Abstract
OBJECTIVE
Throughout the 1990s, the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure recommended initial antihypertensive therapy with a thiazide diuretic or a β-blocker based on evidence from randomized, controlled trials, unless an indication existed for another drug class. The committee also recommended β-blockers in hypertensive patients with a history of myocardial infarction (MI), and angiotensin-converting enzyme (ACE) inhibitors in patients with congestive heart failure (CHF). Our objective was to determine whether prescribing practices for older hypertensive patients are consistent with evidence-based guidelines.
METHODS
We examined prescription patterns from January 1, 1991 through December 31, 1995 for 23,748 patients 65 years or older with a new diagnosis of hypertension from the New Jersey Medicaid program and that state's Pharmacy Assistance for the Aged and Disabled program (PAAD). We linked drug use data with information on demographic variables and comorbid medical conditions.
RESULTS
During the study period, calcium channel blockers were the most commonly prescribed initial therapy for hypertension (41%), followed by ACE inhibitors (24%), thiazide diuretics (17%), and β-blockers (10%). Eliminating patients with diabetes mellitus, CHF, angina, or history of MI did not substantially affect these results. Overall, initial use of a thiazide declined from 22% in 1991 to 10% in 1995, while initial use of a calcium channel blocker increased from 28% to 43%, despite publication during these years of studies demonstrating a benefit of thiazides in older patients. Only 15% of older hypertensive patients with a history of MI received β-blockers.
CONCLUSIONS
Prescribing practices for older hypertensive patients are not consistent with evidence-based guidelines. Interventions are needed to encourage evidence-driven prescribing practices for the treatment of hypertension.
Keywords: hypertension, evidence-based medicine, older patients
The Sixth Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI), recommends initial hypertension treatment with diuretics and β-blockers, unless there are specific indications for a different drug class.1 These same recommendations were promulgated in JNC V, published in January of 1993.2 JNC IV, published in 1988, had recommended initial therapy with any of the 4 major classes of antihypertensives.3 The change in recommendations in 1993 was supported by 3 major trials of antihypertensive therapy with thiazide diuretics or β-blockers in older patients published in 1991 and 1992.4–6 However, despite these clinical trial data and recommendations, prescriptions for thiazides and β-blockers declined in the early 1990s,7–9 continuing a trend toward decreased thiazide use that began in the 1980s.10
Further, randomized, controlled trial data indicate that patients with particular diagnoses are likely to benefit from a specific antihypertensive agent. For example, among hypertensive patients with congestive heart failure (CHF) or diabetes mellitus, an angiotensin-converting enzyme (ACE) inhibitor is likely to be a rational choice, based on evidence that ACE inhibitors reduce mortality in patients with CHF11,12 and can reduce nephropathy13,14 in diabetic patients. Similarly, a β-blocker would be the drug of choice for most hypertensive patients with a history of myocardial infarction (MI), given the data showing a mortality benefit in this setting.15,16
To assess whether prescribing practices for older hypertensive patients are consistent with such trials and guidelines, we examined prescription patterns among 23,748 patients aged 65 years and older with a diagnosis of hypertension, using Medicaid and Medicare data encompassing all health care encounters and filled prescriptions. This database enabled us to examine the association between comorbidity and demographic factors and prescribing patterns in order to determine whether prescribing practices are consistent with evidence-based recommendations in the older population as a whole as well as in specific patient subgroups.
METHODS
Sources of Data
The study population was drawn from enrollees aged 65 years and older in the New Jersey Medicaid program and that state's Pharmacy Assistance for the Aged and Disabled (PAAD) program for the period from January 1, 1991 through December 31, 1995. Eligibility for Medicaid requires an income below the poverty level, whereas the PAAD program provides drug coverage to patients with modest incomes who are not eligible for Medicaid. Information on all filled prescriptions was extracted from the paid claims files of these programs. Previous studies have shown a high degree of reliability and validity of such prescription data.17,18 We restricted our analyses to patients with a diagnosis of hypertension newly begun on a single antihypertensive agent. We then linked drug use data with information on other health service use to identify medical diagnoses. Personal identifiers were removed from all claims to protect the confidentiality of program participants.
During the study period, New Jersey's Medicaid program had no deductible or maximum benefit for drugs, and charged no copayment for prescribed medications. New Jersey's PAAD program had no deductible and no maximum benefit but had a $2 copayment for each prescription filled. In addition, neither program had formulary restrictions during the study period. Given the economic incentives to fill prescriptions through these channels, almost all patients eligible for Medicaid and PAAD fill their prescriptions through the system.
