Abstract
OBJECTIVE
To examine the influence of utilization review and denial of specialty referrals on patient satisfaction with overall medical care, willingness to recommend one’s physician group to a friend, and desire to disenroll from the health plan.
DESIGN
Two cross-sectional questionnaires: one of physician groups and one of patient satisfaction.
SETTING
Eighty-eight capitated physician groups in California.
PARTICIPANTS
Participants were 11,710 patients enrolled in a large California network-model HMO in 1993 who received care in one of the 88 physician groups.
MEASUREMENTS AND MAIN RESULTS
Our main measures were how groups conducted utilization review for specialty referrals and tests, patient-reported denial of specialty referrals, and patient satisfaction with overall medical care. Patients in groups that required preauthorization for access to many types of specialists were significantly (p≤ .001) less satisfied than patients in groups that had few preauthorization requirements, even after adjusting for patient and other group characteristics. Patients who had wanted to see a specialist in the previous year but did not see one were significantly less satisfied than those who had wanted to see a specialist and actually saw one (p < .001). In addition, patients who did not see a specialist when desired were more likely to want to disenroll from the health plan than patients who saw the specialist (40% vs 18%, p≤ .001) and more likely not to recommend their group to a friend (38% vs 13%, p≤ .001).
CONCLUSIONS
Policies that limited direct access to specialists, and especially denial of patient-desired referrals, were associated with significantly lower patient satisfaction, increased desire to disenroll, and lower likelihood of recommending the group to a friend. Health plans and physician groups need to take these factors into account when designing strategies to reduce specialty care use.
Keywords: patient satisfaction, access to specialists, gatekeeping, utilization management, managed care
Few managed care strategies to reduce costs have raised as much controversy as those aimed at restricting access to specialists.1–3 This access restriction positions the primary care physician as both the main provider of health care services and the physician charged with controlling decisions about whether a specialty referral is necessary. Some 40% of Americans obtain their health care under such “gatekeeping” arrangements.4 In some cases gatekeeping is augmented with utilization review, so that even after primary care physicians approve or initiate a referral, they must still have the referral preauthorized.5 More recently, there has been a growth of point-of-service plans and “open-access” HMOs, which allow patients direct access to specialists, albeit with a higher copayment than patients would pay with a referral from the primary care provider.6 However, such systems typically use gatekeeping arrangements as well.
Gatekeeping and utilization review strategies are based on the idea that reducing patient access to specialists and specialized services reduces the opportunity for further medical resource use and may protect patients from overtreatment.7 Although previous studies have examined the influence of specialty differences on the quality and costs of care,8–16 we could not locate any studies of the influence of utilization review methods or denial of specialty referral on patient satisfaction with care.
Patient satisfaction is an important tool to measure the performance of providers, managed care organizations, and health care systems. Results of patient satisfaction surveys have been used in many ways, including to identify quality problems, to track the performance of medical groups and health plans, to modify capitation rates, and to make health care purchasing decisions.17 Although satisfaction alone is not a sufficient measure of patient outcomes, there are several important reasons to measure and improve patient satisfaction with medical care. First, patient satisfaction is an important aspect of health care quality and can be used for monitoring at least some aspects of quality.18,19 High levels of satisfaction predict important aspects of care including the likelihood of following medical advice,20 the strength of the patient–physician relationship,21,22 and continuity of care. In addition, patients who are dissatisfied are more likely to switch physicians and medical groups,23 which could lead to decreased viability of the medical practice.24,25 Health plans are also using satisfaction ratings to modify payment and capitation rates, provide bonuses, and identify outliers, at both the medical group and individual physician levels.17 Finally, purchasers are basing contracting decisions at least in part on patient satisfaction reports. Indeed, the National Council for Quality Assurance (NCQA) has recently required a standardized patient satisfaction survey as part of the Health Plan Employer Data and Information Set (HEDIS 3.0, 1997) for plans seeking NCQA accreditation.
Although many health care organizations would like to improve patient satisfaction, in order to do so, the plan or group must identify modifiable sources of dissatisfaction and understand how their management strategies influence satisfaction. For example, some studies have demonstrated that patients enrolled in managed care plans are less satisfied with their access to specialty care than those enrolled in fee-for-service arrangements.24,26–28 However, these studies did not examine whether the specific management strategies used to control access to specialty services influenced satisfaction. Building on our study of utilization management in capitated physician groups,5 we examined the influence of physician groups’ utilization review mechanisms and denial of specialty referrals on patient satisfaction with overall medical care provided by the groups, willingness to recommend one’s group to a friend, and desire to disenroll from the health plan.
METHODS
Setting
In late 1993, we surveyed medical directors from all 133 physician groups (medical group practices and independent practice associations [IPAs]) having capitated contracts with one of the largest network-model health plans in California regarding their utilization management and quality assurance practices.5,29 Both medical group practices and IPAs care for patients covered under many different managed care contracts, as well as those covered through more traditional forms of insurance. The physician groups are paid a set fee for patients who enroll in their groups through capitated contracts. From these set fees, the groups cover all services that are used by patients and are included in the contract. In addition, the physician groups retain control over how they reimburse their own physicians and assume the primary responsibility for utilization management.
