Abstract
OBJECTIVE
To study the attitudes of preclinical and clinical medical students toward the importance of telling patients they are students, and to compare their attitudes with those of patients.
METHODS
We conducted a cross-sectional survey of medical students from five Philadelphia medical schools, and a longitudinal follow-up in one medical school, to assess the importance students place on telling patients they are medical students before interacting with them. We asked similar questions of 100 general medical outpatients from two academically affiliated hospitals.
MAIN RESULTS
In total, 2,603 students (58%) responded to the cross-sectional survey, 74 (50%) responded to the longitudinal survey, and 100 patients responded to our interview survey (94% response rate). In the cross-sectional survey, there were negligible differences in the importance that patients and medical students placed on informing alert patients that they are interacting with students in nonsurgical settings. In surgical settings involving anesthetized patients, patients placed significantly more importance on being informed of students' roles in their surgery than did students, and preclinical students placed more importance on this than did clinical students. Results from the cross-sectional survey were supported by the longitudinal survey, in which fourth-year medical students placed significantly less importance on informing patients of their student status than the same cohort had done 2 years previously.
CONCLUSIONS
Medical students place less importance on informing patients about their student status than patients desire, especially in surgical settings in which the patient is to be anesthetized. Medical students already having completed a clinical rotation stray further from patient ideals than preclinical medical students. These findings suggest that, as medical students advance in their training, they suffer an erosion in their attitudes about telling patients they are students.
Keywords: informed consent, education, medical ethics, survey, patients, medical students
In teaching hospitals, medical students frequently interact with patients purely for educational purposes, such as when students perform physical examinations that must be repeated by physicians. Medical ethics curricula in medical schools generally emphasize that medical students have a duty to inform patients that they are students.1 However, many studies show that students choose to be less than candid in their dealings with patients.2–6 This may occur because students receive mixed messages about the importance of informing patients that they are students. For example, sometimes clinical departments instruct students to introduce themselves to patients as “doctors.”5,7 And sometimes on clinical rotations students are encouraged to perform examinations or procedures on patients without telling patients they are medical students. For example, it is common in many obstetrics and gynecology rotations for students to practice pelvic examinations on anesthetized patients prior to their operations.8,9 The students may wonder, in these instances, whether patients have been asked about participating in this educational examination. Students concerned with this issue may find little support from their colleagues or instructors.10 With these mixed messages, students may become confused about whether to tell patients that they are participating in educational activities.
There are many reasons, however, that students ought to inform patients that they are students. First, patients have the right to refuse to allow medical students to participate in their care.11 But patients cannot refuse medical student participation if they do not know they are interacting with medical students.12,13 Second, knowledge that they are interacting with medical students may allow patients to participate more effectively in educating the medical student. For example, patients may be more tolerant of students' awkwardness. Third, patients aware that they are interacting with students may ask them questions which they would not want to bother asking attending physicians. Fourth, patients may gain satisfaction by knowing that they are interacting with medical students and, thereby, contributing to medical education.
In this article, we present a study exploring how preclinical and clinical medical students view the importance of telling patients they are students, and compare these attitudes with those of patients.
METHODS
Subjects
In October of 1995, we distributed questionnaires to all 4,511 medical students at the five Philadelphia area medical schools. Questionnaires were delivered to the medical school mail rooms and placed in students' on-campus mailboxes. We distributed a second questionnaire to all students 3 months later, with directions not to respond if they had previously completed it. In October of 1997, we redistributed the questionnaire to the 148 fourth-year medical students at one of these five medical schools who had been second-year (preclinical) students at the time of the original questionnaire. Students completing questionnaires received a chance to win a $75 gift certificate to the restaurant of their choice.
In October and November of 1995, we interviewed a convenience sample of 100 general medicine outpatients: 50 patients at the Hospital of the University of Pennsylvania's general medicine clinic and 50 at the Philadelphia Veterans Affairs Medical Center's general medicine clinic. At each location, the clinic's nursing coordinator identified patients who were expected to wait at least 30 minutes for their appointment. Interviews were conducted by a trained research assistant.
