Abstract
OBJECTIVE
To compare rates of contact for mental problems and receipt of appropriate antidepressant medication management for persons in the general population with major depression in the United States and Ontario, Canada.
DESIGN
Survey using the U.S. National Comorbidity Survey and the Mental Health Supplement of the Ontario Health Survey.
PARTICIPANTS
All persons with major depression as described in DSM-III-R in the previous 12 months, from a multistage random sample of persons aged 21 to 54 years living in households in the United States (n=574) and Ontario (n=250) in 1990.
MEASUREMENTS AND MAIN RESULTS
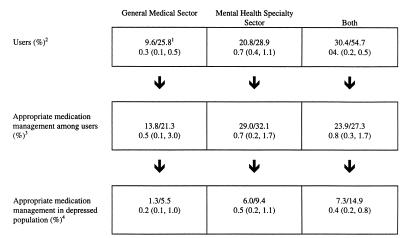
Self-reported contact with general medical or mental health specialty providers for mental problems and appropriate medication management, defined as a combination of antidepressant medication use and four or more visits to any provider within the previous 12 months, were the main outcome measures. The proportion of depressed persons receiving appropriate management was lower in the United States than in Ontario (7.3% vs 14.9% in Ontario, adjusted odds ratio [AOR] 95% CI 0.4; 95% confidence interval [CI] 0.2, 0.8). This difference was largely the result of fewer Americans than Canadians having any mental health care from general medical physicians (9.6% in the United States vs 25.8% in Ontario; AOR 0.3; 95% CI 0.1, 0.5) rather than from specialty providers (20.8% in the United States vs 28.9% in Ontario; AOR 0.7; 95% CI 0.4, 1.1). These between-country differences were much greater for the poor than for those with higher incomes. The Ontario–United States AOR of making contact with either type of clinical provider was 7.5 (95% CI 2.7, 20.7) for lowest-income persons but 2.1 (95% CI 0.3, 5.6) for highest-income persons. The proportions of depressed recipients of any mental health care who received appropriate management were similar between countries (23.9% in the United States vs 27.7% in Ontario; AOR 0.8; 95% CI 0.3, 1.7).
CONCLUSIONS
Most persons with depression in the United States and Ontario do not receive appropriate medication management. The rate of appropriate medication management in the United States relative to Ontario is lower largely because there is less contact with general medical physicians for mental problems, especially for the poor. Economic barriers, rather than knowledge and attitudinal factors, appear to explain this difference.
Keywords: mental health, medication management, major depression
A ccess to mental health care is an important focus of health policy debates in the United States, in part, because of concerns by clinicians and policy makers that many people with mental illness do not receive appropriate treatment. 1 Recent federal legislative initiatives have sought to mandate more generous insurance coverage for ambulatory and hospital services related to mental illness. 2, 3 However, the impact of such initiatives on access to mental health care is unclear, especially for vulnerable populations such as the poor and those with major psychiatric disorders.
Major depression is an excellent reference condition to address access issues because it is highly prevalent, 4, 5 it strongly impacts morbidity, 6, 7 and effective treatments for it can markedly improve patient outcomes. 6, 8 Indeed, indicators of appropriate medication management of depression may be incorporated into U.S. national quality reporting standards for providers such as those proposed by the National Council on Quality Assurance. 9
Canada is often cited as a useful comparative benchmark for the United States because its comprehensive health insurance system provides an important opportunity to assess the impact of expanded coverage on access to care. Many persons in the United States do not have mental health insurance, and for those who do, the coverage for ambulatory and hospital care is often limited. 10 By contrast, Canada has universal and comprehensive insurance coverage for mental health services. For instance, in Ontario there are no limits on outpatient visits or inpatient stays for psychiatric care. There is minimal patient cost sharing for ambulatory mental health services. 11 However, there are some potential constraints on the availability of providers. Only physicians are reimbursed through the government insurance plan, while psychologists and social workers are reimbursed either through salaried positions in government-funded mental health centers or by out-of-pocket payments.
