outcomes of frail older adults who live alone in the community after hospitalization, data suggest that adequate social support is essential for functional recovery and maintenance of community living.11–13 However, these studies did not specifically examine posthospital living arrangements. In a population of older adults receiving home nursing services following hospitalization for medical illness, we have described the deficits in function and mobility among patients who are discharged to home alone, in comparison with those who are discharged to home with others, and the temporal changes in ADL and instrumental ADL (IADL) function over 1 month, comparing those living alone and those living with others. Finally, we have analyzed, controlling for other factors, the association of living alone with 2 adverse outcomes 1 month after hospitalization. For the subset of patients dependent in ADL function at hospital discharge, we have evaluated the association of living alone with lack of improvement in ADL function and, for the full cohort, the association of living alone with nursing home admission. We also determined whether frequency of informal support would affect outcomes for those who lived alone. We hypothesized that increased frequency of informal supports would be associated with greater likelihood of functional improvement and decreased risk of nursing home admission.
METHODS
Study Population
This study was a secondary analysis of a prospective study that enrolled patients from April 1994 to May 1996 to examine risk of falls after discharge. Patients were consecutively enrolled in the study if they were age 65 or older, admitted to a Madison, Wis-area hospital with a medical diagnosis (nonsurgical and nonpsychiatric) and enrolled in 1 of 2 local home health agencies following discharge. Area hospitals included 1 rural hospital, 1 urban veterans hospital, 1 urban university hospital, and 2 urban community hospitals. Of 1,245 patients meeting inclusion criteria, 482 were excluded for enrollment in hospice (n = 26), a new diagnosis of cerebral vascular accident or myocardial infarction within the last 2 months (n = 189), diagnosis of dementia if no caregiver in the home (n = 35), time lapse of greater than 5 days from hospital discharge to home health enrollment (n = 106), nonambulatory status (n = 96), or miscellaneous (inability to speak English, anticipated move from the community in the next week, etc.; n = 30).
Of 763 patients meeting study criteria, 613 were contacted for enrollment (150 patients were missed because of inability to contact within 5 days of discharge). Patients who were contacted were similar in age, race, and gender to those who were not contacted, but were more likely to be married (37% vs 26%; P = .025). Of the 613 patients who were asked to participate, 312 (51%) accepted. Patients who refused were not different from those who accepted in age, race, gender, marital status, or hospital length of stay. Informed consent was obtained in accordance with University of Wisconsin Institutional Review Board guidelines.
Initial Assessment
Patients were seen in their homes within 5 days of hospital discharge. Baseline data included demographic information, length of hospital stay, medications, presence of depressed mood,14 self-reported history of weight loss in the previous 3 months, and cognitive status using the Mini-Mental State Examination (MMSE).15 Diagnoses were obtained from hospital admission histories and physicals and from home health records. Patients were asked about mobility status and ability to perform ADLs and IADLs at the present time (postdischarge) and for the period 2 weeks prior to hospitalization. Mobility questions included use of assistive device (defined as cane, walker, wheelchair, or other ambulation aid more than 50% of the time) for indoor and outdoor mobility. Function was assessed by the Katz scale for 6 ADLs (bathing, dressing, toileting, transferring, walking, and eating),16 and by the Lawton scale for 7 IADLs (telephoning, transportation, shopping, meal preparation, housework, medications, and ability to handle finances).17 Patients were considered independent in an ADL or IADL if they were able to perform the activity without help from another person.
Functional and mobility characteristics at hospital discharge and for the period 2 weeks prior to hospitalization were obtained by self-report from the patient (or proxy if the patient was deemed unreliable based on clinical judgment). Most (76%) of the data were provided by the patient. In a random subsample of 12 patient-proxy pairs, there was complete agreement on prehospital ADL and IADL scores in 83% of pairs. Patients were equally likely to underrate as overrate ADL function compared with the proxy.
Patients were categorized as living alone versus living with others. Living with others included living with a spouse or other person in the home, or residing in a community-based retirement facility. Patients who had another person stay with them on a temporary basis after hospitalization (n = 12) were classified as living with others.
To determine the degree of informal support, at the first posthospital home assessment, patients who lived alone were asked to identify the person outside the home (family, friend, or neighbor) who provided the most significant consistent interaction over the previous 2 months. We then contacted each identified person to ask how often he/she had seen the patient since discharge. Informal support frequency was classified as daily versus less than daily, based on proxy responses.
Follow-up Assessment
One month after hospital discharge, information was obtained in the home or nursing home regarding survival, ADL and IADL function, and nursing home utilization during the previous month. Information was obtained by the same interviewer as the initial evaluation. The same source of data reporting (patient or proxy) was used in 98% of cases. We reviewed hospital and nursing home records to verify reports of nursing home admissions.
