Abstract
Thymidine-dependent small-colony variants (SCV) of Staphylococcus aureus exhibited unusual colony morphology with “fried-egg” or pinpoint white colonies on agar plates and pleomorphic cocci as determined by Gram staining. Electron microscopy revealed enlarged cocci with incomplete or multiple cross walls consistent with impaired cell separation. Fried-egg SCV phenotypes could be reversed by thymidine supplementation.
Staphylococcus aureus is a major human pathogen causing significant morbidity and mortality in both community- and hospital-acquired infections (5). Today, the prevalence of methicillin-resistant S. aureus (MRSA) is steadily increasing, and treatment of staphylococcal infections has become more difficult due to the emergence of multidrug-resistant strains (5, 8). Infections caused by S. aureus range from mild skin and wound infections to acute life-threatening diseases such as endocarditis, pneumonia, arthritis, and osteomyelitis. However, S. aureus can also cause a chronic type of disease with recurrent infections, as demonstrated for osteomyelitis (7, 10) and cystic fibrosis (CF) (3; Kahl et al., submitted). These infections have been associated with the isolation of subpopulations of S. aureus with the small-colony variant (SCV) phenotype. In contrast to normal S. aureus with typical colony size, pigmentation, and hemolysis on Columbia agar, SCVs are often altered in their electron transport activity (4) or in their ability to synthesize thymidine 1 (2). Thus, SCVs grow as small, nonpigmented, nonhemolytic colonies which produce greatly reduced amounts of α-hemolysin, thereby persisting intracellularly in in vitro systems (1).
Recently, we demonstrated high prevalence and long-term persistence of normal and SCV S. aureus in the airways of CF patients during a 6-year prospective study (B. C. Kahl, A. Duebbers, G. Lubritz, J. Haeberle, H. G. Koch, B. Ritzerfeld, M. Reilly, E. Harms, R. A. Proctor, M. Herrmann, and G. Peters, submitted for publication). In many patients, normal and SCV S. aureus isolated at the same time were isogenic, as determined by pulsed-field gel electrophoresis (3; Kahl et al., submitted). Most SCVs (148 of 212; 69.8%) were thymidine dependent, and nearly all of them emerged due to long-term treatment with trimethoprim-sulfamethoxazole (SXT), thus being SXT resistant, as was also described by Gilligan et al. (2). Importantly, treatment with SXT often represents a last choice in patients with infections caused by MRSA because more than 50% of multidrug resistant MRSA strains are still SXT susceptible (8). However, during long-term treatment with SXT, chances for selection or induction of thymidine-dependent SCVs arise. Accordingly, reports on thymidine-dependent MRSA SCVs causing fatal infections are increasing (9). However, due to their unusual morphology, the correct identification of these variants is extremely difficult, and therefore SCVs are easily missed or misdiagnosed as normal flora in the routine laboratory. This report illustrates this unusual morphology and correlates it with the underlying ultrastructural changes present in thymidine-dependent SCVs.
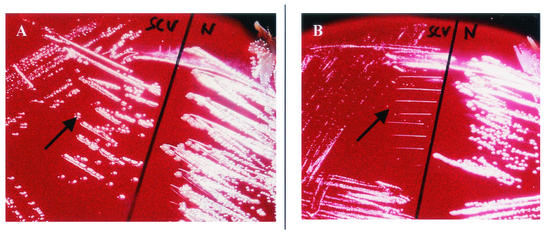
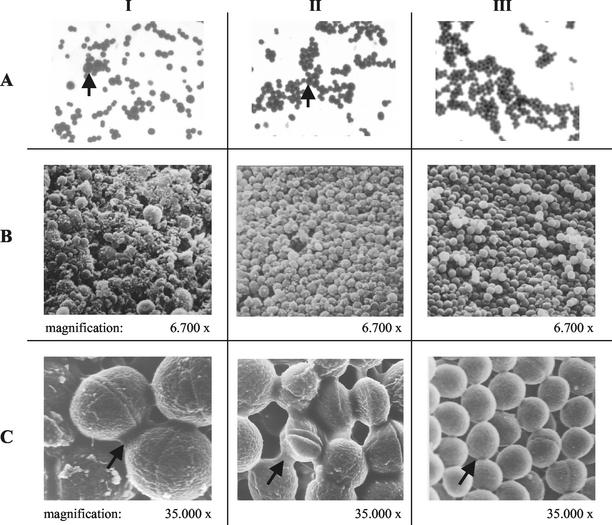
In contrast to the growth of normal S. aureus on Columbia sheep blood (Oxoid, Wesel, Germany) agar (Becton Dickinson, Heidelberg, Germany) (Fig. 1, N), thymidine-dependent SCVs grew either as “fried-egg” colonies with translucent edges surrounding a smaller, elevated pigmented center (Fig. 1A, SCV) or as pinpoint colonies approximately 10 times smaller (Fig. 1B, SCV) than normal S. aureus. In contrast to homogenous cocci of the isogenic normal S. aureus (Fig. 2A, panel III), Gram staining of thymidine-dependent SCVs revealed pleomorphic cocci, including colonies of sizes resembling fungi (Fig. 2A, panels I and II). Since growth on Columbia blood agar and Gram staining morphology were highly unusual for S. aureus, extended identification procedures such as PCR of the highly conserved nuc gene in addition to standard procedures were necessary (3) to confirm species identification.