Questionnaire Instruments
Medical students were asked to rate the importance of identifying themselves as medical students (on a 5-point scale ranging from “very unimportant” to “very important”) for clinical scenarios taking place on alert patients:
In each of the situations described below, please say how important you think it is for patients to know that the examiner is a medical student. Be sure that in each of these nonemergency situations the patient is awake and alert and a resident or attending physician will repeat the examination or history after the medical student is done.
How important would it be for you to tell a patient that you are a medical student before you :
take their blood pressure?
examine their abdomen?
perform a prostate examination during an annual checkup?
perform a pelvic examination during their annual checkup?
take their medical history?
perform a spinal tap with supervision? (The procedure will not be repeated if the specimen is good.)
take their sexual history?
The students were asked the following questions about the importance of asking permission before being involved in patients' surgeries:
Medical students participate in surgeries during their required clinical clerkship. This offers students a chance to learn and practice skills they otherwise might not be able to learn. Since medical students frequently arrive in the operating rooms after the patients are anesthetized, students do not always have a convenient opportunity to speak with patients before becoming involved in their care. Please respond to the following situations regarding the need for a patient's presurgery permission for medical student involvement.
How important would it be for a patient to be told that a medical student is going to:
watch the surgery?
make the initial incision for abdominal surgery with supervision?
hold a retractor with supervision?
perform a rectal examination before rectal surgery with supervision?
perform a pelvic examination before pelvic surgery with supervision?
suture the incision with supervision?
intubate the patient with supervision?
We changed the perspective in the surgical settings from “how important would it be for you to tell a patient” to “how important would it be for a patient to be told” in order to acknowledge that in surgical settings, medical students may not always be available to ask permission of patients before interacting with them, whereas in office settings with alert patients, medical students always have the opportunity to inform the patient that they are medical students.
Patients were interviewed using the same questionnaire except for the following changes. First, before being asked these questions, patients were told the educational differences between medical students, residents, and faculty physicians. Second, the questionnaire was altered to make the questions appropriate for patients. For example, patients were asked, “How important would it be for you to be told that a medical student is going to watch your surgery?” Third, the questionnaire was administered as a face-to-face interview rather than as a written questionnaire. We did this in order to include patients at all reading levels, and to clarify any terminology the patients did not understand. Fourth, only female patients were asked to rate the importance of obtaining informed consent for the two pelvic examination scenarios and only male patients for the two rectal examination scenarios.
Data Analysis
Using the cross-sectional data, we compared the importance ratings of patients, preclinical students (medical school students who had not begun clinical rotations), and clinical students using analysis of variance (ANOVA), and when these analyses were significant (at p <.01), we performed Tukey tests to compare preclinical students to clinical students, preclinical students to patients, and clinical students to patients. Using the longitudinal data, we compared the importance ratings of preclinical students in 1995 with fourth-year medical students in 1997 using independent-samples t tests. (Because the original questionnaire was anonymous, we were not able to match subjects across the time periods.) We also performed independent-samples t tests to test for differences in the mean importance ratings of 1997 respondents who did and 1997 respondents who did not say they had responded to our 1995 questionnaire. All p values were two-sided.
RESULTS
In the cross-sectional study, we received completed questionnaires from 2,603 students (58% response rate). The students' average age was 25.4 years (SD = 3.5 years). Forty-six percent were female. Seventy-five percent were white, 13% Asian American, 5% African American, and 3% other; the remainder did not signify their race. Sixty-three percent were preclinical students, and 37% had completed at least one clinical rotation. In the longitudinal follow-up study, we received completed questionnaires from 74 subjects (50%). Their mean age (after subtracting 2 years from the age of the 1997 respondents), race, and gender did not differ from the same school's preclinical respondents in 1995 (all p values >.2).
We approached 106 patients in order to complete our 100 interviews, for an enrollment rate of 94%. Patients' average (SD) age was 58 (15) years, with a mean (SD) of 12 (3) years of education. Fifty-four percent were African American, 26% white, and 20% other. Fifty-eight percent were male.