In this article, we compare use of mental health care in general, and receipt of appropriate antidepressant medication management in particular, for persons in the general population with major depression in the United States and Ontario. We focus on antidepressant medication use because it is a major treatment approach available in medical settings. We use a marker of appropriate medication management (any use of an antidepressant and having made four or more mental health visits to a provider) that approximates the recommendations of the Agency for Health Care Policy and Research depression guidelines panel. 12
Receipt of appropriate medication management may differ between the United States and Ontario for several reasons related to patient, provider, and system factors. Because differences in severity of illness may result in different treatment rates, we controlled in the analysis for differences across depressed groups in severity of depression and comorbidity. Differences in access between countries may also be the result of differences in provider mix because rates of treatment for depression have been shown to be higher for patients seen by mental health specialists than for patients seen by general physicians. 13 Thus, we examined between-country differences in utilization from all providers and separately by clinical specialty. Finally, differences between countries may be due to differences in economic barriers to care. Thus, we examined between-country differences by socioeconomic and insurance status.
The study addressed four questions: Does the proportion of depressed persons making contact with any provider (general physician or mental health specialist) for a mental problem differ between countries? If so, do respondent attitudes toward mental health care, or structural factors such as socioeconomic status or insurance status, explain these between-country differences? Once depressed persons make contact with a provider, are there between-country differences in the likelihood of their receiving appropriate medication management? If so, does either illness severity or treatment setting (general medical vs psychiatric specialty sector) explain these between-country differences?
METHODS
Study Population
The study sample is representative of all household residents with major depression aged 21 to 54 years living in the United States (n= 574) and Ontario (n= 250) during 1990. Persons meeting DSM-III-R criteria for mania during the study period were excluded.
Data
We used the U.S. National Comorbidity Survey (NCS) and the Mental Health Supplement to the Ontario Health Survey (OHS Supplement), parallel population-based surveys that collected detailed information on mental health care use, disorders, health status, and disabilities by administering face-to-face interviews. The diagnostic interview used in both the NCS and the OHS Supplement was a modified version of the Composite International Diagnostic Interview (CIDI), a structured interview designed to be used by nonclinician interviewers. 14 The surveys used the same questions about the utilization of services for psychiatric disorders.
The NCS and the OHS Supplement both used two-part sampling designs. The part 1 NCS was a psychiatric interview administered to a nationally representative probability sample of 8,098 respondents in the household population of the coterminous United States (response rate 82.4%). The part 2 NCS was a risk factor battery and questions about utilization of services administered to all part 1 respondents in the age range 15 to 24 years (99.4% of whom completed part 2), all others who screened positive for any lifetime psychiatric disorder in part 1 (98.1% of whom completed part 2), and a random subsample of other part 1 respondents (99.0% of whom completed part 2). A total of 5,877 interviews were completed in the part 2 NCS; 574 of the interviewees were aged 21 and older and met diagnostic criteria for major depression within the previous 12 months.
The OHS Supplement administered the same psychiatric diagnostic questions and service utilization questions to a follow-up sample consisting of one random respondent from each household participating in the last two replicates of the OHS. The OHS is a probability survey of Ontario households similar in content to the U.S. National Health Interview Survey. The response rate for the OHS Supplement was 69.3% (n= 9,953); 250 of the respondents were aged 21 and older and met criteria for depression in the previous 12 months.
Approach to the Analysis
The likelihood of receiving appropriate management can be decomposed into two components—the probability of receiving any service and, once making contact, the likelihood that care will be appropriate. We focused first on predicators of the likelihood of any contact with a general medical or specialty provider for a mental problem within the previous 12 months. We then examined between-country differences in the likelihood of receiving appropriate management for persons receiving any mental health care.