FIG. 1.
Growth of thymidine-dependent SCVs with fried-egg appearance and with pinpoint colonies on Columbia blood agar. (A) Fried-egg thymidine-dependent SCVs (left, arrow) in comparison to the isogenic normal S. aureus (right, N). (B) Pinpoint SCVs (left, arrow) in comparison to the isogenic normal S. aureus (right, N). All strains were grown overnight at 37°C.
FIG. 2.
Gram staining and SEM of fried-egg SCVs (panels I), pinpoint SCVs (panels II), and normal S. aureus (panels III). (A) Gram staining. Arrows indicate large cocci. (B and C) Low- and high-magnification SEM, respectively. Arrows indicate the enhanced intercellular substance present in SCVs compared to normal S. aureus.
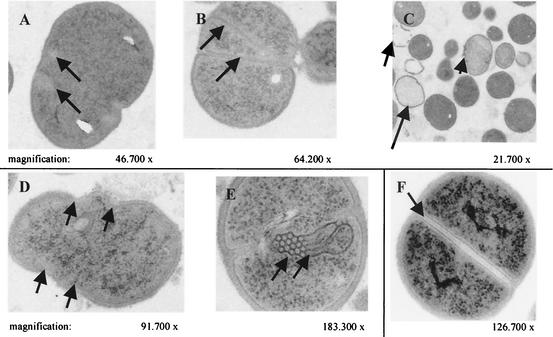
Scanning electron microscopy (SEM) of SCVs revealed heterogeneous bacteria of different sizes in addition to cells which seemed to be empty or dented and were covered with debris (Fig. 2B, panels I and II), which was more pronounced in fried-egg SCVs than in pinpoint SCVs. This was in stark contrast to homogenous cocci of the isogenic normal S. aureus (Fig. 2B, panel III, and C, panel III), on which no debris was present. Some SCVs were nearly eight times larger than normal S. aureus, presumably due to impaired cell separation. Moreover, an intercellular substance was more abundant in SCVs than in the normal S. aureus (Fig. 2C). Transmission electron microscopy (TEM) disclosed large “swollen” cells with several uncompleted cross walls and a reduced or undetectable splitting system in both SCV phenotypes (Fig. 3A, C, and D), whereas only in pinpoint SCVs were mesosome-like structures at the cross wall site detectable (Fig. 3E). In addition, some fried-egg SCVs possessed branched and multiple cross walls without obvious cell separation (Fig. 3B), while other cells lacked the cytoplasm (Fig. 3C), and debris of cell walls of dead cells was visible (Fig. 3C). For comparison, the morphology of the isogenic normal S. aureus is shown in Fig. 3F, demonstrating regular cell separation by cross walls surrounding a highly contrasting rectangular splitting system. The same images were seen with S. aureus ATCC 29213 (data not shown). All structural alterations present in fried-egg SCVs could be reversed to normal S. aureus morphology by supplementation of the culture medium with 100 μg of thymidine per ml (data not shown). While fried-egg SCVs reverted with a frequency of 10−3 in Mueller-Hinton (MH) broth without thymidine, pinpoint SCVs did not grow without additional thymidine, being absolutely dependent on thymidine, and thus did not revert.
FIG. 3.
TEM of fried-egg SCVs (A, B, and C), pinpoint SCVs (D and E), and normal S. aureus (F). (A and B) Arrows indicate incomplete or multiple cross walls. (C) Incomplete cross wall (small arrows), cellular debris (intermediate arrow), and empty cells (large arrows) are seen. (D and E) Pinpoint SCVs with atypical unrounded cells and mesosome-like structures (arrow). (F) Normal S. aureus cells displaying regular cell separation by a cross wall (arrow) surrounding a highly contrasting splitting system.
Interestingly, the morphological changes described in this report were similar to those induced by in vitro treatment of S. aureus with trimethoprim (6). However, thymidine-dependent SCVs collected in our study were isolated not only from patients currently undergoing SXT therapy but also from patients who had received SXT therapy in the past but had not received it for months or years (3). To test if it is possible to induce SCVs in vitro by application of SXT to MH broth, we cultured S. aureus Newman in MH broth with 16/304 μg of trimethoprim-sulfamethoxazole per ml, which is above the MIC. While no SCVs were found in Newman cultured in MH broth alone, SCVs were isolated from Newman grown in MH broth with SXT. Although most SCVs reverted upon the first subculture, we were able to isolate several stable SCVs which grew as pinpoint SCVs, indicating the possibility of in vitro induction of SCVs by SXT application.
