Abstract
OBJECTIVE
Although longitudinal care constitutes the bulk of primary care, physicians receive little guidance on the fundamental question of how to time follow-up visits. We sought to identify important predictors of the revisit interval and to describe the variability in how physicians set these intervals when caring for patients with common medical conditions.
DESIGN
Cross-sectional survey of physicians performed at the end of office visits for consecutive patients with hypertension, angina, diabetes, or musculoskeletal pain.
PARTICIPANTS/SETTING
One hundred sixty-four patients under the care of 11 primary care physicians in the Dartmouth Primary Care Cooperative Research Network.
MEASUREMENTS
The main outcome measures were the variability in mean revisit intervals across physicians and the proportion of explained variance by potential determinants of revisit intervals. We assessed the relation between the revisit interval (dependent variable) and three groups of independent variables, patient characteristics (e.g., age, physician perception of patient health), identification of individual physician, and physician characterization of the visit (e.g., routine visit, visit requiring a change in management, or visit occurring on a “hectic” day), using multiple regression that accounted for the natural grouping of patients within physician.
MAIN RESULTS
Revisit intervals ranged from 1 week to over 1 year. The most common intervals were 12 and 16 weeks. Physicians’ perception of fair-poor health status and visits involving a change in management were most strongly related to shorter revisit intervals. In multivariate analyses, patient characteristics explained about 18% of the variance in revisit intervals, and adding identification of the individual provider doubled the explained variance to about 40%. Physician characterization of the visit increased explained variance to 57%. The average revisit interval adjusted for patient characteristics for each of the 11 physicians varied from 4 to 20 weeks. Although all physicians lengthened revisit intervals for routine visits and shortened them when changing management, the relative ranking of mean revisit intervals for each physician changed little for different visit characterizations—some physicians were consistently long and others were consistently short.
CONCLUSION
Physicians vary widely in their recommendations for office revisits. Patient factors accounted for only a small part of this variation. Although physicians responded to visits in predictable ways, each physician appeared to have a unique set point for the length of the revisits interval.
Keywords: follow-up, revisit interval
Longitudinal care is a fundamental component of primary care and implies that patients will be asked to return for follow-up visits. Although primary care physicians spend much of their time delivering longitudinal care, little guidance is available to help them in timing these follow-up visits. Neither medical school nor residency curricula include explicit training in how to time primary care follow-up visits, nor can physicians find guidance for the optimal interval in the medical literature or from published guidelines. In our literature search, we found two studies modeling revisit intervals for patients undergoing chronic anticoagulation1 and patients with recurrent bladder cancer.2 The literature about primary care revisits was limited to one abstract that examined actual intervals assigned by primary care doctors,3 three studies about hypothetical patients,4–6 and three administrative database reviews (examining return visit intervals rather than physician-recommended revisit intervals).7–9 These studies consistently demonstrate twofold to threefold variation in the revisit interval.
How do physicians select revisit intervals? Physician decisions about the revisit interval may be determined by patient characteristics, the physician, and characteristics of the current visit. For example, physicians probably ask sicker patients to return sooner than healthier patients.10 In addition, even in the absence of an explicit algorithm, physicians most likely develop (or “inherit” during training) heuristics about how often to see different categories of patients. It is also likely that features of the current visit (whether a medication was started or changed, or a test was ordered) affect the length of the revisit interval. The relative contribution of such factors in explaining the variation in revisit intervals has been largely unexplored.
We examined how a group of primary care physicians participating in the Dartmouth Primary Care Cooperative Research Network (COOP) designated revisit intervals for established patients with four common medical conditions: hypertension, diabetes mellitus, angina, and musculoskeletal pain. At the end of office visits, physicians completed surveys that described their recommended revisit interval and perceptions. The goal of this study was to identify and assess the relative importance of patient, physician, and visit characteristics in determining the revisit interval.
METHODS
Setting and Participants
The Dartmouth COOP is a voluntary network of independent clinicians.11,12 In 1994, a Dartmouth COOP study group (see acknowledgments) selected the revisit interval as a research topic. After a pilot test of forms and methods, we randomly selected 18 primary care physicians practicing in separate rural locations from the list of providers participating in the Dartmouth COOP. Eleven physicians agreed to participate. We obtained descriptive information about these physicians from the Dartmouth COOP database.
