Abstract
OBJECTIVE
To compare the effectiveness of two means for increasing the use of advance medical directives: written materials only versus written materials and an educational videotape.
DESIGN
Population-based, randomized controlled trial with 3-month follow up.
SETTING
Kaiser Permanente Colorado Region, a not-for-profit group-model health maintenance organization.
PARTICIPANTS
A population-based sample of all 1,302 members aged 75 years and older who used the Franklin Medical Office, excluding 55 persons who died or disenrolled during the study period or were identified by their physicians as blind or cognitively impaired.
INTERVENTIONS
All subjects were mailed a 10-page cartoon-illustrated educational pamphlet on patient choices, a selection of Colorado advance medical directive forms, and a guide to their completion; 619 subjects also were mailed a 20-minute videotape on advance directives. Both groups had access to a study nurse for assistance in completing and placing advance medical directives.
MEASUREMENTS AND MAIN RESULTS
The main outcome measure is the proportion of subjects who placed a directive in their medical record for the first time. Placement rates increased almost identically, from 21.2% to 35.0% in the written materials-only group and from 18.9% to 32.6% in the group receiving the videotape (95% confidence interval for difference −0.04, 0.04, p = .952).
CONCLUSIONS
In an elderly population with a substantial baseline placement rate, mailing of written materials substantially increased placement of an advance directive in the medical record, but the addition of a videotape did not. Mailing the video did increase the use of treatment trials and made patients more aware of reasons not to use advance directives.
Keywords: advance medical directives, aged, social marketing, end-of-life care, video
Many clinicians, managers, policy makers, ethicists, and researchers advocate increased completion and use of advance medical directives (AMDs), which include living wills and durable powers of attorney for health care (DPAHCs).1, 2 Most elderly Americans believe that they should complete a directive.3–7 Most have not, however.7, 8 Of those who have, many have not placed their directive in their medical record, where it would be readily available for clinical use.9–12
One potentially low-cost method to increase AMD completion is mass mailing of educational materials and forms. Rubin et al. achieved an 18.1% net increase in AMD completion using this approach, along with telephone access to assistance and additional information, in an unselected population of elderly HMO members, 94% of whom had not previously completed an AMD.13 The distribution of information by video offers another social marketing approach. The Foundation for Informed Medical Decision Making develops interactive videodisks and videotapes to help patients and physicians improve medical decision making in areas such as breast-cancer treatment, surgery for benign prostatic hyperplasia, and use of the prostate-specific antigen test.14 With support and collaboration from the Colorado Permanente Medical Group and the Veterans Administration Hospital in White River Junction, New Hampshire, the Foundation developed and is now marketing a videotape, entitled Peace of Mind: Advance Directives, that explains AMDs and encourages their use. We designed and implemented a population-based, randomized controlled trial that compared a mailing of written materials to a mailing that also included the Peace of Mind videotape. We hypothesized that the addition of the videotape would stimulate AMD completion more than written materials alone.
METHODS
Our study site was the Colorado Region of Kaiser Permanente, an established not-for-profit group-model HMO of 312,000 members. To focus on study subjects likely to be concerned about end-of-life choices, we used an administrative database to identify all 1,302 Kaiser Permanente members aged 75 years or older whose personal primary care physician practiced at the Franklin Medical Office. We limited the study to a single medical office for logistical reasons and used the Franklin Medical Office because it served the largest complement of elderly members. Before analyzing study results, we excluded 55 members who were withdrawn by their physicians because of blindness, illiteracy, or dementia; who moved out of the area, terminated HMO membership, or died before the end of the follow-up period; or whose medical record could not be located.
Interventions
We mailed a collection of printed materials and a cover letter signed by the HMO’s associate medical director (PB) to a randomly selected half of the study population (n = 628, after the exclusions described above). The printed materials included an educational pamphlet, You and Your Choices, published in 1994 by Choice in Dying, Inc.; a 6-page, 5-by-8-inch Colorado Advance Directive Guide, also published by Choice in Dying, Inc.; and Colorado-specific forms for the execution of a DPAHC, a living will, and a cardiopulmonary resuscitation directive.