Variables
In the first part of the analysis the dependent variable was any contact with a general medical or mental health specialty provider for a mental problem. The outpatient utilization questions probed respondents about the timing and number of visits within the previous year to several types of providers for problems with “nerves or emotions.” Mental health specialty contact is defined as (1) seeing a psychiatrist or psychologist regardless of setting; (2) seeing a social worker or counselor in an emergency department, a psychiatric outpatient clinic, a drug or alcohol outpatient clinic, a doctor's office, a drop-in center, or a program for persons with emotional problems or problems with drugs or alcohol; or (3) seeing a nurse in a psychiatric outpatient clinic, a drug or alcohol outpatient clinic, a drop-in center, or a program for persons with emotional problems or problems with drugs or alcohol. General medical sector contact is defined as (1) seeing a physician other than a psychiatrist regardless of place, or (2) seeing a nurse, occupational therapist, or other allied health professional in either a hospital emergency department or a doctor's private office. Persons were considered to be users of specialty care if they received any service from a specialty provider. Persons were considered to be users of general medical service if they did not receive any services from the specialty sector but received some service from the general medical sector. This division is consistent with previous studies of treatment differences across specialties. 15, 16
In the second part of the analysis, we examined the distribution of appropriate management among users of any services. The dependent variables were (1) self-reported antidepressant use within the previous 12 months, (2) a binary variable indicating four or more visits for a mental problem within either the general medical or mental health specialty sector in the previous 12 months, and (3) appropriate management defined as the presence of both variables 1 and 2. The questions ascertaining medication use queried respondents about any use of several classes of drugs prescribed under the supervision of a doctor in the past 12 months. One question specifically ascertained use of antidepressants by giving examples of product brand names (Prozac, Elavil, etc.).
All independent variables for the first part of the analysis were chosen because they have been previously shown to be associated with medical service use in general, 17 and with mental health service use in particular. 18 These included predisposing factors (age, gender, family size, and education), enabling factors (income and insurance), and need factors (psychiatric and medical comorbidity, impairments, and depression severity). For incomes we used a purchase power parity factor (0.763) to deflate Canadian dollars to U.S. dollars. 19 In both surveys family income is categorical. Similarities in categories allowed us to create four dummy variables: the lowest is less than $15,300 (U.S. dollars) and the highest is greater than $45,800 (U.S. dollars). In both surveys, income information is missing in approximately 15% of cases. For these cases, we imputed income using the same set of covariates in each country. 20 Family size is included as a continuous variable. Education (four dummy variables) is categorized as less than high school graduate, high school graduate, some college, and college graduate.
We also created a number of binary variables indicating the presence of comorbidity, impairments, and depression severity: two variables indicating psychiatric comorbidity within the previous 12 months (one for generalized anxiety, panic, or agoraphobia disorders and one for dysthymia); a variable indicating one or more chronic medical conditions; a variable indicating disability related to mental health (3 or more days within the 30 days prior to the interview that a person cut down or was unable to perform his or her usual activities because of a mental problem); and seven variables indicating depression severity (one variable indicating suicidal ideation within the previous 2 years; three variables indicating the duration of symptoms within the previous 12 months [≤6 weeks, 7–23 weeks, ≥24 weeks]; and three variables indicating the number of lifetime episodes of depression [1, 2–3, 4, or more]).
In the first part of the analysis, we also examined whether between-country differences in the likelihood of contact were explained by cultural factors such as attitudes toward seeking mental health care or structural barriers associated with financial or insurance factors. Respondents in both surveys were asked two questions to assess their perceived need for help because of an emotional problem. Persons who saw any professional for a mental health problem were asked: “Was this something you wanted to do or did you go only because someone else put pressure on you?” Persons who indicated that they wanted to go were considered to have a perceived need for care. Persons who did not go to a professional for a mental health problem were asked: “Was there a time during the past 12 months when you thought you needed to see someone for a problem with your nerves or emotions or your use of alcohol or drugs?” Persons who answered yes to this question were considered to perceive a need for mental health care. For these persons, additional questions were asked about perceived reasons for not going (allowing for multiple reasons). Finally, respondents in the United States were asked whether they have insurance coverage for mental and physical health care. We created three insurance categories: full private coverage, Medicaid, and no mental health insurance.