Hypertensive subjects were identified as having either an outpatient or an inpatient diagnosis of hypertension as defined by codes from the International Classification of Diseases, Ninth Revision (ICD-9). The earliest qualifying date from 1991 to 1995 on which the patient filled a first prescription for any antihypertensive medication was defined as the index date. To ensure that all patients were active participants in the drug programs studied and were newly begun on antihypertensive medication, we required that patients fill at least one prescription in the period more than 6 months prior to the index date and fill at least one prescription during the 6 months immediately prior to the index date.
For each patient studied, we identified several characteristics which might influence prescribing patterns. These included age, race, gender, use of the Medicaid program, number of nonantihypertensive prescription drugs filled in the prior 180 days, and nursing home residency in the 180 days prior to the index date. We also identified the following comorbidities 180 days prior to the index date: diabetes mellitus, MI, CHF, angina, chronic obstructive pulmonary disease (COPD), and asthma. Inpatient and outpatient ICD-9 codes, along with filled insulin or oral hypoglycemic prescriptions, were used to identify diabetics. Inpatient and outpatient ICD-9 codes were also used to identify subjects with a history of MI, CHF, or angina. Diagnosis-related group (DRG) codes were used to identify hospitalizations for COPD and asthma to identify patients with active pulmonary disease in whom β-blockers would be contraindicated. Outpatient diagnoses and use of pulmonary medications were not used to identify such patients in order to identify only those with higher disease severity in whom β-blocker therapy would clearly be contraindicated.
Statistical Analysis
Predictors of specific antihypertensive therapy use were identified by placing all of the prespecified potential predictors individually into separate logistic regression models. The outcome variables studied were use of one of four specific antihypertensive medication classes to initiate therapy: thiazide diuretics, β-blockers, calcium channel blockers, or ACE inhibitors. We excluded from our main analyses the relatively small number of patients who were prescribed other antihypertensive medications. We examined trends in prescribing in all of the analyses. For our initial analyses, we chose thiazides as the referent group because of the strength of the evidence for their use in older patients. First, we analyzed the likelihood of being prescribed a thiazide relative to all other major antihypertensive medications. Second, we separately examined β-blocker, calcium channel blocker, or ACE inhibitor use relative to thiazides. Third, we separately examined prescription patterns for preferred antihypertensive therapy in subjects with CHF, diabetes mellitus, and a history of MI. For patients with CHF and diabetes mellitus, we compared ACE inhibitor prescriptions with prescriptions for the other major antihypertensive medications. For patients with a history of MI, we compared β-blocker prescriptions with the other major antihypertensive medications. All results were analyzed using SAS software, version 6.12 (SAS Institute, Cary, NC).
RESULTS
We identified 23,748 new users of antihypertensive medications during the study period; their mean age was 76 ± 7 years (range, 65 to 99). Of these, 11,103 had at least 1 of the following comorbid conditions: diabetes mellitus, CHF, history of MI, or history of angina. The demographic and clinical characteristics of patients and their patterns of antihypertensive medication use are presented in Table 1.
Table 1.
Antihypertensive Medication Usage
| Variable | n (%) | Thiazide (%) | β-blocker | Calcium Channel Blocker (%) | ACE inhibitor (%) |
|---|---|---|---|---|---|
| All patients | 23,748 (100) | 17 | 10 | 42 | 24 |
| Age, y | |||||
| 65 to 74 | 10,995 (46) | 15 | 12 | 43 | 23 |
| 75 to 84 | 9,694 (41) | 18 | 10 | 41 | 24 |
| ≥85 | 3,059 (13) | 19 | 7 | 40 | 27 |
| Male | 6,683 (28) | 13 | 10 | 43 | 26 |
| Race | |||||
| White | 18,069 (76) | 17 | 11 | 40 | 25 |
| African American | 3,786 (16) | 16 | 6 | 48 | 21 |
| Nursing home patients | 1,964 (8) | 9 | 6 | 51 | 27 |
| Medicaid enrollees | 8,662 (36) | 13 | 7 | 48 | 25 |
| Comorbidities | |||||
| Diabetes | 5,219 (22) | 13 | 8 | 44 | 28 |
| CHF | 4,206 (18) | 8 | 7 | 39 | 41 |
| Angina | 5,912 (25) | 9 | 11 | 50 | 25 |
| History of MI | 1,402 (6) | 6 | 15 | 46 | 29 |
| Severe COPD/asthma | 446 (2) | 12 | 2 | 59 | 21 |
| No. of other medications | |||||
| 1 | 5,854 (25) | 17 | 13 | 40 | 22 |
| 2 to 4 | 10,396 (44) | 17 | 11 | 41 | 23 |
| ≥5 | 7,498 (32) | 16 | 8 | 44 | 26 |
ACE indicates angiotension-converting enzyme; CHF, congestive heart failure; MI, myocardial infarction; COPD, chronic obstructive pulmonary disease.
