Abstract
OBJECTIVE
To compare the number of preoperative tests ordered for elective ambulatory surgery patients during the 2 years before and the 2 years after the establishment of new hospital testing guidelines.
MEASUREMENTS
The patterns of preoperative testing by surgeons and a medical consultant during the 2 years before and the 2 years after the establishment of new guidelines at one orthopedic hospital were reviewed. All tests ordered preoperatively were determined by review of medical records. Preoperative medical histories, physical examinations, and comorbidities were obtained according to a protocol by the medical consultant (author). Perioperative complications were determined by review of intraoperative and postoperative events, which also were recorded according to a protocol.
MAIN RESULTS
A total of 640 patients were enrolled, 361 before and 279 after the new guidelines. The mean number of tests decreased from 8.0 before to 5.6 after the new guidelines (p = .0001) and the percentage decrease for individual tests varied from 23% to 44%. Except for patients with more comorbidity and patients receiving general anesthesia, there were decreases across all patient groups. In multivariate analyses only time of surgery (before or after new guidelines), age, and type of surgery remained statistically significant (p = .0001 for all comparisons). Despite decreases in surgeons’ ordering of tests, the medical consultant did not order more tests after the new guidelines (p = .60) The majority of patients had no untoward events intraoperatively and postoperatively throughout the study period, with only 6% overall requiring admission to the hospital after surgery, mainly for reasons not related to abnormal tests. Savings from charges totaled $34,000 for the patients in the study.
CONCLUSIONS
Although there was variable compliance among physicians, new hospital guidelines were effective in reducing preoperative testing and did not result in increases in untoward perioperative events or in test ordering by the medical consultant.
Keywords: preoperative procedures, testing, guidelines, consultation
Preoperative tests are obtained to detect unsuspected conditions that may alter assessment of surgical and anesthetic risks and to obtain baseline values that may help in decision making perioperatively and postoperatively.1–5 Ideally, these tests should be ordered after a medical history and physical examination have been performed.1, 3, 4, 6–9 In practice, however, these tests are usually ordered by surgeons according to preoperative testing guidelines (“routine preop tests”) that have been established at the hospital.4, 10
Traditionally, routine preoperative tests have included a panel of blood and urine tests, as well as an electrocardiogram and a chest radiograph.1, 5, 11 Current knowledge, however, indicates that the incidence of unanticipated test abnormalities that alter management is too low to warrant such extensive testing on all surgical patients.1–3, 10, 12–15 In addition, the desire to decrease costs has led many hospitals to change their preoperative testing guidelines.2, 13
On August 1, 1993, the Hospital for Special Surgery officially changed its preoperative testing guidelines. The objective of this study was to compare the number and types of preoperative tests ordered for patients undergoing elective ambulatory surgery the 2 years before and the 2 years after the establishment of the new hospital testing guidelines.
METHODS
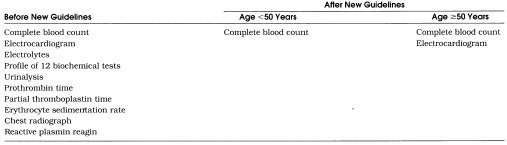
On August 1, 1993, the Hospital for Special Surgery (specializing in orthopedic surgery) implemented new Minimum Preoperative Testing Requirements to contain costs. The new requirements were decided on by an appointed committee and approved by the Departments of Medicine, Anesthesiology, Radiology, Pediatrics, Laboratory, and Orthopedics. Prior to August 1, 1993, a full battery of tests including blood, urine, electrocardiogram, and chest radiographic evaluations were routinely ordered on all patients. The new guidelines, outlined in Table 1), were established according to the patient’s age and the type or extent of surgery, and mostly affected elective ambulatory (outpatient) surgery patients. The new guidelines were sent to all physicians in a memorandum. Orthopedists were informed that these were minimal requirements only and they could order further tests as necessary. Orthopedists were also free to refer patients to an internist or pediatrician (medical consultant) for preoperative medical evaluations. According to standard practice, orthopedists typically order preoperative tests and simultaneously refer patients to a medical consultant before reviewing the test results. The medical consultant also could order any other preoperative tests necessary.
