Abstract
OBJECTIVE
To compare primary care providers’ depression-related knowledge, attitudes, and practices and to understand how these reports vary for providers in staff or group-model managed care organizations (MCOs) compared with network-model MCOs including independent practice associations and preferred provider organizations.
DESIGN
Survey of primary care providers’ depression-related practices in 1996.
SETTING AND PARTICIPANTS
We surveyed 410 providers, from 80 outpatient clinics, in 11 MCOs participating in four studies designed to improve the quality of depression care in primary care.
MEASUREMENTS AND MAIN RESULTS
We measured knowledge based on depression guidelines, attitudes (beliefs about burden, skill, and barriers) related to depression, and reported behavior. Providers in both types of MCO are equally knowledgeable about treating depression (better knowledge of pharmacologic than psychotherapeutic treatments) and perceive equivalent skills in treating depression. However, compared with network-model providers, staff/group-model providers have stronger beliefs that treating depression is burdensome to their practice. While more staff/group-model providers reported time limitations as a barrier to optimal depression treatment, more network-model providers reported limited access to mental health specialty referral as a barrier. Accordingly, these staff/group-model providers are more likely to treat patients with major depression through referral (51% vs 38%) or to assess but not treat (17% vs 7%), and network-model providers are more likely to prescribe antidepressants (57% vs 6%) as first-line treatment.
CONCLUSIONS
Whereas the providers from staff/group-model MCOs had greater access to and relied more on referral, the providers from network-model organizations were more likely to treat depression themselves. Given varying attitudes and behaviors, improving primary care for the treatment of depression will require unique strategies beyond enhancing technical knowledge for the two types of MCOs.
Keywords: depression, knowledge, attitudes, practice, primary care, managed care
At least 40% of individuals with major depression receive some mental health care in primary care settings.1, 2 Assessment and treatment of depression as primary care, rather than or in addition to referral to a mental health specialist, may be increasing under policies that hold primary care providers (PCPs) accountable for delivering high-quality and cost-efficient health services.3 These policies include requiring or encouraging adherence to guidelines or best practices, gatekeeping, restricted panels, and utilization review.4–10
Policies within a managed care organization (MCO) may encourage or discourage primary care treament of depression. The literature suggests, however, that broad organizational features of the practice environment may also affect how care for depression is delivered to primary care patients. One method for examining these broad organizational features is to compare primary care depression treatment in staff or group-model MCOs versus network-model MCOs. In staff/group-model MCOs, all providers work within a relatively large, uniform clinical practice management structure, in most cases work exclusively for the MCO, and are paid through a single source. These MCOs typically include both primary care and a wide range of specialty care providers within the same organizational structure. Network-model MCO providers, in contrast, manage their clinical practices independent of plan dictates. In network-model MCOs, primary care providers and specialty care providers often work in different small practices linked only by the payment plan, and may serve multiple payers. Although some have argued that this simple classification scheme is insufficient given the recent emergence of diverse types of plans,11 such comparisons are useful for initially exploring whether previously documented differences in clinical practice may be affecting depression treatment as well.
The literature documents a number of differences between staff/group-model and network-model MCOs that can affect care for depression.12, 13 Compared with network models, staff/group-model MCOs tend to have more accessible referrals because PCPs and mental health specialists (psychiatrists, psychologists, and social workers) all work for a centrally managed organization and frequently practice in the same physical location. Staff/group-model MCOs also tend to have less financial risk to individual providers for referral 14 because network-model MCOs are more likely to pay providers by capitation, to require referral through the patient’s gatekeeper, and to subject referrals to intensive utilization review or physician profiling.7, 15–17 Staff/group-model MCOs also have more uniform standards for staff recruitment and review. In general, they have more demanding requirements for selecting physicians (e.g., higher rates of board certification) but are more supportive of using nonphysician staff.18 In the area of quality of care assessment and improvement, the literature is less consistent. Compared with network models, staff/group-model MCOs are equally or more likely to implement guidelines and to develop quality assurance programs,19 use more outcomes studies in quality improvement programs,8 have less autonomy in implementing practice changes,20, 21 and possibly have higher quality of care, though the last study had limited precision for comparing MCO types.22
The literature on staff/group-model and network-model MCOs provides clues about how the major organizational differences affect clinical practice in general, but there is little or no information on how these differences affect care for mental health. This article assesses reports about depression care from providers in these two types of MCOs as part of a broader effort to improve care for depression in a wide variety of managed primary care settings. In order to better design quality improvement strategies for different types of managed care settings, we assess whether and how the organizational differences between MCOs translate into differences among practicing PCPs’ knowledge, attitudes, and reported treatment practices. We use the term “attitudes” broadly to represent not only beliefs about the burden of treating depressed patients in providers’ practices, but also perceived skill in treating depression, and perceived financial and organizational barriers encountered by providers in trying to care for depressed patients.