From 1991 to 1995, in the entire population of hypertensive patients, the most commonly prescribed initial antihypertensive drugs were calcium channel blockers, used by 42% of patients, followed by ACE inhibitors (24%), thiazides (17%), β-blockers (10%), central antiadrenergic agents (4%), peripheral antiadrenergic agents (3%), α-blockers (<1%), direct vasodilators (<1%), and angiotensin II receptor blockers (<1%). Among the 12,645 patients with uncomplicated hypertension who lacked the comorbid conditions listed above, calcium channel blockers were also the most commonly used initial drugs (38% of patients), followed by thiazides (22%), ACE inhibitors (21%), and β-blockers (11%).
Using multivariate analysis to control for comorbidity and patient demographics, we found that the likelihood of being on a thiazide declined 9% per year (95% confidence interval [CI], 7% to 10%) relative to all other antihypertensives (Table 2). Patients who were older or used five or more other medications were more likely to receive thiazides than other major antihypertensives. By contrast, several characteristics were associated with a reduced likelihood of receiving thiazides relative to all other major antihypertensives (Table 2). These results did not change substantially when we eliminated patients with angina, CHF, diabetes mellitus, or history of MI from the analysis.
Table 2.
Multivariate Model of Thiazide Use Relative to All Other Antihypertensives
| Variable | All Patients, OR (95% CI ) | Patients Without Angina, CHF, Diabetes, or History of MI, OR (95% CI ) |
|---|---|---|
| Time (per year)* | 0.92 (0.90 to 0.93) | 0.92 (0.90 to 0.94) |
| Age, y | ||
| 75 to 84* | 1.17 (1.08 to 1.26) | 1.13 (1.03 to 1.24) |
| ≥85† | 1.38 (1.24 to 1.55) | 1.30 (1.13 to 1.48) |
| Male | 0.72 (0.66 to 0.78) | 0.64 (0.58 to 0.72) |
| African American | 1.00 (0.91 to 1.11) | 1.01 (0.89 to 1.15) |
| Nursing home resident | 0.76 (0.64 to 0.91) | 0.70 (0.53 to 0.92) |
| Medicaid | 0.72 (0.66 to 0.79) | 0.69 (0.63 to 0.77) |
| No. of other medications‡ | ||
| 2 to 4 | 1.03 (0.94 to 1.12) | 1.04 (0.94 to 1.15) |
| ≥5 | 1.22 (1.11 to 1.35) | 1.13 (1.00 to 1.28) |
| Diabetes | 0.80 (0.73 to 0.88) | — |
| CHF | 0.56 (0.50 to 0.64) | — |
| History of MI | 0.52 (0.41 to 0.66) | — |
| COPD/asthma | 1.02 (0.76 to 1.37) | 0.92 (0.55 to 1.58) |
| Angina | 0.52 (0.47 to 0.58) | — |
The time variable represents the odds ratio (OR) per year of receiving a thiazide relative to other major antihypertensive medications.
Compared with subjects aged 65 to 74 years.
Compared with subjects on one other medication.
CHF indicates congestive heart failure; MI, myocardial infarction; CI, confidence interval; COPD, chronic obstructive pulmonary disease.
Calcium channel blockers were more likely to be prescribed than thiazides to men, African Americans, Medicaid enrollees, nursing home residents, diabetics, and those with a history of pulmonary disease or angina; patients aged 75 years and older were the only group less likely to be prescribed calcium channel blockers (Table 3). ACE inhibitors were more commonly prescribed relative to thiazides to for men, Medicaid enrollees, diabetics, CHF patients, and patients with a history of MI or angina; patients aged 85 years and older, African Americans, and patients with pulmonary disease were less likely to initially receive this class of antihypertensive medication compared with thiazides (Table 3). Beta-blockers were more likely to be the initial therapy compared with thiazides for patients who had had a history of MI, or angina; β-blockers were less likely to be the initial therapy for patients aged 75 years and older, African Americans, or those having Medicaid enrollment, polypharmacy (use of 5 or more other medications), diabetes mellitus, or pulmonary disease (Table 3).
Table 3.