To the remaining subjects (n= 619), we mailed the same collection of written materials described above but added the Peace of Mind: Advance Directives videotape. In this video, actual patients and family members describe their feelings and choices about advance directives and their experiences with fatal and nearly fatal illnesses, with and without advance directives. The video presents nine interviews. It opens with an extended interview of a man with respiratory disease who thought he should have had a DPAHC before his recent hospitalization. Had he completed one, however, he may not have survived his 3-month stay in the intensive care unit to do the interview. In another interview, the patient expresses the concern that “you don’t want to burn bridges” by being too restrictive with your directives. For the remainder of the interviews, most patients and family members express the belief that AMDs are beneficial in preventing family conflict and relieving the burden of decision making during times of emotional strain. The primary objective of the video is to increase subjects’ motivation to complete a directive by exposing them to the personal experiences of others.
Before mailing intervention materials to the videotape group, we wrote to tell them that they would soon receive an AMD videotape and asked them to return a stamped, self-addressed postcard if they did not want the videotape or if they needed to schedule an appointment with the study nurse to view it at the medical office. Thirty-one percent asked us not to send the videotape. We mailed the written materials to all subjects in the videotape group, regardless of their desire to receive the videotape. No data on VCR ownership were collected. Subjects in both groups were given the name and telephone number of the study nurse and told that she would answer AMD-related questions and help subjects place completed directives in their clinical record. Subjects in the video group were also told that the study nurse could assist them with viewing the video. No data on utilization of the study nurse were collected.
Follow-Up Questionnaire and Record Review
We mailed the videotapes and written materials in October 1994. Three months later we mailed a follow-up questionnaire to all subjects in both study groups. After a postcard reminder and a second letter plus questionnaire, we received completed questionnaires from 381 written-materials subjects and 354 videotape subjects, yielding response rates of 60.7% and 57.2%, respectively. The questionnaire, which we developed after reviewing instruments mentioned in the published literature, asked about reasons for not completing a DPAHC (among patients reporting not doing so), stages of thought and action toward completing a DPAHC, knowledge of facts and terms about DPAHCs, memory of and exposure to the intervention, and demographic characteristics.
After the 3-month follow-up period, we reviewed the consolidated Kaiser Permanente medical record for each subject to identify those whose records contained a new or old AMD and to ascertain its type, content, and dates of execution and placement.
Outcome Measures and Analytic Methods
Before initiating the intervention, we defined our primary outcome measure to be the proportion of study subjects without a previously executed AMD in their medical record who executed an AMD and placed it in their record within 3 months after the mailing of intervention materials. Our analysis was performed on an intent-to-treat basis, comparing the completion rates of the written-materials and videotape groups. Our sample size gave us 80% power to detect a 15% difference in completion rates (two-tailed test). We used χ2analysis to determine differences between the two groups on dichotomous data, and the Mann-Whitney U tests to analyze group differences on ordinal data.
RESULTS
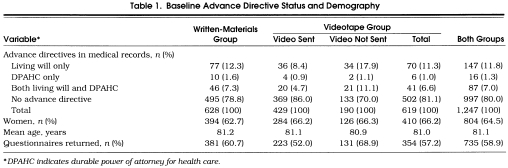
As shown in Table 1, randomization yielded two populations that were very similar in mean age (81.2 vs 81.0 years) and not significantly different in the proportion of members who were women (62.7% vs 66.2%). Of the final study population, 86% reported their ethnic background as white, 46% lived alone, and 41% had attended or graduated college. Twenty-one percent of the written-materials group had completed an AMD prior to the intervention, compared with 18.9% of the videotape group. The kinds of AMDs found at baseline in the medical records of each group were also very similar.
Table 1.
Baseline Advance Directive Status and Demography
Exposure to Intervention
Table 1 also shows that 190 (30.7%) of the 619 subjects in the videotape group asked us by postcard or telephone not to mail the videotape. These “decliners” were significantly more likely than others in the videotape group to have previously completed an AMD (30% vs 14%, p < .001) and more likely to return a completed follow-up questionnaire (66.3% vs 48.7%, p < .001). However, “decliners” and “accepters” were almost exactly similar in mean age, gender distribution, and—among questionnaire responders—racial background, living arrangements, and education.
