Abstract
Recent interest in anthrax is due to its potential use in bioterrorism and as a biowarfare agent against civilian populations. The development of rapid and sensitive techniques to detect anthrax spores in suspicious specimens is the most important aim for public health. With a view to preventing exposure of laboratory workers to viable Bacillus anthracis spores, this study evaluated the suitability of PCR assays for detecting anthrax spores previously inactivated at 121°C for 45 min. The results indicate that heat treatment ensures the complete inactivation of B. anthracis spores without significantly affecting the efficiency of PCR assays.
Since the attacks of 11 September, there has been an increase in global concerns regarding bioterrorist attacks. Recent interest in anthrax is due to its potential use in bioterrorism and as a biowarfare agent against civilian populations (4, 6, 7, 9, 11, 12). Cases of pulmonary and cutaneous anthrax occurred in postal workers and in mail handlers exposed to envelopes contaminated with Bacillus anthracis spores in the United States. As of the end of November 2001, it had been reported that 5 people had died and 13 others had been infected with anthrax (3). Before these events, vials containing B. anthracis spores had been found in U.S. Postal Service facilities on at least two occasions over the past 30 years. The last case occurred in 1999 (5).
The culture of powders or samples from envelopes having any powdery substance on the outside is the classical method of detecting B. anthracis. An alternative method is the direct detection of B. anthracis DNA in letters, packages, or other materials suspected of being contaminated. PCR assays for detecting genes for virulence markers in B. anthracis strains were recently described (2, 14, 16, 17, 20, 22). The main problems in setting up a test procedure for DNA testing of suspected B. anthracis spore-containing material are the risk of exposing laboratory workers and the costly procedures for transferring contaminated material and/or cultures to specialized laboratories. Both problems can be addressed by inactivating the vegetative and spore phases of the organism prior to testing. In this study, the suitability of using previously described PCR assays to detect DNA from heat-inactivated spores is described. The sensitivity of the PCR test was also estimated by using different sets of primers to detect both chromosomal and plasmid genes specific for virulent strains of B. anthracis.
For this study B. anthracis A0843 was used as a virulent strain for spore production. This strain, isolated from an outbreak of anthrax which occurred in Italy, was microbiologically identified according to the work of Turnbull et al. (21), and the presence of plasmids pXO1 and pXO2 has been confirmed by PCR assay (8, 10, 19). Genotyping analysis performed by multiple-locus variable-number tandem repeat analysis included this strain in cluster A1a, genotype 3, one of the most frequently isolated in Italy (13; A. Fasanella, K. L. Smith, C. Keys, P. Coker, P. Keim, and M. Hugh-Jones, Program Abstr. 4th Int. Conf. Anthrax, p. 14, 2001). Bacillus cereus ATCC 14579 was used as an avirulent control strain, and all strains were maintained on sheep blood agar plates (Oxoid) at 37°C.
To promote sporulation, B. anthracis was cultured on tryptose agar at 37°C for 48 h followed by 2 weeks at 23°C. Sporulation was periodically monitored by using the Schaeffer-Fulton stain: the vegetative cells appeared red to pink, while spores were green (18). When sporulation reached 95%, the vegetative organisms were inactivated by incubation with a suspension of 50% methanol-50% saline at 37°C for 1 h. For methanol elimination, spores were washed three times with saline and the pellet was suspended. The number of spore-forming units was evaluated by plating 10-fold dilutions in saline onto plate count agar plates (Bio-Rad), which were incubated at 37°C for 48 h. Successively, from a suspension containing about 107 × 106 ± 9.6 × 106 spore-forming units per ml, dilutions of viable spores were prepared in distilled water from 10−1 to 10−5, and 2 ml of each dilution was aseptically distributed onto containers. The containers were sealed and stored at −80°C overnight before freeze-drying was performed with a Drywinner (Heto). Finally, the lyophilized spores were treated at 121°C for 45 min in an autoclave, according to official procedures of the Ministry of Health of Italy. Some samples were alternatively heated at 125°C for 60 min to determine if a stronger treatment affected the efficiency of PCR assays.
Prior to molecular testing, all autoclaved spore samples were suspended in 2 ml of distilled water and tested for purity and sterility according to standard procedures (15). None of the spores were viable after the heat treatment. For the PCR test, 200 μl of each suspension was heated to 98°C for 30 min and then centrifuged at 5,000 rpm for 10 min. DNA templates from methanol-killed (1) B. anthracis and B. cereus strains were used as positive and negative controls, respectively. The PCR assay and the primers have been described; the latter are listed in Table 1 (8, 17, 19). Amplified samples were electrophoresed in a 2% agarose gel containing 0.5 μg of ethidium bromide/ml at 120 V for 60 min, and amplified bands were transilluminated under UV light and compared to a 50-bp DNA ladder.