Table 1.
Recommended Preoperative Tests Before and After the New Guidelines
At the Hospital for Special Surgery orthopedists are specialized according to surgical subtype, and for ambulatory patients these subtypes correspond to foot/ankle surgery, hip/knee surgery, hand/wrist surgery, and shoulder/sports surgery.
This study reports on the preoperative testing and outcome of all orthopedic patients undergoing ambulatory surgery who were referred to a single medical consultant (the author) during the 2 years before and the 2 years after the new guidelines (from August 1, 1991, through December 31, 1995). This study is a retrospective review of preoperative, intraoperative, and postoperative information that was obtained and recorded according to a set protocol for all patients. Comorbidities were also obtained according to a set protocol and included calculation of the Charlson Comorbidity Index.16 The Charlson Comorbidity Index is a weighted index that provides a comprehensive assessment of multiple diseases and disease severity, and evaluates the longitudinal risk of mortality attributed to comorbid disease. It has been extensively tested with perioperative patients and has been used in clinical outcomes studies.17, 18 Scores on the Charlson Comorbidity Index are reported from 0 to ≥3, with higher scores indicating more comorbidity. At the time of the medical evaluation, the medical consultant was aware of which tests had been ordered by the surgeons, although in most cases the results of these tests were not yet available. The medical consultant ordered any further tests considered necessary.
Type of anesthesia was categorized as general, regional (epidural, spinal, combined spinal and epidural, interscalene, axillary, ankle, or femoral nerve), or local. An anesthesiologist was present in the operating room for all patients. Postoperatively all patients received standardized recovery room care, which included electrocardiographic monitoring, oxygen saturation measurement, vital sign measurement, as well as measurements of certain surgical and anesthetic variables. In order to be discharged from the recovery room, patients had to attain specific milestones, which were no intraoperative complications, return of vital signs to within 20% of preanesthesia levels, ability to take fluids orally, ability to urinate, ability to ambulate, fully awake consciousness, adequate analgesia, no wound drainage, and absence of nausea and vomiting.19 If these criteria were not fulfilled, patients were admitted to the hospital and followed in-hospital by surgeons and the medical consultant. All discharged patients received a telephone call 24 to 48 hours after surgery by a designated ambulatory surgery nurse to screen for postoperative complications. Telephone calls followed a set protocol and included questions about the operative wound, ability to move the affected extremity, medication use, degree of pain, other symptoms such as nausea, vomiting, difficulty urinating, fever, other pains, and plans for follow-up. Any positive findings were noted and referred to the surgeons and anesthesiologists, who then decided whether to ask the patient to return to the hospital for evaluation and possible admission.
Means and standard deviations were calculated for continuous variables, such as age and total laboratory tests ordered. Frequencies were calculated for all ordinal variables, such as the Charlson Comorbidity Index. Responses were compared by the Student’s t test and χ2tests. Variables that were statistically significant at the p≤ .05 level were entered into multivariate analyses with total laboratory tests as the dependent variable. All statistical analyses were performed with SAS statistical software (SAS Institute, Cary, NC).
Institutional Review Board approval was obtained for this study.
RESULTS
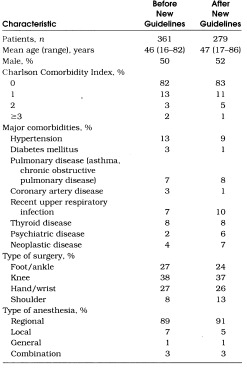
A total of 640 patients were included in this study, representing 5% of the total ambulatory surgery patients at the Hospital for Special Surgery during the 2 years before and the 2 years after the new guidelines. Characteristics of patients in the before and after groups are listed in Table 2. Patient groups did not differ significantly from each other in any of these characteristics. Also, there were no differences in the percentages of younger and older patients according to type of surgery between the before and after groups.
Table 2.
