Abstract
A rapid procedure was developed for detection and identification of methicillin-resistant Staphylococcus aureus (MRSA) directly from sterile sites or mixed flora samples (e.g., nose or inguinal swabs). After a rapid conditioning of samples, the method consists of two main steps: (i) immunomagnetic enrichment in S. aureus and (ii) amplification-detection profile on DNA extracts using multiplex quantitative PCR (5′-exonuclease qPCR, TaqMan). The triplex qPCR assay measures simultaneously the following targets: (i) mecA gene, conferring methicillin resistance, common to both S. aureus and Staphylococcus epidermidis; (ii) femA gene from S. aureus; and (iii) femA gene from S. epidermidis. This quantitative approach allows discrimination of the origin of the measured mecA signal. qPCR data were calibrated using two reference strains (MRSA and methicillin-resistant S. epidermidis) processed in parallel to clinical samples. This 96-well format assay allowed analysis of 30 swab samples per run and detection of the presence of MRSA with exquisite sensitivity compared to optimal culture-based techniques. The complete protocol may provide results in less than 6 h (while standard procedure needs 2 to 3 days), thus allowing prompt and cost-effective implementation of contact precautions.
Staphylococcus aureus is a major pathogen responsible for nosocomial and community-acquired infections. Since 1960, the emergence of multiresistant strains of S. aureus carrying resistance to methicillin (MRSA) and to most currently available antibiotics (4, 23) has dramatically narrowed the therapeutic arsenal to the exclusive use of glycopeptides (such as vancomycin and teicoplanin) as the mainstay of MRSA treatment. Unfortunately, vancomycin overuse has led to the emergence of MRSA strains with decreased susceptibilities to glycopeptides (22, 37).
The presence of MRSA in an institution is clearly paralleled by an increased number of bacteremias due to MRSA (41), which carry a threefold attributable cost and a threefold excess length of hospital stay when compared with methicillin-susceptible S. aureus (MSSA) bacteremia (1). These data, together with successful containment effort programs (6, 7, 9, 16, 18, 34, 36), prompt screening of high-risk patients even in a setting of high endemicity (43). Screening for MRSA is a key component of successful infection control strategies (11, 38, 43) aiming to identify hidden reservoirs of MRSA patients and appropriately apply isolation precautions (17, 40). To this end, infection control benefits from automated alerts upon admission in order to identify patients who have been previously colonized by MRSA (39). Early detection of MRSA carriers is crucial not only for infection control (11) but also for therapeutic decision with last-line antibiotics against MRSA, e.g., glycopeptides and oxazolidinones (49).
Rapid detection of MRSA by standard clinical microbiological procedures is tedious and time consuming, since it first requires identification of isolated S. aureus colonies within mixed flora samples before assessing their level of methicillin resistance. The development of selective media containing antibiotics and phenol red has provided better sensitivity than conventional agar-based cultures after 48 h of incubation, but at the expense of a longer turnaround time (10, 46, 51).
Direct or indirect particle agglutination assays using antibody-coated beads offer a rapid alternative to oxacillin susceptibility testing. For example, MRSA-Screen (Denka Seiken, Tokyo, Japan) provides sensitive and specific immunodetection of MRSA in a pure culture by using anti-PBP2′ antibodies, which is similar to standard oxacillin disk diffusion or oxacillin-salt agar screening (5, 24, 42). However, the specific immunodetection of MRSA based on PBP2′ cannot be performed in the presence of methicillin-resistant Staphylococcus epidermidis (MRSE), which is a frequent commensal contaminant of mixed flora samples (5). Indeed, the high level of sequence homology of the mecA gene present in S. aureus, S. epidermidis, and potentially other coagulase-negative staphylococci (CNS) species (52) precludes discrimination of methicillin-resistant strains of S. aureus from those of S. epidermidis (24).
Since the mecA gene, encoding the low-affinity penicillin-binding protein (PBP2′) (44), represents the “gold standard” for detecting methicillin resistance (32), several assays based on the direct detection of the mecA gene have been described, using chemiluminescent probes (53), amplification methods such as PCR (42), or cycling probe technology (12). A PCR immunoassay was reported by Towner et al., based on the amplification and immunodetection of mecA and femB amplicons, and performed after overnight culture enrichment of clinical samples. This technique outperforms conventional detection methods (48) by providing rapid immunodetection and avoiding the use of acrylamide gel. In another approach, PCR-amplified products were detected with low-density oligoarrays, providing detection of several targets during the same hybridization step (13). Other more elaborated multiplexed PCR, using different targets (coagulase and femA genes) (25, 50) or S. aureus toxins (47), yielded promising results with good specificity. Promising results were also obtained by using either triplex PCR assays based on the detection of S. aureus rRNA, mecA, and nuc (27, 29) or clfA genes (30) or by in situ hybridization performed on blood culture bottles (35).
The recent introduction of multiplexed real-time qPCR techniques (19, 26) combining accurate identification with limits of detection close to a single gene copy/sample provided a significant technological advantage for the rapid and large-scale identification of various microorganisms (8, 28, 31). This report describes a novel immuno-qPCR procedure allowing rapid detection of MRSA from mixed flora samples. The procedure consists in a direct one-step enrichment of MRSA present in either nasal or inguinal swabs, followed by DNA extraction of immunocaptured bacteria and their identification by a triplex qPCR. The specificity of MRSA molecular identification is based on the presence of the mecA gene and the presence of an S. aureus-specific femA signal that does not cross-react with other bacterial species, including S. epidermidis. This novel qPCR assay allows detection and identification of MRSA in less than 6 h after sample collection and may provide substantial benefits for infection control by allowing prompt and cost-effective implementation of contact precautions.