One-Month Outcomes, Adjusting for Other Covariates
The 2 primary adverse outcomes at 1-month posthospitalization were lack of improvement in ADL function and nursing home utilization. We defined lack of improvement in ADL function as no improvement (i.e., no change or a decrease) in the number of independent ADLs between hospital discharge and 1-month follow-up. We evaluated this outcome only for the subset of patients who were dependent in 1 or more ADLs at discharge. We defined nursing home utilization as any stay in a nursing home over the month after discharge, including patients who were in the nursing home at the 1-month interview. We evaluated this outcome for the full cohort.
Sample for Analysis
Temporal Changes in ADL and IADL Function from Prehospital to 1-month Posthospitalization
The sample for the description of change in ADL and IADL status excluded 56 patients who did not have 1-month data regarding function (16 were hospitalized, 33 refused or could not be scheduled, and 7 had died), yielding 256 for analysis (82% of enrolled patients). Of the 16 who were hospitalized, 9 lived with others and 7 lived alone. Of the 7 who died, 5 lived with others and 2 alone. Comparing those with (n = 256) and without (n = 56) complete 1-month functional data, there were no differences in demographic characteristics, prehospital ADL or IADL status, or principal diagnosis. However, patients with complete data had slightly higher ADL function (5.0 vs 4.6 ADLs independent, P = .078) and IADL function (2.8 vs 2.4 IADLs independent, P = .074) at hospital discharge.
One-Month Outcomes, Adjusting for Other Covariates.
For the outcome of lack of improvement in ADL function at 1-month postdischarge, we considered only patients who were dependent in ADLs at hospital discharge. (Patients who were independent in ADLs were excluded as they could not improve further.) Of patients with complete 1-month functional data, 130 were dependent in ADL function at discharge and formed the sample for analysis. For the outcome of nursing home utilization, we considered the full cohort. Of the 312 patients in the full cohort, 17 had missing data regarding nursing home utilization and 7 had died, yielding 288 for analysis (92% of sample).
Data Analysis
We evaluated differences in binary and ordinal outcomes between those who lived alone and those who lived with others using χ2tests or Fisher's exact test if any cell size was expected to be less than 5. For continuous outcomes, we used parametric tests unless the parametric assumptions were violated sufficiently to require a nonparametric test. To examine the temporal changes of ADL and IADL function over time, we used repeated measures analysis of variance with unstructured covariance matrix to determine if there was a significant interaction between time and living status. If a significant interaction effect was found, then parametric tests were performed to test for significance of changes in functional status between living arrangement groups.
We used logistic regressions to test the independent association of living alone with the 1-month outcomes, lack of improvement in ADL function, and nursing home utilization. We utilized literature review to determine potential predictors for consideration in the models. Along with living arrangement, all models included, a priori, variables found to be strongly associated with the outcomes in past research (age, cognition, and discharge ADL status).4,7,9,10,18–23 We also evaluated other variables, less strongly associated with the outcomes in past research, in the regression models. These variables were prehospital ADL status, use of assistive device, subjective health rating, vision, depression, and weight loss, for the outcome of lack of ADL improvement,7,24–27 and length of hospital stay, decline in ADL function from prehospitalization to discharge, number of diagnoses at hospital discharge, number of hospitalizations in the previous year, and admission to a nursing home in the previous year, for the outcome of nursing home utilization.8,10,19,20,22 We also evaluated principal diagnosis (cardiovascular, pulmonary, gastrointestinal, neurologic, or other) in the regression models. From the above list of variables, a variable was retained in the final regression model if it reached a significance level of P < .05 or if it was a confounder. All variables in the final regression models were tested for interaction effects.
For both outcomes, we developed the first regression model (base model) without gender as a covariate. This was done because of the strong association between being a woman and living alone, and because there was not sufficient power for meaningful subgroup analysis of men and women separately. We then conducted analyses adding gender to each base model (base model with gender).
We performed secondary analyses to test for the association between frequency of informal support for patients who lived alone and 1-month outcomes. We again fit the base model and the base model with gender for each outcome, classifying the live alone group by the frequency of informal supports (i.e., visited daily vs less than daily by another person), using the live-with-others group as the reference. Data were analyzed using SAS version 6.12 (SAS Institute, Inc., Cary, NC).
RESULTS
Prehospital and Discharge Characteristics of the Sample
The characteristics of the sample of 312 subjects who received home nursing following hospitalization for medical illness are shown in Table 1. The study sample was predominantly white, and the majority were women. Patients stayed an average of 7 days in the hospital and took an average of 6 medications at discharge.
Table 1.
