Abstract
The ImmunoCard STAT! Cryptosporidium/Giardia rapid assay (Meridian Bioscience, Inc.) is a solid-phase qualitative immunochromatographic assay that detects and distinguishes between Giardia lamblia and Cryptosporidium parvum in aqueous extracts of human fecal specimens (fresh, frozen, unfixed, or fixed in 5 or 10% formalin or sodium acetate-acetic acid-formalin). By using specific antibodies, antigens specific for these organisms are isolated and immobilized on a substrate. After the addition of appropriate reagents, a positive test is detected visually by the presence of a gray-black color bar (regardless of the intensity) next to the organism name printed on the test device. A control is included in the device. Steps include tube preparation (buffer, patient specimen, conjugates A and B), testing (addition of sample onto the test device), and visual reading (total time, 12 min). Test performance was evaluated with known positive and negative stool specimens (170 specimens positive for Giardia and 231 specimens negative for Giardia) (85 specimens positive for Cryptosporidium and 316 specimens negative for Cryptosporidium); they were tested with trichrome, iron-hematoxylin, or modified acid-fast stains or the Meridian Bioscience, Inc., Giardia/Cryptosporidium Merifluor combination reagent; specimens with discrepant results were retested by using the Merifluor combination reagent. On the basis of the results of the reference methods, the sensitivities, specificities, and positive and negative predictive values were as follows: for G. lamblia, 93.5, 100, 100, and 95.5%, respectively; for C. parvum, 98.8, 100, 100, and 99.7%, respectively. False-negative results for G. lamblia were obtained with specimens with low parasite numbers (n = 7) or specimens containing trophozoites only (n = 3); one specimen with a false-negative result contained numerous cysts. The one specimen false negative for C. parvum was confirmed to be positive by immunofluorescence. No cross-reactivity was seen with 10 different protozoa (152 challenges), nine different helminths (35 challenges), or human cells (4 challenges) found in fecal specimens. This rapid test system may be very beneficial in the absence of trained microscopists; however, for patients who remain symptomatic after a negative result, the ova and parasite examination and special stains for other coccidia and the microsporidia should always remain options.
With continued interest in rapid diagnostic testing, potential waterborne outbreaks, fewer well-trained microscopists, and expanding evidence that Giardia lamblia and Cryptosporidium parvum can cause severe symptoms in humans, laboratories are reviewing their test ordering options with regard to immunoassay kits that can be incorporated into their routine diagnostic protocols (3, 4, 6, 11-15, 19-22, 24). Revised recommendations related to ordering ova and parasite (O&P) examinations, the newer stool immunoassays, and special tests (stains) for coccidia and microsporidia have been developed and laboratories are incorporating these changes into new ordering protocols (9, 10). Depending on specific patient information, each of the three test options has very specific benefits in terms of clinically relevant testing. Although different institutions may provide different ordering options, there are patient situations in which specific test options are recommended. If the results of the first tests are negative and the patient remains symptomatic, additional testing can then be performed.
Optimally, the stool immunoassays should provide adequate sensitivities and specificities and should provide clinically relevant, cost-effective, rapid results, particularly in a potential waterborne outbreak situation (1, 2, 7, 8, 16, 17). Renewed awareness of potential waterborne transmission of these parasites is based on the number of well-documented outbreaks during the past few years and the publicity surrounding water regulations and testing, particularly since it has been established that the infective dose of Cryptosporidium oocysts in humans can be relatively low (7, 18).
In patients who are infected with one or more of these parasites, the use of routine diagnostic methods such as concentration and trichrome and modified acid-fast staining may be insufficient to demonstrate the presence of these organisms (5, 15, 23). As acute infections with C. parvum resolve, the number of oocysts dramatically decreases. Also, the number of C. parvum oocysts passed by patients, including those with human immunodeficiency virus disease, varies from day to day and week to week.