We hypothesized that because staff/group-model MCOs employ both PCPs and mental health specialists in the same organization, the PCPs in these MCOs would rely more on specialist care to treat depression. We suspected that network-model MCO providers, of necessity, would perceive themselves as more skilled in caring for depression and initiate treatment themselves more often.
METHODS
The data reported are from four separately funded studies, collectively referred to as Quality Improvement for Depression (QID), which evaluate the effectiveness of alternative quality improvement strategies for major depression in primary care. Each of the four depression studies in this article surveyed all participating PCPs in specific MCOs during 1996 before undertaking interventions to improve care for depression using a core questionnaire. In general, MCOs were selected by their willingness to participate in the original study to improve the quality of primary care treatment for depression. One study selected seven different MCOs with at least one organization in each of the four U.S. census regions; a second study selected 12 practices across 10 different U.S. states; and the remaining two studies selected one or two staff/group-model MCOs within a single state. Eligible PCPs in each study included physicians, physician assistants, and nurse practitioners working in practices enrolled in one of the four studies. One of the practices included house officers in training.
Classification of Practices
The study sites included 80 participating primary care practices affiliated with 11 different MCOs. Each depression study had specific reasons for selecting its participating MCOs, but the QID was formed because the four studies collectively represent variation in geographic region and in the nature of the arrangements between the practices and MCOs. We grouped the 11 MCOs enrolled in the studies into staff/group-model or network-model categories based on definitions from the literature.11–13, 16, 23, 24 Staff/group-model MCOs were defined as practices with prospective budgeting in which most PCPs worked exclusively for a single integrated health care system or as part of a single medical group that contracts exclusively with one capitated health plan. Network-model MCOs included solo or small group practices linked through some kind of practice network and one voluntary research network of unrelated practices, all of which usually negotiate contracts with various managed care plans.
Using this definition, providers from three of the participating MCOs fell into the staff/group-model category, including a traditional not-for-profit HMO, a Veteran’s Health Administration (VA) system of clinics, and an HMO that contracts exclusively with a single provider group. We grouped the 69 VA clinicians (all from study A in Table 1)) along with those in the other staff/group-model MCOs because the VA system is structured similarly to other MCOs in this category. Many characteristics (demographics, patient volume, training, and consultations with mental health professionals) are also comparable. But the VA practices have more physicians-in-training, see more new, male, and older patients, spend more time in specialty care, are more likely to participate in utilization management, and are more likely to use practice guidelines compared with the other practices classified as staff/group-model MCOs.
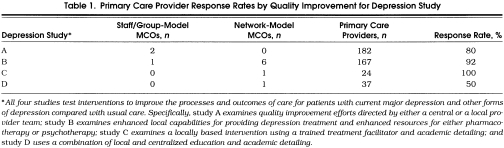
Table 1.
Primary Care Provider Response Rates by Quality Improvement for Depression Study
Providers from the remaining MCOs fell into the network-model MCO category, including a large network-style HMO, a large physician practice management company, a system of not-for-profit multispecialty public health centers, a mixed-model network of practices, and four multifinanced HMOs. Providers in the mixed-model group were categorized with the network-model MCOs after analysis showed that they were significantly different from the “pure” staff/group-model MCO providers and quite similar to the “pure” network-model MCO providers on demographic characteristics and practice activities.
Primary Care Provider Survey
Data were collected by a self-administered survey mailed to the 500 eligible PCPs in the 80 practices. The confidential survey took approximately 20 minutes to complete. Nonresponding providers were telephoned and encouraged to return a survey. Depending on the study and participating MCO, some providers were rewarded for completing surveys with small gifts (e.g., a certificate for a cup of gourmet coffee) or given small monetary incentives ($5 cash). Analyses in this article are based on core survey items that were uniform across all four depression studies with the exception of the attitude questions on perceived burden. These questions were not asked by study B (see Table 1). The survey consisted both of batteries previously evaluated for reliability and validity and of batteries developed specifically for this study. Key batteries used in these analyses focus on the measures of knowledge, attitudes, and reported treatment behavior relative to depression, as described below. More information about the four depression studies including the full Clinical Background Questionnaire instrument used here is publicly available at the QID Website: qid.org.