Characteristics of Patients Receiving Home Nursing Services Following Hospitalization for Acute Medical Illness and of Patients Living Alone Versus with Others
| Living Arrangements | ||||
|---|---|---|---|---|
| Characteristic | Total (N=312) | Alone (n=141) | With Others (n=171) | P Value* |
| Demographics | ||||
| Mean age, y (SD) | 80.0 (7.1) | 81.2 (7.3) | 79.0 (6.8) | .008 |
| Women, n(%) | 196 (63) | 111 (79) | 85 (50) | .001 |
| White, n(%) | 302 (97) | 138 (98) | 164 (96) | .327 |
| Married, n(%) | 121 (39) | 7 ( 5) | 114 (67) | .001 |
| Prehospital function | ||||
| Mean IADL (SD)† | 4.1 (2.3) | 4.8 (1.8) | 3.5 (2.5) | .0001 |
| Mean ADL (SD)‡ | 5.5 (1.2) | 5.8 (0.8) | 5.2 (1.4) | .0001 |
| Dependent in 1 or more IADLs, n(%) | 246 (79) | 106 (76) | 140 (82) | .151 |
| Dependent in 1 or more ADLs, n(%) | 78 (25) | 19 (14) | 59 (35) | .001 |
| Hospital/discharge-related | ||||
| Mean length of stay, days (SD) | 6.9 (4.7) | 6.1 (4.9) | 7.5 (4.5) | .008 |
| Mean total no. of diagnoses (SD) | 7.1 (2.7) | 7.0 (2.7) | 7.1 (2.8) | .765 |
| Principal diagnosis, n(%) | ||||
| Cardiovascular | 59 (18.9) | 35 (20.5) | 24 (17) | |
| Pulmonary | 75 (24.0) | 42 (24.6) | 33 (23.4) | |
| Gastrointestinal | 37 (11.9) | 21 (12.3) | 16 (11.4) | .783 |
| Neurologic | 31 (9.9) | 18 (10.5) | 13 (9.2) | |
| Other | 110 (35.3) | 55 (32.2) | 55 (39) | |
| Mean no. of medications (SD) | 6.1 (3.1) | 6.2 (2.9) | 6.0 (3.2) | .684 |
| Mean MMSE (SD)§ | 25.9 (4.2) | 26.6 (3.1) | 25.3 (4.8) | .057 |
| Depressed mood, n(%) | 83 (27.0) | 39 (28) | 44 (27) | .846 |
Test for significance comparing living alone versus with others; unless otherwise noted, parametric tests were used for all continuous variables.
Instrumental activities of daily living (IADL), maximum = 7 (telephoning, transportation, shopping, meal preparation, housework, medications, and ability to handle finances).
Activities of daily living (ADL), maximum = 6 (bathing, dressing, toileting, transferring, walking, eating).
Mini-Mental State Examination (MMSE), maximum score = 30; nonparametric test.
At hospital discharge, 171 (55%) patients lived with someone (35% with spouse, 15% with family, 5% with hired help) and 141 (45%) lived alone. Characteristics of patients who lived alone versus those who lived with others are shown in Table 1. Of those who lived alone, 79% were women, and 78% were widowed. The group living alone was older, had higher prehospital ADL and IADL function, and had a shorter hospital stay.
Table 2 shows discharge functional and mobility status of patients living alone. Forty percent of those who lived alone were dependent in ADL function at discharge. Forty percent were dependent on another person for bathing; 12% were dependent for dressing. Over half of those living alone needed help in meal preparation, and almost two thirds were unable to walk outdoors. Half of those living alone received services from a home health aide after discharge.
Table 2.
Posthospital Functional Ability and Home Health Utilization Comparing Patients Living Alone Versus with Others After Discharge
| Characteristic | Alone (n=141) n(%) | With Others (n=171) n(%) | P Value* |
|---|---|---|---|
| Functional ability after discharge | |||
| Dependent in 1-2 ADLs† | 54 (38) | 73 (42.7) | |
| Dependent in 3-6 ADLs | 3 (2) | 34 (19.9) | .001‡ |
| Unable to or needs help with | |||
| Dressing | 17 (12) | 47 (27) | .001 |
| Eating | 2 (1) | 25 (14) | .001 |
| Toileting | 2 (1) | 24 (14) | .001 |
| Transferring | 3 (2) | 27 (16) | .001 |
| Walking across a room | 3 (2) | 17 (10) | .003 |
| Dependent in 1-3 IADLs§ | 64 (45) | 43 (25) | |
| Dependent in 4-7 IADLs | 74 (52) | 126 (74) | .001‡ |
| Unable to or needs help with | |||
| Preparing meals | 74 (52) | 132 (77) | .001 |
| Taking medication | 45 (32) | 98 (57) | .001 |
| Uses assistive device‖ | 69 (50) | 90 (53) | .564 |
| Homebound¶ | 86 (61) | 94 (55) | .284 |
| Received home health services from# | |||
| Registered nurse | 140 (99.3) | 169 (100) | .273 |
| Physical therapist | 64 (45.4) | 91 (53.9) | .138 |
| Occupational therapist | 36 (25.5) | 30 (17.8) | .096 |
| Home health aide | 71 (50.4) | 59 (34.9) | .006 |
Test for significance comparing living alone versus living with someone.
