Abstract
OBJECTIVE
To determine if a mailed patient education brochure (addressing demonstrated reasons for vaccination refusal) would result in a higher rate of influenza vaccination than a mailed postcard reminder without educational content.
DESIGN
Randomized, controlled trial.
SETTING
Urban, predominantly African-American, low-income community.
PARTICIPANTS
There were 740 community-dwelling individuals aged 65 years and older in the study.
MEASUREMENTS
Receipt of influenza vaccination and beliefs about influenza and influenza vaccination were measured by telephone survey self-report.
MAIN RESULTS
We successfully contacted 202 individuals (69.9%) who received the postcard reminder and 229 individuals (71.1%) who received the educational brochure. People receiving the educational brochure were more likely to report influenza vaccination during the previous vaccination season than those who received the postcard reminder (66.4% vs 56.9%, p = .04). They also reported more interest in influenza vaccination in the coming year. (66.5% vs 57.1%, p = .05).
CONCLUSIONS
A mailed educational brochure is more effective than a simple reminder in increasing influenza vaccination rates among inner-city, elderly patients.
Keywords: influenza, vaccination, educational reminder, elderly, inner-city population
Influenza vaccination reduces mortality from influenza and is recommended for all Americans aged 65 years or older.1–6 However, only 65% of elderly whites and 50% of elderly African Americans reported influenza vaccination in 1997.7
Both simple and educational patient reminders have been found to increase influenza vaccination rates.8–17 However, the mailed reminders studied varied widely in design, content, and effectiveness, making it difficult to determine if educational information adds any benefit to a simple reminder. The only published studies comparing a simple reminder with an educational patient reminder were completed almost 20 years ago when only 10% to 20% of eligible individuals were vaccinated and public educational efforts had only just begun.16,17 Furthermore, sociodemographic characteristics of the study populations were not provided, raising questions about their generalizability to minority populations. Because educational information increases the cost of the mailing and could obscure the primary message of the reminder, comparative, empiric information is needed.
In this article, we report the results of a randomized controlled trial assessing the effect of educational content on vaccination rates in an urban, predominantly African-American population.
METHODS
Study Population and Subject Selection
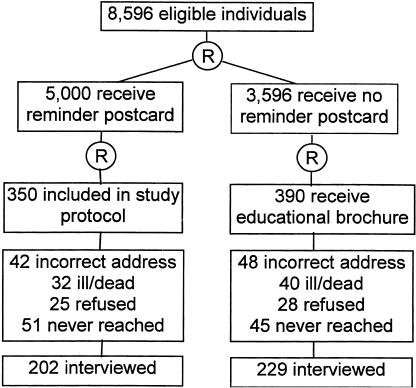
In October 1996, a random sample of 5,000 of the 8,596 community-dwelling West Philadelphia residents aged 65 years or older who received care at a University of Pennsylvania primary care site between September 1, 1995, and September 1, 1996, were mailed a simple postcard as an influenza vaccine reminder by the University of Pennsylvania Health System. To compare how an alternative mailing would influence vaccination rates, we simultaneously mailed an educational brochure to 390 of the 3,596 eligible individuals who were not mailed a postcard reminder. Following vaccination season, we compared the vaccination rate of a random sample of 350 individuals who received the postcard reminder and 390 individuals who received the educational brochure (Fig. 1). Budgetary constraints necessitated the inclusion of 350 (rather than 390) individuals from the postcard reminder arm. This sample size was adequate to provide 80% power to detect an absolute difference of 10% between groups with a type I error of 0.05, assuming a survey response rate of 70% and a 50% vaccination rate in the postcard reminder group. Assuming that vaccination reduces influenza-related mortality by 50%, a 10% increase in vaccination could result in an overall reduction in influenza mortality of 5%, thus preventing approximately 1,000 deaths each year. The study protocol was approved by the Human Subjects Committee of the University of Pennsylvania Institutional Review Board.
FIGURE 1.
Subject selection and response. The circled letter “R” indicates randomly selected.
Interventions
Patient Education Brochure
We evaluated 11 educational brochures from organizations in the Philadelphia area to see if they were comprehensible at a 12th-grade reading level, focused on established reasons for vaccination refusal identified in prior studies, and included information about Medicare coverage and local access to vaccination. Because no brochure met all criteria, we developed a new 2-page educational brochure (Appendix A).
Appendix A.
Educational Brochure
Postcard Reminder
The postcard reminder informed recipients that influenza is a leading cause of sickness, hospitalization, and death in people over 65 years of age and that it was time for influenza vaccination.
Instrument Development and Data Collection
A telephone questionnaire measured receipt of vaccination between October 1996 and April 1997, intention to get vaccinated the following year, health beliefs about influenza and influenza vaccination, sociodemographic characteristics, and prior vaccination history. After pilot testing, trained interviewers made at least four attempts to reach each study subject between March and October 1997.