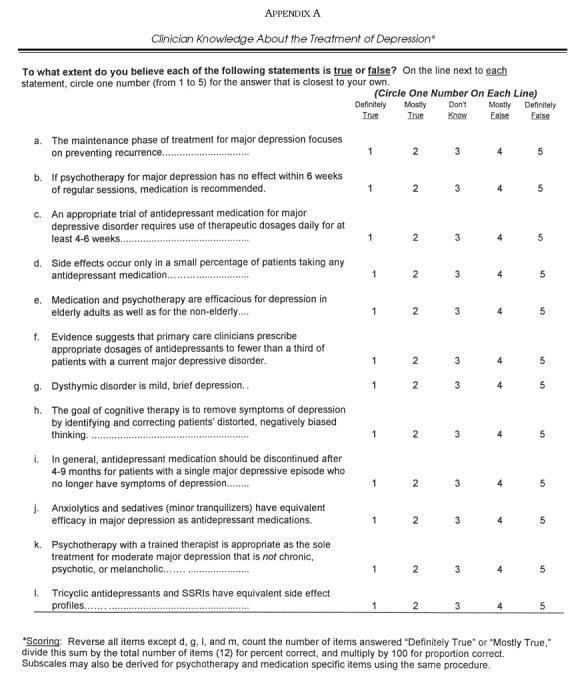
Knowledge
We examined four aggregate measures of knowledge about the treatment of depression based on a 12-item test measuring endorsement of evidence-based statements from the Agency for Health Care Policy and Research (AHCPR) practice guidelines for depression and validated by a panel of clinicians as unambiguous indicators of knowledge (items and scoring rules are shown in Appendix A).25 Statements were rated on a 5-point Likert scale ranging from “very false” to “very true.” We computed an overall knowledge scale(percentage answered correctly) and subscales for general knowledge (e.g., about phases of treatment), knowledge of antidepressant medication, and knowledge of psychotherapy. We included a single-item measure of providers’familiarity with the AHCPR guidelines for the treatment of depression. This item was dichotomized to represent the percentage of providers who “have discussed them with colleagues or heard information on them presented,”“have read them,” or “refer to them sometimes when treating patients” versus “have never heard of them.”
Attitudes.
Attitudinal measures include beliefs about burden due to depression, perceived depression treatment skill, and perceived barriers to optimal treatment of depression.
The beliefs about burden measure is a 7-item subscale of the psychosocial belief battery developed by Ashworth, Williamson, and Montano,26 and later adapted for depression.27 Items included statements regarding the practice burden associated with treating depression: for example, “evaluating and treating depression problems will cause me to be more overburdened than I already am.” We scored these 5-point Likert agreement items by reversing negatively indicated items, computing their average, and rescaling the distribution to a 0-to-100 scale, where a high score indicates stronger feelings of burden (α=.70).
Providers rated their skill in counseling and education, diagnosis, prescribing medication, and referral for depression on a 4-point scale (not at all, slightly, somewhat, or very skilled). We present data for each item dichotomized so that 1 indicates “very skilled” (versus all other categories) and also used an aggregate scale, averaged across all four originally scored items and scored as a 0-to-100 scale, where a high score indicates more perceived skill (α=.68).28
Perceived barriers to treating depression were assessed by asking providers to rate the extent to which seven different factors limit their ability to provide optimal treatment for depression: (1) patient or family is reluctant to accept diagnosis or treatment, (2) medical problems are more pressing, (3) preferred medication is difficult to obtain, (4) mental health professionals are not available, (5) limited visit time is available for counseling/education, (6) inadequate time is available to provide follow-up, and (7) reimbursement is poor or benefits are limited. Providers report whether they are limited a “great deal” versus “somewhat limited” or “not at all limited” by each barrier in their care for depressed patients. The measure is based on the work of Rost, Humphrey, and Kelleher.29
Behavior.
To assess reported behavior, we used responses to items from two different batteries. One battery asks providers about the likelihood of their using five treatment strategies as the first-line treatment for major depression: (1) assess but not treat at this time, (2) personally prescribe medication, (3) personally counsel or provide psychotherapy, (4) refer to mental health specialty, and (5) refer to patient education or self-help program. These treatment proclivities are based on a brief scenario describing a female patient with major depressive disorder. We report the percentage of providers who are “very likely” (versus “somewhat likely,”“neutral,”“somewhat unlikely,” or “very unlikely”) to use each treatment. The other battery asks providers to report the percentage of patients in their practice with moderate to severe depression for whom they typically prescribe tricyclic antidepressants, or selective serotonin reuptake inhibitors (SSRIs).