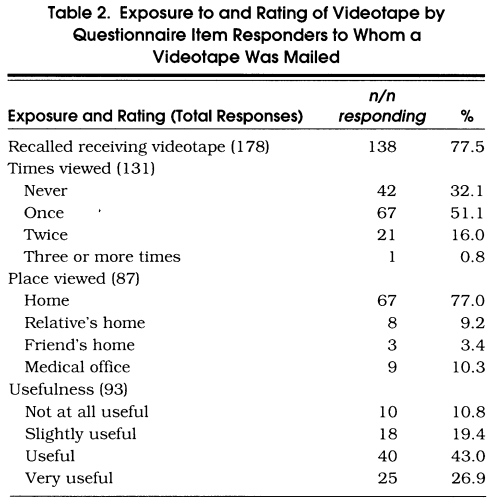
As shown in Table 2, among the questionnaire responders in the videotape group who were mailed the videotape and answered the questions, 77.5% recalled receiving the video and, of these, 67.9% reported that they viewed it at least once. Of the latter group, 77% said they viewed the tape at home. The remainder viewed it with relatives or, less frequently, with friends or in the medical office.
Table 2.
Exposure to and Rating of Videotape by Questionnaire Item Responders to Whom a Videotape Was Mailed
Among those who answered the questions, 78% of the videotape group and 71.1% of the written-materials group recalled receiving the printed materials. As detailed in Table 3, 91.5% of the written-materials group and 88.1% of the videotape group reported reading the written materials, and 54% of both groups reported reading them “with care.” About 70% of the subjects who recalled receiving the video or who reported reading the written materials said that these materials were “useful” or “very useful.”
Table 3.
Self-Reported Exposure to and Rating of Written Materials
Completion and Placement of Directives
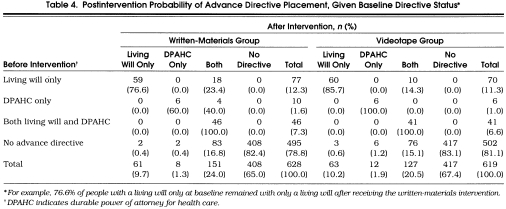
Table 4 describes the postintervention proportions of AMD placement by written-materials and videotape members, based on the types of AMDs placed in their medical records before the intervention. The overall proportion of members with AMD placements increased by 13.8 percentage points in the written-materials group and by 13.7 points in the videotape group, growth rates of 65.4% and 72.6%, respectively. By the end of the follow-up period, we found at least one AMD in the medical records of 33.8% of the study population, compared with 20.0% at baseline.
Table 4.
Postintervention Probability of Advance Directive Placement, Given Baseline Directive Status*
Self-reported rates of placement of DPAHCs “in my medical record” among questionnaire responders were also equal between the study arms, although more subjects reported placement than we could confirm from our records. Written-materials questionnaire responders self-reported 39.3% placement compared with 35.1% in the videotape group. Another 14.3% of questionnaire responders said that they had signed but not placed an AMD (16.9% videotape vs 12.0% written materials, p= .050). Thus, among questionnaire respondents in a posttest-only comparison, the videotape group self-reported slightly greater total DPAHC completion (but not placement) than the written-materials group. Even more subjects reported their desire to take some action. After our intervention, only 20% of questionnaire completers said they “haven’t thought about” executing a DPAHC. Of the remainder, 10% already thought they “should” complete a directive, 20% planned to or were “taking steps now,” and the rest had already completed one.
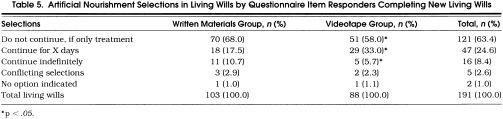
As detailed in Table 4, a substantial number of subjects who had previously placed an AMD completed and placed additional or updated directives. Overall, the rate of new AMD placement was about equal among persons who had previously placed an AMD and among those who had not. Nearly 20% of subjects who had previously placed only a living will added a DPAHC. Written-material members were more likely to do this than videotape members. Almost all subjects who completed a new living will answered a 3-response, closed-end question about tube feeding and parenteral nutrition that is part of this legislatively designed document in Colorado. As detailed in Table 5, among the subset submitting living wills, members in the videotape group were more likely to request a treatment trial of these interventions (p= .034).
Table 5.
Artificial Nourishment Selections in Living Wills by Questionnaire Item Responders Completing New Living Wills
Other Results
When asked to select up to 13 reasons why they did not complete a DPAHC, noncompleters in the videotape “accepter” group marked more reasons not to complete one than did videotape “decliners” (1.3 per person vs 1.0 per person, p= .058). Item-specific differences among the 13 reasons were not statistically significant.