Statistical Analysis
Statistical analysis was based on intention to treat. All tests of statistical significance were two-tailed. Baseline comparability of the two respondent groups was assessed using χ2test for categorical variables and Student's t test for continuous variables. The primary analysis used ordinary χ2test to compare the proportion reporting vaccination in each group. Exploratory post-hoc stratified analyses examined the effect of the brochure according to previous vaccination use and history of vaccination side effects.
RESULTS
Seventy percent (202) of the individuals in the postcard reminder arm and 71% (229) of the individuals in the educational brochure arm completed the telephone interview (Fig. 1). The study population had a mean age of 77 years (range, 65 to 104 years), a mean of 12 years of education (range, 4 to 23 years), and was 75% female and 76% African American. Eighty-one percent of study subjects had a previous influenza vaccination, 23% had previously refused the influenza vaccine, and 25% reported prior side effects from vaccination. These characteristics did not differ between groups (p values >.07).
Subjects receiving the educational brochure were significantly more likely to report receiving influenza vaccination during the following 1996–97 vaccination season (66.4% vs 56.9%, p = .04) and more likely to intend to be vaccinated in the coming year (66.5% vs 57.1%, p = .05). No differences were found between groups in beliefs about influenza or influenza vaccination, including belief in the severity of influenza, personal susceptibility to influenza, the benefits of the influenza vaccination, and the risks of the influenza vaccination (all p values >.1).
The effect of the educational brochure appeared to be greatest among individuals who had not had a previous vaccination or had previously refused vaccination (Table 1)These trends were suggestive but not statistically significant.
Table 1.
Educational Brochure Effect Accordingto Vaccination History
| Vaccinated, % | ||||
|---|---|---|---|---|
| History | Brochure | Reminder | Relative Risk | 95%ConfidenceInterval |
| Prior vaccination | ||||
| Yes (n= 338) | 75.3 | 70.9 | 1.06 | .93–1.21 |
| No (n= 78) | 20.0 | 9.3 | 2.15 | .69–6.75 |
| Prior vaccination refusal | ||||
| Yes (n= 93) | 40.9 | 22.4 | 1.82 | .97–3.42 |
| No (n= 312) | 71.9 | 67.9 | 1.06 | .91–1.23 |
| Prior side effects | ||||
| Yes (n= 99) | 60.0 | 51.9 | 1.16 | .82–1.64 |
| No (n= 302) | 67.8 | 56.3 | 1.20 | 1.00–1.45 |
DISCUSSION
The present trial suggests that patient information targeting common reasons for refusing influenza vaccination is more effective in convincing individuals to get vaccinated than a reminder alone. Although the absolute increase in vaccination rate was less than 10%, the public health benefit could be substantial. Influenza vaccination decreases influenza-related mortality by up to 60%.3 Assuming that 90% of deaths occur in individuals aged 65 years and older and 50% of individuals will be vaccinated with a reminder alone, increasing the vaccination rate by 10% would have saved more than 1,500 lives in the 1996–97 influenza season alone.1 Furthermore, these results were found in an inner-city, low-income population (a group often believed to be the most difficult to reach with preventive care); the benefit of educational mailings in more traditionally receptive populations may be even greater.18
These results are consistent with the only previously published randomized trials comparing an educational mailer with a simple reminder.16,17 In the late 1970s, adding educational content to a reminder increased vaccination rates by 15% to 25%. In an urban, predominantly African-American, low-income population, the increase is currently only 9.5% but is still present. Together, these studies provide strong evidence that educational information mailed to patients can change health behavior and, thus, improve health outcomes.
Our study has several limitations. Because insurance claims data substantially underestimate vaccination rates, we measured receipt of influenza vaccination by self-report.19 Although some respondents may have misclassified their vaccination status, this misclassification is unlikely to be related to the intervention, thus actually making it more difficult to have a found effect of the brochure.20 Survey respondents may have differed from nonrespondents. Although it is possible that nonrespondents were less likely to have been vaccinated, response rates did not differ by intervention and are unlikely to bias the results of our study.
As the U.S. population ages, the threat from influenza grows. Action must be taken to prevent unnecessary deaths. Adding educational content to influenza reminders is a simple and effective intervention that may save hundreds of lives each year.
Acknowledgments
This project was supported by the University of Pennsylvania Research Foundation. Dr. Armstrong is supported by Primary Care Research Training Grant T32-PE-10026. Dr. Ubel is a Robert Wood Johnson Generalist Physician Faculty Scholar and the recipient of a career development award in health services research from the Department of Veterans Affairs.