Because of limited sample size in the second part of the analysis (only 188 depressed persons in the United States and 124 depressed persons in Ontario reported contact with a health professional for an emotional problem within the past year), we limited the number of independent variables. Thus, we included clinical specialty (general medical vs specialty), a measure of clinical severity, and country. For clinical severity we created a binary variable indicating the presence of any of the following conditions: comorbid dysthymia (double depression), recent suicidal ideation, prolonged episode (≥24 weeks) within the past year, or four or more lifetime episodes. These are clinical indicators for specialty care in clinical guidelines for treatment of depression. 12
Analysis
The first part of the analysis focused on between-country differences in any use of the general medical or specialty sector for a mental problem. We first examined the proportion of persons reporting contact by clinical specialty and country. We then examined the association of any use with the demographic, socioeconomic, and clinical variables within country using logistic regression. We tested for interactions between covariates within country and found none. Thus, we report only main effects for the within-country models. We then tested for differences between countries by constructing interaction terms between selected covariates and country in a combined logistic regression model based on the within-country analyses. This final model regressed any service use on the following independent variables: age, gender, education, family size, income, psychiatric comorbidity (anxiety and dysthymia disorders), any chronic medical condition, mental disability, the depression severity measures (recent suicidal ideation, symptoms duration, and number of lifetime episodes of depression), and a set of interaction terms for income indicator variables and country. From this model we calculated Ontario–United States adjusted odds ratios of any use, by income levels. We also conducted descriptive analyses of perceived attitudinal and structural barriers to care by country.
In the second part of the analysis, we examined the proportion of users of any services who received antidepressant medication, four or more visits, and appropriate management (the combination of reported antidepressant use and four or more visits) by clinical specialty group, depression severity, and country.
Both surveys used complex sampling designs, so all analyses were performed using weights that adjust for variations in within-household probabilities of selection owing to variation in household size, for differential nonresponse, and, in the case of the NCS, for differential probabilities of selection into the part 2 subsample. Variances for the regression coefficients were estimated using a Taylor series expansion technique, 21 which accounts for the different sampling strategies in each survey. Wald tests were used to assess the significance of coefficients. All analyses were run using STATA 5.0 (College Station, Tex.).
RESULTS
Distribution of Clinical and Sociodemographic Variables by Country
As shown in Table 1, the distributions of age, gender, and education were similar for depressed persons across country, but the proportion of depressed persons with low income was higher in the United States than in Ontario (χ 2 [3 df] = 8.6, p < .05). Illness severity was similarly high across countries: a substantial proportion of persons reported psychiatric comorbidities (general anxiety disorder or dysthymia), disability (3 or more days within the previous 30 days that a person cut down or was unable to perform his or her usual activity), suicidal ideation within the previous 2 years, and multiple previous episodes. Americans, however, were more likely to have a shorter duration of depression symptoms during the previous year (χ 2 [2 df] = 18.0, p < .01).
Table 1.
Population Characteristics*

Utilization by Clinical Sector and Country
As shown in Figure 1, the proportion of persons with depression in the previous year who received appropriate management was lower in the United States than in Ontario (7.3% in the United States vs 14.9% in Ontario, United States–Ontario odds ratio adjusted for age, gender, and education 22 = 0.4; 95% confidence interval [CI] 0.2, 0.8). This is largely because fewer Americans than Canadians reported making contact with the general medical or mental health specialty sector within the previous 12 months (30.4% in the United States vs 54.7% in Ontario; adjusted odds ratio [AOR] 0.4; 95% CI 0.2, 0.5). This lower probability of use in the United States was largely due to lower use of the general medical sector (9.6% in the United States vs 25.8% in Ontario; AOR 0.3; 95% CI 0.1, 0.5) rather than lower use of specialty sector (20.8% in the United States vs 28.9% in Ontario; AOR 0.7; 95% CI 0.4, 1.1). By contrast, the proportions of users receiving appropriate management were much more similar between countries (23.9% in the United States vs 27.3% in Ontario; AOR 0.8; 95% CI 0.3, 1.7) and, thus, do not account for the overall lower receipt of appropriate management in the United States versus Ontario.
Figure 1.
Utilization of mental health services by sector and country.
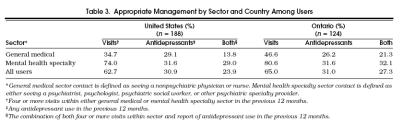
Associations of Clinical and Sociodemographic Variables with Any Use
There was generally a weak independent association of morbidity and impairment factors with any mental health care use, and there were no significant differences between countries (Table 2) The presence of suicidal ideation, anxiety disorders, and greater duration of symptoms in the previous 12 months were positively associated with any use across countries. However, the association of income with use differed between the two countries. In the United States there was a positive association of income with use; while in Ontario there was a trend toward a negative association. The test of the interaction (the set of interaction terms for country × income categories) in the full model was borderline statistically significant (χ 2 [df] = 8.3, p= .05). The Ontario–United States AOR for contact among persons with the lowest income was 7.8 (95% CI 2.7, 20.7), but for the highest income group it was 2.1 (95% CI 0.3, 8.6).