Multivariate Model of Factors Associated with Specific Antihypertensive Therapy Compared with Thiazide Therapy
| Variable | Calcium Channel Blocker, OR (95% CI ) | ACE Inhibitor, OR (95% CI ) | β-blocker, OR (95% CI ) |
|---|---|---|---|
| Time (per year)* | 1.08 (1.07 to 1.10) | 1.09 (1.07 to 1.10) | 1.04 (1.02 to 1.06) |
| Age, y† | |||
| 75 to 84 | 0.90 (0.83 to 0.96) | 0.92 (0.85 to 1.00) | 0.68 (0.61 to 0.75) |
| ≥85 | 0.77 (0.69 to 0.85) | 0.85 (0.75 to 0.96) | 0.52 (0.43 to 0.61) |
| Male | 1.09 (1.01 to 1.18) | 1.10 (1.01 to 1.20) | 0.90 (0.81 to 1.01) |
| African American | 1.10 (1.01 to 1.21) | 0.77 (0.69 to 0.86) | 0.54 (0.46 to 0.64) |
| Nursing home resident | 1.21 (1.04 to 1.40) | 0.93 (0.78 to 1.11) | 0.89 (0.69 to 1.14) |
| Medicaid | 1.44 (1.33 to 1.56) | 1.23 (1.13 to 1.35) | 0.85 (0.75 to 0.96) |
| No. of other medications‡ | |||
| 2 to 4 | 0.99 (0.91 to 1.07) | 0.98 (0.89 to 1.08) | 0.82 (0.73 to 0.92) |
| ≥5 | 0.94 (0.85 to 1.03) | 0.94 (0.84 to 1.04) | 0.69 (0.60 to 0.79) |
| Diabetes | 1.12 (1.03 to 1.22) | 1.28 (1.16 to 1.41) | 0.81 (0.71 to 0.92) |
| CHF | 1.12 (1.00 to 1.25) | 2.95 (2.63 to 3.31) | 0.90 (0.76 to 1.07) |
| History of MI | 1.85 (1.51 to 2.25) | 1.64 (1.32 to 2.03) | 2.99 (2.35 to 3.81) |
| Severe COPD/asthma | 1.50 (1.15 to 1.96) | 0.65 (0.47 to 0.90) | 0.24 (0.12 to 0.48) |
| Angina | 2.22 (2.02 to 2.43) | 1.30 (1.16 to 1.45) | 2.11 (1.85 to 2.41) |
The time variable represents the odds ratio (OR) per year of receiving the specified antihypertensive medication relative to a thiazide diuretic during the course of the study.
Compared with subjects aged 65 to 74 years.
Compared with subjects on 1 other antihypertensive medication.
ACE indicates angiotensin-converting enzyme; CI, confidence interval; CHF, congestive heart failure; MI, myocardial infarction; COPD, chronic obstructive pulmonary disease.
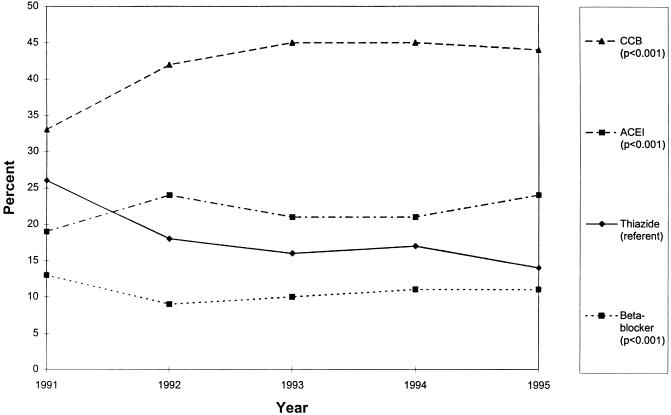
From 1991 to 1995, thiazide use declined from 22% to 10% of new users of antihypertensive medications, β-blocker use was relatively stable (12% to 11%), calcium channel blocker use increased from 37% to 46%, and ACE inhibitor use increased from 21% to 30%. During this same time period, in the subgroup of patients without specific indications for another agent (CHF, a history of MI, diabetes mellitus, or angina), thiazide use decreased from 26% to 14%, β-blocker use decreased from 13% to 11%, calcium channel blocker use increased from 33% to 44%, and ACE inhibitor use increased from 19% to 24% (Fig. 1).
FIGURE 1.
Initial antihypertensive therapy in patients without congestive heart failure, angina, diabetes mellitus, or a history of myocardial infarction. The y-axis is percent of patients receiving the specified medication. The P value represents the trend in prescribing over time relative to thiazide therapy (the referent group). CCB indicates calcium channel blocker; ACE I, angiotensin-converting enzyme inhibitor.