Analysis
We used Student’s t tests, χ2analysis, and correlational methods to examine bivariate relations between type of MCO (staff/group model vs network model) and provider knowledge about depression, attitudes about treating depression (including beliefs, skill, and barriers), and reported depression treatment behavior. We then used multivariate regression analysis (logistic for binary and ordinary least squares for continuous variables) to evaluate the MCO effect on knowledge, attitudes, and reported behavior using the items or scales identified as important in bivariate analysis. We examined the total effect, and then the unique effect of MCO type after sequentially controlling for underlying provider characteristics, examining the effects of adding each potential confounder. Provider characteristics included age, gender, hours worked, and participation in depression-specific continuing medical education (CME), all of which may be associated with MCO type either causally or by chance in our sample. As nearly two thirds of the MCOs represented here are from the Western United States, we tested the regional effect of MCO maturity by also including a “west” variable in our regression models. Our final sequential model included provider characteristics (age, gender, ethnicity, specialty, and type), general practice activities (time spent in primary care, intensity of follow-up with patients, and intensity of participation in utilization management), and depression-specific practice activities (providers’ estimated proportion of visits involving patients with depression, participation in CME for depression, and participation in quality assurance for depression) and assessed these measures of provider type in relation to knowledge, attitudes, and behavior. The 32 residents based in staff/group-model MCOs were excluded from all analyses reported here, yielding data for 378 of the 410 QID provider participants. We also use sensitivity analysis to determine whether or not to analyze the VA data separately.
Because of the hierarchical nature of these data, with multiple providers nested within practices and practices nested within MCOs, we also explored the sensitivity of multivariate models to the clustered sampling design using robust standard errors, adjusted nonparametrically by effectively decreasing the sample size to reflect the nonindependence of observations.30, 31
RESULTS
Response Rates
We received completed surveys from 410 (82%) of the 500 clinicians eligible for participation. Response rates varied across the four studies (see Table 1).
Provider Characteristics
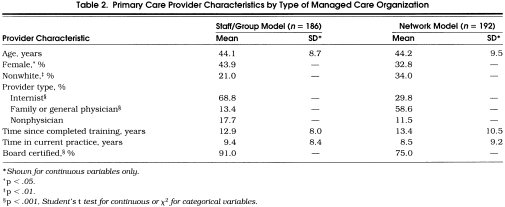
Table 2 shows provider characteristics by type of MCO. Staff/group–model MCOs had significantly more women practitioners (p < .05), fewer ethnic-minority providers (p < .01), more internists versus family or general physicians, largely due to selection into the particular organizations studied (p < .001), and more board-certified providers (p < .001) than network-model MCOs.
Table 2.
Primary Care Provider Characteristics by Type of Managed Care Organization
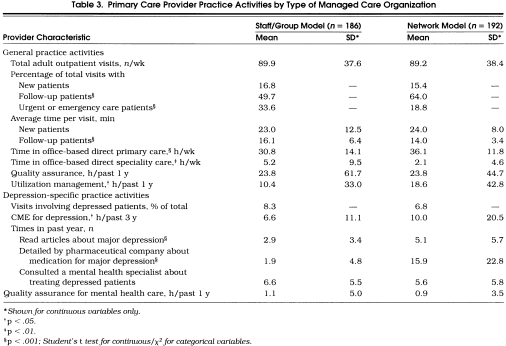
Table 3 shows the practice activities of these providers. Compared with network-model MCO providers, staff/group-model MCO providers reported spending significantly more of their work day seeing patients for urgent care (p < .001) than for follow-up care. They also spent significantly more time providing specialty care (p < .01) than primary care (p < .01), and spent less time in utilization management (p < .05). With regard to depression-specific activities, these staff/group-model MCO providers spent fewer hours in CME (p < .05), read fewer articles about depression (p < .001), and had less exposure to detailing about antidepressants from a pharmaceutical company (p < .001).
Table 3.
Primary Care Provider Practice Activities by Type of Managed Care Organization
What Providers Know About Depression Treatment and Guidelines
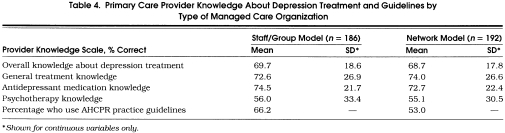
Overall, PCPs answered approximately 70% of our knowledge questions correctly (Table 4 Providers had higher scores on knowledge about treating depression with medication (three fourths of items correct) than knowledge about psychotherapy (slightly more than half of items correct). Knowledge about depression treatment did not differ by type of MCO, nor did knowledge of AHCPR practice guidelines.
Table 4.
Primary Care Provider Knowledge About Depression Treatment and Guidelines by Type of Managed Care Organization
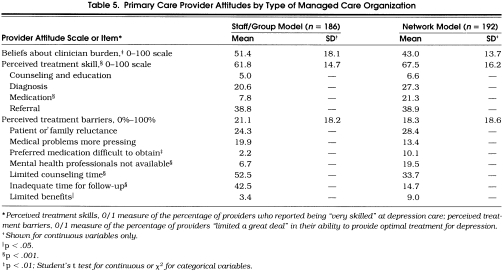
What Providers Think About Their Depression Care
Significantly more PCPs from staff/group-model MCOs reported that dealing with depression is burdensome to their practice (p < .01) than did network-model providers (Table 5)Network-model MCO providers reported higher overall perceived skill at treating depression especially for treatment with medication (p < .001). There were no overall differences in providers’ perceived barriers to depression care. However, staff/group-model MCO providers reported significantly more time limitations, either for counseling (p < .001), or for follow-up (p < .001), or because the preferred medication was difficult to obtain (p < .01). Network-model MCO providers were significantly more likely to report that unavailability of mental health professionals created limitations (p < .001) or that patients had limited benefits (p < .05).