Established patients were recruited from the offices of the 11 physicians. Each patient contributed data for only one revisit interval (i.e., each patient had only one study visit). Eligible patients were required to have at least one of four common primary care diagnoses: hypertension, angina pectoris, diabetes mellitus, or musculoskeletal pain (including any arthritis or back pain). Patients could have more than one of these entry diagnoses.
At the end of each eligible patient’s study visit, physicians completed a pocket-sized data entry card. The card asked physicians to respond to questions about the patient and the visit and to indicate for each patient their recommended revisit interval in weeks.
Data and Analysis Plan
The distribution for revisit intervals was right skewed; therefore, for all analyses, we used the log-transformed data to calculate mean revisit intervals, but for simplicity, we expressed the results in the corresponding natural units (i.e., the geometric mean). We used Student’s t tests to assess the relation between revisit intervals and individual characteristics. All comparisons were two-sided and considered statistically significant at p < .05.
One goal was to explain variance in the revisit interval. To assess the relation between the revisit interval and its potential determinants, we grouped the measures into three blocks: patient characteristics, identification of individual physician, and physician characterization of the visit.
The patient characteristics obtained included age and sex, the number of prescription medications regularly taken, the physician’s perceptions of patient’s overall health status, psychological status, medical stability, and continuity with the physician, and the four entry diagnoses (angina, diabetes, hypertension, or musculoskeletal pain).
The block to identify the individual physician consisted of 11 indicator variables. Each indicator variable represented a single study physician. To begin to understand the importance of the physician, we used these indicator variables to summarize the physician’s role in determining the revisit interval.
The Dartmouth COOP study group hypothesized that three visit characteristics might influence revisit intervals. Physicians were asked to characterize the visit by indicating whether or not the visit was routine, required a change in medical management, or occurred on a “hectic day.”
To assess the relative contribution of these blocks of variables in determining the revisit interval, we used multiple linear regression. Because revisit intervals may be more similar for the patients of one physician than for patients of different physicians, we used a method of variance calculation to account for the natural grouping of patients within physicians (robust variance calculation; Stata Statistical Software, release 5.0, Stata Corp., College Station, Tex., 1997). The linear regression model expresses the revisit interval (dependent variable) as a function of the three blocks of independent variables where the unit of analysis was the patient. To maximize the explanatory power of our model, we used forward stepwise linear regression (p to enter = .15, p to remove>.3) with robust variance estimation to select the best variables in block 1. We then locked the selected variables from block 1 (patient characteristics) and the block 2 variables (physician indicators) and entered block 3 variables (visit characteristics) for selection.
To assess the explanatory power of each block of variables, we compared the r2 of the model after the addition of each new block. There is some controversy about the interpretation of r2 in a regression model using robust variance calculation. Repeating our stepwise regression using ordinary linear regression resulted in exactly the same set of selected variables and only minimal differences in the variance estimates of the regression coefficients. The stability of our findings suggests that accounting for the natural grouping of patients within physicians made little difference.
To directly assess physician variation in setting revisit intervals, we calculated each physician’s average revisit interval. To account for differences in patient mix between physicians, we solved the regression equation, which included the patient characteristics selected in our stepwise regression (block 1) and the physician indicator variables (block 2), using the sample means for each patient characteristic. To see how each physician responded to different visit conditions, we created four separate models using indicator variables for the different visit categories (block 3): all visits (no additional variable), routine visit, change in management visit, and visit occurring on a hectic day. We found no significant interactions between physician and any of the other potential determinants. All analyses were performed using Stata Statistical Software.
RESULTS
Study Sample
Physicians
All 11 Dartmouth COOP physicians were male; 6 were internists, and 5 were family practitioners. Physician ages ranged from 42 to 60 (median age 48), and year of graduation from medical school ranged from 1961 to 1979 (median 1974). All practices were largely rural; six of the physician practices were solo, and the remainder were group practices. These 11 physicians enrolled 164 patients (mean of 15 patients per physician, range 6–18).
Patients
Patient ages ranged from 28 to 89 (median age 68), and most (89%) had fee-for-service insurance. Hypertension was the most common entry diagnosis (55%), followed by musculoskeletal pain (44%), diabetes mellitus (32%), and angina (26%). Thirty-seven percent had multiple entry diagnoses, 11% had three or more diagnoses, and many regularly used three or more medications (Table 1) The physicians rated about one third of patients as being in fair to poor general health and almost one quarter as in fair to poor mental health. Almost all physicians felt that they had good or excellent continuity with the patient.
Table 1.