Activities of daily living (ADL), maximum = 6 (bathing, dressing, toileting, transferring, walking and eating).
χ2test for ordinal variables.
Instrumental activities of daily living (IADL), maximum = 7 (telephoning, transportation, shopping, meal preparation, housework, medications and ability to handle finances).
Assistive device included cane, wheeled walker, standard walker, and wheelchair.
Homebound defined as not going outdoors even when the weather was favorable.
Data available on 141 patients living alone, 169 living with others.
Temporal Changes in ADL and IADL Function from Prehospital to 1-Month Postdischarge
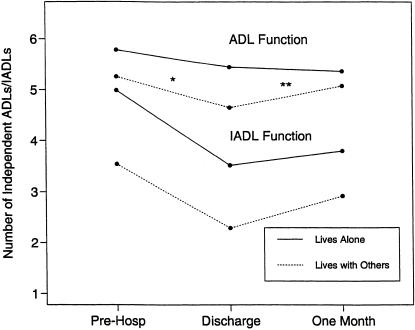
Figure 1 shows mean functional status over the 3 time periods (prehospital, discharge, 1-month postdischarge) according to living arrangement. Although both groups showed a decline in ADL function from prehospitalization to discharge, the group that lived alone showed significantly less improvement in the month after discharge compared with the group living with others (P = .0001). A decline in IADL function was demonstrated in both groups from prehospitalization to discharge. For both groups, recovery of IADL function 1 month later was only partial.
FIGURE 1.
Change in ADL and IADL function over time comparing patients living alone versus those living with others. For ADL function, P = .0001 for time-group interaction. For IADL function, P = .708 for time-group interaction. *P = .0193 comparing ADL change (prehospital to discharge) for living alone group versus living with others group. **P = .0001 comparing ADL change (discharge to 1-month) for living alone group versus living with others group.
At discharge, most patients were dependent in only 1 ADL. Among patients dependent in only 1 ADL, most were dependent in bathing (29 of 30 patients who lived alone; 32 of 38 who lived with others). Of patients dependent in bathing and only bathing, 6 (21%) of 29 patients living alone improved versus 18 (56%) of 32 patients living with others (P = .005). Among patients dependent in 2 ADLs at discharge, all were dependent in bathing, and most were dependent in dressing (11 of 13 patients who lived alone, and 16 of 20 patients who lived with others). Of patients dependent in dressing (plus/minus another ADL), 7 (64%) of 11 who lived alone improved versus 11 (69%) of 16 who lived with others (P = .78). Thus, patients who lived alone differed from those living with others in the likelihood of improving in bathing, but not in dressing.
One-Month Outcomes, Adjusting for Other Covariates
Lack of Improvement in ADL Function
Among the subgroup of patients who were dependent in ADL function at discharge and had complete 1-month functional data (n = 130), 63.6 % of patients who lived alone did not improve (47.7% stayed the same in ADLs, and 15.9% worsened). Among those who lived with others, 39.5% did not improve (31.4% stayed the same, and 8.1% worsened). Table 3 shows the unadjusted and adjusted odds ratios (OR) for not improving in ADL function if a patient lived alone after hospitalization. In logistic regression after adjusting for age, cognitive status, prehospital assistive device use, and discharge function (base model), patients who lived alone were approximately 3 times more likely to not improve in ADL function compared with those who lived with others. This effect was the same after adjusting for sex. We examined the relationship between the likelihood of not improving and level of ADL function at discharge, excluding ADL levels below 4 as only 1 patient had an ADL level in this category and lived alone. For discharge ADL levels above 4, the effect of living alone did not vary by level of discharge function.
Table 3.
Association of Living Alone with Lack of Improvement in ADL Function and Nursing Home Placement in the Month After Hospital Discharge
| Odds Ratio (95% Confidence Interval) | ||||||
|---|---|---|---|---|---|---|
| Adverse Outcome | Population at Risk | Number with Outcome (%) | Unadjusted | Age-Adjusted | Base Model | Base Model with Gender* |
| No improvement in ADL function | 130† | 68 (53) | 2.68 (1.26 to 5.67) | 2.78 (1.30 to 5.93) | 3.01 (1.26 to 7.18)‡ | 3.10 (1.27 to 7.54) |
| Admitted to nursing home | 288 | 14 (5) | 2.45 (0.80 to 7.51) | 2.38 (0.77 to 7.35) | 3.47 (1.01 to 11.90)§ | 2.98 (0.84 to 10.53) |
Gender added as covariate to base model for each outcome.