Antigen detection assays for G. lamblia and C. parvum have proven to be very useful in the diagnosis of enteric parasites (4, 11-15, 20-22, 24). The advantages of these assays include labor, time, and batching efficiencies that may lead to cost reductions. These reagents offer relevant alternative methods to the routine O&P examination method and provide the added sensitivity required to confirm infections in patients with low parasite numbers.
Most commercially available immunoassays use the enzyme immunoassay format, which requires multiple reagent additions, washing steps, and incubations. A nonenzymatic rapid immunoassay for Giardia and Cryptosporidium antigens has been developed. This test (ImmunoCard STAT! Cryptosporidium/Giardia Rapid Assay; Meridian Bioscience, Inc.) is marketed commercially. The assay can be performed in approximately 12 min on formalin-fixed (5 or 10% formalin or sodium acetate-acetic acid-formalin) or unfixed stool specimens. In this study, this cartridge was tested against known positive and negative fecal specimens on the basis of the results of the O&P examination for the detection of G. lamblia and on the basis of the results of acid-fast staining or immunofluorescence for the detection of C. parvum. Specimens with discrepant results were retested by fluorescent-antibody methods.
MATERIALS AND METHODS
Specimens.
Human fecal specimens were collected in 10% formalin or sodium acetate-acetic acid-formalin and submitted to the author-affiliated laboratories. A total of 401 specimens were tested by the reference methods and the ImmunoCard STAT! Cryptosporidium/Giardia Rapid Assay. The following numbers of specimens were tested by the various sites: 28 at Children's Hospital of Eastern Ontario; 86 at Kaiser Permanente, North Hollywood; 74 at LSG & Associates; 89 at Turner Laboratory; and 124 at the University of California, Los Angeles, for a total of 401 specimens.
Routine O&P examination, modified acid-fast staining examination, or fluorescent-antibody immunoassay.
The O&P examination (formalin-ethyl acetate concentration, trichrome or iron hematoxylin staining) and modified acid-fast staining or the fluorescent-antibody immunoassay were considered the reference methods (10, 11). The various reference methods used to test the specimens for Giardia and Cryptosporidium included iron-hematoxylin-Kinyoun staining, which reveals both parasites, at Children's Hospital of Eastern Ontario; trichrome and modified acid-fast staining, respectively, at Kaiser Permanente, North Hollywood; trichrome staining and direct fluorescent-antibody assay, respectively, at LSG & Associates; trichrome staining and modified acid-fast staining, respectively, at Turner Laboratory; and trichrome staining and direct fluorescent-antibody assay, respectively, at the University of California, Los Angeles. Of the 401 specimens examined, a certain number were positive for the following parasites on the basis of the results of the reference methods: Giardia, n = 162 specimens; Cryptosporidium, n = 77 specimens; and mixture of Giardia and Cryptosporidium, n = 8 specimens. Different parasites (10 protozoa, including trophozoites, cysts, oocysts, and spores; nine helminths, including eggs and larvae; and four specimens containing human cells [polymorphonuclear leukocytes, macrophages]) were included among the negative specimens (n = 154). All specimens were patient specimens, not seeded specimens, and some contained multiple organisms. Specific organisms included Blastocystis hominis (n = 40), Cyclospora cayetanensis (n = 5), Dientamoeba fragilis (n = 15), Endolimax nana (n = 46), Entamoeba coli (n = 25), Entamoeba hartmanni (n = 5), Entamoeba histolytica/E. dispar (n = 10), Iodamoeba bütschlii (7), Isospora belli (n = 1), microsporidia (n = 2), Ascaris lumbricoides (n = 10), Diphyllobothrium latum (n = 2), Dipylidium caninum (n = 1), Enterobius vermicularis (n = 3), hookworm (n = 5), Hymenolepis nana (n = 8), Strongyloides stercoralis (n = 4), Taenia sp. (n = 1), and Trichuris trichiura (n = 1). Although the results of the reference methods were known, the specimens were coded and tested blind when the cartridge was used.