The study methods and administrative structures of the 94 groups (71%) that responded are detailed elsewhere.5 All of the physician groups had capitated contracts with multiple health plans. The capitated rate covered all primary care services and outpatient specialty services. Some groups had capitated contracts that covered all services. In addition, physicians in all of the groups continued to see some proportion of patients who were not covered by capitated contracts. All groups monitored access to specialty care through gatekeeping and utilization review. Utilization review consisted primarily of preauthorization of specialty referrals and tests, which reflected that someone in the group needed to authorize a referral submitted by the primary care doctor before a service (e.g., consultation) could be performed. Preauthorization policies were set individually by each group, so the intensity of preauthorization varied across groups, with some groups requiring preauthorization for nearly all specialty visits, tests, and procedures, and other groups requiring preauthorization for only selected specialty visits and tests.5 Nonetheless, within an individual group, preauthorization policies were the same for all health plan contracts (except when a health plan specified that patients were to have direct access to certain specialists). Further, groups reported a range of average denial rates for preauthorization as well as a wide range of turnaround times for preauthorization referrals. Responding groups did not differ from those not responding to the survey with respect to size or type.5
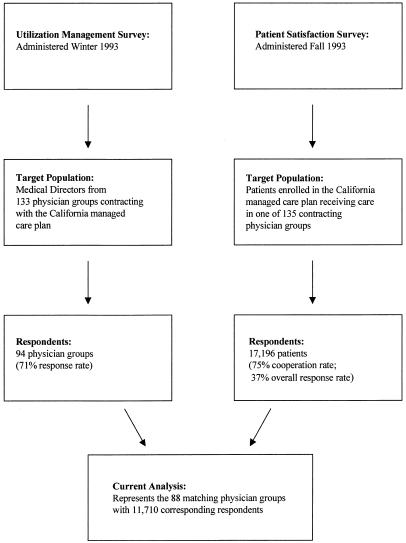
In order to examine the influence of preauthorization on patient satisfaction, we obtained 1993 patient satisfaction data from the same California health plan. This plan surveyed the satisfaction of members enrolled in all of the groups with which they had contracts (135 at the time of the survey, which took place approximately 3 months before the utilization management survey). Of the 94 physician groups for which we had utilization management data, 88 were the same as groups for which the health plan had collected patient satisfaction data (Fig. 1).
FIGURE 1.
Data collection for the two surveys used in the current analysis.
Survey Design and Data Collection
Satisfaction data were collected by telephone interviews with patients enrolled in the California health plan. An external survey research firm hired by the health plan conducted the telephone survey in the fall of 1993. Survey participants were persons aged 18 years or older who had used medical services at least once in the previous year. To facilitate comparisons of patient satisfaction among the groups contracting with the plan, the plan attempted to obtain responses from 140 randomly sampled patients from each group. In physician group practices with more than one site, the size of the sample from each site was proportional to the total number of enrollees at that site.
The survey was based on the Group Health Association of American (GHAA) questionnaire of consumer satisfaction.30 The survey included a question assessing satisfaction with overall care in the medical group: “All things considered, how do you rate the medical care you and your family receive from your participating medical group?” To ease telephone administration, participants were asked to rate elements of their medical care using a scale of 1 to 10 (1 being unacceptable and 10 superior or excellent) rather than the 5-point Likert-type scale (from poor to excellent) used in the GHAA survey. Respondents were also asked if they would be willing to recommend their physician group to a friend and if they would change from the health plan given the opportunity. In addition, the survey included questions about whether or not patients felt they had needed to see a specialist in the previous year and whether they had obtained specialty referral if they desired it. These questions read, “In the past 12 months, were there any times that you wanted to see a specialist, even after you discussed your problem with your primary care doctor?” and “In the past 12 months, when you wanted to see a specialist did you get to see one?” A final specialty question asked about the reasons for not seeing a specialist if desired. The survey also contained five demographic items and two items on previous insurance. Further information on survey design and administration is reported elsewhere.25
The survey firm completed as many telephone calls as necessary to obtain as close to 140 respondents from each group as possible. In 20 groups, fewer than 100 patients were successfully surveyed (range of patients surveyed per group, 24–140; median, 140). Of the 52,525 attempted calls, 6,403 of the potential participants did not meet eligibility criteria and 23,096 were to wrong or disconnected numbers. Of those contacted and eligible, 17,196 (75%) completed the survey, while 5,830 persons refused.
For the utilization management survey of the physician groups, data were collected using two detailed self-report questionnaires focusing on organizational characteristics of the physician groups and the use of utilization management techniques and quality assurance methods. The methods used to collect these data and subsequent analyses have been previously reported.5,29 Of the 17,196 respondents who completed the satisfaction survey (representing all 135 groups), we had the corresponding physician groups data for 11,710 enrollees (from the 88 matching groups) (Fig. 1). The analyses presented in this report are based on this sample of 11,710, linked to the group utilization data by a variable in both data sets that identified the physician group.
Analysis
We constructed two multivariate models to examine the influence of utilization review and denial of specialty referrals on patient satisfaction with the overall medical care provided by their physician group. The first model (all respondents) was estimated for all patients who answered the survey, and the second model (specialist desired) was estimated for only those patients who reported that they had wanted to see a specialist in the past year (n = 4,567). The second model allowed us to further examine the influence of utilization review and denial on those who felt they needed specialty care.