DISCUSSION
The mailing of written materials only and the mailing of the videotape along with written materials each increased AMD placement substantially. These increases of nearly 14 percentage points are similar to the best results achieved from other single-contact interventions to induce health-related behaviors such as smoking cessation in unselected populations.15 They also compare favorably to the best results of other interventions to increase AMD completion.11, 13, 16, 17 Our study provides strong evidence that HMOs can use direct mail campaigns to increase AMD completion and placement rates among their elderly members.
Two years before our study began, most of our study subjects received a mailing of a booklet and AMD forms from the HMO to encourage AMD completion. Thus, one fifth had already completed and placed an AMD at baseline. Our results suggest that, as has been found for smoking cessation,15 repeated efforts to encourage AMD completion do not rapidly reach a plateau of diminishing marginal return. In the trial of Rubin et al., mailed printed materials increased DPAHC completion by about 14 percentage points over a base of 4.7%.13 Written materials in our study increased AMD completion by about 14 percentage points over a base of 20%. By the end of our study, self reports of questionnaire responders indicated that over 50% had executed a directive and another 7% were “taking steps now” to complete one.
The addition of the Peace of Mind videotape clearly did not add to the effect of written materials on medical record placement, our primary study outcome. The videotape intervention may have increased completion rates short of placement, as indicated by posttest-only self-reports from questionnaire responders. However, either the extra mailing (asking subjects if they wanted to decline receipt of the videotape) or the videotape itself might have stimulated this increase.
Because our design allowed subjects to decline the videotape in advance, and because about one third of those who received it said they did not play it, we estimate that only about half the videotape group actually viewed the tape. A larger percentage—about two thirds—of each group looked at the written materials, with about two thirds of these doing so “with care.” It does not appear that the addition of the videotape increased the likelihood of paying attention to written materials.
The results of our intent-to-treat analysis also suggest that videotape exposure influenced treatment preferences by increasing knowledge of AMDs and of the issues surrounding their use. Members of the videotape group who placed living wills were more likely to specify a treatment trial before the withdrawal of artificial nourishment. Videotape group members also identified more reasons not to complete an AMD.
We are uncertain about why videotape exposure did not increase AMD placement. It may be that videotapes have limited impact in an older population that is not video-oriented. Another reason may be that knowledge is not the rate-limiting factor in AMD completion among elders.18 Most elders think they should complete an AMD and even plan to do so. Like smokers who think they should quit cigarettes or alcoholics who would like to stop drinking, noncompleters may be stuck at a more advanced “stage of change” in which further general knowledge has little motivating effect.19 Nearly a third of our questionnaire completers who had not already completed an AMD thought they “should” complete one or were “taking steps now.”
If more than knowledge is needed, the availability—in both study arms—of a nurse to answer questions and receive and place directives in the medical record may have contributed substantially to the success of both arms. Our study nurse was frequently contacted. Other studies suggest that personal assistance promotes directive completion.17, 20 We recommend including a similar resource in future social marketing efforts, along with the provision of forms that subjects can fill out and return.
A second reason why videotape mailing did not increase placement may be that the value of AMDs becomes more unclear the more one knows about them. Dying instead of making an unexpected recovery is a genuine risk of AMD execution. So are the chances that your surrogate will make a poor decision, that your doctors will ignore or misinterpret your directive or surrogate, or that you will fail to anticipate—not know in advance your preferences about—the many possible medical conditions and interventions that could arise. Indeed, the growth in uncertainty and skepticism among patients who viewed the Peace of Mind videotape parallels the developing criticism of AMDs in the health services research literature.12, 21–29 If one’s objective is to enable patients to make better-informed decisions about AMDs, and not merely to increase completion rates, then inclusion of the videotape with written materials (or in other educational approaches) may well be appropriate.
For those who advocate increased use of AMDs, our results pose a paradox. Most advocates promote AMDs to increase self-determination and the likelihood that patients will get the end-of-life treatment that they want. Legally and philosophically, AMDs extend patients’ rights to informed consent.6 Our results suggest that as some patients come to know more about AMDs and the circumstances of their use, they are less convinced of their value. Many completed AMDs also seem internally inconsistent.13 Increased AMD completion rates may not always increase self-determination.
