Abstract
OBJECTIVE
To test the significance of health literacy relative to other predictors of adherence to treatment for HIV and AIDS.
PARTICIPANTS
Community sample of HIV-seropositive men (n = 138) and women (n = 44) currently taking a triple-drug combination of antiretroviral therapies for HIV infection; 60% were ethnic minorities, and 73% had been diagnosed with AIDS.
MEASUREMENTS
An adapted form of the Test of Health Literacy in Adults (TOFHLA), a comprehensive health and treatment interview that included 2-day recall of treatment adherence and reasons for nonadherence, and measures of substance abuse, social support, emotional distress, and attitudes toward primary care providers.
MAIN RESULTS
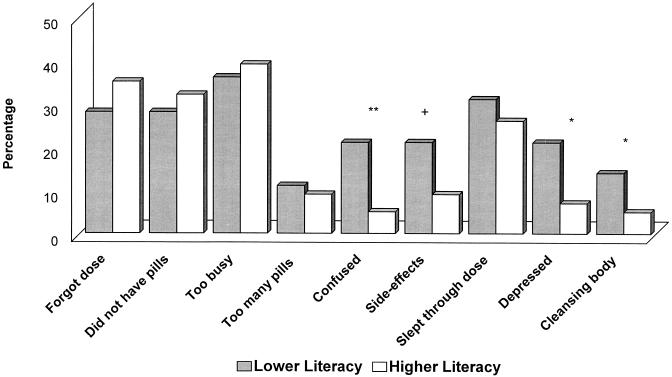
Multiple logistic regression showed that education and health literacy were significant and independent predictors of 2-day treatment adherence after controlling for age, ethnicity, income, HIV symptoms, substance abuse, social support, emotional distress, and attitudes toward primary care providers. Persons of low literacy were more likely to miss treatment doses because of confusion, depression, and desire to cleanse their body than were participants with higher health literacy.
CONCLUSIONS
Interventions are needed to help persons of low literacy adhere to antiretroviral therapies.
Keywords: HIV infection, AIDS treatment, medication adherence
Combination antiretroviral therapies for HIV infection have demonstrated efficacy in improving immune function, reducing viremia, and reducing HIV-related morbidity and mortality. However, the promises of revolutionary HIV-AIDS treatments also bring significant challenges. Highly active antiretroviral therapy (HAART) includes complex regimens that require strict adherence to complicated treatment schedules. Of great concern are treatment-resistant variants of HIV that rapidly develop in response to underdosing and intermittent, irregular use of antiretroviral agents.1 Factors that negatively influence adherence to HAART therefore pose considerable threats to both individual and public health.
Several factors related to adherence to reverse transcriptase inhibitor regimens were reported before protease inhibitors became available.2 As many as one third of patients taking reverse transcriptase inhibitors, particularly zidovudine, may discontinue their use,3 and one third may intentionally alter prescribed doses.4 Failing to adhere to treatment can result from forgetting, lack of motivation, and intolerance of side effects. Treatment nonadherence can also be a response to the burdens of complicated drug regimens that disrupt one’s daily routine.5 Among persons studied in one AIDS clinical trial, missed doses of antiretroviral agents were most likely to occur because of forgetting (43%), sleeping through a dose (36%), being away from home (32%), changing one’s routine (27%), being too busy to take the dose (22%), feeling sick (11%), and experiencing depression (9%).6 People who refuse to take antiretroviral therapy commonly state that they believe the drugs are ineffective and toxic.7 Social support is associated with adhering to antiretroviral therapy, with greater social support predicting more consistent adherence.8 Another key factor in medication adherence is the relationship between patient and primary care provider. Patients who trust their provider and are satisfied with their quality of care are more likely to adhere to treatment regimens.9,10
Substance abuse also raises concerns about antiretroviral treatment owing to the cognitive and behavioral disturbances common in substance-abusing populations. For example, Singh and colleagues found that HIV-seropositive patients with a history of injection drug use were more likely to be nonadherent to antiretroviral therapy than were those who had not used injection drugs.11 Nonadherent patients also were more likely to experience symptoms of depression and lacked adaptive coping strategies. Broers et al. reported that injection drug users delayed initiating anti-HIV treatment, but were adherent once treatment was started.12 O’Connor and Samet suggested that substance-abusing patients have a host of problems, including resistance to comply with instructions, potential drug interactions, and conditions of living in poverty, that present considerable challenges to medical management of HIV infection.13