TABLE 1.
Primers used in this study
| Locus | Primer | Position | Length (bp) | Sequence (5′-3′) | Reference |
|---|---|---|---|---|---|
| pag | 67 | 1925-1944 | 747 | CAGAATCAAGTTCCCAGGGG | 19 |
| 68 | 2652-2671 | 747 | TCGGATAAGCTGCCACAAGG | 19 | |
| 23 | 2006-2027 | 151 | CTACAGGGGATTTATCTATTCC | 19 | |
| 24 | 2135-2156 | 151 | ATTGTTACATGATTATCAGCGG | 19 | |
| cya | 65 | 1255-1274 | 929 | CAGCATGCGTTTTCTTTAGC | 19 |
| 66 | 2164-2183 | 929 | CCCTTAGTTGAATCCGGTTT | 19 | |
| 25 | 1459-1478 | 546 | GGTTTAGTACCAGAACATGC | 19 | |
| 26 | 1990-2004 | 546 | CGGCTTCAAGACCCC | 19 | |
| lef | 3 | 1238-1258 | 385 | CTTTTGCATATTATATCGAGC | 19 |
| 4 | 1599-1622 | 385 | GAATCACGAATATCAATTTGTAGC | 19 | |
| 59 | 949-970 | 993 | GGATATGAACCCGTACTTGTAA | 19 | |
| 60 | 1921-1941 | 993 | TAAATCCGCACCTAGGGTTGC | 19 | |
| capC | 57 | 1603-1622 | 264 | ACTCGTTTTTAATCAGCCCG | 19 |
| 58 | 1847-1866 | 264 | GGTAACCCTTGTCTTTGAAT | 19 | |
| capBCA | 17 | 1230-1249 | 873 | GAAATAGTTATTGCGATTGG | 19 |
| 20 | 2083-2102 | 873 | GGTGCTACTGCTTCTGTACG | 19 | |
| Ba813 | R1 | 227-249 | 152 | TTAATTCACTTGCAACTGATGGG | 18 |
| R2 | 98-120 | 152 | AACGATAGCTCCTACATTTGGAG | 18 |
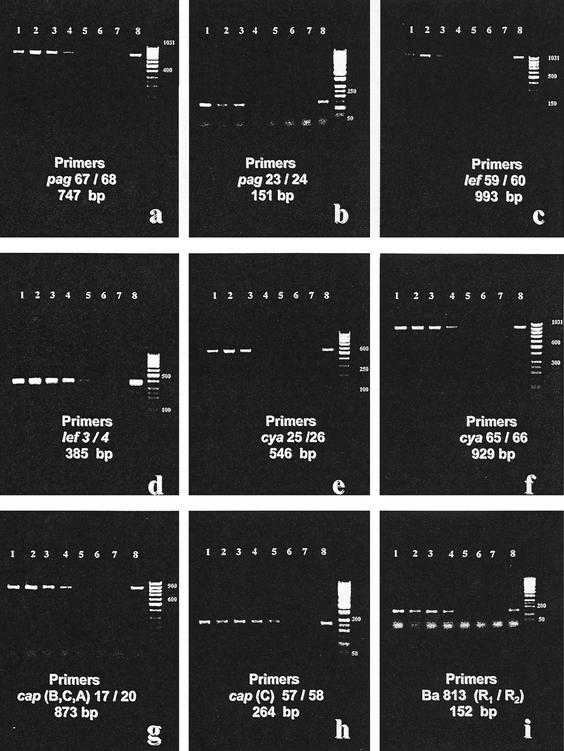
For samples previously heated at 125°C for 60 min, the 747-bp fragment of the pag gene recognized by primers 67 and 68 was amplified from the spore suspensions from undiluted to 10−4-diluted samples (Fig. 1a, lanes 1 to 5), and the 151-bp fragment of the pag gene recognized by primers 23 and 24was still weakly evident in samples diluted 10−5 (Fig. 1b, lanes 1 to 6). The 993-bp fragment amplified by lef-specific primers 59 and 60 remained evident in the undiluted to 10−2-diluted samples (Fig. 1c, lanes 1 to 3); an amplification of a lef primer 3- and 4-specific 385-bp fragment was obtained in the undiluted to 10−4-diluted samples (Fig. 1d, lanes 1 to 5), while the 546-bp fragment of the cya sequence recognized by primers 25 and 26 appeared in undiluted samples through the 10−2 dilutions (Fig. 1e, lanes 1 to 3). In contrast, the 929-bp fragment amplified from the cya plasmid gene sequence recognized by primers 65 and 66 was still evident up to a 10−3 dilution (Fig. 1f, lanes 1 to 4). Amplification of the capBCA 17 and 20 primer-specific 873-bp fragment was apparent in undiluted to 10−3-diluted samples (Fig. 1g, lanes 1 to 4); the capC 57 and 58 primer-specific 264-bp fragment was amplified in samples diluted up to 10−4 (Fig. 1h, lanes 1 to 5), as was the 152-bp Ba813 chromosomal fragment (Fig. 1i, lanes 1 to 5).