The dependent variable in both models was the single measure of overall satisfaction with medical care, described above under Survey Design and Data Collection. The four main independent variables in both models consisted of three factors related to how the group performed utilization review (preauthorization intensity scale, referral denial scale, and preauthorization turnaround time) and one factor related to patient-reported denial of specialty referrals. The first independent variable, the preauthorization intensity scale, reflects the degree of rigor with which groups institute their preauthorization programs. To construct this scale, we summed responses from the physician group utilization management survey to four multi-item questions regarding (1) the degree of importance placed on preauthorization of elective admissions, certain ambulatory procedures, and specialty referrals; (2) the mechanism of referral to 11 listed specialists (primary care physician referral only, primary care referral and preauthorization of the group, or self-referral only); (3) the mechanism of referral for nine listed ambulatory tests and procedures (whether or not preauthorization was required for specific nonurgent ambulatory testing); and (4) how often preauthorization was required for urgent specialty referrals, tests, or procedures. The scale was standardized to have a mean (SD) of 50 (10). The questions in the scale and the scoring used to construct the scale are provided in Appendix A. To illustrate, a group at the 10th percentile of preauthorization intensity (lowest 10%, corresponding to a score of 35) required preauthorization for 3 of the 11 listed specialty consultations and three of the nine nonurgent ambulatory tests and procedures. In contrast, a group at the 90th percentile (highest 10%, corresponding to a score of 61) required preauthorization for all 11 specialty referrals and six of the nine nonurgent tests and procedures.
Similarly, we constructed the referral denial scale, our second independent variable, by summing answers in the group utilization management survey to four items regarding how often the group denied urgent or nonurgent specialty consultations, tests or procedures. This scale was also standardized to have a mean (SD) of 50 (10). To illustrate, groups at the 10th percentile in the denial scale (corresponding to a score of 38) reported denying 2% to 5% of nonurgent specialty consultations, while groups in the 90th percentile (a score of 63) reported denying 11% to 15% of specialty consultations. The preauthorization turnaround time, our third independent variable, was the average number of days that the group reported it took to approve or deny a nonurgent specialty referral. The fourth main independent variable, from the patient satisfaction survey, was whether or not the patient received a specialty referral when desired. This variable categorized patients as those who saw a specialist in the past year if desired (reference group), those who did not see a specialist despite wanting to, and those who reported not wanting to see a specialist.
We controlled the regressions for both physician group and patient characteristics. Physician group characteristics consisted of both the number of primary care physicians (a reflection of group size) and the number of years each organization had existed under its current name. The logarithmic transformation of these two variables was used to provide a better fit for the regression models. Patient characteristics consisted of two continuous variables (age and the number of times the patient used any medical services in the past 12 months), three multiple category variables (household income, education, and previous insurance), and two dichotomous variables (race and gender). We found that increasing age was negatively associated with satisfaction from age 18 to 50, but positively associated with satisfaction after age 50. To adjust for this change of the relation between age and patient satisfaction at age 50, we included an age indicator variable (18–50; 51 and older) in the regressions to allow for best fit in the models.
Because we sampled patients at the physician group level, and because patients in the same group might report scores that are more similar to one another than patients in different groups, we adjusted for this possible clustering effect using the Huber/White cluster correction.31,32 This correction utilizes the intraclass correlation and is proportional to the size of this correlation, thus correcting for any underestimation in the models’ standard errors. Further, because the plan sampled an equal number of plan enrollees per physician group regardless of how many plan enrollees were actually members of the group, we estimated regression models that were weighted by the actual number of enrollees from the health plan in each physician group. There were no significant differences between the results of weighted regressions and unweighted regressions. Therefore, we only present results from unweighted models with the correction for clustering.
There were no missing data for the physician group information and utilization management variables. All of the patient variables had fewer than 5% missing data, except income, which had 15% missing. To reduce bias, missing data for age, race, income, education, and previous insurance were replaced using a regression imputation technique. To examine whether satisfaction scores were different for patients with imputed data, we included in the models a variable indicating whether or not the record contained any imputed values. This variable was significant in both models and denoted that those with missing data had generally lower satisfaction scores than those without any missing data. However, regression models that ignored missing data were very similar to those that included the imputed values.
Regression models allow us to evaluate whether certain variables are significantly associated with the outcome of interest, but it is often difficult to understand from the model how different values of an independent variable influence the dependent variable. Using the model to calculate the value of the dependent variable for different values of an independent variable (e.g., high and low values of a continuous variable or alternate values of a categorical variable) allows one to appreciate the extent of change in the dependent variable for a change in the independent variable. Therefore, to illustrate more clearly the magnitude of the associations between patient satisfaction and both preauthorization intensity and whether or not the patient reported seeing a specialist, we used the all respondents model to calculate predicted mean overall satisfaction with medical care scores for the 10th percentile (score = 35.07) and 90th percentile (score = 61.06) of preauthorization intensity and for whether or not a patient reported seeing a specialist when desired. For these calculations we held all values of the other independent variables constant at their means.
In order to anchor our analysis of global patient satisfaction on easily understood and relevant factors, we assessed the influence of not obtaining a specialty referral when desired on two other indicators of patient satisfaction with care: desire to leave the health plan and willingness to recommend the physician group to a friend. Using the same independent variables and covariates from the all respondents model and correcting for clustering, we constructed two logistic regression models with the dichotomous dependent variables being wanting to leave the plan (yes/no) and willingness to recommend the group to a friend (yes/no). Because adjusting for covariates did not change the effect of receiving a specialty referral on the two dependent variables, we present the unadjusted percentages (see Table 4) All analyses were performed using STATA, Release 5 (Stata Corp., College Station, Tex, 1997).