Characteristics Associated with Shorter Revisit Intervals (n = 164)
| Mean Revisit Interval,* Weeks | |||||
|---|---|---|---|---|---|
| Characteristic | % | CharacteristicPresent | CharacteristicAbsent | WeeksShorter† | p value |
| Patient characteristics | |||||
| Age ≤65 | 36 | 9.3 | 11.2 | 1.9 | .20 |
| Male | 51 | 9.9 | 11.0 | 1.1 | .41 |
| 3+ Entry diagnoses‡ | 11 | 9.5 | 10.6 | 1.1 | .61 |
| 3+ Medications | 62 | 9.8 | 11.4 | 1.6 | .28 |
| Fair or poor general health | 35 | 7.0 | 13.1 | 6.1 | <.001 |
| Fair or poor mental health | 22 | 7.5 | 11.5 | 4.0 | .02 |
| Fair or poor prior medical stability | 21 | 7.3 | 11.5 | 4.2 | .005 |
| Fair or poor continuity | 8 | 6.7 | 10.9 | 4.2 | .06 |
| Physician characterization of visit | |||||
| Not a routine visit for this patient | 43 | 6.4 | 14.9 | 8.5 | <.001 |
| Medical management change | 38 | 5.9 | 15.0 | 9.1 | <.001 |
| Hectic at time revisit scheduled | 37 | 8.7 | 11.6 | 2.9 | .04 |
Mean revisit intervals are represented by the geometric mean because the distribution of revisit intervals is skewed.
The absolute difference between the mean revisit interval with characteristic absent and that with characteristic present.
Entry diagnoses include angina, diabetes mellitus, hypertension, and musculoskeletal pain.
Revisit Intervals
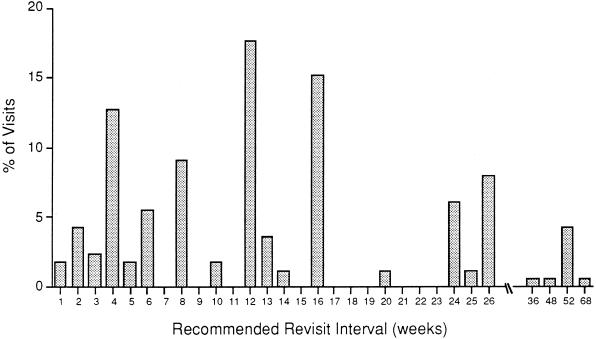
Figure 1 shows the distribution of visits for all 164 patients. Although we asked physicians for the revisit interval in weeks, most physicians appeared to think in months. The most common revisit intervals were 1 month (4 weeks), 3 months (12 weeks), 4 months (16 weeks), and 6 months (24–26 weeks).
FIGURE 1.
Distribution of the revisit intervals in weeks for 164 patients in the Dartmouth COOP revisit study.
Determinants of Revisit Intervals
Patient Characteristics
Table 1 also shows how patient characteristics were related to revisit intervals. We found that physician perception of fair or poor health was associated with significantly shorter revisit intervals. For example, patients rated in fair or poor health had an average revisit interval of 7 weeks, while patients in excellent or good health had an average interval of 13 weeks (p < .001). We observed similar relations for the other health status measures: fair or poor mental health was associated with a 4 week shorter revisit interval (p = .02), as was fair or poor medical stability (p = .005). In addition, poor continuity with the doctor was associated with a shorter revisit interval, although this finding was of borderline statistical significance (p = .06). Age, number of entry diagnoses, and number of medications were not significantly associated with the length of the revisit interval.
Physician Characterization of the Visit
Visit characterizations appeared to be important determinants of the revisit interval (Table 1). For example, the revisit interval for nonroutine visits was about 9 weeks shorter than for routine visits (p < .001); similarly, the interval for visits when there was a change in management was about 9 weeks shorter than for visits without such a change (p < .001). In addition, visits occurring on days that the physician perceived as hectic were associated with revisit intervals approximately 3 weeks shorter (p = .04).
Explaining Variance in Revisit Intervals
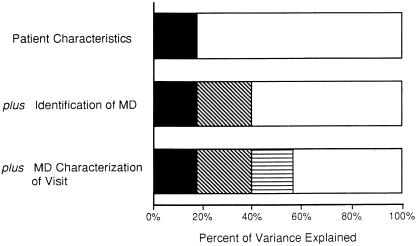
Figure 2 shows the contribution of patient characteristics, knowing who the physician is, and characteristics of the visit in explaining variance. The variables selected from the patient characteristic block were age (p = .11), general health status (p = .001), and continuity with the physician (p = .06). This block explained 18% of the variance. Adding identification of the 11 physicians raised the variance explained to 40% (test of additional significance p < .0001). The final model selected two of the three visit characterizations: routine visit and change in management. Adding these variables raised the variance explained to 57% (test of additional significance, p = .0009). In this final model, only general health status (p < .002) and routine visits (p = .05) were statistically significant independent predictors of the revisit interval.