Comparison of Patients Before and After New Guidelines
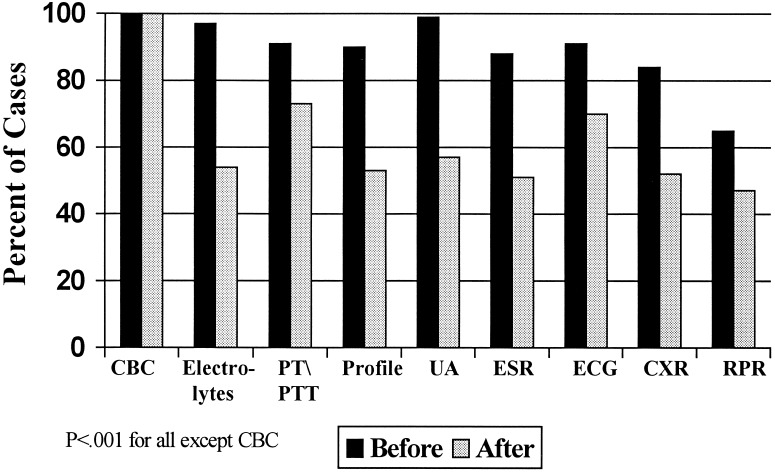
Shown in Figure 1 are the tests ordered by surgeons before and after the new guidelines according to percentage of cases. As expected, the rate of ordering complete blood count did not change. For all other tests, however, there was a significant decrease in the percentage of tests ordered after the new guidelines (p < .001). Before the guidelines, more than 80% of patients had eight or nine preoperative tests; after the new guidelines, only 48% had eight or nine tests.
Figure 1.
Types of tests ordered by surgeons according to percentage of cases before and after new guidelines. CBC indicates complete blood count; PT, prothrombin time; PTT, partial thromboplastin time; Profile, panel of 12 biochemical tests; UA, urinalysis; ESR, erythrocyte sedimentation rate; ECG, electrocardiogram; CXR, chest radiograph; RPR, reactive plasmin reagin.
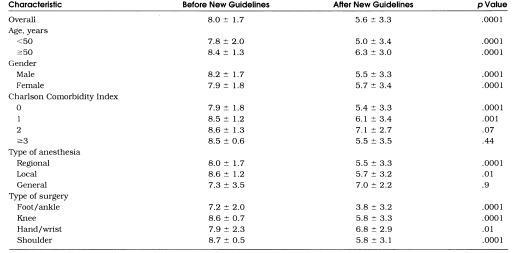
Overall, a mean ± SD of 8.0 ± 1.7 tests were ordered before and a mean ± SD of 5.6 ± 3.3 tests were ordered after the new guidelines, a decrease of 30% (Table 3 By simple univariate analyses, decreases in test ordering were found for all patient groups according to age, gender, and type of surgery. Decreases were also found for patients with lower comorbidity scores (0–1). Decreases were not found for those with more comorbidity (2–3); however, there were few patients in these categories. Except for general anesthesia, decreases in test ordering were also noted according to most types of anesthesia. By multivariate analyses, only time of surgery (before or after new guidelines), age, and type of surgery were statistically significant (p= .0001 for all comparisons). There was a strong association between comorbidity and age (p < .0001), and therefore comorbidity did not remain statistically significant in the multivariate analyses.
Table 3.
Mean Number of Tests (±SD) Ordered by Surgeons Before and After New Guidelines According to Selected Patient Characteristics
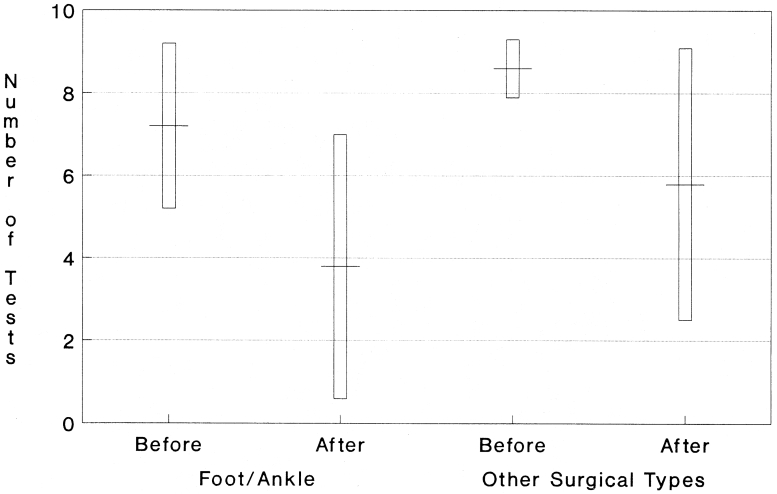
Rates of decrease in test ordering varied depending on surgical type. Although the different surgical specialists ordered similar numbers of tests before the new guidelines, the foot/ankle surgeons ordered fewer tests after the new guidelines compared with other surgeons (p= .007), as shown in Figure 2. The rate of decrease in test ordering was greater for younger patients than for older patients, but this was less statistically significant (p= .05).