Table 4.
Association Between Wanting to See a Specialist and Patient Satisfaction with Medical Care, Desire to Leavethe Health Plan, and Willingness to Recommend Their Group to a Friend for 11,532 Patients Who Responded tothe Satisfaction Survey
| Patient Category | n | Predicted Satisfaction with Medical Care Score,Mean (95% CI) | Patients Wanting to Leave the Health Plan, % | Patients Who Would Not Recommend Groupto a Friend, % |
|---|---|---|---|---|
| Patients who saw a specialist if desired | 2,858 | 8.22 (8.12, 8.32) | 18.0 | 12.8 |
| Patients who did not see a specialist if desired | 1,709 | 6.58*(6.46, 6.70) | 39.6* | 37.9* |
| Patients who did not want to see a specialist | 6,965 | 8.32 (8.24, 8.40) | 14.8† | 11.3 |
Patients who wanted to see a specialist and did not were less satisfied, more likely to want to leave the plan, and less likely to recommend the group to a friend than patients who wanted to see a specialist and did (p < .001).
Patients who did not want to see a specialist were less likely to want to leave the plan than patients who wanted to see a specialist and did (p < .001).
RESULTS
The characteristics of respondents are reported in Table 1. Sixty-five percent of respondents were women, 70% were white, and 41% had completed college. The mean age was 41 and the median was 39. Forty percent of patients reported having wanted to see a specialist in the previous year.
Table 1.
Characteristics of 11,710 Patients Who Responded to the Health Plan Satisfaction Survey
| Characteristic | Value* |
|---|---|
| Gender (n = 11,710) | |
| Female | 7,646 (65%) |
| Male | 4,064 (35%) |
| Race (n = 11,475) | |
| White | 8,012 (70%) |
| Nonwhite | 3,463 (30%) |
| Education (n = 11,585) | |
| High school or less | 3,072 (27%) |
| Some college | 3,727 (32%) |
| College graduate | 4,786 (41%) |
| Previous insurance (n = 11,574) | |
| Managed care | 4,929 (43%) |
| Indemnity | 4,706 (41%) |
| Unspecified type | 357 (3%) |
| No insurance | 1,582 (14%) |
| Desire to see specialist (n = 11,553) | |
| Yes | 4,615 (40%) |
| No | 6,938 (60%) |
| Household income–1992 (n = 10,001) | |
| Under $20,000 | 913 (9%) |
| $20,000–$39,999 | 3,331 (33%) |
| $40,000–$79,999 | 4,198 (42%) |
| Over $75,000 | 1,559 (16%) |
| Age, in years (n = 11,513) | 41.2 |
| (32, 39, 49) | |
| Number of times services used in past 12 months (n =11,710 ) | 7.1(2, 4, 9) |
Values are presented as n(%) for categorical variables and as mean (25th, 50th, and 75th percentiles) for continuous variables.
The 88 physician groups comprised 43 IPAs and 45 medical group practices. These groups had existed under their current names an average of 17 years and had a median of 40 primary care physicians. Average turnaround time for preauthorization approval was 4.4 days (SD = 4.2 days) with a range of 0 to 35 days. Approximately 89% of groups reported denying referrals, procedures, or tests less than 10% of the time. Other details about these groups have been previously published.5,29
The overall satisfaction measure had a mean (SD) of 8.03 (2.03). The estimated reliability of the measure at the physician group level using a one-way analysis of variance model, with physician group as the between factor,33 was 0.77. Both the preauthorization intensity scale and the referral denial scale exhibited good reliability at the physician group level (internal consistency reliability = 0.91). The observed range of the preauthorization intensity scale was 26 to 65, while the denial index scale scores ranged from 36 to 76.
The results of the all respondents regression model predicting overall patient satisfaction with the medical care provided by the physician group are listed in Table 2. This model is based on the data provided by the 11,523 respondents who rated their overall satisfaction. Increasing preauthorization intensity, but not group referral denial or referral turnaround time, was significantly related to decreased satisfaction with medical care. Further, patients who had wanted to see a specialist in the previous year but did not see one were significantly less satisfied than those who saw a specialist when they had wanted to. Patients who reported not wanting to see a specialist at all in the previous year were more satisfied than patients who wanted to see a specialist and saw one. This model explained 13% of the variance in overall satisfaction with medical care.
Table 2.
Regression Model Predicting Satisfaction with Medical Care for 11,532 Health Plan Enrollees(All Respondents Model) Who Respondedto the Satisfaction Survey (R2= .13)
| Variable* | Parameter Estimate | p Value |
|---|---|---|
| Did not see specialist when desired (vs saw specialist)† | −1.645 | <.001 |
| Specialty referral not desired (vs saw specialist)‡ | 0.100 | .033 |
| Preauthorization intensity scale§ | −0.016 | <.001 |
| Referral denial scale | −0.002 | .552 |
| Preauthorization turnaround time | −0.000 | .984 |
| Number of visits | 0.010 | <.001 |
| Female | 0.224 | <.001 |
| Previous insurance indemnity (vs managed care) | −0.184 | <.001 |
| Previous insurance none (vs managed care) | 0.033 | .522 |
| Education ≤high school (vs>high school) | 0.188 | <.001 |
| Higher income | −0.076 | <.001 |
| White | −0.074 | .124 |
| Age 18–99∥ | 0.008 | <.001 |
| Age ≤50∥ | −0.006 | <.001 |
| Type of physician group medical group practice (vs IPA) | −0.250 | .002 |
| Years group in existence | 0.010 | .784 |
| Number of primary care physicians in physician group | 0.009 | .882 |
| Intercept | 9.210 | — |
Main independent variables are in boldface.