In the current study, we examined adherence to antiretroviral therapies in a community sample of men and women living with HIV-AIDS. Although a number of variables influence adherence to non-HIV treatments, many of which have been associated with adherence to zidovudine therapy among people living with HIV-AIDS, these factors are currently being examined in adherence to HAART. Among other influences of treatment adherence, we were particularly interested in the patient’s ability to comprehend medical information and the association between literacy skills and HIV treatment adherence. Health literacy is frequently below functional levels in medical populations, and people with lower health literacy often experience poor health and negative treatment outcomes.14,15 Understanding medical instructions is a necessary, although for many not sufficient, condition for treatment adherence. To our knowledge, this is the first study to examine health literacy, a more sensitive and specific index of understanding medical instructions than general education level, among factors related to antiretroviral therapy adherence. We hypothesized that health literacy would significantly predict adherence to antiretroviral regimens over and above other well-established predictors of treatment adherence. If confirmed, this would indicate that interventions to improve adherence must be adjusted to accommodate reading and comprehension skills of people with low literacy.
METHODS
Participants
Of the 318 study participants, 223 (70%) were men, 93 (29%) were women, and 2 (1%) were transgender persons. The majority of the sample was African American (65%), with 30% white, and the remaining 5% being of other ethnic backgrounds. The mean (SD) age was 39.1 (7.4) years. Of the 318 persons enrolled in the study, 81 (25%) were not currently taking antiretroviral drugs, 7 (2%) were taking one antiretroviral drug, 46 (15%) were on a two drug-regimen, and 184 (58%) were taking a combination of three antiretroviral drugs. All remaining analyses focus on the 184 persons taking triple combination therapies.
Measures
Participants completed three sets of measures in a single assessment session: (1) assessment of health literacy; (2) an interview to elicit demographic characteristics, information concerning health status, current treatments for HIV-AIDS and treatment adherence, and factors related to treatment adherence; and (3) self-administered measures (or interview-administered for persons who could not read) of substance abuse, emotional distress, perceived social support, and attitudes toward primary care providers. These measures are described below.
Health Literacy
Health-related literacy was measured using an adaptation of the Test of Functional Health Literacy in Adults (TOFHLA). This instrument formed the basis for defining literacy in the current study. The TOFHLA, developed as a comprehensive assessment of literacy in relation to health status and care delivery,14 was designed to capture reading comprehension skills in the middle to lower levels of literacy. We administered an adapted version of the reading comprehension section of the TOFHLA. We selected two of the three standard passages: instructions written for patients receiving an upper gastrointestinal series, and the patient rights and responsibilities section of a Medicaid application form. We also included a third passage, matched for grade level and word frequency of target words, that specifically addressed HIV-AIDS–related care. The scale includes 53 four-option multiple choice items, in which sentences are completed by selecting the correct word among the four options. Scores ranged from 0 to 53 correct responses.
We also administered the numeracy scale of TOFHLA using standardized procedures and items. The numeracy scale consists of actual medical instructions that concern receiving, following, and paying for medical treatments and asks nine questions concerning these situations. Unlike the reading comprehension scale, the numeracy scale is administered in an interview and used to assess one’s ability to understand and act on numerical instructions for health care. Scores range from 0 to 9 correct responses. For the purposes of the current study, the numeracy scale was used to internally validate our definition of literacy based on the reading comprehension scale.
