Abstract
OBJECTIVE
To summarize current information on the relation between CD4 counts and the risk of different HIV-related diseases.
MEASUREMENTS AND MAIN RESULTS
MEDLINE search of English language articles between 1985 and 1996 using the medical subject heading (MeSH) term “CD4 lymphocyte count” and searches using key words of multiple HIV-related diseases were conducted. Some HIV-related diseases can be stratified to different CD4 count levels. Regardless of their CD4 count, HIV-infected patients are susceptible to sinusitis, Kaposi's sarcoma, community-acquired pneumonia, and oral hairy leukoplakia. In advanced HIV, when CD4 is below 200/mm 3, Pneumocystis carinii pneumonia, toxoplasmosis, progressive multifocal leukoencephalopathy, Mycobacterium avium complex, molluscum contagiosum, and bacillary angiomatosis all increase in incidence. In very advanced HIV disease, when CD4 counts are below 50/mm 3, patients are at risk of pseudomonas pneumonia, cytomegalovirus retinitis, central nervous system lymphoma, aspergillosis, and disseminated histoplasmosis.
Keywords: CD4 count, HIV-related disease, risk stratification
Risk of many HIV-related disease varies with the patient's degree of immunosuppression. CD4 count, CD4 percentage, quantitative HIV-1 RNA (viral load), neopterin level, and p-24 antigenemia have all been proposed as surrogate markers of immune function. Among these, CD4 counts and quantitative HIV-1 RNA levels are used most commonly. Quantitative HIV-1 RNA is a more reliable surrogate marker for progression to AIDS and death than CD4 counts.1 However, HIV-1 RNA levels can vary up to fourfold during acute infections,2 and there is no defined relation between HIV-1 RNA levels and risk of opportunistic infections. Consequently, the CD4 count remains the most useful test for estimating risk of many HIV-related diseases.
The advent of combination antiretroviral therapy using protease inhibitors, nucleoside analogues, and nonnucleoside reverse transcriptase inhibitors has led to substantial increases in CD4 counts in some patients. Whether these increased CD4 counts alter patients' risk of opportunistic infections is uncertain. Until studies clarify this issue, it is prudent to base patients' management on their CD4 counts before initiation of antiretroviral therapy.
Technical and physiologic variability contributes to the overall variability of CD4 counts. In one study of clinically stable, HIV-infected patients, CD4 counts varied by 13.7% when measured 4 weeks apart. Laboratory variance accounted for 15% of the overall variance, while physiologic variance accounted for 85%.3 In a different study, CD4 counts varied by 25% when measured 8 weeks apart.4 CD4 counts vary throughout the day and in response to acute infections, smoking, exercise, and stress.5 One approach to address this variability is to draw specimens at a similar time of the day, use the same laboratory to process the specimens, and use serial tests to guide management decisions.
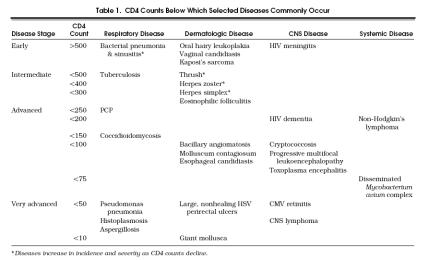
By appreciating the CD4 counts below which certain HIV-related diseases occur (Table 1) and by appreciating the various ways diseases manifest at different CD4 counts, clinicians can focus their differential diagnoses and improve the efficiency of their diagnostic evaluations. This review examines the relation between CD4 counts and common HIV-related diseases that cause respiratory, central nervous system (CNS), dermatologic, and systemic problems.
Table 1.
CD4 Counts Below Which Selected Diseases Commonly Occur
METHODS
A MEDLINE search for relevant English language articles between 1985 and 1996 was completed using the MeSH term “CD4 lymphocyte count.” We also searched using the terms Pneumocystis carinii, tuberculosis, pneumonia, sinusitis, cryptococcus, toxoplasmosis, dermatology, Mycobacterium avium complex, lymphoma, and CNS. All were combined with the term HIV. Studies were reviewed for information on CD4 count and correlation with specific diseases.