Cross-sectional Study
Clinical Scenarios Involving Alert Patients
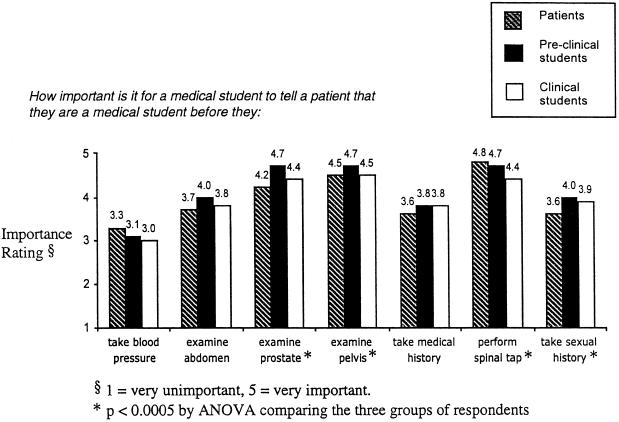
Figure 1 shows the relative importance that patients, preclinical students, and clinical students placed on having medical students identify themselves as students before interacting with alert patients. Respondents thought information about student status was least important when medical students take a patient's blood pressure, and most important when they perform a lumbar puncture. However, differences in responses across subjects were small and not in a consistent direction.
FIGURE 1.
Importance of being identified as a medical student when interacting with alert patients.
Clinical Scenarios Involving Anesthetized Patients
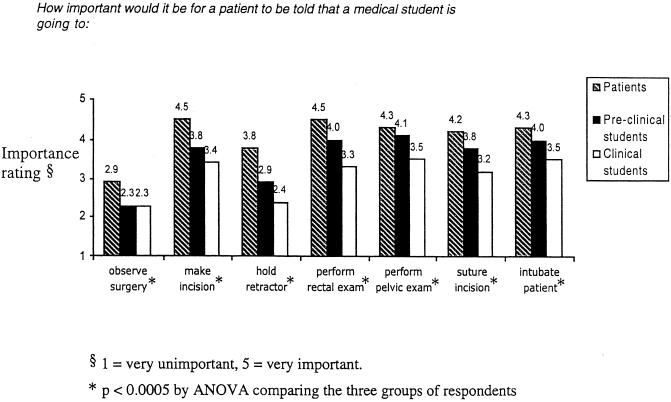
Figure 2 shows the relative importance that patients, preclinical students, and clinical students placed on asking permission of patients before allowing medical students to participate in their surgery. In contrast to the nonsurgical scenarios, in these surgical scenarios all differences in the mean importance ratings across the three groups of subjects were statistically significant (with p values < .0005 by ANOVA). In all of these scenarios except the first (in which the student observes the surgery), patients placed significantly more importance on being asked permission than did preclinical students, and preclinical students placed significantly more importance on asking permission than did clinical students (with p values < .0005 by Tukey tests). In most cases, these differences were not only statistically significant, but also were as large or larger than 0.5 point on the 5-point scale. The gap between patients' and clinical students' attitudes ranged from 0.6 point on the scale (for medical students observing surgeries) to 1.4 points (for medical students holding retractors at the surgery). The mean difference in importance ratings for patients and clinical students in surgical settings was 1 point on the 5-point scale.
FIGURE 2.
Importance of asking permission before interacting with patients in a surgical setting.
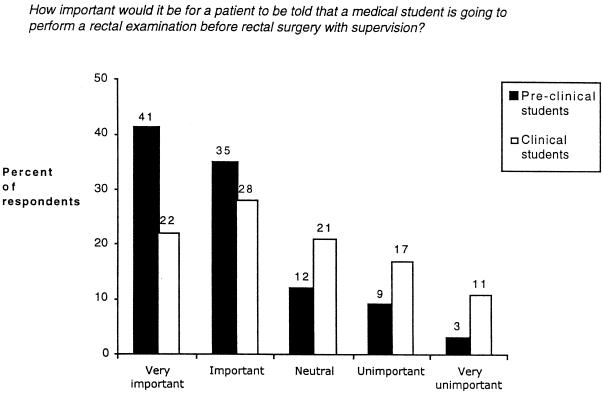
To illustrate how attitudes differed between preclinical and clinical students,Figure 3 shows the distribution of their responses to the question of how important it is to ask permission from patients before allowing medical students to perform rectal examinations during surgery (the question with the largest difference between preclinical students' and clinical students' importance ratings). Figure 3 shows that 76% of preclinical students thought it was either “important” or “very important” to ask permission in this scenario, compared with only 50% of clinical students. Only 12% of preclinical students thought it was either “unimportant” or “very unimportant” to ask permission in this scenario compared with 28% of clinical students.