Health and Treatment Interview
Demographic characteristics
Participants were asked their age, years of education completed, and their self-identified ethnicity and gender (for those who were transgender).
Health status
Because the study was conducted in a community-based service setting, biomedical data were collected through self-report measures. Participants were asked what month and year they tested HIV seropositive, whether they had experienced 15 different HIV-related symptoms, and whether they had been diagnosed with AIDS-defining conditions. Participants provided their most recent CD4 cell count and viral load.
Treatment status and adherence
Participants were interviewed to identify the HIV treatments they were currently taking and the doses taken in the past 2 days. First, participants were asked to name the drugs they were taking. Next, interviewers asked participants to confirm the drugs they were taking by identifying their treatments among pictures of drugs shown on a chart. Interviewers proceeded to ask participants to think back about what they did yesterday and recall the times they had taken each drug. A daily calendar was used to cue participants’ memory and help structure their responses. Interviewers recorded the number of doses reportedly taken for each drug. Participants were then asked whether they were off schedule from the prescribed dose time by ±1 hour for each dose taken. This section of the interview was then repeated, asking participants to report the same information using the same procedures for the day before yesterday. Two-day treatment recall, for yesterday and the day before yesterday, formed the basis of calculating the proportion of prescribed doses using the following formula: Total antiretroviral pills taken in past 2 days/Total antiretroviral pills prescribed for past 2 days. Finally, participants were asked about other treatments they were currently taking that were not part of the antiretroviral therapy.
Perceived barriers to treatment and reasons for non-adherence
Participants were asked to reflect back on the past 30 days, recall to the best of their ability the times when they had missed a dose of their antiretroviral medications, and mark the circumstances that played a role in their not taking their medication at those times. This measure included nine barriers to medication adherence identified in the literature: forgetting to take a dose, not having medications on hand, being too busy, having too many medications to manage, feeling confused about dosing, medication side effects, sleeping through a dose, feeling depressed, and wanting to cleanse one’s body. A calendar method was again used to help participants structure and recall events.
Survey of Factors Influencing Adherence
Substance use
Participants were asked to report their use of alcohol, marijuana, powder or crack cocaine, nitrite inhalant (poppers), injection drugs, and other drug use over the past 3 months. Participants indicated whether they had used each drug in the past 3 months in a yes/no response format. Reporting use of any drug other than alcohol was coded as having used other drugs.
Emotional distress
The 53-item Brief Symptom Inventory (BSI) was administered as an index of psychological distress and disturbances. The BSI includes items representing symptoms of somatic anxiety, obsessive-compulsive thoughts, depression, anxiety, hostility, paranoia, and psychoticism. The total score yields a General Severity Index, a reliable and valid measure of emotional distress with scores ranging from 53 to 265.16
Perceived social support
Perceived social support was assessed with a 15-item scale reflecting availability and quality of support. Example items include “There are several people that I trust to help me solve problems,”“If I were sick, I could easily find someone to help me with my daily chores,” and “I feel a strong emotional bond with at least one person.” Items were responded to on 4-point scales, where 1 = definitely true, and 4 = definitely false. Scores ranged from 15 to 60. The social support scale was reliable in the current sample (α coefficient = .86).
Attitudes toward primary care provider
An assessment of perceived quality of one’s relationship with the primary care provider was adapted from the Functional Assessment of HIV Infection Scale.17 This instrument consists of seven items responded to on 4-point scales, where 1 = never, and 4 = always. Example items include “Does your doctor answer all of your questions about HIV?,”“Does your doctor ask for your opinions and concerns regarding your HIV treatment?,” and “Do you have confidence in your doctor?” Scores ranged from 7 to 28. The provider attitudes scale was found reliable in the current sample (α coefficient = .75).