Specimen preparation for cartridge immunoassay.
All tests were performed with unconcentrated, preserved stool specimens (formalin-based fixatives).
ImmunoCard STAT! Cryptosporidium/Giardia Rapid Assay.
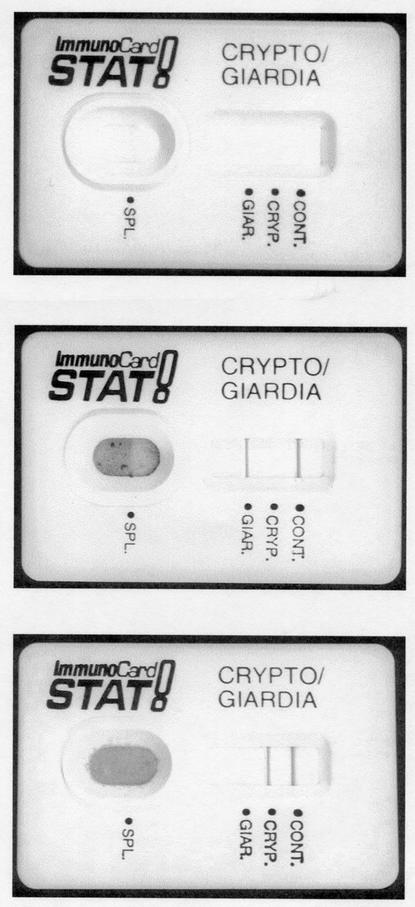
The ImmunoCard STAT! Cryptosporidium/Giardia Rapid Assay (Meridian Bioscience, Inc.) immunoassay diagnostic kit was used according to the directions of the manufacturer. By using specific antibodies, antigens specific for Giardia and Cryptosporidium are captured and immobilized on a membrane. The assay procedure involves the sequential addition of 2 drops of sample treatment buffer to a tube, the pipetting of 60 μl of an uncentrifuged stool specimen into the tube, the addition of 2 drops of a Giardia capture antibody conjugate, and the addition of 2 drops of a colloidal carbon-conjugated detection reagent for Giardia and Cryptosporidium. None of these reagent addition steps are timed; the reagents are pipetted one after the other. After the sample is mixed, it is immediately poured into the test device. Assay results are read after 10 min. Positive results are visualized as gray-black lines (regardless of intensity) in the appropriate position in the results window (Fig. 1). The tubes, pipettes, devices, and all reagents are provided with the kit.
FIG. 1.
ImmunoCard STAT! Cryptosporidium/Giardia Rapid Assay (Meridian Bioscience, Inc.). Top, unused cartridge; middle, positive result for Giardia; bottom, positive result for Cryptosporidium. Note that the control line is positive for the images in both the middle and bottom cartridges.
Testing for resolution of discrepant results.
Specimens with discrepant results for G. lamblia and C. parvum were retested with the Meridian Bioscience, Inc., Merifluor combination Cryptosporidium/Giardia reagent for G. lamblia and C. parvum.
RESULTS
Immunochromatographic assay for Giardia.
On the basis of the reference methods, known positive specimens (G. lamblia, n = 162; mixture of G. lamblia and C. parvum, n = 8) and negative specimens (n = 231) were tested by the ImmunoCard STAT! Cryptosporidium/Giardia Rapid Assay. All specimens with discrepant results by the ImmunoCard STAT! Cryptosporidium/Giardia Rapid Assay were retested by using the Meridian Bioscience, Inc., Merifluor combination Cryptosporidium/Giardia reagent. If the specimen was positive by any two methods, the specimen was considered truly positive. After resolution, the total number of positive specimens was 159 of 170, the sensitivity was 93.5%, the specificity was 100%, the positive predictive value (PPV; predictive value of a positive test result) was 100%, and the negative predictive value (NPV; predictive value of a negative test result) was 95.5% (Table 1). False-negative results for G. lamblia were obtained for seven specimens with low parasite numbers (10 to 100 cysts by immunofluorescence) and three specimens containing trophozoites only; one specimen with false-negative results contained numerous cysts. The false-negative results were obtained on repeat testing with the cartridge; these results are indicative of the sensitivity limitations of the assay with specimens containing low parasite numbers. However, we have no reasonable explanation for why the specimen with false-negative results containing numerous G. lamblia cysts was negative on repeat testing. This false-negative result may reflect improper specimen handling prior to fixation and/or the use of an improperly prepared fixative.