Table 2.
Adjusted Odds Ratios for Any Mental Health Care Use by Country*
Perceived Barriers to Care
Our data suggest that the lower probability of contact in the United States versus Ontario is due more to between-country differences in economic barriers than to differences in attitudes toward seeking help. Overall, there was little difference in the proportion of depressed persons who perceived a need for care (56.1% in the United States vs 65.0% in Ontario, p= .10). However, among persons who did perceive need, Americans were much less likely than Canadians to make contact (32.8% vs 52.4% of Canadians, p < .05). Among persons who perceived need but did not make contact, there were no significant between-country differences in the proportion of persons reporting that they did not go because they believed that they would get better on their own, that they could solve the problem on their own, or that care would not be helpful (58.8% in the United States vs 63.0% in Ontario, p= 0.8). By contrast, there was a substantial between-country difference in perceived economic and structural barriers as reasons for not getting professional help among persons who perceived need. For instance, more Americans reported that services were too expensive (31.7% vs 7.7%, p < .05) or that they were unsure where to go for them (33.0% vs 15.2%, p < .05). But the effect of health insurance status in the United States on the probability of making contact and on the between-country difference in use was not significant.
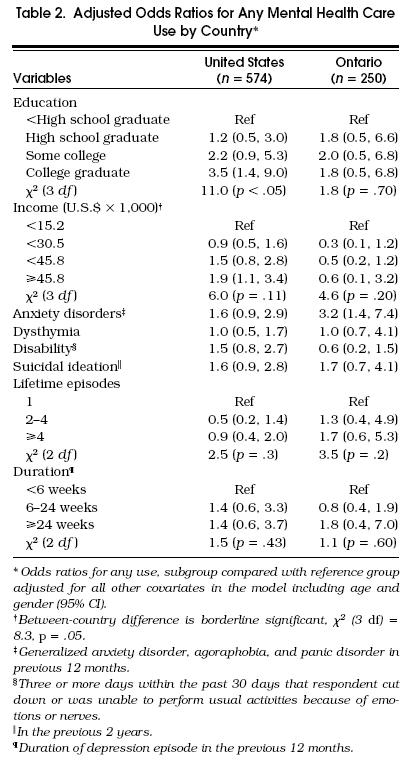
Appropriate Management Among Users of Any Service
As shown in Table 3, patterns of care among users of any mental health care services were similar by country. Approximately two thirds of users in both samples reported four or more visits within either the general medical or specialty sector (62.7% in the United States vs 65.0% in Ontario), one third reported antidepressant medication use (30.9% in the United States vs 31.0% in Ontario), and one quarter reported receiving both antidepressants and four or more visits (23.9% in the United States vs 27.3% in Ontario).
Table 3.
Appropriate Management by Sector and Country Among Users
Furthermore, in both countries, persons seen by specialists were more likely to receive appropriate management than those seen by general physicians, especially for persons with greater severity of illness. Twenty-nine percent of Americans and 32.1% of Canadians who saw specialists for mental health problems received appropriate management compared with 13.8% of Americans and 21.3% of Canadians who saw general physicians. The specialists-to-generalists odds ratio for receiving appropriate management was 2.1 (adjusted for age, gender, clinical severity, and country; 95% CI 1.1, 4.3). However, for persons with higher clinical severity, the AOR was 4.8 (95% CI 1.7, 14.1). For persons with lower clinical severity, the odds ratio was 0.9 (95% CI 0.3, 2.8). This interaction between sector and clinical severity was significant (χ 2 = 2.4, p < .05).