Indicates the number of patients with activity of daily living (ADL) dependency at discharge, excluding 34 patients who were dependent at discharge but lacked 1-month outcomes.
Adjusted for age, Mini-Mental State Examination (MMSE), prehospital assistive device use, and discharge ADL function. Discharge ADL function categorized as ADL score of 5 versus <5. Mini-Mental State Examination used as continuous variable.
Adjusted for age, MMSE, and ADL function at discharge. Discharge ADL function categorized as ADL score of 6, 5, or <5. Mini-Mental State Examination used as continuous variable.
Nursing Home Utilization.
At 1-month postdischarge, of those originally discharged home, 9 (7.2%) of those living alone had been admitted to a nursing home compared with 5 (3.1%) of those living with others. As shown in Table 3, nursing home admission 1-month postdischarge was significantly increased for patients living alone after adjusting for age, cognitive status, and discharge functional ability (base model). The risk remained high after adjusting for gender but did not reach significance.
Association of 1-Month Outcomes with Availability of Informal Support
Fifty-one percent of patients who lived alone were visited at least daily by another person during the week after hospital discharge. In logistic regression using the same covariates as in the base models, the frequency of informal support was significantly related to both functional improvement and nursing home placement. Patients who lived alone who were visited less than daily were more likely to have lack of improvement in ADLs (OR, 6.31; 95% confidence interval [95% CI], 1.74 to 22.82 vs reference group of living with someone) than were those who were visited daily (OR, 2.23; 95% CI, 0.73 to 6.84 vs reference group of living with someone). These effects were consistent after controlling for sex.
Interestingly, a reverse relationship was noted with level of informal support and nursing home placement. After adjusting for age, cognition, and discharge function, patients living alone with more informal supports were more likely to go to a nursing home (OR, 6.2; 95% CI, 1.64 to 23.48 vs reference group of living with someone) than those with fewer informal supports (OR, 2.9; 95% CI, 0.57 to 14.35 vs living with someone). These effects were consistent after controlling for gender.
DISCUSSION
In our study, almost half of patients who received home nursing services following medical hospitalization lived alone. Patients living alone had a substantial burden of dependency in very basic tasks. Half needed help preparing meals, and almost half were dependent in 1 or more ADLs. Inability to perform these tasks or to obtain help in performing them poses a significant threat to independent living.
Our data suggest that those who live alone, although at a higher functional level both prehospital and at discharge, are less likely to improve in ADL function in the month after discharge, even after controlling for age, cognitive ability, prehospital assistive device use, and discharge function. The poorer improvement among the living alone group is not just due to their higher discharge functional level. Our results are consistent across different ADL levels, suggesting that the effect of living alone is independent of discharge function. Patients discharged from the hospital to home alone are also more likely to be admitted to a nursing home in the month following discharge.
While previous studies have evaluated the effects of task support or marital status on ADL outcomes posthospitalization,11–13 there is little research specifically examining the effects of living alone. Wilcox et al. found that lack of adequate task support 6 weeks posthospitalization for stroke, myocardial infarction, or hip fracture predicted increased disability 6 months later.13 Oxnam et al. found that adequacy of social support predicted subsequent functional level for patients following open heart surgery.11 Finally, Verbrugge et al. demonstrated lower self-rated health and activity levels for unmarried older adults posthospitalization.12 Our data complement these studies by extending findings of increased risk to the general medical population and by demonstrating that functional recovery is jeopardized for those living alone.
In addition, our study clarifies the relationship between type of ADL dependency and likelihood of improvement. There was no difference in likelihood of improvement in dressing; however, patients who lived alone were significantly less likely to improve in bathing. Bathing is a complex physical activity that poses significant challenges to postural control. Indeed, older adults are more fearful of falling while bathing than with any other ADL or IADL.28–30 Patients who live alone may be more afraid of falling because of their higher risk for a long lie and thus are more reluctant to attempt independent bathing.
The trajectory of improvement in IADL function was similar for both groups; however, this does not contradict the findings related to ADLs. For patients who have caregivers at home, IADLs may be slower to improve than ADLs. Independent activities of daily living, such as shopping and meal preparation, are tasks that can be performed by another person. Activities of daily living, such as bathing and toileting, are basic self-care tasks. Patients may have a greater impetus to become independent in basic self-care tasks because of their personal nature.