Procedures
Men and women were recruited from AIDS service organizations, health care providers, social service agencies, community residences for people living with HIV-AIDS, and infectious disease clinics in Atlanta, Georgia. Flyers announcing the study opportunity were posted in these locations, and stacks of flyers were placed in waiting areas. Interested persons telephoned the research program offices to schedule an appointment to participate in the study. The research program was located in a community setting in an area of Atlanta accessible by public transportation. Individuals were told they would be asked to complete an anonymous survey and interview concerning their health, mental health, social relationships, and substance use. Participants were informed that they would have to verify their HIV status by presenting a photo ID as well as their clinic card from an HIV-infectious disease clinic, a prescription or drug bottle for antiretroviral medication, seropositive results of an HIV test, or other links to HIV-related services or treatment. Names were not recorded in this study, but proof of HIV status was necessary to keep seronegative persons from participating for cash incentives.
Participants completed informed consent in accordance with Institutional Review Board guidelines, followed by literacy assessments, the health and treatment interview, and survey of factors associated with adherence. Participants who were unable to read the self-administered survey were interviewed to complete all study measures. Trained research staff conducted all interviews. The study required 2 to 3 hours to complete, and participants were given $50 compensation for their time and participation. Participants were given flyers before leaving and asked to tell their friends and other acquaintances who have HIV about the study to increase word-of-mouth recruitment.
Data Analyses
Analyses compared persons who had missed at least one dose of antiretroviral medications (<100% adherent) in the previous 2 days and persons who had not missed a dose (100% adherent). Continuous measures are represented by means and standard deviations, and categorical data are represented by percentages of nonadherent and adherent group members. Significance tests were conducted using univariate logistic regressions followed by multivariate logistic regressions with forward entry procedures. Adjusted odds ratios (ORs) with 95% confidence intervals (CIs) are presented.
We also examined the associations between health literacy and perceived barriers to HIV treatment adherence. By extrapolation from scoring for the standardized TOFHLA, participants who scored below 85% correct on the adapted TOFHLA reading comprehension scale were defined as lower literacy and persons scoring 86% correct or better were defined as higher literacy. Comparisons between lower and higher literacy groups on perceived barriers to treatment adherence were examined using contingency table χ2tests.
RESULTS
According to cued recall for the previous 2 days, 36 (20%) of the 182 participants taking HAART had missed at least one dose of antiretroviral medications. Persons who were not completely adherent in the past 2 days reported taking a mean (SD) of 62% (32.1%) of their antiretroviral medications during that time. Compared with persons who did not miss a dose (37%), participants who missed at least one dose (56%) were also more likely to have been off schedule (p < .05). As shown in Table 1), individuals who were nonadherent reported lower education levels (p < .01) and were more likely to be ethnic minorities (p < .05). They also reported significantly lower CD4 cell counts (p < .05) and were less likely to have an undetectable viral load compared with adherent participants (p < .05).
Table 1.
Characteristics of People Living with HIV-AIDS Taking Three-Drug Combination Therapies Who WereNonadherent and Adherent in the Past Two Days
| Characteristic | Nonadherent(n = 36) | Adherent(n = 148) | p Value* |
|---|---|---|---|
| Age in years, mean (SD) | 38.2 (7.1) | 40.4 (7.2) | NS |
| Years of education, mean (SD) | 12.2 (2.7) | 13.7 (2.3) | .01 |
| CD4 cell count, mean (SD) | 239.4 (198.9) | 315.9 (266.5) | .05 |
| Months tested HIV positive, mean (SD) | 89.3 (48.9) | 87.7 (60.8) | NS |
| Demographic, n(%) | |||
| Annual income <$10,000 | 23 (66) | 91 (62) | NS |
| Male | 24 (67) | 114 (78) | NS |
| Female | 12 (33) | 32 (21) | NS |
| Transgender | 1 (1) | NS | |
| White | 6 (17) | 66 (45) | .05 |
| African American | 27 (75) | 72 (49) | NS |
| Other ethnicity | 3 (8) | 9 (6) | NS |
| Heterosexual | 14 (39) | 47 (32) | NS |
| Homosexual | 16 (44) | 87 (59) | NS |
| Bisexual | 6 (17) | 13 (9) | NS |
| Health status, n(%) | |||
| Injection drug use history | 9 (25) | 39 (26) | NS |
| Undetectable viral load | 13 (36) | 80 (54) | .05 |
| AIDS diagnosis | 23 (79) | 110 (83) | NS |
Univariate significance tests; NS indicates not significant.