DISCUSSION
Our results show that most persons with depression in the United States and Ontario do not receive appropriate medication management. Overall, only 7.3% of the Americans and 14.9% of the Canadians in this study with symptoms meeting criteria for major depression within the previous year received appropriate medication management. Failure to make contact accounted for a substantial part of this low rate of treatment and largely explains the lower treatment rate in the United States compared with Ontario. Only 30.4% of persons in the United States compared with 54.7% of persons in Ontario with depression in the previous year received any services for a mental problem from the general medical or specialty sectors. The low rate of such contact in the United States is consistent with previous studies. 23, 24 These results are also consistent with our previous articles showing lower use rates of mental health services in the United States than in Ontario for persons with any mental morbidity. 20, 25, 26
Our results are also consistent with previous research suggesting that knowledge and attitude factors may play a more important role in mental health care seeking than illness severity and impairments. 18, 27 We found that clinical factors were not significantly associated with care seeking but that factors such as low problem recognition and negative attitudes toward care seeking were important barriers to care. Approximately 40% of depressed persons who did not make contact did not perceive the need for professional help. Furthermore, more than half of those who did perceive need for professional help did not seek it because they felt that they would get better on their own or that professional help would do no good.
These factors, however, do not explain the large between-country difference in contact because the distributions of these factors are similar in the two countries. Financial barriers appear to play a more important role. Persons in the United States perceived more financial barriers to care than did persons in Ontario. This finding parallels our results showing that between-country differences are greater for persons with lowest incomes than for persons with highest incomes. However, our crude measure of mental health insurance coverage made it difficult to test the effects of insurance coverage on between-country differences in use across income groups.
Among users, the treatment patterns were quite similar between countries. In both countries, approximately two thirds of these persons reported four or more visits to either general physicians or mental health specialists, one third reported antidepressant use, and one quarter reported both medication use and four or more visits during the study period. Furthermore, in both countries, treatment rates were higher for persons seeing specialists than for those seeing general physicians, especially for those with greater clinical severity. This difference was largely due to greater use of antidepressants by persons with more severe illness seen in the specialty sector. Our findings are consistent with those of previous studies showing that medication treatment by mental health providers is more responsive to clinical severity than treatment by general physicians. 28 This issue may be particularly important in Ontario, where the role of general physicians in the care of depressed persons is much greater than in the United States.
Limitations
Several aspects of the study merit comment. Although our definition of appropriate medication management is based on published clinical guidelines, there may not be consensus among all providers in the community regarding approaches to treatment for depression. 29 We may have underestimated the rate of appropriate management if respondents underreported mental health visits or if persons terminated care with fewer than four visits because they improved (11.6% of U.S. users and 15.6% of Ontario users). Excluding from the analysis those persons who improved, however, had little effect on our between-country findings. In addition, a small number of users who were classified as having inappropriate management based on too few visits were still receiving care as of the interview date (4.4% of U.S. users and 1.5% of Ontario users). Excluding these persons did not substantially change our results. We could have overestimated appropriate management, however, because we did not have detailed information on the content of visits or on antidepressant dosages. Several studies have shown that many persons use antidepressants at dosages that are too low. 28, 30
Implication
Our findings suggest that a system that has expanded access to mental health care, such as exists in Ontario, may improve rates of treatment of depression, especially for the poor. Our results support the contention of mental health care advocates in the United States that reducing financial barriers to mental health care can improve quality. Opponents of expanding mental health coverage in the United States have raised concerns that reducing financial barriers to mental health care may lead to overuse of services for those with less need.
Even under a more generous insurance coverage scenario such as exists in Ontario, however, the prevalence of appropriate medical management for depression remains far too low. Our results suggest several strategies to improve care. First, the low rate of contact due to knowledge and attitudinal barriers supports the importance of efforts to educate the public, especially those at high risk, about depression and its treatments. Second, our findings clearly reinforce the notion that the treatment of depression represents a missed opportunity for clinicians in both countries. Only one third of depressed persons who made contact with a professional for a mental problem reported taking antidepressants in the previous year. Other studies have shown that low treatment rates for depression are, in part, the result of low recognition, particularly in the general medical sector. 31 Sturm and Wells found that low levels of appropriate care among users diminishes the cost-effectiveness of depression treatment and that quality improvement, especially in the primary care setting, may substantially improve the cost-effectiveness of care for depression. 6 Thus, clinical guidelines that educate providers, especially general physicians, about the recognition and treatment of depression may improve quality. This strategy may be particularly useful in Ontario, where there is relatively greater reliance on general practitioners to manage the treatment of depression. Future studies should determine whether the higher rates of treatment in Ontario versus the United States, especially for the poor, result in better outcomes.