Satisfaction is lower for persons who wanted to see a specialist and did not compared with those who wanted to see a specialist and did.
Satisfaction is greater for persons who did not want to see a speciaist compared with those who wanted to see a specialist and did.
Satisfaction decreases with greater preauthorization intensity.
Satisfaction increases with age for persons aged 51 years or older and decreases with age for those aged 18–50 years.
The results for the regression model predicting overall satisfaction with medical care for patients who reported having wanted to see a specialist in the past year (specialist desired model, n = 4,567) were very similar to those of the all respondents model. The specialist desired model explained 17% of the variance in satisfaction with overall medical care. The variable indicating whether or not the patient saw a specialist when desired explained 13% of the variance in overall satisfaction, with patients who did not see a specialist when desired being significantly less satisfied than those who did see a specialist. The preauthorization intensity score remained a significant predictor of satisfaction.
Predicted mean satisfaction scores based on the all respondents model for the 10th and 90th percentiles of preauthorization intensity and for whether or not the patient saw a specialist are presented in Table 3. Satisfaction scores at the 10th and 90th percentiles of preauthorization intensity differed by almost one-fourth SD (0.43 units on a scale of 1 to 10). Predicted satisfaction scores for patients who wanted to see a specialist and did (8.2) differed from those for patients who wanted to see a specialist but did not (6.6) by two-third SD (1.6 units on a scale of 1 to 10).
Table 3.
Predicted Mean Satisfaction with Medical Care Scores for Significant Utilization Management Variables*
| Utilization Management Variable | Satisfaction Predicted with Medical Care Scores (Adjusted), Mean (95% CI) |
|---|---|
| Preauthorization intensity scores | |
| 10th percentile (35.07) | 8.27 (8.15, 8.39) |
| 90th percentile (61.06) | 7.84 (7.72, 7.96) |
| Desire and ability to see specialist | |
| Patients who saw a specialist if desired | 8.22 (8.12, 8.32) |
| Patients who did not see a specialist if desired | 6.58 (6.46, 6.70) |
| Patients who did not want to see a specialist | 8.32 (8.24, 8.40) |
Mean satisfaction scores were calculated for alternate values of utilization management variables while holding all other variables constant at the mean, using the model presented in Table 2.
Table 4 portrays the relation between reported access to specialty care and (1) predicted overall satisfaction scores, (2) desire to disenroll, and (3) willingness to recommend the plan to a friend. Eighteen percent of patients who reported seeing a specialist said that, given the opportunity, they would leave the health plan. In contrast, 40% of patients who had not seen a specialist when desired wanted to disenroll. Similarly, 13% of patients who saw a specialist said they would not recommend their group to a friend compared with 38% of patients who had not seen a specialist.
DISCUSSION
Our study combines data collected at the group level (utilization review variables and group characteristics) with patient satisfaction and reported access to care in these same groups at approximately the same time. We show that overall satisfaction with the medical care patients received in their physician groups is influenced by both the denial of specialty referrals and the intensity of the preauthorization programs instituted in the groups. Forty percent of respondents reported that they had wanted to be referred to a specialist in the previous year. For these patients, whether or not they actually saw the specialist was the most important determinant of satisfaction. In fact, this one variable explained a greater percentage of the variance in overall satisfaction than all other model variables combined. Further, patients who did not see the specialist were much less likely to recommend their group to a friend and much more likely to want to disenroll from the health plan.
Because preauthorization intensity is a reflection of the different types of specialty referrals and tests that must go through the group’s utilization review mechanism, patients in groups with higher intensity are more likely to encounter the preauthorization process. In contrast, neither the referral denial scale nor the turnaround time, which are reflections of group-reported average denial rates and turnaround times, influenced satisfaction. In these physician groups, average reported denial rates were less than 10% for the majority of groups.5 Although our study showed that the individual experience with denial affects satisfaction, it is not surprising that individual patient satisfaction is not independently associated with group-reported denial averages, especially when overall denial rates are low.
Our analysis is limited to patients in California physician groups whose medical director answered an initial survey about utilization management mechanisms; therefore its results are not necessarily generalizable to other groups. We cannot comment on the utilization management techniques in the groups who did not respond to our initial survey. However, the mean overall satisfaction score of patients from these nonresponding groups was very similar to the mean satisfaction score of patients whose physician groups did respond (8.05 vs 8.03, p = .684). The regression models accounted for 13% to 17% of the variance in satisfaction with medical care. Similar amounts of variance in patient satisfaction have been accounted for in previous studies that included sociodemographic and practice organizational variables.34–36 Although it is possible that the association of preauthorization intensity with satisfaction would become nonsignificant if other (unmeasured) variables were added, the model does include sociodemographic variables previously shown to be associated with patient satisfaction. In future studies it may be of particular importance to include variables associated with convenience of care (e.g., distance to provider, wait times), which have been shown to be highly associated with desire to leave a plan.25
Although each group may provide care to members of many health plans, our patient satisfaction data pertain to one health plan only and do not include a measure of health status. We did include a variable reflecting the number of times the patient used services in the past year. Though an imperfect proxy for health status, several previous studies have shown that utilization is significantly correlated with health status.37,38 Our measure of overall satisfaction is based on one item, but this item was reliable at the physician group level. Further, these data are from 1993, and it is likely that both management strategies and patient expectations from managed care organizations continue to change. Nonetheless, the desire to control specialty utilization through gatekeeping and utilization management continues to be a highly prevalent but controversial aspect of managed care. In addition, although the cooperation rate for the study was high, the overall response rate was limited by a large proportion of wrong and disconnected numbers. Specifically, responses were obtained from 37% of potentially eligible respondents (we do not know how many persons with disconnected numbers were actually eligible for the study). Therefore, the possibility of a systematic bias in our findings exists if the patients whom the plan failed to reach had different experiences regarding utilization review and referral denial than the responding patients. The survey research firm did not gather characteristics of nonrespondents, nor did it track differences in response rates by physician group. Finally, we cannot comment on the medical necessity of the desired referral or on the type of referral requested. It is possible that patients who experienced the greatest dissatisfaction regarding preauthorization and denial of a desired referral had unreasonable expectations of their doctor or group regarding specialty care.