MATERIALS AND METHODS
Materials.
Biotinylated mouse monoclonal antibodies raised against S. aureus protein A (anti-spa, mouse immunoglobulin G1 clone spa-27) were obtained from Fluka (Sigma Chemie, Buchs, Switzerland), and streptavidin-coated paramagnetic beads were obtained from Merck (Basel, Switzerland). qPCR kits, primers, and TaqMan probes were purchased from Eurogentec (Seraing, Belgium).
Strains.
Reference strains were ATCC33591 (MRSA), ATCC25923 or NCTC8530 (MSSA), and ATCC12228 (methicillin-susceptible S. epidermidis [MSSE]). The reference MRSE and a panel of various bacterial species were clinical isolates identified using NCCLS procedures at the Clinical Microbiology Laboratory (University Hospitals of Geneva, Geneva, Switzerland). For these assays, overnight cultures were washed in saline and quantified by turbidimetry (ATB 1550; API bioMérieux). Titers were adjusted using 10-fold dilutions in saline and checked by plating on agar.
Specimen collection.
Samples consisting in nasal, inguinal, and wound swabs (Copanswabs; Copan Italia S.p.a, Brescia, Italy) were collected directly from patients admitted to University Hospitals of Geneva according to a previously defined infection control strategy (16, 39). Samples were simultaneously analyzed by molecular and conventional culture-based techniques. Swabs were suspended in 2 ml of colistin-salt broth (CS broth: brain-heart infusion with 10 μg of colistin/ml and 2.5% NaCl) and then divided equally and processed in parallel.
Identification of MRSA by standard microbiological procedure.
One milliliter of CS broth was incubated at 35°C for 24 h and inoculated on phenylethyl alcohol agar plates. Suspect colonies were identified as MRSA based on Pastorex agglutination (Bio-Rad, Reinach, Switzerland), positive reaction on DNase agar, and growth on Mueller-Hinton (MH) oxacillin agar (6 μg of oxacillin/ml, according to NCCLS [33]). The presence of MRSA was confirmed using the Vitek 2 identification and susceptibility testing cards for gram-positives (bioMérieux, Marcy l'Etoile, France).
Immunomagnetic enrichment.
The remaining 1 ml of CS broth was immediately processed by adding an optimized titer of biotinylated anti-spa antibody in the presence of 1% human serum albumin (HSA) (injectable grade; Swiss Red Cross, Bern, Switzerland). After a 30-min incubation at room temperature on a rotary shaker, the bacterial suspension was centrifuged for 10 min at 5,000 × g. The pellet was resuspended in 200 μl of phosphate-buffered saline (PBS) (Invitrogen; Basel, Switzerland) containing 1% human serum albumin (PBS-HSA) and supplemented with 20 μl of streptavidin-coated paramagnetic beads. After a 30-min incubation on a rotary shaker, the magnetic beads were rinsed twice in PBS-HSA on the magnetic holder. The efficiency of the immunomagnetic capture was assessed by plating diluted portions on MH plates and determining the number of CFU after 24 h of incubation.
Optimization of anti-spa antibody titer.
To optimize the antibody titer, 103 CFU of Cowan I (NCTC8530) was incubated with increasing antibody dilutions (1:166 to 1:5′400). The percentage of immunocaptured bacteria recovered from the original spiking was determined by viable counts on MH agar.
Efficiency of the recovery rate for various MRSA titers.
The recovery rate as a function of the number of spiked bacteria was evaluated by incubating a range of MRSA suspensions (ATCC 33591) in the presence of the optimized anti-spa titer in 1 ml of CS broth. The yield was determined by viable counts.
Immunocapture of MRSA from mixed cultures.
Various numbers of MRSA (ATCC 33591) were mixed with increasing titers of MRSE, yielding ratios ranging from 1:1 to 1:1,000. Immunocapture was evaluated by viable CFU counts performed on MH agar. Strains were visually discriminated by their pigmentation.
Bacterial lysis and DNA extraction.
Immunocaptured bacteria were suspended in 400 μl of chaotropic buffer (DNeasy kit; Qiagen) with 200 mg of glass beads (diameter, 100 to 200 μm). Bacteria were lysed at 4°C in a bead-beater (Mixer Mill; Qiagen) using two homogenization cycles of 45 s each at a frequency of 30 Hertz. The liquid phase was cleared from beads and debris by a 10-min centrifugation at 5.000 × g and then transferred into clean tubes containing 200 μl of ethanol. The nucleic acids were purified according to the manufacturer's instructions (Qiagen), eluted in water, dried in an evaporator, and finally resuspended in 20 μl of water.
DNA extraction from reference strains.
Genomic DNA was extracted after a 10-min treatment at 37°C in TE containing 100 μg of lysostaphin (Ambicin; Applied Microbiology, Tarrytown, N.Y.)/ml. DNA concentration and purity were assessed by spectrophotometry (45) using an Uvikon 942 (Kontron; Basel, Switzerland).
Oligonucleotide design and sequences.
Sequences of primers and TaqMan probes are listed in Table 1. The design was performed using the software Primer Express version 1.0 (PE Biosystems, Foster City, Calif.). Since the sequences of both S. aureus and S. epidermidis mecA genes showed 100% homology, primers and TaqMan probe were determined based on the S. aureus gene (GenBank accession no. X52593). On the opposite, whereas femA nucleotide sequences are phylogenetically conserved among the staphylococci (13), S. aureus femA and S. epidermidis femA displayed only 78% homology as determined by LALVIEW (http://www.expasy.ch/). Primers and TaqMan probes were selected in regions displaying low homology with at least four mismatches between both femA oligonucleotide sequences (2, 3). Selected primers and probes were checked against GenBank to exclude potential cross-reacting sequences. Sequence identity between S. aureus femA and the Streptococcus milleri gene for millericin B (GenBank accession no. AF243359) was detected for both primer sequences as well as a homology of 25 of 29 nucleotides in the probe. However, the length of the generated amplicon (703 bp) was found to be excessive for reliable qPCR detection (not shown).