TABLE 1.
Comparison of results prior to and after testing of specimens with discrepant resultsa
| Organism | Result (no. of specimens) | No. of specimens with the indicated result
|
|||||
|---|---|---|---|---|---|---|---|
| Trichrome, modified acid-fast staining and/or Merifluor DFA (reference methods)
|
ImmunoCard STAT! Cryptosporidium/Giardia combination rapid solid-phase qualitative immunochromato- graphic assay
|
After FA to resolve discrepancies
|
|||||
| Pos | Neg | Pos | Neg | Pos | Neg | ||
| G. lamblia | Pos (170) | 170 | 0 | 159 | 11b | 170 | 0 |
| Neg (231) | 0 | 231 | 0 | 231 | 0 | 231 | |
| Total (401) | |||||||
| C. parvum | Pos (85) | 85 | 0 | 84 | 1c | 85 | 0 |
| Neg (316) | 0 | 316 | 0 | 316 | 0 | 316 | |
| Total (401) | |||||||
Abbreviations: DFA, direct fluorescent-antibody assay; FA, fluorescent-antibody assay; Pos, positive; Neg, negative.
Specimens with false-negative results for G. lamblia had low parasite numbers (n = 7) or trophozoites only (n = 3); one specimen with a false-negative result contained numerous cysts.
The one specimen with a false-negative result for C. parvum was confirmed to be positive by immunofluorescence.
Immunochromatographic assay for Cryptosporidium.
On the basis of the reference methods, known positive specimens (C. parvum, n = 77; mixture of G. lamblia and C. parvum, n = 8) and negative specimens (n = 316) were tested by the ImmunoCard STAT! Cryptosporidium/Giardia Rapid Assay. All specimens with discrepant results by the ImmunoCard STAT! Cryptosporidium/Giardia Rapid Assay were retested by using the Meridian Bioscience, Inc., Merifluor combination Cryptosporidium/Giardia reagent. If the specimen was positive by any two methods, the specimen was considered truly positive. After resolution, the total number of positive specimens was 84 of 85, the sensitivity was 98.8%, the specificity was 100%, the PPV was 100%, and the NPV was 99.7% (Table 1). The one specimen with a false-negative result was confirmed to be positive by immunofluorescence.
DISCUSSION
In patients with giardiasis or cryptosporidiosis, the use of routine diagnostic methods such as concentration and trichrome or modified acid-fast staining may be insufficient to demonstrate the presence of these organisms (10, 13, 24). On the basis of O&P examination with the trichrome stain, as well as the Meridian Bioscience, Inc., Merifluor combination Giardia/Cryptosporidium reagent, the sensitivity for Giardia was 93.5%, the specificity was 100%, the PPV was 100%, and NPV was 95.5%. The sensitivity for Cryptosporidium was 98.8%, the specificity was 100%, the PPV was 100%, and the NPV was 99.7%. This testing approach is more relevant for patient care when particular infections such as cryptosporidiosis or giardiasis are suspected. In many geographic areas, physicians should have the option to order tests that are most appropriate given their patients' histories, including the O&P examination for those who live in large metropolitan areas or have traveled to countries where multiple parasites are found. In contrast, in possible day care or waterborne outbreak situations or geographic areas where very specific organisms tend to be found, specific tests for giardiasis or cryptosporidiosis may be more appropriate. Specific test orders are also relevant for those who are immunocompromised. In a situation in which the test ordered is negative and the patient remains symptomatic, other tests can then be ordered. Laboratories and physicians are now beginning to use specific ordering algorithms that take into account the patient's condition and complete history, an approach that is more relevant for quality patient care.