FIG. 1.
Electrophoretic analysis (2% agarose gel) of amplified DNA fragments obtained by PCR assays performed with different sets of primers on DNA samples from heat-inactivated B. anthracis spore suspensions. The PCR assay was conducted on undiluted (lanes 1) to 10−5-diluted (lanes 6) DNA samples in distilled water. (a) Fragment of 747 bp amplified by the pag primers 67 and 68; (b) 151-bp fragment amplified by the pag primers 23 and 24; (c) 993-bp fragment amplified by the lef primers 59 and 60; (d) 385-bp fragment amplified by lef primers 3 and 4; (e) 546-bp fragment amplified by cya primers 25 and 26; (f) 929-bp fragment amplified by cya primers 65 and 66; (g) 873-bp fragment amplified by capBCA primers 17 and 20; (h) 264-bp fragment amplified by capC primers 57 and 58; (i) 152-bp fragment amplified by Ba813 primers R1 and R2. DNA samples of virulent B. anthracis and B. cereus used as positive and negative controls, respectively, are shown in lanes 7 and 8. Lanes 9 contain a 50-bp ladder as a size standard.
Bands in lane 8 of all panels in Fig. 1 are from the B. anthracis-positive control strain, and lane 7 contains the B. cereus negative control. The same results were obtained when spore samples were heated under less stringent conditions (121°C for 45 min), with no apparent viable cells observed in subculture of the treated spores (data not shown).
Results indicated that dilutions spore suspensions of B. anthracis could be killed by heating at 125°C for either 45 or 60 min and that sufficient template DNA was released after either treatment for PCR analysis. Moreover, amplicons of the cya, pagA, and lef genes, encoding edema factor, protective antigen, and lethal factor, respectively, as well as the chromosomal Ba813 sequence could be amplified from this template DNA (19). The most sensitive results appeared to be obtained with the pagA fragment recognized by primers 23 and 24, which still could be amplified at a 10−5 dilution, corresponding to approximately 1.07 × 103 inactivated spores/ml. To evaluate the loss in sensitivity that occurs following heat treatment, PCR assays were carried out in parallel by testing viable and heated spores. The results indicated that when the supernatant of viable spores, previously treated at 98°C for 30 min, was tested, a maximum of a 10-fold increase in the sensitivity was obtained depending on the set of primers used (data not shown). Thus, the loss in sensitivity as a result of autoclaving should not be considered significant. It is also possible that this drop in sensitivity could also reflect the variability of the DNA extraction and PCR assay on a given day.
In conclusion, the data presented in this paper indicate that the PCR system described here can be proposed as a safe diagnostic method for detecting anthrax contamination of nonclinical specimens. Although a slight decrease was also noted when results for inactivated and viable spores were compared, this would be problematic only when spore contamination reached 1,000/ml.
Acknowledgments
We thank Martin Hugh-Jones (Department of Pathobiological Sciences, School of Veterinary Medicine, Louisiana State University, Baton Rouge) for scientific support.
REFERENCES
- 1.Adone, R., F. Ciuchini, G. La Rosa, C. Marianelli, and M. Muscillo. 2001. Use of polymerase chain reaction to identify Brucella abortus strain RB51 among Brucella field isolates from cattle in Italy. J. Vet. Med. B 48:107-113. [DOI] [PubMed] [Google Scholar]
- 2.Beyer, W., S. Pocivalsek, and R. Bohm. 1999. PCR-ELISA to detect Bacillus anthracis from soil samples limitations of present published primers. J. Appl. Microbiol. 87:229-236. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Diseases Control and Prevention. 2001. Update: investigation of bioterrorism related anthrax. Morb. Mortal. Wkly. Rep. 50:1008-1010. [PubMed] [Google Scholar]
- 4.Centers for Diseases Control and Prevention. 2001. Interim guidelines for investigation of and response to bacillus anthracis exposures. Morb. Mortal. Wkly. Rep. 50:987-990. [PubMed] [Google Scholar]
- 5.Chicago Department of Health. 2000. Bioterrorism: a public health threat. CDInfo 2:1-4. [Google Scholar]
- 6.Christopher, G. W., T. J. Cieslak, J. A. Pavlin, and E. M. Eitzen. 1997. Biological warfare: a historical perspective. JAMA 278:412-417. [PubMed] [Google Scholar]
- 7.Eitzen, E. M. 1997. Use of biological weapons, p.437-450. In F. R. Sidell, E. T. Takafuji, and D. R. Franz (ed.), Medical aspects of chemical biological warfare. Office of the Surgeon General, Washington, D.C.