Despite these limitations, our results are intriguing because they do show an association between group-level management policies and overall patient satisfaction. Because patient dissatisfaction has been linked to changing physicians,23 disenrollment,39 and not following medical advice,19 and because our study shows that patients who do not obtain desired specialty referrals are also less likely to recommend their group to a friend and more likely to disenroll, managed care organizations may want to examine their policies regarding the intensity of their preauthorization programs and denials for specialty referral. Despite explanations from their primary care physicians regarding the appropriateness of specialty care for a particular problem, certain patients may nonetheless perceive that they are denied necessary care, and this perception may have consequences not only for their health behaviors but also for the patient–physician relationship.40 Patients denied specialty care were clearly less satisfied; however, 60% of them would still recommend their group to a friend and did not want to disenroll. It is possible that the nature of the request was different for these patients. It is also possible that the doctors of these patients found a more acceptable way to communicate the denial or offer alternative options.
Should we infer from this study that patients should be given open access to specialty care when they want it? If the main goal is to optimize patient satisfaction in the short run, then the answer may well be yes. Indeed, many health plans are already responding to this perceived dissatisfaction by creating open-access or point-of-service plans. However, the optimal long-term approach is not clear, and important research questions remain to be addressed and answered. For example, would effective communication approaches between the patient and primary care physician surrounding perceived need for specialty referral mitigate some of the dissatisfaction? Could balanced economic incentives (for primary care physicians, specialists, and patients), as opposed to capitation only at the level of primary care, provide open access without either dramatically increasing utilization or promoting underuse of specialty procedures?
In the long run, health plans, medical groups, and physicians will need to decide how much dissatisfaction they are willing to tolerate. This will at least in part depend on how much dissatisfaction “costs.” Health plans are increasingly linking physician compensation to patient satisfaction. Therefore, low satisfaction scores may directly influence physician income.17 Further, patients who do not follow medical advice because of dissatisfaction or an impaired relationship with their physicians may cost the group and plan more over the course of time. In addition, turnover from disenrollment is generally costly, from both the physician group and plan point of view. The long-term answer to both improving the satisfaction of consumers and enhancing the appropriate utilization of primary care and specialty services may lie with a “team approach,”41 which incorporates generalists, specialists, and patients. Such an approach could balance economic incentives for generalists and specialists, focus on education for physicians and patients, incorporate some degree of utilization review centering on inappropriate overutilization of specialty services, and establish quality monitoring mechanisms that concentrate on underutilization. Americans have learned to expect freedom of choice within the medical care system. Managed care organizations, physicians, and consumers need to reach a conclusion about when direct access to specialists is desirable, and determine how much they are willing to pay for it.
Acknowledgments
The authors thank Drs. Rodney Hayward, Joel Howell, Steven Katz, and Susan Goold for their valuable input on drafts of this manuscript and Tracy Metski for manuscript preparation.
This study was supported by grant 623332 from the Robert Wood Johnson Foundation.