FIGURE 3.
Students' importance ratings for asking permission from patients before performing a rectal examination under anesthesia.
Longitudinal Study
Table 1 compares the importance ratings of preclinical students from 1995 and fourth-year students from 1997 at one of the five medical schools. The pattern of differences between the importance ratings of preclinical and fourth-year students is similar to that shown in the cross-sectional study. Specifically, there were consistent and large differences between the importance that preclinical and clinical students placed on asking permission before interacting with anesthetized patients in a surgical setting. As with the cross-sectional study, most of these differences were greater than 0.5 point on the 5-point scale, and all but one of these differences was statistically significant. We found no differences in the importance ratings of fourth-year students who remembered responding to the 1995 questionnaire compared with those who did not remember responding (all p values >.2, data not shown).
Table 1.
Longitudinal Comparison of the Importance Students Placed on Identifying Themselves as Students or onAsking Permission Before Interacting with Patients
| Importance Ratings* | ||||
|---|---|---|---|---|
| Setting | Clinical Scenario | Preclinical Students from 1995(n = 153) | Fourth-year Medical Students from 1997(n = 74) | p Value† |
| Alert patients | Take blood pressure | 3.3 | 2.8 | .018 |
| Examine abdomen | 4.2 | 3.7 | .017 | |
| Examine prostate | 4.3 | 3.5 | .019 | |
| Examine pelvis | 4.8 | 4.6 | .142 | |
| Take medical history | 4.0 | 3.9 | .794 | |
| Perform spinal tap | 4.7 | 4.5 | .133 | |
| Take sexual history | 5.0 | 4.9 | .312 | |
| Anesthetized patients | Observe surgery | 2.3 | 2.0 | .052 |
| Make incision | 3.8 | 3.2 | .003 | |
| Hold retractor | 3.0 | 2.3 | <.0005 | |
| Perform rectal exam | 4.0 | 3.0 | <.0005 | |
| Perform pelvic exam | 4.1 | 3.4 | <.0005 | |
| Suture incision | 3.8 | 3.2 | <.0005 | |
| Intubate patient | 4.0 | 3.4 | .002 | |
1 = very unimportant, 5 = very important.
By independent samples t test.
DISCUSSION
In most of the clinical settings explored in this study, the majority of preclinical and clinical medical students thought it was important to identify themselves as medical students and ask permission before interacting with patients. However, clinical students responding to our questionnaire placed less importance on informing patients of their student status than did preclinical respondents. Previous studies have shown that students doing clinical clerkships act in ways that they think are unethical.6 Our study suggests that these actions are accompanied by changes in beliefs. Students seem to change their minds about what ought to happen. In surgical settings, situations in which an anesthetized patient is unlikely to discover the role of the medical student, preclinical and clinical students placed significantly less emphasis on informing patients of their role in the surgery than patients thought they should.
Although it is gratifying to see that the majority of students thought that informing patients of their student status was important in most of these clinical scenarios, it is disturbing to see that clinical students placed less importance on informing patients than did preclinical students. It would be less disturbing if the different responses from clinical and preclinical students reflected changes in importance ratings only from “very important” to “important.” Unfortunately, our data show that the difference results in part from an increased proportion of clinical students (compared with preclinical) who thought informing patients was “unimportant” or even “very unimportant.” Moreover, the differences between clinical students, preclinical students, and patients were sizable: Cohen has defined effect sizes in studies comparing two means as “large” if the means are separated by 0.8 SD, and “moderate” if separated by 0.5 SD.14 For the responses reported here, the average SD was 1.2; thus, by Cohen's criteria, most of the statistically significant differences between these three groups are moderate or large.