Figure 2.
Mean number of tests ordered before and after new guidelines for foot/ankle surgeons versus other orthopedic surgeons.
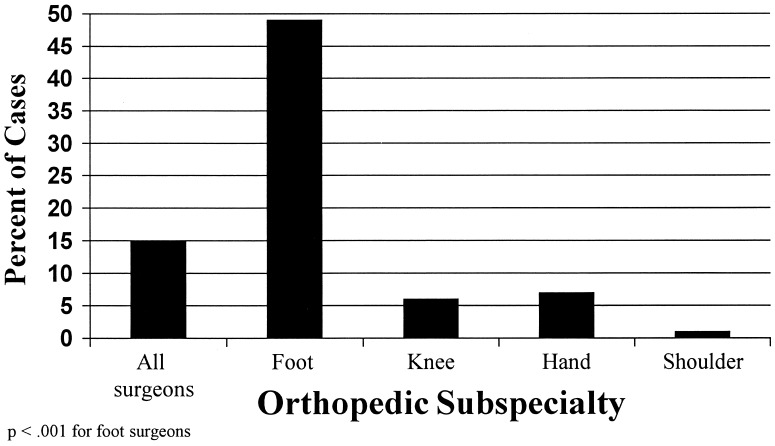
Shown in Figure 3 is the percentage of cases in which the guidelines were followed exactly. In only 15% of cases overall did surgeons follow the new guidelines exactly. There were no significant differences when stratified by age; guidelines were followed exactly in 17% of patients less than 50 years old and in 14% of patients at least 50 years old. There were differences, however, according to type of surgery, with foot/ankle surgeons following the guidelines in 49% of cases. Foot/ankle surgeons also tended to follow the guidelines more often with younger patients, 59%, than with older patients, 35% (p= .05). Such a trend was not found for the other surgical types.
Figure 3.
Percentage of cases in which tests were ordered exactly according to new guidelines versus orthopedic specialty.
Additional Tests Ordered by the Medical Consultant
The medical consultant ordered additional tests for 10% of patients before and for 9% of patients after the new guidelines (p= .60). Before the new guidelines, the majority of additional tests ordered by the medical consultant were in response to already obtained abnormal laboratory results (for example, repeating abnormal coagulation tests). After the new guidelines, additional tests were also ordered for these same reasons; however, first-time electrocardiograms composed over 30% of additional tests, mainly in patients under 50 years of age.
Pregnancy testing was not included in the new or old guidelines. Throughout the study period all women of childbearing age were asked about the possibility of pregnancy, and the medical consultant ordered pregnancy tests for those women who stated they might be pregnant. In total, pregnancy tests were ordered in 3% of women of childbearing age before the new guidelines, and in 2% after the new guidelines.
The medical consultant recommended postponing surgery in 2% of patients before and in 1% of patients after the new guidelines, for a total of 11 patients. For 5 patients surgery was postponed because of abnormal laboratory findings, specifically new anemia, new inverted T waves on electrocardiogram, new low calcium level, new fasting blood glucose of 360, and new atrial fibrillation at a rate of 60. For the remaining 6 patients, surgery was postponed for nonlaboratory findings, specifically rash, breast mass (which was subsequently diagnosed as a malignant neoplasm), palpitations with shortness of breath, current high aspirin use, recent onset of neurologic symptoms, and reduced exercise tolerance with a known history of cardiac disease.