Factors Related to Treatment Adherence
Participants who had missed at least one dose of their antiretroviral medications in the past 2 days and those who had been adherent were compared on key demographic, health, mental health, and social factors (Table 2). Results of univariate logistic regression analyses showed that ethnic minorities (OR 4.1; 95% CI 1.6, 10.4), people with less than 12 years of education (OR 3.6; 95% CI 1.5, 8.7), less social support (OR 2.0; 95% CI 1.1, 3.7), greater emotional distress (OR 0.98; 95% CI 0.97, 0.99), and lower literacy (OR 2.6; 95% CI 1.1, 6.3) were more likely to be nonadherent in the past 2 days. Multivariate logistic regression, however, indicated that only years of education and literacy had significant independent associations with treatment adherence (see Table 2). Those with less than 12 years of education were over 3 times more likely to be nonadherent than those with at least a high school education, and those with lower reading literacy were nearly 4 times more likely to be nonadherent than those with higher literacy.
Table 2.
Results of a Multivariate Logistic Regression Predicting Adherence toCombination Antiretroviral Therapies over a Two-Day Recall Period
| Characteristic | Nonadherent(n = 36) | Adherent(n = 148) | OR (95% CI) |
|---|---|---|---|
| Age <35 years, n(%) | 12 (33) | 38 (26) | 1.7 (0.6, 4.9) |
| Ethnic minority, n(%) | 30 (83) | 81 (55) | 3.1 (0.9, 10.3) |
| Income <$10,000, n(%) | 23 (66) | 91 (62) | 0.6 (0.2, 1.8) |
| Education <12 years, n(%) | 11 (31) | 16 (59) | 3.3 (1.1, 10.7)* |
| HIV symptoms, mean (SD) | 6.2 (4.0) | 6.3 (3.4) | 1.0 (0.8, 1.2) |
| Alcohol use,†n(%) | 19 (53) | 71 (48) | 0.5 (0.2, 1.5) |
| Other drug use,†n(%) | 10 (28) | 58 (40) | 1.0 (0.3, 3.2) |
| Social support, mean score (SD) | 2.9 (0.5) | 3.2 (0.6) | 1.1 (0.5, 2.6) |
| Emotional distress, mean score (SD) | 109.9 (45.1) | 94.1 (29.9) | 0.99 (0.98, 1.0) |
| Provider attitudes, mean score (SD) | 21.1 (2.0) | 21.8 (2.7) | 1.1 (0.6, 1.4) |
| Lower literacy, n(%) | 10 (28) | 19 (13) | 3.9 (1.1, 13.4)* |
Significant, p < .05.
Substance use for the past 3 months.
Barriers to Treatment Adherence and Reading Literacy
Participants who scored less than 85% correct on the adapted TOFHLA reading comprehension scale, defined as being of lower literacy, were compared with persons who scored 86% correct or better, defined as being of higher literacy. Validating the literacy classification, we found that persons of lower literacy had significantly fewer years of education (mean [SD] 12.0 [2.6]) than persons of higher literacy (mean [SD] 13.7 [2.4]) (p < .01). One in three persons with less than 12 years of education scored below 85% correct on the reading comprehension scale, whereas 89% of those with 12 years education or more scored 86% correct or better (p < .01). The lower-literacy group also scored significantly lower on the independent measure of numerical health literacy (mean [SD] 6.7 [3.1]) than did the higher literacy group (mean [SD] 8.3 [3.0]) (p < .01).