Strengths and Limitations
The greatest strength of our study is its population-based, randomized design, which allowed us to observe and experimentally attribute changes in AMD completion in an unselected population of elders who were not aware (until receiving the follow-up questionnaire) that their actions were being studied. Another strength is our ability to track actual medical record placement. Finally, our intervention used carefully designed, widely available products.
Two limitations imposed by our population-based randomized effectiveness design are the lack of baseline questionnaire responses from which to measure change and the lack of completed questionnaires from 41% of subjects. These weaknesses did not impinge on our ability to measure the primary study outcome, AMD completion and placement, but they do affect our ability to explain it.
A third limitation is the low rate of viewing in the videotape group. Of the 619 subjects randomized to the videotape mailing, only 429 actually were sent the video; of these, 223 returned a questionnaire; of these, 138 answered the questions about recalling the video and remembered receiving it in the mail, and 89 reported viewing it. The intent-to-treat design of our study assesses the impact of receiving a mailing that includes written materials and may include a videotape—it does not assess the impact of actually reading or viewing these materials.
Conclusions
We conducted a randomized controlled trial to compare the effectiveness of written materials alone versus written materials and a videotape for increasing the placement of AMDs. We found that rates of placement of AMDs into the medical record were nearly identical for the two groups, indicating that the addition of a videotape did not increase placement. Subjects in the videotape group, however, did increase their selection of treatment trials in living wills, and the videotape likely made them more aware of reasons not to use AMDs. We conclude that managers should not incur the extra expense of the Peace of Mind videotape when launching a direct mail campaign solely to increase AMD completion rates among the elderly.
Acknowledgments
The authors acknowledge the valuable and effective support of Mary O’Neill Kershner, RNC, who served as study nurse and medical record abstractor, Leo Ablicki, RPh, and James Bavry, PhD, who performed data analyses.
This study was supported by a grant from Kaiser Permanente’s Sidney Garfield Memorial Fund.
References
- 1.Emanuel LL, Emanuel EJ. The medical directive: a new comprehensive advance care document. JAMA. 1989;261:3288–93. doi: 10.1001/jama.261.22.3288. [DOI] [PubMed] [Google Scholar]
- 2.Schneiderman LJ, Arras JD. Counseling patients to counsel physicians on future care in the event of patient incompetence. Ann Intern Med. 1985;102:693–8. doi: 10.7326/0003-4819-102-5-693. [DOI] [PubMed] [Google Scholar]
- 3.American Diabetes Association. Screening for diabetes: position statement. Diabetes Care. 1989;12:588–90. [Google Scholar]
- 4.Cohen-Mansfield J, Rabinovich BA, Lipson S, et al. The decision to execute a durable power of attorney for health care and preferences regarding the utilization of life-sustaining treatments in nursing home residents. Arch Intern Med. 1991;151:289–94. [PubMed] [Google Scholar]
- 5.Eddy DM. A piece of my mind: a conversation with my mother. JAMA. 1994;272:179–81. [PubMed] [Google Scholar]
- 6.Emanuel LL, Barry MJ, Stoeckle JD, Ettelson LM, Emanuel EJ. Advance directives for medical care—a case for greater use. N Engl J Med. 1991;324:889–95. doi: 10.1056/NEJM199103283241305. [DOI] [PubMed] [Google Scholar]
- 7.Gamble ER, McDonald PJ, Lichstein PR. Knowledge, attitudes, and behavior of elderly persons regarding living wills. Arch Intern Med. 1991;151:277–80. [PubMed] [Google Scholar]
- 8.Stelter KL, Elliott BA, Bruno CA. Living will completion in older adults. Arch Intern Med. 1992;152:954–9. [PubMed] [Google Scholar]
- 9.Morrison RS, Olson E, Metz KR, Meier DE. The inaccessibility of advance directives on transfer from ambulatory to acute care settings. JAMA. 1995;274:478–82. [PubMed] [Google Scholar]