For patients who lived alone, provision of adequate informal supports from outside the home aided functional recovery. We found that patients who lived alone and had greater frequency of visits from a primary outside support were more likely to improve in function. One reason could be that frequent informal support from an outside source may encourage rehabilitation, improve compliance with medical and physical therapy, and decrease patients' fear of falling. An alternative explanation suggested by Welch et al. is that patients who lack informal supports may remain dependent in ADLs in order to continue to use formal supports, such as home nursing services, to meet their practical needs.31
Admission to a nursing home, whether for a short stay or on a more permanent basis, is one consequence of not being able to obtain help with daily tasks. Previous literature has shown that people living alone are at increased risk for institutionalization,20,21 especially at hospital discharge.8–10 Our study extends previous findings to show that risk of nursing home admission does not end after hospital discharge. Patients who are discharged to home alone with home nursing services remain at increased risk for nursing home admission throughout the subsequent month.
Interestingly, we found that those who lived alone and had a greater frequency of outside informal support from another person were at higher risk for being admitted to a nursing home than those who lived alone with less outside support. One explanation for this could be that closely involved family, friends, or neighbors have a greater sense of responsibility for the person's well-being and are more apt to seek out living arrangements that provide more supervision. An alternative explanation could be that those utilizing more informal supports are more frail. Although we adjusted for multiple measures of frailty, including discharge ADL function, cognition, and prehospital assistive device use, there may have been additional components that we were unable to measure.
Adequate planning during the discharge planning phase from the hospital is necessary to ensure that individuals who live alone will receive sufficient help with ADLs and IADLs. For patients who live alone, discharge planning should take into account the capacities of the patient and the availability of social resources in the home. In particular, patients who live alone after hospital discharge may require more intensive resources to maintain community living and improve in function. In our study, all patients received home nursing services, often including physical therapy and occupational therapy. This suggests that home nursing and rehabilitative services may not be sufficient in intensity, frequency, or duration to provide adequate support to improve ADL function. Informal supports are another important consideration for care provision. Our study suggests such supports may increase functional independence, but may not be sufficient to prevent nursing home admissions. Discharge planning should consider the availability of informal supports for patients who live alone, but should note that they may be of limited benefit in preventing nursing home placement.
There are a number of limitations to this analysis. First, determination of functional status was subjective. In hospitals, subjective report may overestimate ADL function compared with objective performance32 or reports of family and nurses.33 However, our study relied on subjective determination of ADL function within the first week after hospital discharge, and patients may have more accurate knowledge of abilities at this time. Indeed, studies of outpatients have shown a high correlation between objective and subjective functional measures.34,35 To maximize accuracy, we used proxies when necessary, and to prevent measurement error over time, we used the same interviewers and proxies 1 month later. Second, measurement error may result in regression toward the mean over time. However, because ADL function assesses categorical abilities rather than continuous numerical data, measurement error is less likely to occur. A third concern is the potential for reporting bias by those living alone (i.e., bias toward overestimating function at discharge compared with those living with others). However, in a separate study (the St. Mary's site of the Hospital Outcomes Project for the Elderly) that examined objective and subjective ADLs at hospital discharge, patients who lived alone were no more likely to overestimate function than patients who lived with others (M. Jalaluddin, personal communication, September 1998). Fourth, small sample size may have decreased our ability to control for multiple additional risk factors and to evaluate the effect of living alone independent of gender. However, other potential risk factors from the literature were examined and included if significant, or borderline significant, in univariate analysis. Fifth, our sample consisted of predominantly white and fairly well-educated patients. Significant racial differences in posthospitalization formal and informal care patterns exist,36 and our findings may not be generalizable to nonwhite populations. In addition, this study excluded patients who had a recent stroke or myocardial infarction, were nonambulatory, or had a diagnosis of dementia, and lived alone. Thus, our data apply primarily to those ambulatory at home after a general medical hospitalization. However, similar findings have been found for poststroke and post-myocardial infarction populations.13 Finally, our findings apply only to the first month after discharge. However, 1-month outcomes are of particular relevance, given the fact that home health expenditures are greatest in the immediate posthospital period.
From 33% to 44% of hospitalized older adults receive home health services following discharge;37,38 thus, this study potentially represents a large segment of the post-hospitalization population. Our study shows that older adults who live alone after hospital discharge and receive home nursing services frequently have a significant burden of dependency in ADLs and IADLs that jeopardizes their ability to live independently. Patients who live alone after hospitalization are less likely to improve in ADL function and are more likely to be admitted to a nursing home in the subsequent month. Such patients may benefit from increased social and medical supports to maintain independent living and improve function.
Acknowledgments
This work was supported by grants from the American Physical Therapy Foundation, the Dean Foundation, and the University of Wisconsin Medical School and Graduate School. Dr. Mahoney was the recipient of a Clinical Investigator Award from the NIA (K08AG00623).
The authors gratefully acknowledge Jill Johnson, PT and Diane Krueger for research assistance, and M. Jalaluddin, MS for assistance with data management.