TABLE 1.
List and characteristics of oligonucleotides used in the triplex qPCR assay
| Gene and primer or probe namea | Sequence (5′→3′) | Length | 5′ dyeb | GenBank accession no. (reference) |
|---|---|---|---|---|
| mecA | X52593 (44) | |||
| F mecA | CATTGATCGCAACGTTCAATTT | 22 | ||
| R mecA | TGGTCTTTCTGCATTCCTGGA | 21 | ||
| P mecA | TGGAAGTTAGATTGGGATCATAGCGTCAT | 29 | JOE | |
| femA-SA | X17688 (3) | |||
| F femA-SA | TGCCTTTACAGATAGCATGCCA | 22 | ||
| R femA-SA | AGTAAGTAAGCAAGCTGCAATGACC | 25 | ||
| P femA-SA | TCATTTCACGCAAACTGTTGGCCACTATG | 29 | FAM | |
| femA-SE | U23713 (2) | |||
| F femA-SE | CAACTCGATGCAAATCAGCAA | 21 | ||
| R femA-SE | GAACCGCATAGCTCCCTGC | 19 | ||
| P femA-SE | TACTACGCTGGTGGAACTTCAAATCGTTATCG | 32 | TET |
femA-SA, S. aureus femA; femA-SE, S. epidermidis femA.
All probes are quenched by TAMRA bound to the 3′ end.
Nucleic acid detection by qPCR.
For robustness issues, each analysis was performed in triplicate. Nucleic acids from reference MRSA, MSSA, MRSE, and MSSE strains (100 pg of genomic DNA in each well) were simultaneously analyzed in each run and used as standards to adjust threshold values (Ct). Amplification procedure on the SDS 7700 (PE Biosystems) was the following: t1, 2 min at 50°C; t2, 10 min at 95°C; t3, 15 s at 95°C; t4, 1 min at 60°C (t3 and t4, repeated 50 times). The final volume of the PCR mixture was 20 μl and contained all primers and TaqMan probes at 100 nM concentrations except the mecA probe, which was adjusted to 75 nM, following assay optimization (data not shown). The cycling procedure was immediately started upon addition of 6 μl of sample. The specificity of qPCR identification was assessed using the following pathogens (number of different strains): Escherichia coli (10), Campylobacter fetus (4), Proteus vulgaris (4), Enterococcus faecalis (11), Enterococcus faecium (4), Enterobacter cloacae (3), Klebsiella pneumoniae (3), Streptococcus pneumoniae (4), Streptococcus alpha-haemolyticus (4), S. agalactiae (2), S. milleri (3), Pseudomonas aeruginosa (10), Stenotrophomonas maltophilia (1), Lactococcus cremoris (1), Neisseria sp. (1), and Staphylococcus haemolyticus (10); also Candida glabrata (2) and Candida albicans (2). None of these different species yielded any false-positive qPCR signal.
Analysis of multiplex qPCR signals.
After fluorescence background subtraction, we calibrated each run using the signals of the reference strains MRSA and MRSE. Detection thresholds were adjusted so that the mecA signal matched the corresponding femA signal for each reference strain. MRSA was considered present only when average Ct values (triplicates) met the following conditions: (i) average Ct for mecA of <50; (ii) average Ct for S. aureus femA of <50; and (iii) Ct for mecA that is less than the Ct for S. epidermidis femA.
RESULTS
Optimization of S. aureus immunocapture.
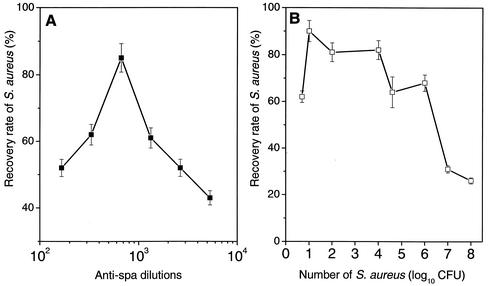
The enrichment procedure for S. aureus was based on the ubiquitous and specific presence of protein A on S. aureus bacterial cells (either MRSA or MSSA). To optimize the conditions for S. aureus recovery, we incubated bacterial suspensions with various anti-spa antibody dilutions, ranging from 1:166 to 1:5,400. An optimal recovery of 85% from a suspension of 103 Cowan I CFU/ml was obtained with a titer of 1:666, equivalent to 1.5 μl of anti-spa antibody per milliliter of CS broth (Fig. 1A). Higher antibody concentrations led to lower bacterial recovery, presumably due to saturation of streptavidin-coated beads. Using this optimal antibody titer, we assessed the recovery rates from S. aureus suspensions over >7 orders of magnitude. Figure 1B shows that the highest recovery rates (>60%) were consistently obtained from bacterial suspensions of 0.8 to 6 log10 CFU/ml. This good recovery of diluted bacterial suspensions is a prerequisite for sensitive molecular detection and molecular identification of MRSA.
FIG. 1.