- 8.Fasanella, A., S. Losito, T. Trotta, R. Adone, S. Massa, F. Ciuchini, and D. Chiocco. 2001. Detection of anthrax vaccine virulence factors by polymerase chain reaction. Vaccine 19:4214-4218. [DOI] [PubMed] [Google Scholar]
- 9.Freidlander, A. M. 1997. Anthrax, p. 467-478. In F. R. Sidell, E. T. Takafuji, and D. R. Franz (ed.), Medical aspects of chemical biological warfare. Office of the Surgeon General, Washington, D.C.
- 10.Green, B. D., L. Battisti, T. M. Koehler, C. B. Thorne, and B. E. Ivins. 1985. Demonstration of a capsule plasmid in Bacillus anthracis. Infect. Immun. 49:291-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Inglesby, T. V., D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. M. Friedlander, J. Hauer, J. McDade, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, and K. Tonat. 1999. Anthrax as a biological weapon: medical and public health management. JAMA 281:1735-1745. [DOI] [PubMed] [Google Scholar]
- 12.James, C. P., D. M. John, M. E. Edward, and M. F. Arthur. 1998. Anthrax as a potential biological warfare agent. Arch. Int. Med. 158:429-434. [DOI] [PubMed] [Google Scholar]
- 13.Keim, P., L. B. Price, A. M. Klevytska, K. L. Smith, J. M. Schupp, R. Okinaka, P. J. Jackson, and M. E. Hugh-Jones. 2000. Multiple-locus variable-number tandem repeat analysis reveals genetic relationships within Bacillus anthracis. J. Bacteriol. 182:2928-2936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mikesell, P., B. E. Ivins, J. D. Ristroph, and T. M. Dreier. 1983. Evidence for plasmid-mediated toxin production in Bacillus anthracis. Infect. Immun. 39:371-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Office International des Epizooties. 2000. Manual of standards for diagnostic tests and vaccines. Office International des Epizooties, World Organization for Animal Health, Paris, France.
- 16.Okinaka, R. T., K. Cloud, O. Hampton, A. R. Hoffmaster, K. K. Hill, P. Keim, T. M. Koehler, G. Lamke, S. Kumano, J. Mahillon, D. Manter, Y. Martinez, D. Ricke, R. Svensson, and P. J. Jackson. 1999. Sequence and organization of pXO1 the large Bacillus anthracis plasmid harboring the anthrax toxin genes. J. Bacteriol. 181:6509-6515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patra, G., P. Silvestre, V. Ramisse, J. Therasse, and J. I. Guesdon. 1996. Specific oligonucleotide primers for rapid identification of Bacillus anthracis strains. Salisbury Med. Bull. 87(Special Suppl.):45-46. [Google Scholar]
- 18.Poli, G. 1998. Microbiologia ed immunologia, p. 60. Unione Tipografico-Editrice Torinese, Turin, Italy.
- 19.Ramisse, V., G. Patra, H. Garrigue, J. L. Guesdon, and M. Mock. 1996. Identification and characterization of Bacillus anthracis by multiplex PCR analysis of sequences on plasmids pXO1 and pXO2 and chromosomal DNA. FEMS Microbiol. Lett. 145:9-16. [DOI] [PubMed] [Google Scholar]
- 20.Ramisse, V., G. Patra, J. Vaissaire, and M. Mock. 1999. The Ba813 chromosomal DNA sequence effectively traces the whole Bacillus anthracis community. J. Appl. Microbiol. 87:224-228. [DOI] [PubMed] [Google Scholar]
- 21.Turnbull, P., J. Kramer, and J. Melling. 1990. Bacillus, p. 187-210. In M. T. Parker and L. H. Collier (ed.), Topley and Wilson's principles of bacteriology, virology and immunity, VII ed. Edward Arnold, London, United Kingdom.
- 22.Turnbull, P. C. B., R. Boehm, O. Cosivi, M. Doganay, M. E. Hugh-Jones, M. K. Lalitha, and V. De Vos. 1998. Guidelines for the surveillance and control of anthrax in humans and animals. WHO/EMC/ZDI/98.6. World Health Organization, Geneva, Switzerland.