Appendix A
Questions Used to Form Preauthorization Intensity Scale*
| Below is a list of elements that physician organizations may implement to manage capitated patients’ utilization of ambulatory and hospital services. For each element that your organization utilizes, please indicate how important it is in the ability of your overall utilization management programs to control utilization. Please circle a number on the importance scale (1 = very important, 5 = not at all important); or, if your organization does not utilize the particular element, please circle “0” in the far right column. | |||||||
| VeryImportant | Midpoint | Not at All Important | Don’tUtilize | ||||
| a. | Requiring preauthorization of certain ambulatory procedures or specialty referrals | 5 | 4 | 3 | 2 | 1 | 0 |
| b. | Requiring preauthorization for elective admissions | 5 | 4 | 3 | 2 | 1 | 0 |
| Please indicate how capitated patients generally obtain nonurgent ambulatory consultations with each of the specialists and providers listed. (Circle one on each line.) | ||||
| Primary Care Provider Must Refer; No Preauthorization Necessary | Primary Care Provider Must Refer and Group Must Preauthorize Referral | Patient May Self-Refer | ||
| a. | Internal medicine subspecialist | 0 | 1 | 0 |
| b. | Dermatologist | 0 | 1 | 0 |
| c. | Obstetrician (pregnancy) | 0 | 1 | 0 |
| d. | Gynecologist | 0 | 1 | 0 |
| e. | Surgical subspecialist | 0 | 1 | 0 |
| f. | General surgeon | 0 | 1 | 0 |
| g. | Mental health specialist | 0 | 1 | 0 |
| h. | Optometrist (refraction) | 0 | 1 | 0 |
| i. | Physical therapist | 0 | 1 | 0 |
| j. | Chiropractor | 0 | 1 | 0 |
| k. | Podiatrist | 0 | 1 | 0 |
| In general, must a primary care provider obtain preauthorization (for medical necessity) for the following nonurgent ambulatory tests and procedures? (Circle one on each line.) | |||
| Yes | No | ||
| a. | Pulmonary function tests | 1 | 0 |
| b. | Echocardiogram | 1 | 0 |
| c. | MRI | 1 | 0 |
| d. | Chest x-ray | 1 | 0 |
| e. | Upper endoscopy | 1 | 0 |
| f. | Exercise stress test | 1 | 0 |
| g. | Screening sigmoidoscopy | 1 | 0 |
| h. | Upper GI series | 1 | 0 |
| i. | Bone scan | 1 | 0 |
| Approximately how often must a physician obtain preauthorization when ordering urgent ambulatory referrals, tests or procedures? An urgent service is one the physician feels needs to be performed within 48 hours. | ||||||
| None ofthe Time | A Little ofthe Time | Half ofthe Time | Most ofthe Time | All ofthe Time | ||
| a. | Urgent outpatient specialty referrals | 1 | 2 | 3 | 4 | 5 |
| b. | Urgent high-cost (>$500) outpatient tests or procedures | 1 | 2 | 3 | 4 | 5 |
Numbers indicate scoring.
REFERENCES
- 1.Kassirer JP. Access to specialty care. N Engl J Med. 1994;331(17):1151–3. doi: 10.1056/NEJM199410273311709. Editorial. [DOI] [PubMed] [Google Scholar]
- 2.Greenfield S. Dividing up the turf: generalists versus specialists. J Gen Intern Med. 1996;11(4):245–6. doi: 10.1007/BF02642484. [DOI] [PubMed] [Google Scholar]
- 3.Mechanic D, Schlesinger M. The impact of managed care on patients’ trust in medical care and their physicians. JAMA. 1996;275(21):1693–7. [PubMed] [Google Scholar]
- 4. St. Peter RF. Gatekeeping Arrangements are in Wide-Spread Use. Results from the Community Tracking Study. Washington, DC: Center for Studying Health System Change; 1997(7). [PubMed]
- 5.Kerr EA, Mittman BS, Hays RD, Siu AL, Leake B, Brook RH. Managed care and capitation in California: how do physicians at financial risk control their own utilization? Ann Intern Med. 1995;123(7):500–4. doi: 10.7326/0003-4819-123-7-199510010-00004. [DOI] [PubMed] [Google Scholar]
- 6.Gold M, Hurley R. Role of managed care products in managed care plans. Inquiry. 1997;34:29–37. [PubMed] [Google Scholar]
- 7.Franks P, Clancy CM, Nutting PA. Gatekeeping revisited: protecting patients from overtreatment. N Engl J Med. 1992;327(6):424–9. doi: 10.1056/NEJM199208063270613. [DOI] [PubMed] [Google Scholar]
- 8.Greenfield S, Nelson EC, Zubkoff M, et al. Variations in resource utilization among medical specialities and systems of care: results from the medical outcomes study. JAMA. 1992;267(12):1624–30. [PubMed] [Google Scholar]
- 9.Forrest CB, Starfield B. The effect of first-contact care with primary care clinicians on ambulatory health care expenditures. J Fam Pract. 1996;43(1):40–8. [PubMed] [Google Scholar]
- 10.Jollis JG, DeLong ER, Peterson ED, et al. Outcome of acute myocardial infarction according to the specialty of the admitting physician. N Engl J Med. 1996;335:1880–7. doi: 10.1056/NEJM199612193352505. [DOI] [PubMed] [Google Scholar]
- 11.Sturm R, Meredith LS, Wells KB. Provider choice and continuity for the treatment of depression. Med Care. 1996;34:723–34. doi: 10.1097/00005650-199607000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Ayanian JZ, Hauptman PJ, Guadagnoli E, Antman EM, Pashos CL, McNeil BJ. Knowledge and practices of generalist and specialist physicians regarding drug therapy for acute myocardial infarction. N Engl J Med. 1994;331(17):1136–42. doi: 10.1056/NEJM199410273311707. [DOI] [PubMed] [Google Scholar]