Effect of antibody concentration on S. aureus recovery rate. Cowan I strain (NCTC8530; 103 CFU) was used to evaluate the optimal concentration of anti-spa antibodies required for the enrichment step. (A) Recovery was determined by CFU counts of immunocaptured colonies. The curve showed maximal recovery at an antibody dilution of 1:666. (B). Using this optimized anti-spa dilution, recovery was assessed across >7 orders of magnitude in inoculum size. Average values ± standard errors of the means for four experiments performed in duplicate are given.
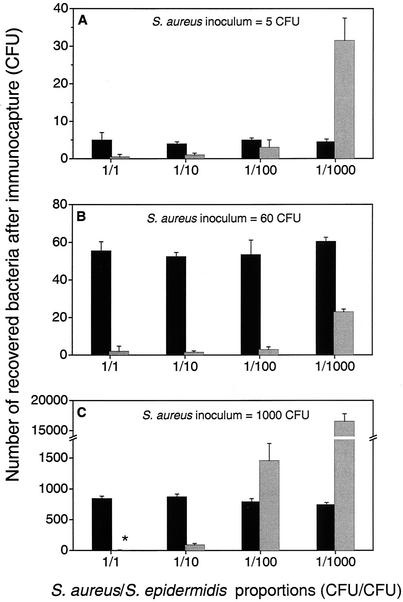
Optimized recovery conditions in mixed cultures of S. aureus and S. epidermidis.
To validate the immunocapture procedure, three different titers of MRSA (5, 60, and 1,000 CFU/ml) were incubated with increasing amounts of MRSE (Fig. 2A, B, and C). The recovery of MRSA was excellent and not significantly affected by adding MRSE in ratios ranging from 1:1 to 1:1,000. Constant recovery rates (>80%) were recorded for MRSA concentrations ranging from 5 to 1,000 CFU/ml, even in the presence of a 1,000-fold excess amount of MRSE. Equivalent data were recorded with two Pastorex-negative MRSA isolates (not shown). This suggests that the minimal amount of protein A expressed by Pastorex-negative strains can be reliably immunocaptured.
FIG. 2.
Immunocapture of MRSA from mixed cultures. 5 (A), 60 (B), or 1,000 (C) CFU of MRSA (ATCC 33591) was mixed with increasing titers of MRSE, yielding ratios ranging from 1:1 to 1:1,000 for S. aureus (black bars) versus S. epidermidis (grey bars). Immunocapture was evaluated by viable CFU counts performed on MH agar. Means ± ranges for two experiments performed in duplicate are shown. ∗, <10 CFU of MRSE.
Multiplex PCR assay.
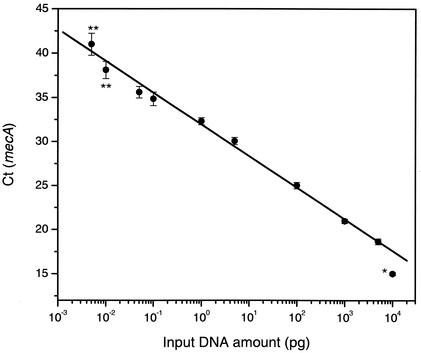
The limits of detection as well as the linearity of the qPCR assay were calibrated using increasing amounts (2 fg to 10 ng) of purified genomic DNA from MRSA (ATCC 33591). The Ct values for mecA (Fig. 3) and S. aureus femA (not shown) were linear across 6 orders of magnitude of DNA input. The upper limit of linearity was >5 ng of template DNA, equivalent to 106 genome copies. The lower limit of MRSA DNA detection was reached with 5 fg of genomic DNA, which is nearly equivalent to the genome of 1 to 2 S. aureus bacterial cells (3.5 fg/cell). As expected, the qPCR signals were no longer consistently detected when using less than 10 fg of genomic DNA. On the other hand, the mecA and S. aureus femA signals detected from an input genomic DNA amount of 100 pg (100 pg of genomic DNA corresponds to >4 log10 CFU) yielded similar Ct values without generating a nonspecific S. epidermidis femA signal. The specificity of the femA signals was also verified with other reference strains (Table 2).
FIG. 3.
Linearity and limits of detection of the qPCR assay. The linear response of the qPCR mecA assay as a function of input genomic DNA (2 fg to 10 ng) purified from strain ATCC33591 is shown. Correlation coefficient, >0.99; slope, −3.59. Values are means ± standard errors of the means of 4 to 16 determinations. ∗, value excluded from linear regression. ∗∗, amounts of input DNA leading to irregular signal detection.
TABLE 2.
qPCR results for reference strains
| Strain |
Ct value fora:
|
||
|---|---|---|---|
| femA-SA | femA-SE | mecA | |
| MRSA (ATCC33591) | 27.5 | NAb | 27.5 |
| MSSA (ATCC25923) | 28.5 | NA | NA |
| MRSEc | NA | 28.3 | 28.3 |
| MSSE (ATCC12228) | NA | 27.7 | NA |
| S. haemolyticusc | NA | NA | 25.1 |
Average Ct value for triplicate determinations with 100 pg of genomic DNA. femA-SA, S. aureus femA; femA-SE, S. epidermidis femA.
NA, not assessed; no signals detected within 50 cycles.
Clinical methicillin-resistant isolate.
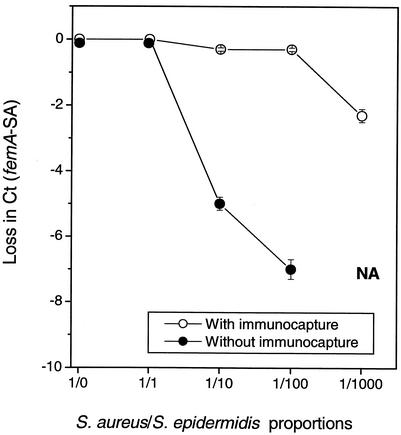
Impact of the immunocapture procedure on the qPCR assay.