FIGURE 2.
The proportion of variance explained for each block of variables is represented by the shaded areas in each of the bars. The white area in each bar represents the proportion of variance unexplained.
Physician Patterns for Setting Revisit Intervals
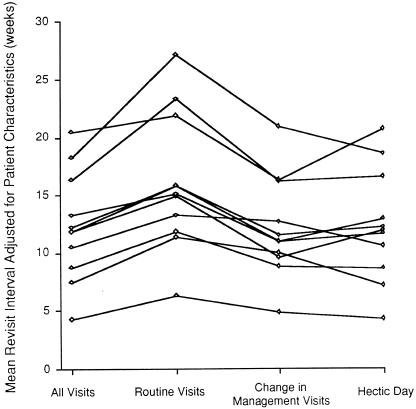
To account for differences in case mix, we calculated the mean revisit interval for each physician after adjusting for the variables selected from the patient characteristic block in our stepwise regression. Adjustment had little effect on the degree of variation. The overall crude physician mean was 10 weeks with a range from 4 to 24 weeks, while the adjusted mean was 12 weeks with a range from 4 to 20 weeks. Figure 3 displays the adjusted mean revisit interval for each physician overall (i.e., for all visits) and stratified by physician visit characterizations (i.e., routine visits, visits involving a change in management, and visits occurring on a hectic day). Each line represents one physician and that physician’s adjusted mean revisit interval for each of these characterizations.
FIGURE 3.
Mean revisit intervals (geometric means) for the 11 study physicians adjusted for patient characteristics. In addition to each physician’s overall mean, means for the three physician characterizations of visits (i.e., routine visits, visits involving a change in management, and visits occurring on a “hectic” day) are shown. Each line represents one physician and that physician’s mean revisit interval for each visit characterization.
Following the lines in Figure 3 from left to right demonstrates how each physician’s mean revisit interval changed with varying characterizations. Even after adjustment for differences in patient characteristics, the physician’s mean revisit interval varied widely under all visit categories. Although all physicians lengthened revisit intervals for routine visits and shortened them when changing management, the relative ranking of the mean revisit interval for each physician changed little under different visit characterizations—some physicians were consistently long and others were consistently short.
DISCUSSION
We found substantial variation in the revisit intervals physicians recommended for patients with common primary care diagnoses. Although patient characteristics such as age or health status explained a small part of this variation, factors related to the patient’s physician had a stronger influence on the timing of follow-up visits. Simply knowing the physician’s identity and whether he or she characterized the visit as routine or requiring a change in management accounted for three times as much of the variation as knowing characteristics about the patient.
The average revisit interval for each physician also varied substantially. We found fivefold variation in mean revisit interval across the 11 physicians in our study. While all physicians responded to different kinds of visits in predictable ways (i.e., shortening the interval for routine visits), the relative ranking of the physician’s mean revisit interval changed little across the different visit characterizations, with each physician exhibiting a tendency to recommend revisit intervals around a given length.
We acknowledge several limitations to our study. First, the small sample of relatively homogeneous practices may limit the generalizability of our results. It is likely, however, that a sample of more heterogeneous practices (i.e., a mix of urban and rural, specialist and generalist practices) would demonstrate even greater variation in the revisit intervals. Second, unmeasured patient factors might account for some of the observed variation in recommended revisit intervals. Our analyses did not include data on the patient’s perceived physical, psychological, or social condition, information that might also influence how the physician chose a given revisit interval. We did, however, have data on a subset of 96 study patients who completed the Dartmouth COOP self-assessment form.13,14 Repeating our analysis on the subset of patients with self-reported health measures did not increase the explanatory power of our model. Some also may be concerned that we used physician perceptions of health status rather than the patient’s self-report in our analyses. We believe that the physician’s own rating of the patient’s physical health, mental health, and “medical stability” are the health status measures most relevant to the physician at the time the revisit interval is being set. Finally, the number of providers made it impossible to look at physician characteristics.