- 13.Engel W, Freund DA, Stein JS, Fletcher RH. The treatment of patients with asthma by specialists and generalists. Med Care. 1989;27(3):306–14. doi: 10.1097/00005650-198903000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Dillon EC, Sergott RC, Savino PJ, Bosley TM. Diagnostic management by gatekeepers is not cost effective for neuro-ophthalmology. Ophthalmology. 1994;101:1627–30. doi: 10.1016/s0161-6420(94)31127-4. [DOI] [PubMed] [Google Scholar]
- 15.Gerbert B, Maurer T, Berger T, et al. Primary care physicians as gatekeepers in managed care. Arch Dermatol. 1996;132:1030–8. [PubMed] [Google Scholar]
- 16.Mitchell JB, Ballard DJ, Whisnant JP, Ammering CJ, Samsa GP, Matchar DB. What role do neurologists play in determining the costs and outcomes of stroke patients? Stroke. 1996;27(11):1937–43. doi: 10.1161/01.str.27.11.1937. [DOI] [PubMed] [Google Scholar]
- 17.Gold M, Wooldridge J. Surveying consumer satisfaction to assess managed-care quality: current practices. Health Care Financing Rev. 1995;16(4):155–73. [PMC free article] [PubMed] [Google Scholar]
- 18.Donabedian A. Explorations in Quality Assessment and Monitoring. Vol. II. Ann Arbor, Mich: Health Administration Press; 1982. The criteria and standards of quality. [Google Scholar]
- 19.Cleary PD, McNeil BJ. Patient satisfaction as an indicator of quality care. Inquiry. 1988;25:25–36. [PubMed] [Google Scholar]
- 20.Sherbourne CD, Hays RD, Ordway L, DiMatteo MR, Kravitz R. Antecedents of adherence to medical recommendations: results from the Medical Outcomes Study. J Behav Med. 1992;15:447–68. doi: 10.1007/BF00844941. [DOI] [PubMed] [Google Scholar]
- 21.DiMatteo MR, Hays R. The significance of patients’ perceptions of physician conduct: a study of patient satisfaction in a family practice center. J Commun Health. 1980;6:18–34. doi: 10.1007/BF01324054. [DOI] [PubMed] [Google Scholar]
- 22.DiMatteo MR, Hays RD, Prince LM. Relationship of physicians’ nonverbal communication skill to patient satisfaction, appointment noncompliance, and physician workload. Health Psychol. 1986;5:581–94. doi: 10.1037//0278-6133.5.6.581. [DOI] [PubMed] [Google Scholar]
- 23.Marquis MS, Davies AR, Ware Je., Jr Patient satisfaction and change in medical care provider: a longitudinal study. Med Care. 1983;21(8):821–9. doi: 10.1097/00005650-198308000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Rubin HR, Gandek B, Rogers WH, Kosinski M. Patients’ ratings of outpatient visits in different practice settings: results from the Medical Outcomes Study. JAMA. 1993;270(7):835–40. [PubMed] [Google Scholar]
- 25.Kerr EA, Hays RD, Lee M, Siu AL. Does dissatisfaction with access to specialists affect the desire to leave a managed care plan? Med Care Res Rev. 1998;55(1):59–77. doi: 10.1177/107755879805500104. [DOI] [PubMed] [Google Scholar]
- 26. Davis K, Collins KS, Schoen C, Morris C. Choice matters: enrollees’ views of their health plans. Health Aff (Millwood). 1995:99–112. [DOI] [PubMed]
- 27. Blendon RJ, Knox RA, Brodie M, Benson JM, Chervinsky G. Americans compare managed care, Medicare, and fee-for-service. J Am Health Policy. May/June 1994:42–7. [PubMed]
- 28.Murray JP. A follow-up comparison of patient satisfaction among prepaid and fee-for-service patients. J Fam Pract. 1988;26(5):576–81. [PubMed] [Google Scholar]
- 29.Kerr EA, Mittman BS, Hays RD, Leake B, Brook RH. Quality assurance in capitated physician groups: where is the emphasis? JAMA. 1996;276(15):1236–9. [PubMed] [Google Scholar]
- 30.Davies AR, Ware JE., Jr . GHAA’s Consumer Satisfaction Survey and User’s Manual. 2nd ed. Washington, DC: Group Health Association of America; May 1991. [Google Scholar]
- 31. Huber PJ. The behavior of maximum likelihood estimates under non-standard conditions. In: Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability; 1967. Berkely, Calif: University of California Press; 1967:1:221–23.
- 32.White H. A heteroskedasticity—consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817–30. [Google Scholar]
- 33.Shrout P, Fleiss J. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–8. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 34.Fincham JE, Wertheimer AI. Predictors of patient satisfaction in a health maintenance organization. J Health Care Marketing. 1986;6(3):5–11. [PubMed] [Google Scholar]
- 35.Mechanic D, Greenley JR, Cleary PD, Hoeper EW, Wenzel FJ. A model of rural health care: consumer response among users of the Marshfield Clinic. Med Care. 1980;18(6):597–608. doi: 10.1097/00005650-198006000-00003. [DOI] [PubMed] [Google Scholar]
- 36. Weiss GL, Ramsey CA. Regular source of primary medical care and patient satisfaction. Qual Rev Bull. June 1989:180–4. [DOI] [PubMed]
- 37.Hornbrook MC, Goodman MJ. Assessing relative health plan risk with the RAND-36 Health Survey. Inquiry. 1995;32(1):56–74. [PubMed] [Google Scholar]
- 38.Andersen R, Newman J. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q. 1973;51:95–124. [PubMed] [Google Scholar]
- 39.Ware JE, Davies AR. Behavioral consequences of consumer dissatisfaction with medical care. Eval Prog Plan. 1983;6:291–7. doi: 10.1016/0149-7189(83)90009-5. [DOI] [PubMed] [Google Scholar]
- 40.Emanuel EJ, Neveloff-Dubler N. Preserving the physician–patient relationship in the era of managed care. JAMA. 1995;273(4):323–40. [PubMed] [Google Scholar]
- 41.Nash DB, Nash IS. Building the best team. Ann Intern Med. 1997;127(1):72–4. doi: 10.7326/0003-4819-127-1-199707010-00012. [DOI] [PubMed] [Google Scholar]