When 103 CFU of MRSA was incubated with MRSE at ratios ranging from 1:1 to 1:1,000, detection of MRSA after immunocapture remained optimal even in the presence of a 100-fold excess amount of MRSE (Fig. 4). Equivalent MRSA detection efficacy was achieved using as few as 5 CFU of MRSA. Average Ct values for S. aureus femA and mecA were then constantly observed around 39.5 ± 0.4. On the opposite, the immunocapture of a 100-fold excess amount of MRSE led to S. epidermidis femA signals >42. Such levels of residual MRSE contamination do not affect appropriate MRSA identification. As suggested by Fig. 2B, the qPCR assay identified correctly the presence of 60 CFU of MRSA even when it was incubated with a 1,000-fold excess amount of MRSE.
FIG. 4.
Effect of the immunocapture procedure on the qPCR assay. S. aureus (ATCC 33591; 103 CFU) was mixed with various S. epidermidis titers (MRSE) and analyzed by qPCR following (○) or not following (•) immunocapture enrichment. MRSA in the presence of >100-fold-excess amounts of MRSE was not detected (NA). Values are means ± standard errors of the means for three experiments performed in triplicate.
When the immunocapture procedure was omitted, the detection of MRSA by the S. aureus femA (Fig. 4) or mecA signals (not shown) was drastically affected by the presence of increasing amounts of MRSE. In the presence of a 1,000-fold excess amount of MRSE, nonimmunocaptured MRSA in suspension failed to be detected by the qPCR assay. Contamination of MRSA suspensions by other bacterial species, such as E. coli or Pseudomonas aeruginosa, in excess amounts yielded similar results (data not shown).
Evaluation of the qPCR assay with consecutive clinical swab samples.
To test the specificity of the qPCR assay, 100 pg of genomic DNA from reference strains was analyzed (Table 2). Manual adjustment of detection thresholds led to an improved matching of species-specific femA signals with their corresponding mecA signal. The mecA signal was specifically detected in MRSA, MRSE, and a methicillin-resistant S. haemolyticus clinical isolate. Furthermore, femA signals were strictly species specific.
Table 3 shows the comparative results of immuno-qPCR and an optimal bacteriological procedure applied to 48 clinical swab samples. All the culture-positive samples were also detected by the immuno-qPCR assay (n = 23). Among the samples found to be MRSA negative by microbiological criteria (n = 25), 16 were also scored as negative by immuno-qPCR. In contrast, a subgroup of nine culture-negative samples was scored as positive by immuno-qPCR. Altogether, these data yielded sensitivity and negative predictive values of 100%. In contrast, the specificity and positive predictive values were 64 and 72%, respectively. A possible reason for the high proportion of false-positive cases might be the recent use of topical antimicrobial agents in those previously identified MRSA carriers. This suggests that the immuno-qPCR procedure detected the presence of nonviable MRSA and yielded misleading results in this subgroup. Furthermore, all these recently decontaminated MRSA carriers relapsed shortly (<2 weeks) after the comparative analysis.
TABLE 3.
Comparison between culture-based and immuno-qPCR methods in the detection of MRSA in clinical swab samplesa
| Method | No. true positive | No. false negative | No. false positive | No. true negative | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|---|
| Cultureb | 23 | 0 | 0 | 25 | 100 | 100 |
| qPCR | 23 | 0 | 9 | 16 | 100 | 64 |
Forty-eight clinical swab samples were collected from different body sites: nares (16), inguinal (17), pooled swabs (4), or wound (11). Sensitivity (23 of 23), 100%; specificity (16 of 25), 64%.
Method used as the reference technique.
Altogether, the immuno-qPCR assay yields performance equivalent to that of optimal culture methods but has a dramatic impact on the delay for MRSA identification and implementation of infection control measures.
DISCUSSION
The identification of MRSA in biological samples is a time-consuming process relying on phenotypic or molecular analysis of isolated bacteria. We describe here a novel molecular method that does not require any bacterial culture, the time-limiting step. The major advantage of this approach, compared to other published techniques, is same-day MRSA identification directly from swab samples or other potentially polymicrobial samples. This two-step molecular assay involves the immunocapture of S. aureus, followed by MRSA identification using a multiplex qPCR. This assay is based on the highly conserved mecA sequence within all methicillin-resistant strains and species of staphylococci, thus warranting the detection of any organism carrying this resistance determinant (52). To strictly discriminate MRSA from any other methicillin-resistant staphylococcal species, the qPCR assay unambiguously detects a species-specific femA region. The femA target was selected because of the following: (i) its presence in all S. aureus and S. epidermidis strains, (ii) the identification of species-specific oligonucleotides, and (iii) the successful development of a triplex qPCR assay. Other conserved sequences, such as nuc for S. aureus and femB for S. epidermidis, might represent alternate targets. Experiments using samples spiked with known amounts of S. aureus and S. epidermidis not only accurately discriminated either species but also maintained the lower limit of detection to one or two genome copies.
A critical innovative step of this method is the enrichment procedure that specifically immunocaptures virtually all strains of S. aureus. The target of our antibody, the protein A, is routinely used to confirm S. aureus identification because of its high prevalence and specificity. Control experiments verified the absence of significant immunocapture by a wide range of gram-positive and gram-negative species (data not shown). Recovery of MRSA was marginally influenced by the presence of S. epidermidis even at a 1,000-fold excess amount. This assumption was verified even for very low titers of S. aureus (<10 CFU) or for two exceptional Pastorex-negative MRSA clinical isolates.