Even in our most comprehensive model, about half of the variance in the revisit interval remained unexplained. Some variance may be explained by pragmatic factors we did not measure. The amount of time the physician has available to see patients (a function of how many clinic slots the physician has available, the time allotted for each slot, and how many patients are in the physician’s panel), for example, may constrain physician options in setting the revisit interval. Thus, average revisit intervals for otherwise identical physicians serving similar patients might differ greatly on the basis of “availability” alone, a hypothesis consistent with the theory of supplier-induced demand.15,16
Some of the unexplained variance is probably unexplainable. The choice of revisit interval undoubtedly reflects a complexity that is not easily measurable. Recent experiences (i.e., “last-case bias”) may exert a powerful influence. Experiencing or hearing about a bad or unexpected outcome for one patient might lead some physicians to look harder at subsequent patients. Physicians’ responses to such experiences may also be affected by other factors such as their confidence, ability to tolerate diagnostic uncertainty,17 beliefs about the appropriate “intensity” of care, and concerns about malpractice litigation.
The relation between a hectic day and the revisit interval also highlights the potential complexities involved in how physicians time follow-up. In our data, although hectic days were associated with a shorter revisit interval, the directionality of this relation is unclear. On hectic days, physicians may feel that they are less able to complete work and recommend shorter revisit intervals to resolve unfinished business. A patient with several active problems, for example, may be asked back in order to address health maintenance issues. Conversely, the causal pathway may be just the reverse. Physicians who recommend short revisit intervals will soon fill all available appointments and may need to overbook patients—producing hectic days. As hectic days are less enjoyable, we surmise that the revisit interval could affect physician satisfaction.
There is evidence that the revisit interval also affects patient satisfaction—although different patients may want different things. In the Veterans Affairs Cooperative study of intensive primary care,18 patients with shorter revisit intervals reported higher levels of satisfaction (although they had higher rates of hospitalization). In contrast, a recent study found that breast cancer patients preferred less frequent follow-up.19
Our data indicate that patient health status does not dominate how physicians time follow-up visits. Rather, physicians appear to have characteristic scheduling tendencies that greatly influence the length of the revisit interval. Even after accounting for important patient characteristics and regardless of whether the visit was characterized as routine or requiring a change in management, physicians’ mean revisit interval varied fivefold. Because how frequently physicians see their patients has a direct influence on how many patients they can care for, the timing of follow-up has profound professional and societal implications. Although a formidable challenge, it is essential that we learn the consequences of this everyday and seemingly routine decision on patient outcomes.
Acknowledgments
This study was supported by the Agency for Health Care Policy and Research (grant HS07350). Drs. Schwartz and Woloshin were supported by Veterans Affairs Career Development Awards in Health Services Research and Development.
The authors thank James Hardin, PhD, for technical assistance.
Study physicians were David Albright, MD, Capital Area CHP, Brattleboro, Vt; Roger Fox, MD, Mountain Valley Health Clinic, Londonderry, Vt; Warner Jones, MD, Springfield Internal Medicine, Springfield, Vt; John Kirk, MD, New London Medical Center, New London, NH; Neil Korsen, MD, Sacopee Valley Health, Kezar Falls, Me; David Little, MD, Villemaire Family Health Center, Milton, Vt; Dennis Plante, MD, Fletcher-Allen Health Care, Williston, Vt; Roger Renfrew, MD, Redington Medical Associates, Skowhegan, Me; Karl Singer, MD, Exeter Family Medicine Associates, Exeter, NH; Robert Tortolani, MD, Brattleboro, Vt; and Timothy Wolfe, MD, Newport Health Center, Newport, NH.
Pilot study participants were Tim Cox, PA, Mt. Mooselauke Health Center, Warren, NH; Paul Friedrichs, MD, Lamprey Health Care, Newmarket, NH; Norbert Goldfield, MD, Northhamptom, Mass; Gene Harkless, NP, University of New Hampshire, Durham, NH; Neil Korsen, MD, Sacopee Valley Health, Kezar Falls, Me; Dennis Plante, MD, Fletcher-Allen Health Care, Williston, Vt; Roger Renfrew, MD, Redington Medical Associates, Skowhegan, Me.; Karl Singer, MD, Exeter Family Medicine Associates, Exeter, NH; and Jerald Ward, MD, Gifford Family Health Center, Bethel, Vt.