Although the reagent costs for the rapid cartridge format may be more than those for the routine O&P methods, the labor costs will be considerably less when the rapid cartridge format is used. When the costs of diagnostic tests are compared, it is important to consider all aspects of testing, including but not limited to, reagents, labor, repeat tests, quality control, reagent storage, the number of tests requested, staff expertise in microscopy, and training requirements.
The ability to concurrently detect and distinguish between Giardia and Cryptosporidium antigens in formalin-fixed or unfixed fecal specimens by a 10-min nonenzymatic immunoassay provides the user with another very useful diagnostic kit, the ImmunoCard STAT! Cryptosporidium/Giardia Rapid Assay (Meridian Bioscience, Inc.). However, it is important to remember that the rapid immunoassays do not take the place of routine O&P examinations, but they are very useful when one is trying to diagnose Giardia and Cryptosporidium infections (10).
Acknowledgments
We thank Meridian Bioscience, Inc., for providing the ImmunoCard STAT! Cryptosporidium/Giardia Rapid Assay diagnostic kits, as well as for financial support and the confirmative diagnostic kits.
REFERENCES
- 1.Addis, D. G., J. P. David, J. M. Roberts, and E. E. Mast. 1992. Epidemiology of giardiasis in Wisconsin: increasing incidence of reported cases and unexplained season trends. Am. J. Trop. Med. Hyg. 47:13-19. [DOI] [PubMed] [Google Scholar]
- 2.Atherton, F., C. P. Newman, and D. P. Casemore. 1995. An outbreak of waterborne cryptosporidiosis associated with a public water supply in the UK. Epidemiol. Infect. 115:123-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boone, J. H., T. D. Wilkins, T. E. Nash, J. E. Brandon, E. A. Macias, R. C. Jerris, and D. M. Lyerly. 1999. TechLab and Alexon Giardia enzyme-linked immunosorbent assay kits detect cyst wall protein 1. J. Clin. Microbiol. 37:611-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chan, R., J. Chen, M. K. York, N. Setijono, R. L. Kaplan, F. Graham, and H. B. Tanowitz. 2000. Evaluation of a combination rapid immunoassay for detection of Giardia and Cryptosporidium antigens. J. Clin. Microbiol. 38:393-394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Current, W. L., and L. S. Garcia. 1991. Cryptosporidiosis. Clin. Microbiol. Rev. 3:325-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doing, K. M., J. L. Hamm, J. A. Jellison, J. A. Marquis, and C. Kingsbury. 1999. False-positive results obtained with the Alexon ProSpecT Cryptosporidium enzyme immunoassay. J. Clin. Microbiol. 37:1582-1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DuPont, H. L., C. L. Chappell, C. R. Sterling, P. C. Okhuysen, J. B. Rose, and W. Jakubowski. 1995. The infectivity of Cryptosporidium parvum in healthy volunteers. N. Engl. J. Med. 332:855-859. [DOI] [PubMed] [Google Scholar]
- 8.Fayer, R., J. M. Trout, and M. C. Jenkins. 1998. Infectivity of Cryptosporidium parvum oocysts stored in water at environmental temperatures. J. Parasitol. 84:1165-1169. [PubMed] [Google Scholar]
- 9.Garcia, L. S. 1999. Practical guide to diagnostic parasitology. ASM Press, Washington, D.C.
- 10.Garcia, L. S. 2001. Diagnostic medical parasitology, 4th ed. ASM Press, Washington, D.C.