Table 5.
Primary Care Provider Attitudes by Type of Managed Care Organization
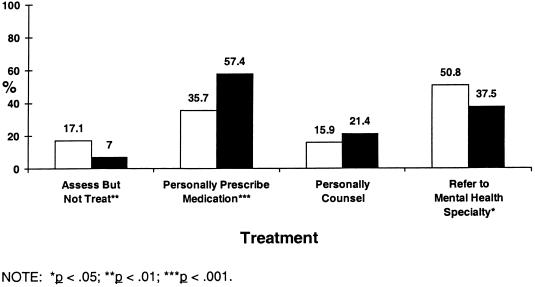
What Providers Say They Do to Treat Depression
Figure 1 shows that across MCO types, the most common first-line treatment strategies are medication and referral to mental health specialists, and the least common strategy is personally providing counseling. Providers in staff/group-model MCOs are more likely to report assessing but not treating patients (p < .01) or referring them to mental health specialty (p < .05), while network-model MCO providers are more likely to report starting their patients on an antidepressant medication (p < .001).
Figure 1.
Percentage of primary care providers “very likely” to use specific treatments for major depression by type of MCO. Open bars are staff/group-model MCOs; closed bars are network-model MCOs.
We also examined more specific differences in PCP antidepressant prescribing behavior from reports of the percentage of patients with moderate to severe depression for whom providers typically prescribe different types of antidepressants (not shown in Fig. 1). According to these data, providers in staff/group-model MCOs are significantly less likely to report routinely prescribing SSRIs compared with network-model MCO providers (13% vs 26%, p < .001). Across groups, SSRIs are more commonly prescribed than tricyclics or minor tranquilizers (19% vs 2% vs 0.3%, respectively).
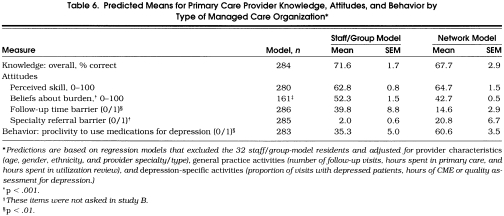
Multiple Regression Effects
Table 6 summarizes MCO differences for selected measures of knowledge(overall scale), attitudes(beliefs about practice burden, perceived treatment skill, and the proportion “very limited” by time or access to mental health resources), and of reported treatment behavior(proportion of providers “very likely” to prescribe antidepressant medication for depression scenario). When we sequentially controlled for the effects of provider demographics, general practice activities, and depression-specific activities, we found that the basic staff/group-model versus network-model MCO comparisons hold with minor changes in significance level. Therefore, we present averages and standard errors from our final regression models (Table 6) adjusted for provider and practice activities (general and depression-specific).
Table 6.
Predicted Means for Primary Care Provider Knowledge, Attitudes, and Behavior by Type of Managed Care Organization *
As in the univariate analyses, there was no MCO effect on knowledge. Although we observed a significant difference in perceived skill in univariate analysis, the effect did not hold after controlling for the other factors. However, even after controlling for provider and practice characteristics, MCO type still had a fairly large effect on beliefs about burden associated with treating depression with staff/group-model providers perceiving significantly more burden (10 points higher on 0–100 scale; p < .001) than network-model providers. In addition, staff/group-model providers were 26% more likely to view time limitations as a barrier to optimal care for depression (p < .01), but were 18% less likely to view limited access to mental health specialists as a barrier to care (p < .001) and 25% less likely to prescribe medications for treating depression (p < .001) compared with network-model providers. We report robust standard errors that correct for the nesting of providers within MCO but note that corrections were small because most of our independent variables varied among providers within the same practices and MCOs. We also analyzed our data following removal of providers from the VA and found identical results.
DISCUSSION
Using a broad two-group classification of MCOs consistent with the literature,12–22 we found that the type of MCO that a PCP works for influences provider attitudes and behavior relative to treating depression. However, type of MCO does not affect either knowledge, which is generally high as found in other work,32 or perceived skill. Disconcertingly, only one half to two thirds of the providers report any exposure at all to the AHCPR practice guidelines for the detection and treatment of depression in primary care settings. Compared with PCPs in network-model MCOs, PCPs in staff/group-model MCOs have stronger beliefs about burden, and perhaps as a result, are less likely to personally initiate care (medication). Primary care providers in staff/group-model MCOs instead rely on specialty care referral or assessment without treatment. Conversely, providers in network-model MCOs reported being more likely to initiate treatment themselves, perhaps because they perceive that patients will have poorer access to specialty mental health services. We also found significant differences in providers’ perceptions of skill, with staff/group-model MCO providers having 6% lower scores on our overall measure (14% for the medication skill item). However, these differences do not appear to be due to the organization as much as to the providers employed, because differences diminish after controlling for provider characteristics.