Acknowledgments
Collaborating National Comorbidity Study sites and investigators are The Addiction Research Foundation (Robin Room), Duke University Medical Center (Dan Blazer, Marvin Swartz), Harvard University (Richard Frank), Johns Hopkins University (James Anthony, William Eaton, Philip Leaf), the Max Planck Institute of Psychiatry—Clinical Institute (Hans-Ulrich Wittchen), the Medical College of Virginia (Kenneth Kendler), the University of Michigan (Lloyd Johnston, Ronald Kessler, Roderick Little), New York University (Patrick Shrout), SUNY Stony Brook (Evelyn Bromet), The University of Toronto (R. Jay Turner), and Washington University School of Medicine (Linda Cottler, Andrew Heath).
Collaborating Mental Health Supplement to the Ontario Health Survey agencies and investigators are The Ontario Mental Health Foundation (Dugal Campbell), The Clarke Institute of Psychiatry (Paula Goering, Elizabeth Lin), McMaster University (Michael Boyle, David Offord), and the Ontario Ministry of Health (Gary Catlin).
References
- 1.Arons BS, Frank RG, Goldman HH, McGuire TG, Stephens S. Mental health and substance abuse coverage under health reform. Health Aff (Millwood) 1994;13(1):192–205. doi: 10.1377/hlthaff.13.1.192. [DOI] [PubMed] [Google Scholar]
- 2.Koyanagi C, Maines J. What did the health care reform debate mean for mental health policy? Health Aff (Millwood) 1995;14(3):124–9. doi: 10.1377/hlthaff.14.3.124. [DOI] [PubMed] [Google Scholar]
- 3.Congress agrees on new health benefits, mandates . The Week in Medicine. (Chicago, Ill): Marketplace; 1996. Oct 7. [Google Scholar]
- 4.Weissman MM, Bland RC, Canino GJ, et al. Cross-national epidemiology of major depression and bipolar disorder. JAMA. 1996;276:293–9. [PubMed] [Google Scholar]
- 5.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 6.Sturm R, Wells KB. How can care for depression become more cost effective? JAMA. 1995;273:51–8. [PubMed] [Google Scholar]
- 7.Greenberg PE, Stiglin LE, Finkelstein SN, Berndt ER. Depression: a neglected major illness. J Clin Psychiatry. 1993;54:419–24. [PubMed] [Google Scholar]
- 8.Mintz J, Mintz LI, Arruda MJ, Hwang SS. Treatments of depression and the functional capacity to work. Arch Gen Psychiatry. 1992;49:761–8. doi: 10.1001/archpsyc.1992.01820100005001. [DOI] [PubMed] [Google Scholar]
- 9.McGlynn EA. Choosing chronic disease measures for HEDIS: conceptual framework and review of seven clinical areas. Manag Care Q. 1996;4:54–77. [PubMed] [Google Scholar]
- 10.Frank RG, Goldman HH, McQuire TG. A model mental health benefit in private insurance. Health Aff (Millwood) 1992;11(3):98–117. doi: 10.1377/hlthaff.11.3.98. [DOI] [PubMed] [Google Scholar]
- 11.Ontario Ministry of Health . Putting People First: The Reform of Mental Health Services in Ontario. Toronto, Ont: Queen's Printer for Ontario; 1993. [Google Scholar]
- 12.McIntyre JS, Zarin DA, Pincus AJ. The role of psychotherapy and the treatment of depression: review of two practice guidelines. Arch Gen Psychiatry. 1996;53:291–3. doi: 10.1001/archpsyc.1996.01830040021004. [DOI] [PubMed] [Google Scholar]
- 13.Wells KB, Sturm R. Care for depression in a changing environment. Health Aff (Millwood) 1995;14(3):78–89. doi: 10.1377/hlthaff.14.3.78. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization . Composite International Diagnostic Interview. Geneva, Switzerland: World Health Organization; 1990. Report No. CIDI, Version 1.0. [Google Scholar]