REFERENCES
- 1.Kent D, Vermes D, McDonell M, Henikoff J, Fihn S. A model for planning optimal follow-up for outpatients on warfarin anticoagulation. Warfarin Optimal Outpatient Follow-up Study Group. Med Decis Making. 1992;12:132–41. doi: 10.1177/0272989X9201200206. [DOI] [PubMed] [Google Scholar]
- 2.Kent D, Nease R, Sox H, Shortliffe L, Shachter R. The Bladder Cancer Follow-up Group. Evaluation of nonlinear optimization for scheduling of follow-up cytoscopies to detect recurrent bladder cancer. Med Decis Making. 1991;11:240–8. doi: 10.1177/0272989X9101100402. [DOI] [PubMed] [Google Scholar]
- 3.Gordon GH, Tyler J, Friis R. Factors influencing return visit intervals in a medical outpatient clinic. Clin Res. 1984;32:32A. Abstract. [Google Scholar]
- 4.Lichtenstein M, Sweetnam P, Elwood P. Visit frequency for controlled essential hypertension: general practitioners’ opinions. J Fam Pract. 1986;23:331–6. [PubMed] [Google Scholar]
- 5.Petitti DB, Grumbach K. Variations in physicians’ recommendations about revisit interval for three common conditions. J Fam Pract. 1993;37:235–40. [PubMed] [Google Scholar]
- 6.Tobacman J, Zeitler R, Cilursu A, Mori M. Variation in physician opinion about scheduling of return visits for common ambulatory care conditions. J Gen Intern Med. 1992;7:312–6. doi: 10.1007/BF02598090. [DOI] [PubMed] [Google Scholar]
- 7.Lichtenstein M, Steele M, Hoehn T, Bulpitt C, Coles E. Visit frequency for essential hypertension: observed associations. J Fam Pract. 1989;28:331–6. [PubMed] [Google Scholar]
- 8.Stern M, Fitzgerald J, Dittus R, Tierney W. Office visits and outcomes of care: does frequency matter? Clin Res. 1991;39:610A. Abstract. [Google Scholar]
- 9.Dittus R, Tierney W. Scheduling follow-up office visits: physician variability. Clin Res. 1987:738A. Abstract. [Google Scholar]
- 10.Kravitz R, Greenfield S, Rogers W, Manning W, Zubkoff M, Nelson E. Differences in the mix of patients among medical specialties and systems of care. JAMA. 1992;267:1617–23. [PubMed] [Google Scholar]
- 11.Nelson E, Kirk J, Bise B, et al. The Cooperative Information Project, part 2: some initial clinical, quality assurance, and practice management studies. J Fam Pract. 1981;13:867–76. [PubMed] [Google Scholar]
- 12.Nelson E, Kirk J, Bise B, et al. The Cooperative Information Project, part 1: a sentinel practice network for service and research in primary care. J Fam Pract. 1981;13:641–9. [PubMed] [Google Scholar]
- 13.Nelson E, Landgraf J, Hays R, Wasson J, Kirk J. The functional status of patients: how can it be measured in physicians’ offices? Med Care. 1990;28:1111–26. [PubMed] [Google Scholar]
- 14.Nelson E, Wasson J, Johnson D, Hays R. Dartmouth COOP Functional Health Assessment Charts: brief measures for clinical practice. In: Spilker B, editor. Quality of Life and Pharmacoeconomics in Clinical Trials. 2nd ed. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. [Google Scholar]
- 15.Wennberg J, Gittelsohn A. Variations in medical care among small areas. Sci Am. 1982;246:120–34. doi: 10.1038/scientificamerican0482-120. [DOI] [PubMed] [Google Scholar]
- 16.Hemenway D, Fallon D. Testing for physician-induced demand with hypothetical cases. Med Care. 1985;23:344–9. doi: 10.1097/00005650-198504000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Geller G, Tambor E, Chase G, Na NH. Measuring physicians’ tolerance for ambiguity and its relationship to their reported practices regarding genetic testing. Med Care. 1993;31:989–1001. doi: 10.1097/00005650-199311000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Weinberger M, Oddone E, Henderson W. Does increased access to primary care reduce hospital readmissions? N Engl J Med. 1996;335:1441–7. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 19.Gulliford T, Opomu M, Wilson E, Hanham I, Epstein R. Popularity of less frequent follow up for breast cancer in randomized study: initial findings from the hotline study. BMJ. 1997;314:174–7. doi: 10.1136/bmj.314.7075.174. [DOI] [PMC free article] [PubMed] [Google Scholar]