Although low concentrations of thymidine present in Columbia blood agar allow culture of thymidine-dependent SCVs (which fail to grow on most MH and chemically defined medium agars [3]), the atypical colony morphology together with the unusual Gram stain appearance may pose major identification problems to the clinical microbiologist. Therefore, thymidine-dependent SCVs might be easily missed in the routine laboratory without appreciation of these colony characteristics, resulting in erroneous species identification or even discard of these pathogens as contaminants. In view of the increasing prevalence of multiresistant MRSA, for which SXT may represent one of the few active drugs, it is important to be aware of the emergence of thymidine-dependent SCVs, especially as a result of long-term therapy necessary for chronic disease such as osteomyelitis, wound infections, or CF (3, 10). In conclusion, our data demonstrate that thymidine-dependent S. aureus SCVs exhibiting unusual colony morphology and atypical Gram stain characteristics were associated with gross ultra structural changes consistent with impaired cell separation.
Acknowledgments
This work was funded by Innovative Medical Research Grant of the Medical Faculty, University of Muenster, Ka-1-6-I/98-45 (to B.C.K.), by a grant of the German Minister of Education and Research for the Interdisciplinary Center for Clinical Research, C8 (to M.H. and G.P.), and by NIH grant R01 42072 (to R.A.P).
We thank B. Ritzerfeld and B. Grünastel for expert technical assistance and U. Keller and E. Kiefermann (Institute for Medical Physics and Biophysics) for excellent assistance with SEM and TEM analysis and for high-class photographic work, respectively.
REFERENCES
- 1.Balwit, J. M., P. van Langefelde, J. M. Vann, and R. A. Proctor. 1994. Gentamicin-resistant menadione and hemin auxotrophic Staphylococcus aureus persist within cultured endothelial cells. J. Infect. Dis. 170:1033-1037. [DOI] [PubMed] [Google Scholar]
- 2.Gilligan, P. H., P. A. Gage, D. F. Welch, M. J. Muszynski, and K. R. Wait. 1987. Prevalence of thymidine-dependent Staphylococcus aureus in patients with cystic fibrosis. J. Clin. Microbiol. 25:1258-1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kahl, B., M. Herrmann, A. Schulze Everding, H. G. Koch, K. Becker, E. Harms, R. A. Proctor, and G. Peters. 1998. Persistent infection with small colony variant strains of Staphylococcus aureus in patients with cystic fibrosis. J. Infect. Dis. 177:1023-1029. [DOI] [PubMed] [Google Scholar]
- 4.Koo, S. P., A. S. Bayer, H. G. Sahl, R. A. Proctor, and M. R. Yeaman. 1996. Staphylocidal action of thrombin-induced platelet microbicidal protein is not solely dependent on transmembrane potential. Infect. Immun. 64:1070-1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lowy, F. D. 1998. Staphylococcus aureus infections. N. Engl. J. Med. 339:520-532. [DOI] [PubMed] [Google Scholar]
- 6.Nishino, T., J. Wecke, D. Krüger, and P. Giesbrecht. 1987. Trimethoprim-induced structural alterations in Staphylococcus aureus and the recovery of bacteria in drug-free medium. J. Antimicrobial. Chemother. 19:147-159. [DOI] [PubMed] [Google Scholar]
- 7.Proctor, R. A., J. M. Balwit, and O. Vesga. 1994. Variant subpopulations of Staphylococcus aureus as cause of persistent and recurrent infections. Infect. Agents Dis. 3:302-312. [PubMed] [Google Scholar]
- 8.Santos Sanches, I., A. Mato, H. de Lencastre, A. Tomasz, CEM/NET Collaborators, and International Collaborators. 2000. Patterns of multidrug resistance among clinical methicillin-resistant hospital isolates of coagulase-positive and coagulase-negative staphylococci collected in the international multicenter study RESIST in 1997 and 1998. Microb. Drug. Resist. 6:199-211. [DOI] [PubMed] [Google Scholar]
- 9.Seifert, H., C. von Eiff, and G. Fätkenheuer. 1999. Fatal case due to methicillin-resistant Staphylococcus aureus small colony variants in an AIDS patient. Emerg. Infect. Dis. 5:450-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.von Eiff, C., D. Bettin, R. A. Proctor, B. Rolaufs, N. Lindner, W. Winkelmann, and G. Peters. 1997. Recovery of small colony variants of Staphylococcus aureus following gentamicin bead placement for osteomyelitis. Clin. Infect. Dis. 25:1250-1251. [DOI] [PubMed] [Google Scholar]