The majority of patients (94%) had no untoward events intraoperatively and postoperatively and fulfilled recovery room discharge criteria. There were no significant differences in the percentage of patients admitted before the new guidelines, 5%, and after the new guidelines, 7% (p= .25). The main reason for admission in both groups was pain management after surgery that was more extensive than originally planned, for example, conversion of an arthroscopy to an open procedure. Rates of admission were not different based on medical comorbidity. There were no admissions for medical reasons in the group after the new guidelines. There was one admission for medical reasons in the group before the new guidelines, specifically for a patient with a known insulinoma who developed confusion in the recovery room.
Savings
Except for complete blood count, there were decreases of 23% to 44% in ordering preoperative tests. These decreases corresponded to a charge reduction of approximately $34,000. The patients included in this study represented 5% of the total ambulatory surgery patients during this time period. By extrapolation, the new guidelines resulted in a total charge reduction of over $650,000 during the first 2 years for ambulatory surgery patients.
DISCUSSION
Numerous investigators of preoperative testing have shown that the incidence of finding unsuspected abnormalities that adversely affect surgical outcome is low, and therefore nonselective routine testing with a large battery of tests is not justified.1–3, 10, 12–15, 20 Some researchers have proposed guidelines based on age, gender, known comorbidity, medications, and extent of surgery, 4–6, 21–23 and estimate that testing can be reduced by 60%.2, 3, 6, 7, 9, 20 In addition, special centers specifically dedicated to preoperative evaluation have been set up at various institutions and have been found to be very effective, for example, in decreasing testing by 55% and in decreasing by nearly 88% day-of-surgery cancellations.24 Some centers have used automated preoperative assessment tools to query patients about symptoms related to major medical comorbidities. These automated systems generate lists of suggested preoperative tests and have been found to vary in usefulness depending on the center.25, 26
In this study we found testing decreases from 23% to 44% for various preoperative tests after new institutional guidelines were recommended. Although decreases were not uniform across all surgeon groups, trends toward ordering fewer tests were seen among most surgeons. Given that the guidelines were followed exactly in only 15% of cases, there is great potential for further charge reductions. Similar to other reports, our decrease in testing did not result in an increase in untoward events in the intraoperative and immediate postoperative periods.10, 12, 20, 21 In addition, our study showed that surgeons responded quickly to the new institutional guidelines even though these guidelines were announced in a simple memorandum and were not specifically emphasized by other methods. Some researchers have shown greater success in getting physicians to order fewer tests through administrative interventions, rather than through physician education.7, 27, 28
In this study we noted variations in test-ordering patterns among the different specialty surgeons. Specifically, foot/ankle surgeons ordered significantly fewer tests than their surgical colleagues. This difference was not related to patient characteristics, anesthesia type, or complexity of surgery. On close inspection, this difference seemed to be more related to habit and the practice styles of a few high-volume foot/ankle surgeons.
In a 1994 retrospective study in Canada of more than 900 patients, other researchers also found a reduction in test ordering after new hospital guidelines were introduced.13 This study included both minor and major surgeries. No untoward perioperative events were attributed to the new guidelines. Although various reinforcements regarding the new guidelines were given in the Canadian study (grand rounds, postings), the reduction in test ordering was only 10% compared with the 30% reduction in our study. This difference may be attributed to the fact that the Canadian study also included major surgeries. In the Canadian study junior staff adhered to the guidelines more closely than senior staff.
Another study by Nardella and colleagues compared test-ordering patterns before and after new guidelines for various surgeries and found the average number of tests decreased from 9.6 per patient to 4.7 per patient (49%).23 Their study also assessed the appropriateness of tests and stressed that guidelines must be established according to rigorous criteria to ensure that all indicated tests are performed. Unique to Nardella’s study, however, was that surgeons signed a written agreement to allow nurse practitioners and anesthesiologists to order all preoperative tests, a policy that could be difficult to implement widely.