Although preclinical students placed more importance on telling patients they were students than did clinical students, this discrepancy was much greater in surgical settings than in office settings, as was the divergence between both groups of students and patients. There are several possible explanations for why the discrepancy primarily occurred in the surgical scenarios. First, in office settings, when interacting with alert patients, preclinical and clinical students may think that patients will recognize they are medical students, even without any formal introduction. In such cases, they may worry that they will “get caught” if they perform sensitive examinations on patients without introducing themselves as medical students. In contrast, in surgical settings, medical students may feel less risk of being identified as students. Thus, they may think informing patients is more important in office settings than in surgical settings. Conversely, patients' attitudes toward the importance of knowing when they are interacting with medical students in office and surgical settings would not be influenced by such matters. Thus, patients would think being informed of when they were being examined by medical students was important in both settings, increasing the discrepancy between their attitudes and those of students.
Second, the large discrepancy between patients and students in surgical settings may reveal different opinions regarding why asking permission is important, with patients placing more emphasis on their bodily integrity and students placing more emphasis on medical risks and harms. For example, rectal and pelvic examinations are physically uncomfortable for alert patients, especially when performed by inexperienced medical students. Thus, medical students may see surgical settings as an opportunity to gain experience in performing these examinations without causing patients discomfort. This realization may be stronger for clinical students who have actually performed such examinations in the operating room and understood their educational benefits. If medical students think that giving patients information is important only when it allows patients to avoid unnecessary pain, then they may not think it is important to inform patients about their involvement in surgical settings when patients are anesthetized. In contrast, if patients think being informed is important regardless of any risk of pain or physical harm, then they will remain adamant that students should be identified before performing sensitive examinations when patients are under anesthesia.
Our study has several limitations. First, we only studied students at Philadelphia medical schools and, thus, cannot comment on whether our findings are generalizable. Nevertheless, Philadelphia area medical schools are quite diverse, including an osteopathic medical school, an inner-city medical center serving primarily a Medicaid population, and a predominantly research-oriented university. Second, only 50% to 54% of medical students responded to our surveys, raising questions about whether nonrespondents would have had different attitudes than respondents. This response rate is typical of responses for physician surveys.15 In addition, nonrespondent bias would have to be profound to alter our results, given the large differences in attitudes we found between patients, preclinical students, and clinical students. Third, part of our study is cross-sectional. Thus, differences between preclinical and clinical students in the cross-sectional study may result from factors that are not comparable across groups. Fourth, we could not link respondents in the longitudinal component of our study because our original questionnaire was anonymous. Thus, it is possible that differences between preclinical and clinical students in both the cross-sectional and longitudinal studies were due not to a shift in attitudes over time, but to a response bias—the type of students responding during their clinical years may be different from the type who respond during their preclinical years. Nevertheless, we think it is plausible that differences between preclinical and clinical students reflect real changes in students' attitudes through the course of their medical training, and not changes in the type of medical students enrolled in medical school over these years, or in their medical school curricula, or in the type of people who respond to our questionnaire. Only a longitudinal study that tracks changes in specific students' attitudes over time could prove a change in attitude. But our data are highly suggestive that such a change occurs. Fifth, our patients were a convenience sample and were overrepresented by African Americans compared with the national population. Our sample, therefore, may not be representative of most patients in teaching hospitals. However, many academic hospitals care for a disproportionate number of minority patients. In addition, the medical students surveyed from the medical school where these patients receive their care revealed the same pattern of responses as did the other schools. This suggests that the discrepancy in attitudes between patients and students was true even for medical students accustomed to interacting with this particular sample of patients.
Some may question whether it is fair to compare students' and patients' attitudes, because patients' attitudes toward the importance of being informed when they are interacting with medical students may merely reflect their misunderstanding of the risks of interacting with medical students. For example, patients may not know how closely supervised medical students are when they make surgical incisions. However, patients placed great importance on being asked permission before allowing medical students to perform pelvic or rectal examinations while they were under anesthesia. The importance they place on being asked permission before allowing medical students to examine these very private parts of their bodies does not reflect their fear of the medical risks of such examinations. If our study does not prove a change in attitudes over time, our results would still be disturbing because they show a gap between patients' and students' attitudes toward informed consent for very private acts, such as pelvic and rectal examinations under anesthesia. For example, not a single patient stated that it was unimportant to be told that a medical student is going to perform a rectal examination under anesthesia before surgery, but 12% of preclinical students and 28% of clinical students stated it was unimportant.