Several groups have already reported on the use of multiplexed PCR assays on pure cultures (25, 47, 48). Two recently described procedures (27, 29) detected the presence of MRSA from positive blood culture bottles, with a limit of detection around 105 CFU/ml (29). The implementation of an immunocapture step allowed the use of qPCR directly on mixed flora samples.
The clinical performance of this immuno-qPCR assay was evaluated by testing 48 consecutive clinical swab samples. All culture-positive MRSA samples were successfully detected by immuno-qPCR. Among 25 culture-negative samples, a surprisingly high number of false-positive results were recorded (n = 9). A retrospective analysis revealed that these nine cases were previously known as MRSA carriers and relapsed, as evidenced by culture. However, in this high-risk population sample, 50% of the 16 cases identified as MRSA negative by both techniques became MRSA positive during their hospital stay. Thus, this low specificity does not compromise the utility of the assay, since it mostly reflects situations of transient decolonization (14, 15, 20, 21).
Larger numbers of samples are warranted to assess the sensitivity and specificity of the immuno-qPCR assay, especially in low-risk patients. A large-scale prospective comparative study was recently initiated in our institution to evaluate the impact of single-day MRSA identification on patient management and infection control decisions.
Acknowledgments
This work was supported by grants from the Swiss National Science Foundation, no. 631-057950.99 (J.S.), 32-63710.00 (P.V.), and 31-55344.98 (D.L.).
We thank Rosemary Sudan for comments on the manuscript.
REFERENCES
- 1.Abramson, M. A., and D. J. Sexton. 1999. Nosocomial methicillin-resistant and methicillin-susceptible Staphylococcus aureus primary bacteremia: at what costs? Infect. Control Hosp. Epidemiol. 20:408-411. [DOI] [PubMed] [Google Scholar]
- 2.Alborn, W. E., Jr., J. Hoskins, S. Unal, J. E. Flokowitsch, C. A. Hayes, J. E. Dotzlaf, W. K. Yeh, and P. L. Skatrud. 1996. Cloning and characterization of femA and femB from Staphylococcus epidermidis. Gene 180:177-181. [DOI] [PubMed] [Google Scholar]
- 3.Berger-Bachi, B., L. Barberis-Maino, A. Strassle, and F. H. Kayser. 1989. FemA, a host-mediated factor essential for methicillin resistance in Staphylococcus aureus: molecular cloning and characterization. Mol. Gen. Genet. 219:263-269. [DOI] [PubMed] [Google Scholar]
- 4.Boyce, J. M. 2001. MRSA patients: proven methods to treat colonization and infection. J. Hosp. Infect. 48(Suppl. A):S9-S14. [DOI] [PubMed] [Google Scholar]
- 5.Cavassini, M., A. Wenger, K. Jaton, D. S. Blanc, and J. Bille. 1999. Evaluation of MRSA-Screen, a simple anti-PBP 2a slide latex agglutination kit, for rapid detection of methicillin resistance in Staphylococcus aureus. J. Clin. Microbiol. 37:1591-1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chaix, C., I. Durand-Zaleski, C. Alberti, and C. Brun-Buisson. 1999. Control of endemic methicillin-resistant Staphylococcus aureus: a cost-benefit analysis in an intensive care unit. JAMA 282:1745-1751. [DOI] [PubMed] [Google Scholar]
- 7.Cohen, S. H., M. M. Morita, and M. Bradford. 1991. A seven-year experience with methicillin-resistant Staphylococcus aureus. Am. J. Med. 91:233S-237S. [DOI] [PubMed] [Google Scholar]
- 8.Corless, C. E., M. Guiver, R. Borrow, V. Edwards-Jones, A. J. Fox, and E. B. Kaczmarski. 2001. Simultaneous detection of Neisseria meningitidis, Haemophilus influenzae, and Streptococcus pneumoniae in suspected cases of meningitis and septicemia using real-time PCR. J. Clin. Microbiol. 39:1553-1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cosseron-Zerbib, M., A. M. Roque Afonso, T. Naas, P. Durand, L. Meyer, Y. Costa, N. el Helali, G. Huault, and P. Nordmann. 1998. A control programme for MRSA (methicillin-resistant Staphylococcus aureus) containment in a paediatric intensive care unit: evaluation and impact on infections caused by other micro-organisms. J. Hosp. Infect. 40:225-235. [DOI] [PubMed] [Google Scholar]
- 10.Davies, S., P. M. Zadik, C. M. Mason, and S. J. Whittaker. 2000. Methicillin-resistant Staphylococcus aureus: evaluation of five selective media. Br. J. Biomed. Sci. 57:269-272. [PubMed] [Google Scholar]
- 11.Farr, B. M., and W. R. Jarvis. 2002. Would active surveillance cultures help control healthcare-related methicillin-resistant Staphylococcus aureus infections? Infect. Control Hosp. Epidemiol. 23:65-68. [DOI] [PubMed] [Google Scholar]
- 12.Fong, W. K., Z. Modrusan, J. P. McNevin, J. Marostenmaki, B. Zin, and F. Bekkaoui. 2000. Rapid solid-phase immunoassay for detection of methicillin-resistant Staphylococcus aureus using cycling probe technology. J. Clin. Microbiol. 38:2525-2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hamels, S., J. L. Gala, S. Dufour, P. Vannuffel, N. Zammatteo, and J. Remacle. 2001. Consensus PCR and microarray for diagnosis of the genus Staphylococcus, species, and methicillin resistance. BioTechniques 31:1364-1366. [DOI] [PubMed] [Google Scholar]