Drug Prescribing in Special Populations
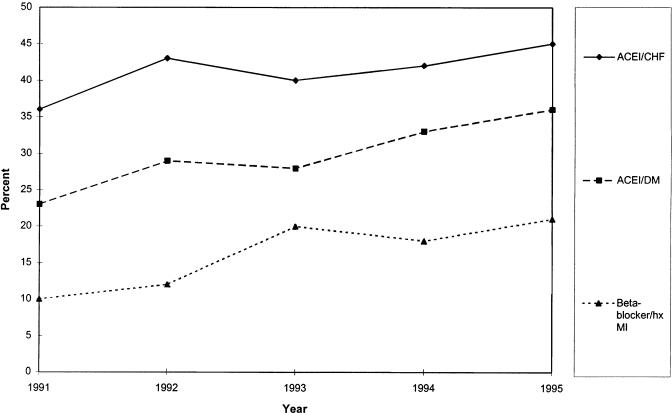
According to our multiple logistic regression analysis, ACE inhibitor use increased at a relative rate of only 4% per year (95% CI, 2% to 6%) compared with other major antihypertensives among the 4,206 patients with CHF, of whom 41% filled prescriptions for this drug class (Fig. 2). Likewise, among the 5,219 diabetics, only 28% were initially prescribed ACE inhibitors, and the relative rate of increase in use of these drugs was 6% (95% CI, 4% to 9%) per year during the study period compared with all other antihypertensives (Fig. 2).
FIGURE 2.
Initial drug choice in hypertensive patients with specific comorbid illnesses. The y-axis is percent of patients with the specified comorbidity. The top line represents the percent of patients with congestive heart failure (CHF) who received angiotensin-converting enzyme inhibitor (ACEI) therapy. The second line is the proportion of diabetics (DM) who received ACEI therapy. The third line is the proportion of patients with a history of myocardial infarction (hx MI) who received β-blocker therapy. For each comorbid illness, there was a statistically significant increase in indicated medication use over time (P < .001).
Among the 1,402 patients with a history of MI, 15% were prescribed β-blockers as the initial antihypertensive therapy. When we eliminated patients with CHF or pulmonary disease, 19% were prescribed β-blockers. However, β-blocker use did increase in post-MI patients at a relative rate of 10% per year (95% CI, 5% to 16%) (Fig. 2). Among the 446 patients with a history of severe COPD or asthma requiring hospitalization, 9 patients were subsequently prescribed β-blockers.
DISCUSSION
Multiple large randomized, controlled trials have yielded extensive data on the clinical outcomes of use of thiazides and β-blockers for the management of hypertension in older persons.19,20 By contrast, only minimal data exists for calcium channel blocker use. Encouraging findings from a 1997 study of nitrendipine in isolated systolic hypertension in older patients,21 published after the time period analyzed here, are counterbalanced by data from observational and experimental studies suggesting a possible increased risk of MI following the use of some calcium channel blockers in the management of hypertension.22–24 The Fifth Report of the JNC, published in January 1993, recommended initial selection of diuretics or β-blockers for the treatment of hypertension.2 This same recommendation was made for older patients, and was based on influential studies of hypertension in the elderly published in 1991 or earlier, including the Systolic Hypertension in the Elderly Program (SHEP).4,5 However, despite these recommendations, the use of these medications declined from 1991 to 1995. One possible explanation for this phenomenon is that compelling comorbid conditions such as diabetes mellitus, CHF, MI, or angina might have warranted the selection of an alternative agent such as a calcium channel blocker or ACE inhibitor. However, when we excluded all patients with these comorbid conditions, recommended medication use still declined.
These results are consistent with other data on patterns of antihypertensive medication use7 and extend these results by studying only diagnosed hypertensive patients and examining prescribing patterns in different subsets of these patients. A study by Maclure et al. based on Canadian data reported much higher rates of first-line therapy with thiazides and dramatically lower calcium channel blocker prescriptions.25 These differences might be explained by national differences in prescribing or ongoing educational interventions in British Columbia, the province studied in the Canadian analysis. However, the difference may also be attributable to a different approach to classifying drug use. In the Canadian study, patients who were simultaneously prescribed two different classes of antihypertensives were classified hierarchically in the following order of priority: thiazides, β-blockers, ACE inhibitors, and calcium channel blockers; this would increase the apparent use of the former drugs at the expense of the latter.