In our study we found that despite decreases in testing by surgeons after the new guidelines, there was no increase in overall testing by the medical consultant. Repeating abnormal tests comprised the bulk of testing by the medical consultant both before and after the guidelines. However, after the new guidelines the consultant ordered more electrocardiograms on younger patients. These electrocardiograms were medically indicated and ideally should have been ordered by the surgeons. Interestingly, one retrospective study of preoperative testing in more than 2,000 patients showed a decrease of 17% in ordering unindicated tests, but also a decrease of 10% in ordering indicated tests, raising concern about the appropriateness of tests ordered.2
This study is limited in that it included only adult patients referred to a medical consultant and therefore may be biased toward those patients with the greatest comorbidity and testing requirements. Also this study focused only on patients undergoing elective ambulatory orthopedic surgery. The impact of new testing guidelines may be different in patients undergoing major surgery, emergency surgery, or nonorthopedic surgery. Also, although patients received a follow-up telephone call within 48 hours after surgery, patients were not followed several days postoperatively to monitor for subsequent complications. In addition, this study did not assess the role of previous recent laboratory tests as substitutes for preoperative tests, which have been shown not to vary significantly with preoperative tests.1, 7
In summary, our results show that a simple memorandum announcing a change in preoperative testing guidelines as part of the hospital’s cost containment strategy was effective. Although compliance varied among surgeons, testing decreased overall by 30% in ambulatory surgery patients. Decreases in testing were noted despite the fact that these guidelines were not discussed with surgeons or reinforced, and feedback to surgeons was not provided regarding individual test-ordering patterns. The decrease in surgeons’ test ordering did not result in the medical consultant ordering more tests and did not result in an increase in intraoperative and immediate postoperative adverse effects. In addition, further substantial cost reductions are possible if tests are ordered according to guidelines recommended by expert panels and rule-based systems.
Acknowledgments
This work was supported in part by the Hospital for Special Surgery Multipurpose Arthritis and Musculoskeletal Disease Center (NIH P60 AR38520-06).
References
- 1.Macpherson DS. Preoperative laboratory testing: should any tests be “routine” before surgery? Med Clinic North Am. 1993;77:289–308. doi: 10.1016/s0025-7125(16)30252-8. [DOI] [PubMed] [Google Scholar]
- 2.Macario A, Roizen MF, Thisted RA, Kim S, Orkin FK, Phelps C. Reassessment of preoperative laboratory testing has changed the test-ordering patterns of physicians. Surg Gynecol Obstet. 1992;175:539–47. [PubMed] [Google Scholar]
- 3.Perez A, Planell J, Bacardaz C, et al. Value of routine preoperative tests: a multicentre study in four general hospitals. Br J Anaesth. 1995;74:250–6. doi: 10.1093/bja/74.3.250. [DOI] [PubMed] [Google Scholar]
- 4.Roizen MF. Preoperative evaluation. In: Miller RD, editor. Anesthesia. New York, NY: Churchill Livingstone Inc.; 1990. [Google Scholar]
- 5.Velanovich V. Preoperative laboratory screening based on age, gender, and concomitant medical diseases. Surgery. 1994;115:56–61. [PubMed] [Google Scholar]
- 6.Roizen MF. Cost-effective preoperative laboratory testing. JAMA. 1994;271:319–20. doi: 10.1001/jama.271.4.319a. [DOI] [PubMed] [Google Scholar]
- 7.Macpherson DS, Snow R, Lofgren RP. Preoperative screening: value of previous tests. Ann Intern Med. 1990;113:969–73. doi: 10.7326/0003-4819-113-12-969. [DOI] [PubMed] [Google Scholar]
- 8.Robbins JA, Mushlin AI. Preoperative evaluation of the healthy patient. Med Clin North Am. 1979;63:1145–56. doi: 10.1016/s0025-7125(16)31632-7. [DOI] [PubMed] [Google Scholar]