- 14.Harbarth, S., S. Dharan, N. Liassine, P. Herrault, R. Auckenthaler, and D. Pittet. 1999. Randomized, placebo-controlled, double-blind trial to evaluate the efficacy of mupirocin for eradicating carriage of methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 43:1412-1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harbarth, S., N. Liassine, S. Dharan, P. Herrault, R. Auckenthaler, and D. Pittet. 2000. Risk factors for persistent carriage of methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 31:1380-1385. [DOI] [PubMed] [Google Scholar]
- 16.Harbarth, S., Y. Martin, P. Rohner, N. Henry, R. Auckenthaler, and D. Pittet. 2000. Effect of delayed infection control measures on a hospital outbreak of methicillin-resistant Staphylococcus aureus. J. Hosp. Infect. 46:43-49. [DOI] [PubMed] [Google Scholar]
- 17.Harbarth, S., and D. Pittet. 1998. MRSA—a European currency of infection control. Q. J. Med. 91:519-521. [DOI] [PubMed] [Google Scholar]
- 18.Herwaldt, L. A. 1999. Control of methicillin-resistant Staphylococcus aureus in the hospital setting. Am. J. Med. 106:11S-18S. [DOI] [PubMed] [Google Scholar]
- 19.Higuchi, R., G. Dollinger, P. S. Walsh, and R. Griffith. 1992. Simultaneous amplification and detection of specific DNA sequences. Bio/Technology (New York) 10:413-417. [DOI] [PubMed] [Google Scholar]
- 20.Hill, R. L., and M. W. Casewell. 1990. Nasal carriage of MRSA: the role of mupirocin and outlook for resistance. Drugs Exp. Clin. Res. 16:397-402. [PubMed] [Google Scholar]
- 21.Hill, R. L., G. J. Duckworth, and M. W. Casewell. 1988. Elimination of nasal carriage of methicillin-resistant Staphylococcus aureus with mupirocin during a hospital outbreak. J. Antimicrob. Chemother. 22:377-384. [DOI] [PubMed] [Google Scholar]
- 22.Hiramatsu, K. 1998. The emergence of Staphylococcus aureus with reduced susceptibility to vancomycin in Japan. Am. J. Med. 104:7S-10S. [DOI] [PubMed] [Google Scholar]
- 23.Hryniewicz, W. 1999. Epidemiology of MRSA. Infection 27(Suppl. 2):S13-S16. [DOI] [PubMed] [Google Scholar]
- 24.Hussain, Z., L. Stoakes, S. Garrow, S. Longo, V. Fitzgerald, and R. Lannigan. 2000. Rapid detection of mecA-positive and mecA-negative coagulase-negative staphylococci by an anti-penicillin binding protein 2a slide latex agglutination test. J. Clin. Microbiol. 38:2051-2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kearns, A. M., P. R. Seiders, J. Wheeler, R. Freeman, and M. Steward. 1999. Rapid detection of methicillin-resistant staphylococci by multiplex PCR. J. Hosp. Infect. 43:33-37. [DOI] [PubMed] [Google Scholar]
- 26.Lee, L. G., K. J. Livak, B. Mullah, R. J. Graham, R. S. Vinayak, and T. M. Woudenberg. 1999. Seven-color, homogeneous detection of six PCR products. BioTechniques 27:342-349. [DOI] [PubMed] [Google Scholar]
- 27.Louie, L., J. Goodfellow, P. Mathieu, A. Glatt, M. Louie, and A. E. Simor. 2002. Rapid detection of methicillin-resistant staphylococci from blood culture bottles by using a multiplex PCR assay. J. Clin. Microbiol. 40:2786-2790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mackay, I. M., K. E. Arden, and A. Nitsche. 2002. Real-time PCR in virology. Nucleic Acids Res. 30:1292-1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maes, N., J. Magdalena, S. Rottiers, Y. De Gheldre, and M. J. Struelens. 2002. Evaluation of a triplex PCR assay to discriminate Staphylococcus aureus from coagulase-negative staphylococci and determine methicillin resistance from blood Cultures. J. Clin. Microbiol. 40:1514-1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mason, W. J., J. S. Blevins, K. Beenken, N. Wibowo, N. Ojha, and M. S. Smeltzer. 2001. Multiplex PCR protocol for the diagnosis of staphylococcal infection. J. Clin. Microbiol. 39:3332-3338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meng, Q., C. Wong, A. Rangachari, S. Tamatsukuri, M. Sasaki, E. Fiss, L. Cheng, T. Ramankutty, D. Clarke, H. Yawata, Y. Sakakura, T. Hirose, and C. Impraim. 2001. Automated multiplex assay system for simultaneous detection of hepatitis B virus DNA, hepatitis C virus RNA, and human immunodeficiency virus type RNA. J. Clin. Microbiol. 39:2937-2945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Murakami, K., W. Minamide, K. Wada, E. Nakamura, H. Teraoka, and S. Watanabe. 1991. Identification of methicillin-resistant strains of staphylococci by polymerase chain reaction. J. Clin. Microbiol. 29:2240-2244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.National Committee for Clinical Laboratory Standards. 2002. Performance standards for antimicrobial susceptibility testing. NCCLS approved standard M100-S11.National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 34.Nettleman, M. D., A. Trilla, M. Fredrickson, and M. Pfaller. 1991. Assigning responsibility: using feedback to achieve sustained control of methicillin-resistant Staphylococcus aureus. Am. J. Med. 91:228S-232S. [DOI] [PubMed] [Google Scholar]