REFERENCES
- 1.Hirsch CH, Sommers L, Olsen A, Mullen L, Winograd CH. The natural history of functional morbidity in hospitalized older patients. J Am Geriatr Soc. 1990;38:1296–1303. doi: 10.1111/j.1532-5415.1990.tb03451.x. [DOI] [PubMed] [Google Scholar]
- 2.McVey LJ, Becker PM, Saltz CC, Feussner JR, Cohn HJ. Effect of a geriatric consultation team on functional status in elderly hospitalized patients. Ann Intern Med. 1989;110:78–84. doi: 10.7326/0003-4819-110-1-79. [DOI] [PubMed] [Google Scholar]
- 3.Sager MA, Franke T, Inouye SK, Landefeld S, Morgan TM, Rudberg MA, et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med. 1996;156:645–52. [PubMed] [Google Scholar]
- 4.Sager MA, Rudberg MA, Jalaluddin M, et al. Hospital admission risk profile (HARP): identifying older patients at risk for functional decline following acute medical illness and hospitalization. J Am Geriatr Soc. 1996;44:251–7. doi: 10.1111/j.1532-5415.1996.tb00910.x. [DOI] [PubMed] [Google Scholar]
- 5.Covinsky KE, Justice AC, Rosenthal GE, Palmer RM, Landefeld CS. Measuring prognosis and case mix in hospitalized elders: the importance of functional status. J Gen Intern Med. 1997;12:203–8. doi: 10.1046/j.1525-1497.1997.012004203.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lamont CT, Sampson S, Matthias R, Kane R. The outcome of hospitalization for acute illness in the elderly. J Am Geriatr Soc. 1983;31:282–8. doi: 10.1111/j.1532-5415.1983.tb04872.x. [DOI] [PubMed] [Google Scholar]
- 7.Wu AW, Damiano AM, Lynn J, et al. Predicting future functional status for seriously ill hospitalized adults: the SUPPORT prognostic model. Ann Intern Med. 1995;122:342–50. doi: 10.7326/0003-4819-122-5-199503010-00004. [DOI] [PubMed] [Google Scholar]
- 8.Wachtel TJ, Fulton JP, Goldfarb J. Early prediction of discharge disposition after hospitalization. Gerontologist. 1987;27:98–102. doi: 10.1093/geront/27.1.98. [DOI] [PubMed] [Google Scholar]
- 9.Narain P, Rubenstein LZ, Wieland GD, et al. Predictors of immediate and 6-month outcomes in hospitalized elderly patients: the importance of functional status. J Am Geriatr Soc. 1988;36:775–83. doi: 10.1111/j.1532-5415.1988.tb04259.x. [DOI] [PubMed] [Google Scholar]
- 10.Rudberg MA, Sager MA, Zhang J. Risk factors for nursing home use after hospitalization for medical illness. J Gerontol. 1996;51:M189–94. doi: 10.1093/gerona/51a.5.m189. [DOI] [PubMed] [Google Scholar]
- 11.Oxman TE, Hull JG. Social support, depression, and activities of daily living in older heart surgery patients. J Gerontol. 1997;52B:P1–14. doi: 10.1093/geronb/52b.1.p1. [DOI] [PubMed] [Google Scholar]
- 12.Verbrugge LM, Balaban DJ. Patterns of change in disability and well-being. Med Care. 1989;27(suppl):S128–47. doi: 10.1097/00005650-198903001-00011. [DOI] [PubMed] [Google Scholar]
- 13.Wilcox VL, Kasl SV, Berkman LF. Social support and physical disability in older people after hospitalization: a prospective study. Health Psychol. 1994;13:170–9. doi: 10.1037//0278-6133.13.2.170. [DOI] [PubMed] [Google Scholar]
- 14.Mahoney J, Drinka TJK, Abler R, et al. Screening for depression: single question vs. GDS. J Am Geriatr Soc. 1994;42 doi: 10.1111/j.1532-5415.1994.tb06597.x. [DOI] [PubMed] [Google Scholar]
- 15.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 16.Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. 1970;10:20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 17.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- 18.Glazebrook K, Rockwood K, Stole P, Fisk J, Gray JM. A case control study of the risks for institutionalization of elderly people in Nova Scotia. Can J Aging. 1994;13:104–17. [Google Scholar]
- 19.Wachtel TJ, Derby C, Fulton C. Predicting the outcome of hospitalization for elderly persons: home versus nursing home. Southern Med J. 1984;77:1283–5. doi: 10.1097/00007611-198410000-00020. [DOI] [PubMed] [Google Scholar]
- 20.Wolinsky FD, Callahan CM, Fitzgerald JF, Johnson RJ. The risk of nursing home placement and subsequent death among older adults. J Gerontol. 1992;47:S172–82. doi: 10.1093/geronj/47.4.s173. [DOI] [PubMed] [Google Scholar]