Medical school and the residency training that follows instill many important changes in people becoming physicians. Most of these changes are undoubtedly for the better. For example, students and residents become better at coping with death and illness and become more comfortable discussing sensitive personal matters with patients. At the same time, however, we need to determine whether other changes occur that are not for the better. The change in medical students' beliefs about the importance of clearly identifying themselves to their patients suggests a troubling erosion of respect for patients' rights to be informed. To counteract this erosion, medical schools should emphasize the importance of asking permission before medical students interact with patients—including a clear explanation of the role and actions of medical students. Such education must not only occur in medical ethics curricula, but also be reinforced during clinical rotations—especially in surgical settings. Medical schools and teaching hospitals should make concerted efforts to request permission before allowing medical students to interact with anesthetized patients in surgical settings. Although most medical students remain aware of the importance of informing patients of their student status, there appears to be room for improvement.
Acknowledgments
This research was funded by the Annenberg Public Policy Foundation through its support of the Center for Bioethics' Project on Informed Consent.
The authors gratefully acknowledge Ellen Wise for assistance in manuscript preparation; Christine Weeks, Dave Weeks, and Laurel Siegel for research assistance; David Asch, Katrina Armstrong, and Genevieve Noone Parsons for comments on an earlier draft; and all the subjects who responded to the survey.
REFERENCES
- 1.Dworkin G, Cassell EJ. The “student doctor” and the wary patient. Hastings Cent Rep. 1982;12:27–8. [PubMed] [Google Scholar]
- 2.Simpson CL. Misrepresentation of medical students in teaching hospitals. Med Trial Technique Q. 1977;23(3):233–70. [PubMed] [Google Scholar]
- 3.Christakis D, Feudtner C. Ethics in a short white coat: the ethical dilemmas that medical students confront. Acad Med. 1993;68(4):249–54. doi: 10.1097/00001888-199304000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Cohen DL, McCullough LB, Kessel RWI, Apostolides AY, Heiderich KJ, Alden ER. A national survey concerning the ethical aspects of informed consent and role of medical students. J Med Educ. 1988;63:821–9. doi: 10.1097/00001888-198811000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Cohen DL, Kessel RWI, McCullough LB. Pelvic examinations by medical students. Am J Obstet Gynecol. 1989;161(4):1013–4. doi: 10.1016/0002-9378(89)90775-8. [DOI] [PubMed] [Google Scholar]
- 6.Feudtner C, Christakis D, Christakis NA. Do clinical clerks suffer ethical erosion? Students' perceptions of their ethical environment and personal development. Acad Med. 1994;69(8):670–9. doi: 10.1097/00001888-199408000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Cohen DL, McCullough LB, Kessel R, Apostolides AY, Alden ER, Heiderich KJ. Informed consent policies governing medical students' interactions with patients. J Med Educ. 1987;62:789–98. doi: 10.1097/00001888-198710000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Lawton FG, Redman CWE, Luesley DM. Patient consent for gynaecological examination. Br J Hosp Med. 1990;44(5):326–9. [PubMed] [Google Scholar]
- 9.Bibby J, Boyd N, Redman CWE. Consent for vaginal examination by students on anaesthetized patients. Lancet. 1988;2(8620):1150. doi: 10.1016/s0140-6736(88)90577-6. Letter. [DOI] [PubMed] [Google Scholar]
- 10.Silver-Isenstadt A. Times of a medical student activist. JAMA. 1996;276(17):1435. doi: 10.1001/jama.276.17.1435. [DOI] [PubMed] [Google Scholar]
- 11.Annas GJ. The Rights of Patients: The Basic ACLU Guide to Patient Rights. 2nd ed. Totowa, NJ: Humana Press; 1992. [Google Scholar]
- 12.Silver-Isenstadt A, Ubel PA. Medical student name tags: identification or obfuscation? J Gen Intern Med. 1997;12:669–71. doi: 10.1046/j.1525-1497.1997.07138.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howell JD. Why medical students are “medical students.”. J Gen Intern Med. 1997;12:718–9. doi: 10.1046/j.1525-1497.1997.07148.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Academic Press; 1977. [Google Scholar]
- 15.Asch DA, Jedreziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50(10):1129–36. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]