- 9.Roizen MF. The compelling rationale for less preoperative testing. Can J Anaesth. 1988;35:214–8. doi: 10.1007/BF03010614. [DOI] [PubMed] [Google Scholar]
- 10.Johnson H, Knee-Ioli S, Butler TA, Munoz E, Wise L. Are routine preoperative laboratory screening tests necessary to evaluate ambulatory surgical patients? Surgery. 1988;104:639–45. [PubMed] [Google Scholar]
- 11.Jones T, Isaacson JH. Preoperative screening: what tests are necessary? Cleve Clin J Med. 1995;62:374–8. doi: 10.3949/ccjm.62.6.374. [DOI] [PubMed] [Google Scholar]
- 12.Turnbull JM, Buck C. The value of preoperative screening investigations in otherwise healthy individuals. Arch Intern Med. 1987;147:1101–5. [PubMed] [Google Scholar]
- 13.Larocque BJ, Maykut RJ. Implementation of guidelines for preoperative laboratory investigations in patients scheduled to undergo elective surgery. Can J Surg. 1994;37:397–401. [PubMed] [Google Scholar]
- 14.Roberts CJ, Fowkes FGR, Ennis WP, Mitchell M. Possible impact of audit on chest X-ray requests from surgical wards. Lancet. 1983;2:446–8. doi: 10.1016/s0140-6736(83)90403-8. [DOI] [PubMed] [Google Scholar]
- 15.Wattsman TA, Davies RS. The utility of preoperative laboratory testing in general surgery patients for outpatient procedures. Am Surg. 1997;63:81–90. [PubMed] [Google Scholar]
- 16.Charlson ME, Ales KA, Pompei P, MacKenzie CR. A new method of classification of prognositc comorbidity for longitudinal studies: development and validation. J Chron Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 17.Charlson ME, Peterson J, Szatrowski T, MacKenzie C, Gold J. Long-term prognosis after peri-operative cardiac complications. J Clin Epidemiol. 1994;47:1389–400. doi: 10.1016/0895-4356(94)90083-3. [DOI] [PubMed] [Google Scholar]
- 18.Charlson ME, MacKenzie C, Gold J. Preoperative autonomic function abnormalities in patients with diabetes mellitus and patients with hypertension. J Am Coll Surg. 1994;179:1–10. [PubMed] [Google Scholar]
- 19.Urmey WF, Stanton J, Peterson M, Sharrock NE. Combined spinal-epidural anesthesia for outpatient surgery. Anesthesiology. 1995;83:528–34. doi: 10.1097/00000542-199509000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Kaplan EB, Sheiner LB, Boeckmann AJ, et al. The usefulness of preoperative laboratory screening. JAMA. 1985;253:3576–81. [PubMed] [Google Scholar]
- 21.Blery C, Charpak Y, Szatan M, et al. Evaluation of a protocol for selective ordering of preoperative tests. Lancet. 1986;1:139–41. doi: 10.1016/s0140-6736(86)92271-3. [DOI] [PubMed] [Google Scholar]
- 22.Vogt AW, Henson LC. Unindicated preoperative testing: ASA physical status and financial implications. J Clin Anesth. 1997;9:437–41. doi: 10.1016/s0952-8180(97)00060-3. [DOI] [PubMed] [Google Scholar]
- 23.Nardella A, Pechet L, Snyder M. Continuous improvement, quality control, and cost containment in clinical laboratory testing. Arch Pathol Lab Med. 1995;119:518–22. [PubMed] [Google Scholar]
- 24.Fischer S. Development and effectiveness of an anesthesia preoperative evaluation clinic in a teaching hospital. Anesthesiology. 1996;85:196–206. doi: 10.1097/00000542-199607000-00025. [DOI] [PubMed] [Google Scholar]
- 25.Fu ES, Scharf JE, Glodek J. Preoperative testing: a comparison between HealthQuiz recommendations and routine ordering. Am J Anesth. 1997;24:237–40. [Google Scholar]
- 26.Beers RA, O’Leary CE, Franklin PD. Comparing the history-taking methods used during a preanesthesia visit: the HealthQuiz versus the written questionniare. Anesth Analg. 1998;86:134–7. doi: 10.1097/00000539-199801000-00027. [DOI] [PubMed] [Google Scholar]
- 27.Schroeder SA, Myers LP, McPhee SJ, et al. The failure of physician education as a cost containment strategy. JAMA. 1984;252:225–30. [PubMed] [Google Scholar]
- 28.Williams SV, Eisenberg JM. A controlled trial to decrease the unnecessary use of diagnostic tests. J Gen Intern Med. 1986;1:8–13. doi: 10.1007/BF02596318. [DOI] [PubMed] [Google Scholar]