- 11.Garcia, L. S., and R. Y. Shimizu. 1997. Evaluation of nine immunoassay kits (enzyme immunoassay and direct fluorescence) for the detection of Giardia lamblia and Cryptosporidium parvum in human fecal specimens. J. Clin. Microbiol. 35:1526-1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garcia, L. S., and R. Y. Shimizu. 2000. Detection of Giardia lamblia and Cryptosporidium parvum antigens in human fecal specimens using the ColorPAC combination rapid solid-phase qualitative immunochromatographic assay. J. Clin. Microbiol. 38:1267-1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garcia, L. S., R. Y. Shimizu, and C. N. Bernard. 2000. Detection of Giardia lamblia, Entamoeba histolytica/Entamoeba dispar, and Cryptosporidium parvum antigens in human fecal specimens using the Triage Parasite Panel enzyme immunoassay. J. Clin. Microbiol. 38:3337-3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garcia, L. S., A. C. Shum, and D. A. Bruckner. 1992. Evaluation of a new monoclonal antibody combination reagent for direct fluorescent detection of Giardia cysts and Cryptosporidium oocysts in human fecal specimens. J. Clin. Microbiol. 30:3255-3257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kehl, K. C., H. Cicirello, and P. L. Havens. 1995. Comparison of four different methods for the detection of Cryptosporidium species. J. Clin. Microbiol. 33:416-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mackenzie, W. R., N. J. Hoxie, and M. E. Proctor. 1994. A massive outbreak in Milwaukee of Cryptosporidium infection transmitted through the public water supply. N. Engl. J. Med. 331:161-167. [DOI] [PubMed] [Google Scholar]
- 17.Marshall, M. M., D. Naumovitz, Y. Ortega, and C. R. Sterling. 1997. Waterborne protozoan pathogens. Clin. Microbiol. Rev. 10:67-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pieniazek, N. J., F. J. Bornay-Llinares, S. B. Slemenda, A. J. da Silva, I. N. S. Moura, M. J. Arrowood, O. Ditrich, and D. G. Addis. 1999. New Cryptosporidium genotypes in HIV-infected persons. Emerg. Infect. Dis. 5:444-449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Priest, J. W., J. P. Kwon, D. M. Moss, J. M. Roberts, M. J. Arrowood, M. S. Dworkin, D. D. Juranek, and P. J. Lammie. 1999. Detection of enzyme immunoassay of serum immunoglobulin G antibodies that recognize specific Cryptosporidium parvum antigens. J. Clin. Microbiol. 37:1385-1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenblatt, J. E., and L. M. Sloan. 1993. Evaluation of an enzyme-linked immunosorbent assay for detection of Cryptosporidium spp. in stool specimens. J. Clin. Microbiol. 31:1468-1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosenblatt, J. E., L. M. Sloan, and S. K. Schneider. 1993. Evaluation of an enzyme-linked immunosorbent assay for the detection of Giardia lamblia in stool specimens. Diagn. Microbiol. Infect. Dis. 16:337-341. [DOI] [PubMed] [Google Scholar]
- 22.Rosoff, J. D., C. A. Sanders, S. S. Sonnad, P. R. De Lay, W. K. Hadley, F. F. Vincenzi, D. M. Yajko, and P. D. O'Hanley. 1989. Stool diagnosis of giardiasis using a commercially available enzyme immunoassay to detect Giardia-specific antigen 65 (GSA 65). J. Clin. Microbiol. 27:1997-2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wolfe, M. S. 1992. Giardiasis. Clin. Microbiol. Rev. 5:93-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zimmerman, S. K., and C. A. Needham. 1995. Comparison of conventional stool concentration and preserved-smear methods with Merifluor Cryptosporidium/Giardia direct immunofluorescence assay and ProSpecT Giardia EZ microplate assay for detection of Giardia lamblia. J. Clin. Microbiol. 33:1942-1943. [DOI] [PMC free article] [PubMed] [Google Scholar]