- 21.Branch LG, Jette AM. A prospective study of long-term care institutionalization among the aged. Am J Public Health. 1982;72:1373–9. doi: 10.2105/ajph.72.12.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jette AM, Branch LG, Sleeper LA, Feldman H, Sullivan LM. High-risk profiles for nursing home admission. Gerontologist. 1992;32:634–40. doi: 10.1093/geront/32.5.634. [DOI] [PubMed] [Google Scholar]
- 23.Greene VL, Ondrich JI. Risk factors for nursing home admissions and exits: a discrete-time hazard function approach. J Gerontol. 1990;45:S250–8. doi: 10.1093/geronj/45.6.s250. [DOI] [PubMed] [Google Scholar]
- 24.Winograd CH, Lindenberger EC, Chavez CM, Mauricio MP, Shi H, Bloch DA. Identifying hospitalized older patients at varying risk for physical performance decline: a new approach. J Am Geriatr Soc. 1997;45:604–9. doi: 10.1111/j.1532-5415.1997.tb03095.x. [DOI] [PubMed] [Google Scholar]
- 25.Femia EE, Zarit SH, Johansson B. Predicting change in activities of daily living: a longitudinal study of the oldest old in Sweden. J Gerontol B Psychol. 1997;53:294–302. doi: 10.1093/geronb/52b.6.p294. [DOI] [PubMed] [Google Scholar]
- 26.Mahoney J, Sager MA, Jalaluddin M. Use of an ambulation assistive device predicts functional decline associated with hospitalization. J Gerontology. 1999;54A:M83–8. doi: 10.1093/gerona/54.2.m83. [DOI] [PubMed] [Google Scholar]
- 27.Covinsky KE, Fortinsky RH, Palmer RM, Kresevic DM, Landefeld CS. Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons. Ann Intern Med. 1997;126:417–25. doi: 10.7326/0003-4819-126-6-199703150-00001. [DOI] [PubMed] [Google Scholar]
- 28.Lachman ME, Howland J, Tennstedt S, Jette A, Assmann S, Peterson EW. Fear of falling and activity restriction: the survey of activities and fear of falling in the elderly (SAFE) J Gerontol. 1998;53B:P43–50. doi: 10.1093/geronb/53b.1.p43. [DOI] [PubMed] [Google Scholar]
- 29.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) scale. J Gerontol. 1995;50A:M28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 30.Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45:P239–43. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- 31.Welch HG, Wennberg DE, Welch WP. The use of medicare home health care services. N Engl J Med. 1996;335:324–9. doi: 10.1056/NEJM199608013350506. [DOI] [PubMed] [Google Scholar]
- 32.Sager MA, Dunham NC, Schwantes A, Mecum L, Halverson K, Harlowe D. Measurement of activities of daily living in hospitalized elderly: a comparison of self-report and performance-based methods. J Am Geriatr Soc. 1992;40:457–62. doi: 10.1111/j.1532-5415.1992.tb02011.x. [DOI] [PubMed] [Google Scholar]
- 33.Rubenstein LZ, Schairer C, Wieland GD, Kane R. Systematic biases in functional status assessment of elderly adults: effects of different data sources. J Gerontol. 1984;39:686–91. doi: 10.1093/geronj/39.6.686. [DOI] [PubMed] [Google Scholar]
- 34.Reuben DB, Siu AL, Kimpau S. The predictive validity of self-report and performance-based measures of function and health. J Gerontol. 1992;47:M106–10. doi: 10.1093/geronj/47.4.m106. [DOI] [PubMed] [Google Scholar]
- 35.Elam JT, Graney MJ, Beaver T, el Derwi D, Applegate WB, Miller ST. Comparison of subjective ratings of function with observed functional ability of frail older persons. Am J Public Health. 1991;81:1127–30. doi: 10.2105/ajph.81.9.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chadiha LA, Proctor EK, Morrow-Howell N, Darkwa OK, Dore P. Post-hospital home care for African-American and white elderly. Gerontologist. 1995;35:233–9. doi: 10.1093/geront/35.2.233. [DOI] [PubMed] [Google Scholar]
- 37.Solomon DH, Wagner DR, Marenberg ME, Acampora D, Cooney LM, Inouye SK. Predictors of formal home health care use in elderly patients after hospitalization. J Am Geriatr Soc. 1993;41:961–6. doi: 10.1111/j.1532-5415.1993.tb06762.x. [DOI] [PubMed] [Google Scholar]
- 38.Mahoney J, Sager M, Dunham NC, Johnson J. Risk of falls after hospital discharge. J Am Geriatr Soc. 1994;42:269–74. doi: 10.1111/j.1532-5415.1994.tb01750.x. [DOI] [PubMed] [Google Scholar]