Among the possible explanations we proposed for differences between providers in staff/group-model compared with network-model MCOs, we find the most support for the idea that the two types of organizations direct resources in different areas. These staff/group-model MCO providers work within systems of care that have greater organizational integration and the opportunity to take advantage of a rich practice support structure—with greater ease of specialty referral. We found a clear and consistent picture in this regard, even after controlling for provider characteristics and practice activities. Those staff/group-model MCO providers who perceive time constraints as a major barrier to providing optimal care for their depressed patients tend to overcome such barriers by using readily available treatments that are less time-consuming, e.g., specialty referrals. Network-model MCO providers, in contrast, do not have the system supports available in staff/group-model MCOs. Instead, network-model MCO providers who report access to specialty care as a major barrier tend to initiate medication management themselves. These providers also reported spending 5 hours more per week in primary care although they see the same number of patients each week for comparable visit lengths, perhaps supporting the notion that they are personally providing more treatment for depression within the primary care setting.
These early results identify trade-offs faced by PCPs practicing in different types of MCOs within the U.S. health care delivery system when treating patients with depression in the primary care setting. Although we observed substantial differences in the style of providing care for depression, we cannot say anything about differences in the quality of care. In fact, quality may be equivalent in the two types of organizations despite the different styles providers use to treat patients with depression. It may be that as many patients are getting treated in both settings, with the largest difference being whether the care is delivered within the primary care setting or within mental health specialty. Further research is needed to explore the consequences of these trade-offs for guideline-concordant care and long-term patient outcomes, particularly because so few patients follow PCP recommendations to see a mental health professional.
This study has limitations. Enrolled plans, practices, and providers were not chosen to be representative, and may not reflect the universe of MCOs. Although the MCOs were not sampled to directly address organizational differences, they reflect a range of MCOs and permit comparisons of clinical processes of care that are rare in the literature. Patient populations may differ from plan to plan, practice to practice, clinician to clinician, and may shape provider practices, yet we have not adjusted our results based on patient case mix.22 We report on what clinicians say they do to assess behaviors, such as treatment choice; actual behavior may differ from reported behavior.28, 33 Organization differences we observed may reflect differences in clinical goals providers brought with them when they were hired,14, 34 but the similarity between staff/group-model and network-model MCO providers’ knowledge of depression treatment suggests that selection bias is not a major confound.
Despite these limitations, our findings suggest that staff/group-model MCO providers are more likely to initiate treatment for depression by referring a patient to mental health specialty care, while those in network-model MCOs are more likely to personally prescribe medication in the primary care setting. Given many similar demographic characteristics, we suspect that differences may be best explained by organizational factors. If this is the case, quality improvement for depression in primary care will require strategies that try to change provider behavior.35, 36
Whether or not a patient with depression receives quality care with good outcomes ultimately depends on factors that differ across MCOs. In staff/group-model MCOs, quality improvement efforts may focus on improving the PCP’s ability to detect depression and coordinate care with the specialty mental health sector or to have a mental health specialist available within the primary care setting. For network-model MCO providers, the most important factor may be to improve PCP knowledge of psychotherapy and proper use of antidepressants to better equip PCPs to personally deliver depression treatments. Besides more availability of low-cost but effective treatment options that providers can use within the primary care setting, community-based resources for educating and referring would help ensure that more patients receive treatment, particularly those who may not benefit solely from medication management.
Disseminating guidelines also would appear to be a fruitful strategy to increase quality depression treatment in network-model MCOs. It will be important to systematically evaluate various guideline implementation strategies (quality improvement teams, academic detailing) for their success in improving quality of care across varying types of network-model MCOs. The decentralized management structure in these MCOs will make it particularly difficult to establish expectations that care for depression will be consistent with guidelines. Given the referral orientation among the staff/group-model MCO providers, the key to improving appropriate care for depression may be to increase accountability for follow-up after referrals are made. Understanding the complex relationships between the type of MCO and different practice management styles revealed through PCP reports of depression-related knowledge, attitudes, and behaviors can and will continue to inform future research efforts to improve care for depression.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health (U01-MH54443, U01-MH54444, U01-MH50732, and P01-MH54623) and the Agency for Health Care Policy and Research (R01-HS08349).