Some trends in therapy for specific patient subgroups deserve special comment. For example, 51% of nursing home patients were prescribed calcium channel blockers for the treatment of hypertension, whereas only 9% received thiazides. The reasons for this are unclear. Even after adjusting for factors including age, angina, CHF, and MI, nursing home patients were still much more likely to receive calcium channel blockers. These results are consistent with a major study of antihypertensive prescribing in the nursing home setting.26
The JNC V and VI reports recommend thiazides as first-line therapy for hypertension in African-American patients, and clinical trial data suggest that β-blockers and ACE inhibitors may be less effective than thiazides and calcium channel blockers in lowering blood pressure in older African-American patients.1,27 Nonetheless, thiazides were prescribed to only 16% of African-American patients, and their use over time declined relative to calcium channel blockers.
In accordance with recommendations from controlled trials, 41% of hypertensive patients with CHF received ACE inhibitors, making them the only subgroup of patients not to receive calcium channel blockers as the most commonly prescribed antihypertensive medication. On multivariate analysis, CHF was strongly associated with an increased likelihood of ACE inhibitor therapy. The negative side of this finding is that more than half of hypertensive patients with CHF did not receive ACE inhibitors despite proven benefits of these drugs in this population.11,12 However, it is possible that some of these patients may not have had systolic dysfunction or may have had some other reason for avoiding ACE inhibitor therapy.
The JNC V did not specifically recommend ACE inhibitors for all hypertensive diabetics, but studies published as early as 1988 showed that ACE inhibitors can prevent nephropathy in many patients with insulin-dependent diabetes mellitus,13,14 and more recent studies have extended these findings to non-insulin-dependent diabetics.28 Despite the availability of such trial data, we found that ACE inhibitors were used as initial antihypertensive therapy by only 29% of diabetics. If these trends have not changed, there is reason for concern, particularly in light of a recent trial of the calcium channel blocker nisoldipine for the treatment of hypertension in diabetics, which found it to be associated with a higher rate of fatal and nonfatal MI compared with enalapril.23
Throughout the study period, β-blockers were noticeably underused in patients with a history of MI: only 15% of patients with hypertension and a history of MI were started on β-blockers. This underuse occurred despite extensive clinical trial data on the efficacy of β-blockers after MI that had been published prior to the study period, and explicit recommendations from JNC V for the use of β-blockers in such patients.1,15,16 These results may be consistent with a lack of physician knowledge about the benefits of β-blocker therapy in this clinical setting.29 It is even more surprising that β-blocker use was so infrequent in this hypertensive population as compared with unselected post-MI patients, because physicians actively selected an alternative medication, rather than failing to add an indicated drug.30,31
Among hospitalized patients with diagnoses of COPD or asthma, 58% were prescribed calcium channel blockers, and only 2% received β-blockers. The low rate of β-blocker usage in this population is consistent with guidelines and rational therapy. However, this small percent of patients may still have been exposed to the potential risk of β-blocker therapy in the setting of significant pulmonary disease.
All patients enrolled in the study were enrolled in Medicaid or a state program for pharmacy assistance for patients with modest income (PAAD). Therefore, these results may not be completely generalizable to higher income populations. However, there is no reason to believe that income level would change these results substantially. It is possible that physicians may be more likely to prescribe newer, more expensive medications (calcium channel blockers and ACE inhibitors) to patients in higher socioeconomic classes. Conversely, Medicaid patients do not have to pay for their medications and PAAD patients pay a nominal copayment, so medication cost may be less of a concern in the population studied.
Another limitation may be lack of precise information to determine comorbidity. Many of the comorbidities were ascertained on the basis of ICD-9 or DRG codes, and these codes may be incomplete. For example, a patient may have had multiple problems, and the physician may not have coded each comorbidity of interest. Thus, these codes may have relatively good specificity but limited sensitivity.32 However, this limitation would not be expected to dramatically affect the overall findings.
In summary, we found that from 1991 to1995, thiazides were rarely used for the treatment of hypertension in older patients, even after controlling for the presence of compelling indications for other antihypertensives. The use of thiazides continued to decline throughout the study period, even in the face of extensive data demonstrating the morbidity and mortality benefits of thiazide therapy for hypertension. This decline continues a trend we observed in an earlier study.10 Calcium channel blockers were the most commonly prescribed drugs for the treatment of hypertension, followed by ACE inhibitors, despite limited data on clinical outcomes for both of these medications for the treatment of hypertension. Thus, clinical trial data from the early 1990s and the JNC V recommendation published in January 1993 appear to have had only a limited impact on prescribing. These data also document low use of recommended medications for hypertension in patients with specific comorbidities. One potential explanation for these findings may be aggressive marketing of calcium channel blockers for the initial treatment of hypertension by their manufacturers. Aside from issues of quality of care, these practice patterns have large economic implications, with a year of calcium channel blocker medication use costing as much as $1,000 per year wholesale, compared to less than $15 per year (drug costs) for hydrochlorothiazide.33,34 Additional educational and systems interventions are needed to improve physician prescribing practices for the treatment of hypertension.