REFERENCES
- 1.Centers for Disease Control. Prevention and control of influenza: Recommendations of the Advisory Committee on Immunization Practices. MMWR. 1997;46 [Google Scholar]
- 2.Public Health Service . Healthy People 2000: National Health Promotion and Disease Prevention Objectives. Washington, DC: US Department of Health and Human Services, Public Health Service; 1991. pp. 121–3. [Google Scholar]
- 3.Nichol KL, Margolis KL, Wuorenma J. The efficacy and cost-effectiveness of vaccination against influenza among elderly persons living in the community. N Eng J Med. 1994;331:778–84. doi: 10.1056/NEJM199409223311206. [DOI] [PubMed] [Google Scholar]
- 4.Fedson DS, Wadja A, Nicol JP. Clinical effectiveness of influenza vaccination in Manitoba. JAMA. 1993;270:1956–61. [PubMed] [Google Scholar]
- 5.Foster DA, Talsma A, Furumoto-Dawson A, Ohmit SE, Margulies JR, Arden NH, Monto AS. Influenza vaccine effectiveness in preventing hospitalization for pneumonia in the elderly. Am J Epidemiol. 1992;136:296–307. doi: 10.1093/oxfordjournals.aje.a116495. [DOI] [PubMed] [Google Scholar]
- 6.Gross PA, Hermogenes AW, Sacks HS, Lau J, Levandowski RA. The efficacy of influenza in elderly persons: a meta-analysis and review of the literature. Ann Intern Med. 1995;123:518–27. doi: 10.7326/0003-4819-123-7-199510010-00008. [DOI] [PubMed] [Google Scholar]
- 7.Center for Disease Control and Prevention Influenza and Pneumococcal Vaccination Levels Among Adults Aged ≥65 Years—United States, 1997. MMWR. 1998;47:797–802. [PubMed] [Google Scholar]
- 8.McDowell I, Newell C, Rosser W. Comparison of three methods of recalling patients for influenza vaccination. Can Med Assoc J. 1986;135:991–7. [PMC free article] [PubMed] [Google Scholar]
- 9.Buchner DM, Larson EB, White RF. Influenza vaccination in community elderly: a controlled trial of postcard reminders. J Am Geriatr Soc. 1987;35:755–60. doi: 10.1111/j.1532-5415.1987.tb06354.x. [DOI] [PubMed] [Google Scholar]
- 10.Mullooly JP. Increasing influenza vaccination among high-risk elderly: a randomized controlled trial of a mail cue in an HMO setting. Am J Public Health. 1987;77:626–7. doi: 10.2105/ajph.77.5.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brimberry R. Vaccination of high risk patients for influenza: a comparison of telephone and mail reminder methods. J Fam Pract. 1988;26:397–400. [PubMed] [Google Scholar]
- 12.Turner BJ, Day SC, Borenstein B. A controlled trial to improve delivery of preventive care: physician or patient reminders. J Gen Intern Med. 1989;4:403–9. doi: 10.1007/BF02599691. [DOI] [PubMed] [Google Scholar]
- 13.Nichol KL, Korn JE, Margolis KL, Poland GA, Petzel RA, Lofgren RP. Achieving the national health objective for influenza immunization: success of an institution-wide vaccination program. Am J Med. 1990;89:156–60. doi: 10.1016/0002-9343(90)90293-m. [DOI] [PubMed] [Google Scholar]
- 14.Barton MB, Schoenbaum SC. Improving influenza vaccination performance in an HMO setting: the use of computer-generated reminders and peer comparison feedback. Am J Public Health. 1990;80:534–6. doi: 10.2105/ajph.80.5.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moran WP, Nelson K, Wofford JL, Velez R, Case LD. Increasing influenza immunization among high-risk patients: education or financial incentive? Am J Med. 1996;101:612–20. doi: 10.1016/S0002-9343(96)00327-0. [DOI] [PubMed] [Google Scholar]
- 16.Larson EB, Bergman J, Heidrich F, Alvin BL, Scneeweiss R. Do postcard reminders improve influenza vaccination compliance? A prospective trial of different postcard “cues”. Med Care. 1982;20:639–48. doi: 10.1097/00005650-198206000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Carter WB, Beach LR, Inui TS. The flu shot study: using multiattribute theory to design a vaccination intervention. Org Behav Hum Decis Proc. 1986;38:378–91. doi: 10.1016/0749-5978(86)90007-5. [DOI] [PubMed] [Google Scholar]
- 18.Doak CC, Doak LG, Root JH. Teaching patients with low literacy skills. Philadelphia: Lippincott; 1985. [Google Scholar]
- 19.Hutchinson BG. Measurement of influenza vaccination status of the elderly by mailed questionnaire: response rate, validity and cost. Can J Public Health. 1989;80:271–5. [PubMed] [Google Scholar]
- 20.Hennekens CH, Buring JE. Epidemiology in medicine. Boston: Little, Brown and Company; 1987. [Google Scholar]