The authors thank Christy Klein for assistance with tracking providers and preparing instrument documentation; Maureen Carney, MS, for help in recruiting PORT providers; Bob Bell, PhD, for statistical consultation; Jeff Smith for administering Dr. Rost’s study; Christine Nelson, RN, and Ray Turner, MD, MPH, for help with recruiting NYLCare providers; and Martha S. Gerrity, MD, PhD, for help with validating the knowledge measures. The authors acknowledge participating managed care organizations and participating primary care providers: Kaiser Permanente Medical Care Programs in Northern California Region, Oakland, Calif.; VA Medical Center, Sepulveda, Calif.; Ambulatory Sentinel Practice Network, Denver, Colo., a practice-based research network of family physicians that voluntarily participates in research; NYLCare Health Plans of the Mid-Atlantic, Greenbelt, Md.; Allina Medical Group, Twin Cities, Minn.; Columbia Medical Plan, Columbia, Md.; Humana Health Care Plans, San Antonio, Tex.; MedPartners, Los Angeles, Calif.; PacifiCare of Texas, San Antonio, Tex.; and Valley-Wide Health Services, Alamosa, Colo.
Appendix A
Clinician Knowledge About the Treatment of Depression*
References
- 1.Regier DA, Narrow WE, Rae DS, Manderschied RW, Locke BZ, Goodwin FK. The de facto U.S. mental and addictive disorder service system: epidemiologic catchment area prospective one-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993;50:85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, McGonagel KA, Shanzang Z, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Study. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 3.Schreter RK. Ten trends in managed care and their impact on the biopsychosocial model. Hosp Commun Psychiatry. 1993;44:325–7. doi: 10.1176/ps.44.4.325. [DOI] [PubMed] [Google Scholar]
- 4.Tunis SR, Hayward RSA, Wilson MC, et al. Internists’ attitudes about clinical practice guidelines. Ann Intern Med. 1994;120:956–63. doi: 10.7326/0003-4819-120-11-199406010-00008. [DOI] [PubMed] [Google Scholar]
- 5.Martin DP, Diehr P, Price KF, Richardson WC. Effect of a gatekeeper plan on health services use and charges: a randomized trial. Am J Public Health. 1989;79:1628–32. doi: 10.2105/ajph.79.12.1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kleinman LC, Boyd EA, Heritage JC. Adherence to prescribed explicit criteria during utilization review: an analysis of communications between attending and reviewing physicians. JAMA. 1997;278:497–501. [PubMed] [Google Scholar]
- 7.Kerr EA, Mittman ES, Hays RD, Siu AL, Leake B, Brook RH. Managed care and capitation in California: how do physicians at financial risk control their own utilization? Ann Intern Med. 1995;123:500–4. doi: 10.7326/0003-4819-123-7-199510010-00004. [DOI] [PubMed] [Google Scholar]
- 8.Goold SD, Hofer T, Zimmerman M, Hayward RA. Measuring physician attitudes toward cost, uncertainty, malpractice, and utilization review. J Gen Intern Med. 1994;333:544–9. doi: 10.1007/BF02599278. [DOI] [PubMed] [Google Scholar]
- 9.Emmons DW, Chawla AJ. Physician perceptions of the intrusiveness of utilization review. Stud Socioecon Environ Med. 1991:3–8. [Google Scholar]
- 10.Kerr EA, Mittman ES, Hays RD, Leake B, Brook RH. Quality assurance in capitated physician groups: where is the emphasis? JAMA. 1996;276:1236–9. [PubMed] [Google Scholar]
- 11.Landon BE, Wilson IB, Cleary PD. A conceptual model of the effects of health care organizations on the quality of medical care. JAMA. 1998;279:1377–82. doi: 10.1001/jama.279.17.1377. [DOI] [PubMed] [Google Scholar]
- 12.Wholey DR, Burns LR. Organizational transitions: form changes by health maintenance organizations. Res Sociol Organi. 1993;1:257–93. [Google Scholar]
- 13.Wholey DR, Feldman R, Christianson JB, Engberg J. Scale and scope economies among health maintenance organizations. J Health Econ. 1996;15:657–84. doi: 10.1016/s0167-6296(96)00499-7. [DOI] [PubMed] [Google Scholar]
- 14.Gold MR, Hurley R, Lake T, Enso T, Berenson R. A national survey of the arrangements managed-care plans make with physicians. N Engl J Med. 1995;333:1678–83. doi: 10.1056/NEJM199512213332505. [DOI] [PubMed] [Google Scholar]