Acknowledgments
Dr. Knight was supported by a fellowship from The Medical Foundation and a grant from the Older Americans Independence Center (OAIC) of the Harvard Medical School Division on Aging.
We are grateful to Sharon Hawley for collection of references and Rita Bloom for her help in the preparation of the manuscript.
REFERENCES
- 1.The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997;157:2413–46. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- 2.The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure Arch Intern Med. 1993;153:154–83. [PubMed] [Google Scholar]
- 3.The 1988 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure Arch Intern Med. 1988;48:1023–38. [PubMed] [Google Scholar]
- 4.Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA. 1991;265:3255–64. [PubMed] [Google Scholar]
- 5.Dahlof B, Lindholm LH, Hansson L, Schersten B, Ekbom T, Wester PO. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension). Lancet. 1991;338:1281–5. doi: 10.1016/0140-6736(91)92589-t. [DOI] [PubMed] [Google Scholar]
- 6.Medical Research Council trial of hypertension in older adults: principal results MRC Working Party. BMJ. 1992;304:405–12. doi: 10.1136/bmj.304.6824.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siegel D, Lopez J. Trends in antihypertensive drug use in the United States. JAMA. 1997;278:1745–8. doi: 10.1001/jama.278.21.1745. [DOI] [PubMed] [Google Scholar]
- 8.Psaty BM, Koepsell TD, Yanez ND, et al. Temporal patterns of antihypertensive medication use among older adults, 1989 through 1992. An effect of the major clinical trials on clinical practice? JAMA. 1995;273:1436–8. [PubMed] [Google Scholar]
- 9.Manolio TA, Cutler JA, Furberg CD, Psaty BM, Whelton PK, Applegate WB. Trends in pharmacologic management of hypertension in the United States. Arch Intern Med. 1995;155:829–37. [PubMed] [Google Scholar]
- 10.Monane M, Glynn RJ, Gurwitz JH, Bohn RL, Levin R, Avorn J. Trends in medications choices for hypertension in the elderly: the decline of the thiazides. Hypertension. 1995;25:1045–51. doi: 10.1161/01.hyp.25.5.1045. [DOI] [PubMed] [Google Scholar]
- 11.Effects of enalapril on mortality in severe congestive heart failure Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). The CONSENSUS Trial Study Group. N Engl J Med. 1987;316:1429–35. doi: 10.1056/NEJM198706043162301. [DOI] [PubMed] [Google Scholar]
- 12.Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure The SOLVD Investigators. N Engl J Med. 1991;325:293–302. doi: 10.1056/NEJM199108013250501. [DOI] [PubMed] [Google Scholar]
- 13.Marre M, Chatellier G, Leblanc H, Guyenne TT, Menard J, Passa R. Prevention of diabetic nephropathy with enalapril in normotensive diabetics with microalbuminuria. BMJ. 1988;297:1092–5. doi: 10.1136/bmj.297.6656.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewis EJ, Hunsicker LG, Bain RP, Rhode RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med. 1993;329:1456–62. doi: 10.1056/NEJM199311113292004. [DOI] [PubMed] [Google Scholar]
- 15.Timolol-induced reduction in mortality and reinfarction in patients surviving acute myocardial infarction N Engl J Med. 1981;304:801–7. doi: 10.1056/NEJM198104023041401. [DOI] [PubMed] [Google Scholar]
- 16.A randomized trial of propranolol in patients with acute myocardial infarction I. Mortality results. JAMA. 1982;247:1701–14. doi: 10.1001/jama.1982.03320370021023. [DOI] [PubMed] [Google Scholar]
- 17.Bright RA, Avorn J, Everitt DE. Medicaid data as a resource for epidemiologic studies: strengths and limitations. J Clin Epidemiol. 1989;42:937–45. doi: 10.1016/0895-4356(89)90158-3. [DOI] [PubMed] [Google Scholar]
- 18.Ray WA, Griffin MR. Use of Medicaid data for pharmacoepidemiology. Am J Epidemiol. 1989;129:837–49. doi: 10.1093/oxfordjournals.aje.a115198. [DOI] [PubMed] [Google Scholar]