- 35.Oliveira, K., G. W. Procop, D. Wilson, J. Coull, and H. Stender. 2002. Rapid identification of Staphylococcus aureus directly from blood cultures by fluorescence in situ hybridization with peptide nucleic acid probes. J. Clin. Microbiol. 40:247-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Papia, G., M. Louie, A. Tralla, C. Johnson, V. Collins, and A. E. Simor. 1999. Screening high-risk patients for methicillin-resistant Staphylococcus aureus on admission to the hospital: is it cost effective? Infect. Control Hosp. Epidemiol. 20:473-477. [DOI] [PubMed] [Google Scholar]
- 37.Park, Y. J., M. Kim, E. J. Oh, S. O. Lee, B. K. Kim, and S. M. Kim. 2000. Screening method for detecting staphylococci with reduced susceptibility to teicoplanin. J. Microbiol. Methods 40:193-198. [DOI] [PubMed] [Google Scholar]
- 38.Pittet, D. 2002. Promotion of hand hygiene: magic, hype, or scientific challenge? Infect. Control Hosp. Epidemiol. 23:118-119. [DOI] [PubMed] [Google Scholar]
- 39.Pittet, D., E. Safran, S. Harbarth, F. Borst, P. Copin, P. Rohner, J. R. Scherrer, and R. Auckenthaler. 1996. Automatic alerts for methicillin-resistant Staphylococcus aureus surveillance and control: role of a hospital information system. Infect. Control Hosp. Epidemiol. 17:496-502. [PubMed] [Google Scholar]
- 40.Pittet, D., and F. A. Waldvogel. 1997. To control or not control colonization with MRSA. That's the question! Q. J. Med. 90:239-241. [DOI] [PubMed] [Google Scholar]
- 41.Pujol, M., C. Pena, R. Pallares, J. Ariza, J. Ayats, M. A. Dominguez, and F. Gudiol. 1996. Nosocomial Staphylococcus aureus bacteremia among nasal carriers of methicillin-resistant and methicillin-susceptible strains. Am. J. Med. 100:509-516. [DOI] [PubMed] [Google Scholar]
- 42.Rohrer, S., M. Tschierske, R. Zbinden, and B. Berger-Bachi. 2001. Improved methods for detection of methicillin-resistant Staphylococcus aureus. Eur. J. Clin. Microbiol. Infect. Dis. 20:267-270. [DOI] [PubMed] [Google Scholar]
- 43.Rubinovitch, B., and D. Pittet. 2001. Screening for methicillin-resistant Staphylococcus aureus in the endemic hospital: what have we learned? J. Hosp. Infect. 47:9-18. [DOI] [PubMed] [Google Scholar]
- 44.Ryffel, C., F. H. Kayser, and B. Berger-Bachi. 1992. Correlation between regulation of mecA transcription and expression of methicillin resistance in staphylococci. Antimicrob. Agents Chemother. 36:25-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sambrook, J., E. F. Fritsch, and T. Maniatis. 1989. Molecular cloning: a laboratory manual, p. E3-E7. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, N.Y.
- 46.Sautter, R. L., W. J. Brown, and L. H. Mattman. 1988. The use of a selective staphylococcal broth v direct plating for the recovery of Staphylococcus aureus. Infect. Control Hosp. Epidemiol. 9:204-205. [DOI] [PubMed] [Google Scholar]
- 47.Schmitz, F. J., M. Steiert, B. Hofmann, J. Verhoef, U. Hadding, H. P. Heinz, and K. Kohrer. 1998. Development of a multiplex-PCR for direct detection of the genes for enterotoxin B and C, and toxic shock syndrome toxin-1 in Staphylococcus aureus isolates. J. Med. Microbiol. 47:335-340. [DOI] [PubMed] [Google Scholar]
- 48.Towner, K. J., D. C. Talbot, R. Curran, C. A. Webster, and H. Humphreys. 1998. Development and evaluation of a PCR-based immunoassay for the rapid detection of methicillin-resistant Staphylococcus aureus. J. Med. Microbiol. 47:607-613. [DOI] [PubMed] [Google Scholar]
- 49.Tsiodras, S., H. S. Gold, G. Sakoulas, G. M. Eliopoulos, C. Wennersten, L. Venkataraman, R. C. Moellering, and M. J. Ferraro. 2001. Linezolid resistance in a clinical isolate of Staphylococcus aureus. Lancet 358:207-208. [DOI] [PubMed] [Google Scholar]
- 50.Vannuffel, P., P. F. Laterre, M. Bouyer, J. Gigi, B. Vandercam, M. Reynaert, and J. L. Gala. 1998. Rapid and specific molecular identification of methicillin-resistant Staphylococcus aureus in endotracheal aspirates from mechanically ventilated patients. J. Clin. Microbiol. 36:2366-2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wertheim, H., H. A. Verbrugh, C. van Pelt, P. de Man, A. Van Belkum, and M. C. Vos. 2001. Improved detection of methicillin-resistant Staphylococcus aureus using phenyl mannitol broth containing aztreonam and ceftizoxime. J. Clin. Microbiol. 39:2660-2662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wielders, C. L., M. R. Vriens, S. Brisse, L. A. Graaf-Miltenburg, A. Troelstra, A. Fleer, F. J. Schmitz, J. Verhoef, and A. C. Fluit. 2001. Evidence for in-vivo transfer of mecA DNA between strains of Staphylococcus aureus. Lancet 357:1674-1675. [DOI] [PubMed] [Google Scholar]
- 53.Youmans, G. R., T. E. Davis, and D. D. Fuller. 1993. Use of chemiluminescent DNA probes in the rapid detection of oxacillin resistance in clinically isolated strains of Staphylococcus aureus. Diagn. Microbiol. Infect. Dis. 16:99-104. [DOI] [PubMed] [Google Scholar]