- 15.Harris JS. Why doctors do what they do: determinants of physician behavior. J Occup Med. 1990;32:1207–20. doi: 10.1097/00043764-199012000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Gold M, Hurley R. The role of managed care “products” in managed care plans. Inquiry. 1997;34:29–37. [PubMed] [Google Scholar]
- 17.Wells KB, Hosek SD, Marquis SM. Effects of preferred provider options on use of outpatient mental health services by three employee groups. Med Care. 1992;30:412–27. doi: 10.1097/00005650-199205000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Felt-Lisk S. How HMOs structure primary care delivery. Managed Care Q. 1996;4:96–105. [PubMed] [Google Scholar]
- 19.Burns LR, Wholey DR. Differences in access and quality of care across HMO types. Health Serv Mgmt Res. 1991;4:32–45. doi: 10.1177/095148489100400105. [DOI] [PubMed] [Google Scholar]
- 20.Shenkin BN. The independent practice association in theory and practice: lessons from experience. JAMA. 1995;273:1937–44. [PubMed] [Google Scholar]
- 21.Shenkin BN. Models of managed care: the potential power of the IPA. Managed Care Q. 1996;4:68–74. [PubMed] [Google Scholar]
- 22.Rogers WH, Wells KB, Meredith LS, Sturm R, Burnam MA. Outcomes for adult depressed outpatients under prepaid and fee-for-service financing. Arch Gen Psychiatry. 1993;50:517–25. doi: 10.1001/archpsyc.1993.01820190019003. [DOI] [PubMed] [Google Scholar]
- 23.Retchin SM, Brown B. The quality of ambulatory care in medicare health maintenance organizations. Am J Public Health. 1990;80:411–5. doi: 10.2105/ajph.80.4.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnstone PM. A glimpse of an IPA as a living system. Behav Sci. 1995;40:304–13. doi: 10.1002/bs.3830400403. [DOI] [PubMed] [Google Scholar]
- 25.Depression Guideline Panel . Agency for Health Care Policy and Research Clinical Practice Guidelines: Depression in Primary Care. Rockville, Md: US Department of Health and Human Services; 1993. [Google Scholar]
- 26.Ashworth CD, Williamson P, Montano D. A scale to measure physician beliefs about psychosocial aspects of patient care. Soc Sci Med. 1984;19:1235–8. doi: 10.1016/0277-9536(84)90376-9. [DOI] [PubMed] [Google Scholar]
- 27.Main DS, Lutz LL, Barrett JE, Matthew J, Miller RS. The role of primary care clinician attitudes, beliefs, and training in the diagnosis and treatment of depression: a report from the Ambulatory Sentinel Practice Network Inc. Arch Fam Med. 1993;2:1061–6. doi: 10.1001/archfami.2.10.1061. [DOI] [PubMed] [Google Scholar]
- 28.Meredith LS, Wells KB, Kaplan S, Mazel RM. Counseling typically provided for depression: role of clinician specialty and payment system. Arch Gen Psychiatry. 1996;53:905–12. doi: 10.1001/archpsyc.1996.01830100053007. [DOI] [PubMed] [Google Scholar]
- 29.Rost K, Humphrey J, Kelleher K. Physician management preferences and barriers to care for rural patients with depression. Arch Fam Med. 1994;3:409–14. doi: 10.1001/archfami.3.5.409. [DOI] [PubMed] [Google Scholar]
- 30.Huber PJ. The behavior of maximum likelihood estimates under nonstandard conditions. Vol. 1. Berkeley, Calif: University of California; 1967. Fifth Berkeley Symposium on Mathematical Statistics and Probability; pp. 221–33. [Google Scholar]
- 31.Neuhous JM. Statistical methods for longitudinal and clustered designs with binary responses. In: Statistical Methods in Medical Research. 1992;1:249–73. doi: 10.1177/096228029200100303. [DOI] [PubMed] [Google Scholar]
- 32.Shao W-A, Williams JW, Lee S, Badgett RG, Aaronson B, Cornell JE. Knowledge and attitudes about depression among non-generalists and generalists. J Fam Pract. 1997;44:161–8. [PubMed] [Google Scholar]
- 33.Meredith LS, Wells KB, Camp P. Clinician specialty and treatment style for depressed outpatients in primary care with and without medical comorbidities. Arch Fam Med. 1994;3:1065–72. doi: 10.1001/archfami.3.12.1065. [DOI] [PubMed] [Google Scholar]
- 34.Veloski J, Barzansky B, Nash DB, Bastacky S, Stevens DP. Medical student education in managed care settings. JAMA. 1996;276:667–71. [PubMed] [Google Scholar]
- 35.Eisenberg JM, Williams SV. Cost containment and changing physicians’ practice behavior: can the fox learn to guard the chicken coop? JAMA. 1981;246:2195–201. [PubMed] [Google Scholar]
- 36.Greco PJ, Eisenberg JM. Changing physicians’ practices. N Engl J Med. 1993;329:1271–4. doi: 10.1056/NEJM199310213291714. [DOI] [PubMed] [Google Scholar]