- 19.Psaty BM, Smith NL, Siscovick DS, Koepsell TD. Health outcomes associated with antihypertensive therapies used as first-line agents. JAMA. 1997;277:739–45. [PubMed] [Google Scholar]
- 20.Messerli FH, Grossman E, Goldbourt U. Are β-blockers efficacious as first-line therapy for hypertension in the elderly? JAMA. 1998;279:1903–7. doi: 10.1001/jama.279.23.1903. [DOI] [PubMed] [Google Scholar]
- 21.Staessen JA, Fagaid R, Thijs L, et al. Randomized double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-EUR) Trial Investigators. Lancet. 1997;350:757–64. doi: 10.1016/s0140-6736(97)05381-6. [DOI] [PubMed] [Google Scholar]
- 22.Alderman MH, Cohen H, Roque R, Madhaven S. Effect of long-acting and short-acting calcium antagonists on cardiovascular outcomes in hypertensive patients. Lancet. 1997;349:594–8. doi: 10.1016/S0140-6736(96)08359-6. [DOI] [PubMed] [Google Scholar]
- 23.Estacio RO, Jeffers BW, Hiatt WR, Biggerstaff SL, Gifford N, Schrier RW. The effect of nisolodipine as compared with enalapril on cardiovascular outcomes in patients with non-insulin-dependent diabetes and hypertension. N Engl J Med. 1998;338:645–52. doi: 10.1056/NEJM199803053381003. [DOI] [PubMed] [Google Scholar]
- 24.Psaty BM, Heckbert SR, Koepsell TD, et al. The risk of myocardial infarction associated with antihypertensive therapies. JAMA. 1995;274:620–5. [PubMed] [Google Scholar]
- 25.Maclure M, Dormuth C, Naumann T, et al. Influences of educational interventions and adverse news about calcium-channel blockers on first-line prescribing of antihypertensive drugs to elderly people in British Columbia. Lancet. 1998;352:943–8. doi: 10.1016/S0140-6736(97)11390-3. [DOI] [PubMed] [Google Scholar]
- 26.Gambassi G, Lapane K, Sgadari A, et al. Prevalence, clinical correlates, and treatment of hypertension in elderly nursing home residents. SAGE (Systematic Assessment of Geriatric Drug Use via Epidemiology) Study Group. Arch Intern Med. 1998;158:2377–85. doi: 10.1001/archinte.158.21.2377. [DOI] [PubMed] [Google Scholar]
- 27.Materson BJ, Reda DJ, Cushman WC, et al. Single-drug therapy for hypertension in men. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. N Engl J Med. 1993;328:914–21. doi: 10.1056/NEJM199304013281303. [DOI] [PubMed] [Google Scholar]
- 28.Ravid M, Lang R, Rachmani R, Lishner M. Long-term renoprotective effect of angiotensin-converting enzyme inhibition in non-insulin-dependent diabetes mellitus: a 7-year follow-up study. Arch Intern Med. 1996;156:286–9. [PubMed] [Google Scholar]
- 29.Ayanian JZ, Hauptman PJ, Guadagnoli E, Antman EM, Pashos CL, McNeil BJ. Knowledge and practices of generalist and specialist physicians regarding drug therapy for acute myocardial infarction. N Engl J Med. 1994;331:1136–42. doi: 10.1056/NEJM199410273311707. [DOI] [PubMed] [Google Scholar]
- 30.Mendelson G, Aronow WS. Underutilization of beta-blockers in older patients with prior myocardial infarction or coronary artery disease in an academic, hospital-based geriatrics practice. J Am Geriatr Soc. 1997;45:1360–1. doi: 10.1111/j.1532-5415.1997.tb02936.x. [DOI] [PubMed] [Google Scholar]
- 31.Sial SH, Malone M, Freeman JL, et al. Beta blocker use in the treatment of community hospital patients discharged after myocardial infarction. J Gen Int Med. 1994;9:599–605. doi: 10.1007/BF02600301. [DOI] [PubMed] [Google Scholar]
- 32.Fisher ES, Whaley FS, Krushat WM, et al. The accuracy of Medicare's hospital claims data: progress has been made, but problems remain. Am J Public Health. 1992;82:243–8. doi: 10.2105/ajph.82.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pearce KA, Furberg CD, Psaty BM, Kirk J. Cost-minimization and the number needed to treat in uncomplicated hypertension. Am J Hypertens. 1998;11:618–29. doi: 10.1016/s0895-7061(97)00488-3. [DOI] [PubMed] [Google Scholar]
- 34.Drug Topics Red Book . Montvale, NJ: Medical Economics Co; 1998. [Google Scholar]