- 10.Roe JM, Goldstein MK, Massey K, Pascoe D. Durable power of attorney for health care. Arch Intern Med. 1992;152:292–6. [PubMed] [Google Scholar]
- 11.Sachs GA, Stocking CB, Miles SH. Empowerment of the older patient: a randomized, controlled trial to increase discussion and use of advance directives. J Am Geriatr Soc. 1992;40:269–73. doi: 10.1111/j.1532-5415.1992.tb02081.x. [DOI] [PubMed] [Google Scholar]
- 12.Teno JM, Lynn J, Phillips RS, et al. Do formal advance directives affect resuscitation decisions and the use of resources for seriously ill patients? J Clin Ethics. 1994;5:23–30. [PubMed] [Google Scholar]
- 13.Rubin SM, Strull WM, Fialkow MF, Weiss SJ, Lo B. Increasing the completion of the durable power of attorney for health care: a randomized controlled trial. JAMA. 1994;271:209–12. [PubMed] [Google Scholar]
- 14.Kasper JF, Mulley AG, Jr, Wennberg JE. Developing shared decision making programs to improve the quality of health care. Qual Rev Bull. 1992;18:183–9. doi: 10.1016/s0097-5990(16)30531-0. [DOI] [PubMed] [Google Scholar]
- 15.Lichtenstein E, Hollis JF, Severson HH, et al. Tobacco cessation interventions in health care settings: rationale, model, outcomes. Addict Behav. 1996;21:709–20. doi: 10.1016/0306-4603(96)00030-5. [DOI] [PubMed] [Google Scholar]
- 16.Hare J, Nelson C. Will outpatients complete living wills: a comparison of two interventions. J Gen Intern Med. 1991;6:41–6. doi: 10.1007/BF02599390. [DOI] [PubMed] [Google Scholar]
- 17.High DM. Advance directives and the elderly: a study of intervention strategies to increase use. Gerontologist. 1993;33:342–9. doi: 10.1093/geront/33.3.342. [DOI] [PubMed] [Google Scholar]
- 18.Moore KA, Danks JH, Ditto PH, Druley JA, Townsend A, Smucker WD. Patient understanding of a physician-initiated advance directive discussion. Arch Fam Med. 1994;3:1057–63. doi: 10.1001/archfami.3.12.1057. [DOI] [PubMed] [Google Scholar]
- 19.DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, Rossi JS. The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. J Consult Clin Psychol. 1991;59:295–304. doi: 10.1037//0022-006x.59.2.295. [DOI] [PubMed] [Google Scholar]
- 20.Haisfield M, McGuire D, Krumm S, Shore AD, Zabora J, Rubin HR. Patients’ and healthcare providers’ opinions regarding advance directives. Oncol Nurs Forum. 1994;21:1179–87. [PubMed] [Google Scholar]
- 21.Kapp MB. Medical empowerment of the elderly. Hastings Cent Rep. 1989;7:5–7. [PubMed] [Google Scholar]
- 22.Menikoff JA, Sachs GA, Siegler M. Beyond advance directives—health care surrogate laws. N Engl J Med. 1992;327:1165–9. doi: 10.1056/NEJM199210153271612. See comments. [DOI] [PubMed] [Google Scholar]
- 23.Peterson LM. Advance directives, proxies, and the practice of surgery. Am J Surg. 1992;163:277–81. doi: 10.1016/0002-9610(92)90001-8. [DOI] [PubMed] [Google Scholar]
- 24.Schneiderman LJ, Kronick R, Kaplan RM, Anderson JP, Langer RD. Effects of offering advance directives on medical treatments and costs. Ann Intern Med. 1992;117:599–606. doi: 10.7326/0003-4819-117-7-599. [DOI] [PubMed] [Google Scholar]
- 25.Schneiderman LJ, Pearlman RA, Kaplan RM, Anderson JP, Rosenberg EM. Relationship of general advance directive instructions to specific life-sustaining treatment preferences in patients with serious illness. Arch Intern Med. 1992;152:2114–22. [PubMed] [Google Scholar]
- 26.Sehgal A, Galbraith A, Chesney M, Schoenfeld P, Charles G, Lo B. How strictly do dialysis patients want their advance directives followed? JAMA. 1992;267:59–63. [PubMed] [Google Scholar]
- 27.Teno JM, Nelson HL, Lynn J. Advance care planning: priorities for ethical and empirical research. Hastings Cent Rep. 1994;24:S32–6. [PubMed] [Google Scholar]
- 28.Virmani J, Schneiderman LJ, Kaplan RM. Relationship of advance directives to physician–patient communication. Arch Intern Med. 1994;154:909–13. [PubMed] [Google Scholar]
- 29.Wolf SM, Boyle P, Callahan D, et al. Sources of concern about the Patient Self Determination Act. N Engl J Med. 1991;325:1666–71. doi: 10.1056/nejm199112053252334. Special Report. [DOI] [PubMed] [Google Scholar]