Closer examination of the associations between education, health literacy, and HAART adherence showed that for persons with less than 12 years of education, the relation between health literacy and treatment adherence was nonsignificant (p>.1); 41% of persons with less than 12 years of education were nonadherent regardless of their health literacy score. In contrast, for persons with 12 or more years of education, the association between health literacy and HAART adherence was significant (p < .05); 32% of persons with low health literacy were not completely adherent in the previous 2 days compared with 14% of persons with higher health literacy scores.
Comparisons between individuals with lower and higher literacy demonstrated significant differences in the reasons they gave for missing antiretroviral drug doses in the previous 30 days. Individuals of lower literacy were more likely to indicate being confused (p < .01), experiencing side effects (p < .06), feeling depressed (p < .05), and wanting to cleanse their body (p < .05), compared with persons of higher literacy (Fig. 1). Differences between the two groups for the remaining barriers to adhering to treatment were not significant.
FIGURE 1.
Barriers to antiretroviral treatment adherence in the past 30 days for persons of lower and higher literacy; significant differences indicated by +p < .06, *p < .05, **p < .01.
DISCUSSION
Results of this study must be interpreted in light of its methodologic limitations. The study was conducted in a community setting rather than a clinic. The advantage of studying persons who may be marginally connected to HIV treatment services and not enrolled in drug trials came at the cost of relying on self-report measures of health status and treatment regimens. Although our measures appeared internally reliable (e.g., people who were nonadherent had lower CD4 cell counts and were less likely to have undetectable viral loads), the degree to which participants provided accurate health information is unknown. Although HIV symptoms and stage of disease were not associated with health literacy, we did not formally assess neurocognitive impairment in this study, a factor that could interfere with remembering treatment regimens and may have affected performance on the literacy scales. Another factor that may have influenced our results is the differential treatment that providers may give to persons with low literacy skills. For example, providers may not give the same level of detailed instructions to patients who experience comprehension difficulties. Future research should therefore examine different practices of instructing patients with low and higher literacy. In addition, we only collected measures at a single assessment session, prohibiting us from making the kind of predictions over time that prospective studies afford. Finally, our sample was partly recruited through flyers describing the study, a method that may have failed to reach people of the lowest literacy; thus, our sample may have underrepresented this group of people who may be experiencing the greatest difficulty adhering to medication regimens. Our findings must therefore be considered a conservative estimate of literacy and its association with antiretroviral adherence among people living with HIV-AIDS.
One in five persons on HAART in the current study were nonadherent to their treatment regimen in the previous 2 days, a rate similar to that in other studies.18 As has occurred with multiple drug-resistant strains of tuberculosis that resulted from irregular and inconsistent use of antibiotics,19 nonadherence to HAART threatens to undermine the promise of effective HIV-AIDS treatments. Failure to adhere to treatment schedules is particularly troublesome with protease inhibitors because of HIV’s ability to rapidly develop resistance to these drugs. Virus-resistant mutations can develop after only days of intermittent protease inhibitor use, and reverse transcriptase inhibitors are not much more forgiving. Identifying factors associated with nonadherence to antiretroviral therapy must, therefore, inform interventions designed to assist people undergoing HAART.
The current study found that factors associated with nonadherence to other treatments were also associated with nonadherence to HAART. Univariate analyses indicated that ethnic minorities, persons who perceived receiving less social support, and those experiencing greater emotional distress were more likely to have been nonadherent in the past 2 days. Surprisingly, substance use and attitudes toward providers were not significantly associated with adherence in this study. However, our measures of substance use reflected global patterns of use for the previous 3 months whereas adherence was defined over a 2-day period. Thus, the association between substance use and treatment adherence may have been obscured by our desynchronized measures.