- 15.Leaf PJ, Livingston MM, Tischler GL, Weissman MM, Holzer CE, Myers JK. Contact with health professionals for the treatment of psychiatric and emotional problems. Med Care. 1985;23:1322–37. doi: 10.1097/00005650-198512000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Wells KB, Manning WG, Duan N, Newhouse JP, Ware JE. Sociodemographic factors and the use of outpatient mental health services. Med Care. 1986;24(1):75–85. doi: 10.1097/00005650-198601000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Aday LA. Indicators and predictors of health services utilization. In: Williams SJ, Torrens PR, editors. Introduction to Health Services. 4th ed. Vol. 59. Albany, NY: Delmar Publishers Inc.; 1993. In. [Google Scholar]
- 18.Leaf PJ, Bruce ML, Tischler GL, et al. Factors affecting the utilization of speciality and general medical mental health services. Med Care. 1988;26:9–26. doi: 10.1097/00005650-198801000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Organization for Economic Cooperation and Development . National Accounts: Main Aggregates I. Vol. 157. Paris, France: Organization for Economic Cooperation and Development; 1992. [Google Scholar]
- 20.Katz SJ, Kessler RC, Frank RG, Leaf P, Lin B. Mental health service use and socioeconomic status in the United States and Ontario. Inquiry. 1997;34(1):38–49. [PubMed] [Google Scholar]
- 21.Binder DA. On the variances of asymptomatically normal estimators from complex surveys. Int Stat Rev. 1983;51:279–92. [Google Scholar]
- 22.Graling PR, Grant JM. Demographics and patient treatment choice in stage I breast cancer. AORN J. 1995;62(3):376–84. doi: 10.1016/s0001-2092(06)63578-3. [DOI] [PubMed] [Google Scholar]
- 23.Narrow WE, Regier DA, Rae DS, Manderscheid RW, Locke BZ. Use of services by persons with mental and addictive disorders: findings from the National Institute of Mental Health epidemiologic catchment area program. Arch Gen Psychiatry. 1993;50:95–107. doi: 10.1001/archpsyc.1993.01820140017002. [DOI] [PubMed] [Google Scholar]
- 24.Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK. The defacto U.S. addictive disorders service system: ECA prospective one-year prevalence and service use rates. Arch Gen Psychiatry. 1993;50:85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- 25.Katz SJ, Kessler RC, Frank RG, Leaf P, Lynn B, Edlund M. The use of outpatient mental health services in the United States and Ontario: the impact of mental health morbidity and perceived need for care. Am J Pub Health. 1997;87:1136–43. doi: 10.2105/ajph.87.7.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kessler RC, Frank RG, Edlund N, Katz SJ, Lynn B, Leaf P. Differences in the use of psychiatric outpatient services between United States and Ontario. N Engl J Med. 1997;336:551–7. doi: 10.1056/NEJM199702203360806. [DOI] [PubMed] [Google Scholar]
- 27.Klerman GL, Olfson M, Leon AC, Weisman MM. Measuring the need for mental health care. Health Aff (Millwood) 1992;11(3):23–33. doi: 10.1377/hlthaff.11.3.23. [DOI] [PubMed] [Google Scholar]
- 28.Wells KB, Katon W, Rogers B, Camp P. Use of minor tranquilizers and antidepressant medications by depressed outpatients: results from the medical outcomes study. Am J Psychiatry. 1994;151(5):694–700. doi: 10.1176/ajp.151.5.694. [DOI] [PubMed] [Google Scholar]
- 29.Persons JB, Thase ME, Crits-Christoph P. The role of pyschotherapy in the treatment of depression: review of true practice guidelines. Arch Gen Psychiatry. 1996;53(4):283–90. doi: 10.1001/archpsyc.1996.01830040013003. [DOI] [PubMed] [Google Scholar]
- 30.Katon W, Von Korff M, Lynn E, et al. Adequacy and duration of anti-depressant treatment in primary care. Med Care. 1992;30:67–76. doi: 10.1097/00005650-199201000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Perez-Stable EJ, Miranda J, Munoz RF, Ying YW. Depression in medical outpatients. Underrecognition and misdiagnosis. Arch Intern Med. 1990;150(5):1083–8. doi: 10.1001/archinte.1990.00390170113024. [DOI] [PubMed] [Google Scholar]