Both univariate and multivariate tests showed that years of education and health literacy were significant independent predictors of treatment adherence. People of lower education and lower literacy were between 3 and 4 times more likely to have missed a dose of antiretroviral medications in the previous 2 days. Income level, ethnic background, and HIV disease progression did not account for these associations. Consistent with these findings, people of lower literacy were more likely to have missed a dose of their medications because they were confused about their treatment regimen, were depressed, or desired to cleanse their body of treatments. Thus, we conclude that education level and, perhaps more importantly, health literacy are important in adherence to combination antiretroviral regimens, and both must be considered in designing patient materials and strategies for enhancing antiretroviral treatment adherence. Low education itself is a reasonable marker for potential nonadherence. However, for persons with at least 12 years of education, it is necessary to assess their literacy to identify the risk of nonadherence.
Although treatment regimens for HIV-AIDS are becoming less complex with the advent of combined drugs in single medications and through twice-a-day and once-a-day dosing, literacy will most likely remain an important barrier to long-term treatment adherence even for the simplest regimens.14,15 Interventions to increase adherence to treatment schedules have relied on daily calendars, outlines of meal schedules, reminder notes, condensed instructions for dietary considerations, and charts for dosing schedules.20,21 Devices such as timers and alarms have also been suggested to increase adherence to antiretroviral therapy.22 Unfortunately, many of these strategies require literacy skills and other resources that people who may be at greatest risk of nonadherence lack. Also, persons with low literacy skills were no more likely to experience forgetfulness or distractions in missing their medications than were persons of higher literacy, suggesting that memory aides may not address the intersection between low literacy and nonadherence. Therefore, interventions to assist people in adhering to antiretroviral therapies must be adapted for persons of lower literacy with specific attention given to relevant treatment barriers.
People of lower literacy may benefit from pictorial displays of their medications, accurate in color and size, with graphic illustration of the instructions including the number of pills to be taken, and at what times. In addition, videotapes tailored to different levels of comprehension may provide a more effective medium than pamphlets and brochures for educating patients about their treatments. Intensive case management and assertive assistance programs may be required for those persons with the greatest difficulty understanding their treatment regimen and the importance of adherence.23 Finally, and perhaps most importantly, primary care providers must tailor their instructions to match the capabilities of their patients. For example, low education and low literacy suggest the importance of including concrete practice exercises with lots of repetition. The necessity of attending to low literacy in patients undergoing HIV-AIDS treatment will become increasingly pressing as the HIV epidemic spreads to impoverished areas of developed countries and as antiretroviral treatments become increasingly available in developing countries. Designing effective interventions to promote treatment adherence in persons of lower literacy must, therefore, be considered a high priority in national AIDS treatment agendas.
Acknowledgments
The authors thank the AIDS Survival Project of Atlanta for its assistance with data collection. National Institute of Mental Health (NIMH) grant R01-MH57624 and CAIR grant P30 MH52776 supported this research.
REFERENCES
- 1.Ho DD. Therapy of HIV infections: problems and prospects. Bull NY Acad Med. 1996;73:37–45. [PMC free article] [PubMed] [Google Scholar]
- 2.Mehta S, Moore RD, Graham NMH. Potential factors affecting adherence with HIV therapy. AIDS. 1997;11:1665–70. doi: 10.1097/00002030-199714000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Samet JH, Libman H, Steger KA, et al. Compliance with zidovudine therapy in patients infected with human immunodeficiency virus, type-1: a cross-sections study in a municipal hospital clinic. Am J Med. 1992;92:495–502. doi: 10.1016/0002-9343(92)90746-x. [DOI] [PubMed] [Google Scholar]
- 4.Aversa SL, Kimberlin C. Psychosocial aspects of antiretroviral medication use among HIV patients. Patient Educ Couns. 1996;29:207–19. doi: 10.1016/0738-3991(96)00910-x. [DOI] [PubMed] [Google Scholar]
- 5.Morse EV, Simon PM, Coburn M, Hyslop N, Greenspan D, Balson PM. Determinants of subject compliance within an experimental anti-HIV drug protocol. Soc Sci Med. 1991;32:1161–7. doi: 10.1016/0277-9536(91)90093-r. [DOI] [PubMed] [Google Scholar]
- 6. Hecht FM. Adherence to HIV Treatment. Presented at the meeting of Clinical Care of the AIDS Patients, San Francisco, Calif, December 1997.
- 7.Perry S, Ryan J, Ashman T, Jacobsberg L. Refusal of zidovudine by HIV-positive patients. AIDS. 1992;6:514–5. [PubMed] [Google Scholar]
- 8.Rabkin JG, Chesney M. Treatment adherence to HIV medications: the Achilles heel of the new therapeutics. In: Ostrow D, Kalichman S, editors. Behavioral and Mental Health Impacts of New HIV Therapies. New York, NY: Plenum Press; 1999. [Google Scholar]
- 9.Ickovics JR, Meisler AW. Adherence in AIDS clinical trials: a framework for clinical research and clinical care. J Clin Epidemiol. 1997;50:385–91. doi: 10.1016/s0895-4356(97)00041-3. [DOI] [PubMed] [Google Scholar]
- 10.Stall R, Hoff C, Coates TJ, et al. Decisions to get HIV tested and to accept antiretroviral therapies among gay/bisexual men: implications for secondary prevention efforts. J AIDS Hum Retrovir. 1996;11:151–60. doi: 10.1097/00042560-199602010-00006. [DOI] [PubMed] [Google Scholar]
- 11.Singh N, Squier C, Sivek M, Wagener M, Nguyen M, Yu VL. Determinants of compliance with antiretroviral therapy in patients with human immunodeficiency virus: prospective assessment with implications for enhancing compliance. AIDS Care. 1996;8:261–9. doi: 10.1080/09540129650125696. [DOI] [PubMed] [Google Scholar]
- 12.Broers B, Morabia A, Hirschel B. A cohort study of drug users’ compliance with zidovudine treatment. Arch Intern Med. 1994;154:1121–7. [PubMed] [Google Scholar]
- 13.O’Connor PG, Samet JH. The substance-using human immunodeficiency virus patient: approaches to outpatient management. Am J Med. 1996;101:435–44. doi: 10.1016/S0002-9343(96)00200-8. [DOI] [PubMed] [Google Scholar]
- 14.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10:537–41. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 15.Williams MV, Parker RM, Baker DW, et al. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274:1677–82. [PubMed] [Google Scholar]
- 16.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- 17. Cella D. The Functional Assessment of Cancer Therapy Scales and the Functional Assessment of HIV Infection Scale, Version 3. Chicago, Ill: Rush–Presbyterian–St. Lukes Medical Center. 1994.
- 18. Hecht FM, Colfax G, Swanson M, Cesney M. Adherence and effectiveness of protease inhibitors in clinical practice. Presented at the 5th Annual Retroviral Conference, Chicago, Ill, 1998.
- 19.Hopewell PC. Tuberculosis in persons with human immunodeficiency virus infection. In: Sande MA, Volberding PA, editors. The Medical Management of AIDS. 5th ed. Philadelphia, Pa: Saunders; 1997. pp. 311–26. [Google Scholar]
- 20.Sikkema K, Kelly J. Behavioral medicine interventions can improve quality of life and health of persons with HIV disease. Ann Behav Med. 1996;18:40–8. doi: 10.1007/BF02903938. [DOI] [PubMed] [Google Scholar]
- 21.Kalichman SC. Understanding AIDS: Advances in Research and Treatment. 2nd ed. Washington, DC: American Psychological Association; 1998. [Google Scholar]
- 22.Besch CL. Compliance in clinical trials. AIDS. 1995;9:1–10. doi: 10.1097/00002030-199501000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Dixon L, Weiden P, Torres M, Lehman A. Assertive community treatment and medication compliance in the homeless mentally ill. Am J Psychiatry. 1997;154:1302–4. doi: 10.1176/ajp.154.9.1302. [DOI] [PubMed] [Google Scholar]