RESPIRATORY DISEASE
HIV-infected individuals frequently present with nonspecific respiratory symptoms including cough, dyspnea, and chest pain. In patients with CD4 counts above 500/mm 3, sinusitis, community-acquired pneumonia, and viral infections commonly account for these symptoms. Tuberculosis can occur at any CD4 count, but it usually occurs when the CD4 count is below 500/mm 3. Once the CD4 count drops below 200/mm 3, the incidence of Pneumocystis carinii pneumonia (PCP), fungal pneumonia, and more severe forms of sinusitis and bacterial pneumonia, including those caused by Pseudomonas aeruginosa, rises dramatically.
Sinusitis
The incidence of sinusitis is greater in HIV seropositive individuals than in HIV-seronegative individuals.6 Although sinusitis can occur at any CD4 count, it increases in incidence and severity as CD4 counts decline. In patients with CD4 counts less than 200/mm 3, sinusitis often involves multiple sinuses, responds incompletely to antibiotic therapy, and becomes chronic.
Patients commonly complain of fever, headache, nasal congestion, and facial tenderness.7, 8 However, symptoms and signs may be nonspecific or absent, particularly in patients with CD4 counts under 200/mm.3 In the review by Godofsky et al. of 72 cases of sinusitis, 10 patients (14%) presented with fever and headache as their only symptoms.7 Of the 75 patients with sinusitis that Zurlo et al. studied, 19 patients (25%) with radiographic evidence of active sinusitis were asymptomatic.8
When patients do not respond to antibiotics targeted at common pathogens such as Streptococcus pneumonia, Viridans streptococcus, and Haemophilus influenzae, Pseudomonas aeruginosa should be considered. Although Pseudomonas aeruginosa rarely causes sinusitis in HIV-seronegative individuals, it may account for 16% to 18% of cases of sinusitis in HIV-infected individuals and is associated with a high rate of recurrent disease.9, 10 When the CD4 count is below 150/mm 3, fungal pathogens such as Aspergillus should also be considered.11
Pneumonia
Like sinusitis, bacterial pneumonia occurs with increased incidence in HIV-infected individuals. In the cohort of 1,281 patients studied by Wallace et al., those infected with HIV had an eightfold greater incidence of bacterial pneumonia than the HIV-seronegative control subjects.12 Although bacterial pneumonia can occur at any CD4 count, its incidence and severity are inversely related to CD4 counts.13 In one series, the incidence of bacterial pneumonia in patients with CD4 counts less than 250/mm 3 approached the incidence of PCP.12 Risk factors include CD4 counts less than 200–250/mm 3, smoking illicit drugs,12, 14 and perhaps, intravenous drug use and cigarette smoking.13
The most common pathogen is Streptococcus pneumoniae. Among patients with pneumococcal pneumonia, HIV-infected individuals are more likely to develop bacteremia and recurrent disease. However, clinical presentation and response to therapy are similar to those in HIV-seronegative individuals.15 Other pathogens include Staphylococcus aureusHaemophilus influenzae,16 and in advanced AIDS, Pseudomonas aeruginosa. Community-acquired Pseudomonas aeruginosa pneumonia occurs at a mean CD4 count of 25/mm 3, often in patients who lack traditional risk factors for pseudomonas infection such as neutropenia, indwelling central venous catheters, or chronic steroid use. It can present with cavitary infiltrates on chest radiography, and is associated with a high relapse rate.17, 18
Although the widespread use of prophylactic antibodies has lowered the incidence of PCP, it remains a common complication of HIV infection. PCP often presents with gradually progressive dyspnea, fever, and cough. It rarely occurs when the CD4 count is greater than 250/mm 3. In one series, Jensen et al. found that only 3 (5%) of 61 cases of PCP occurred with a CD4 count above 250/mm 3.19 Wallace et al. found that only 4 (9%) of 43 patients with PCP had CD4 counts greater than 250/mm 3, and 3 of these 4, had CD4 counts less than 333/mm 3.12 In another series, Masur et al. found that only 3 (6%) of 49 patients with PCP had CD4 counts greater than 200/mm 3.20 Risk factors for PCP include CD4 less than 200/mm 3, prior PCP, and oral thrush. These, as well as unexplained fevers for longer than 2 weeks, are indications for instituting PCP prophylaxis.
Fungal pneumonia occurs in advanced AIDS. Patients usually have indolent, nonspecific symptoms including fever, fatigue, weight loss, cough, and dyspnea lasting weeks to months. Coccidioidomycosis occurs most commonly in the Southwestern states and in patients with CD4 counts below 150/mm 3.21 Disseminated histoplasmosis occurs in the Mississippi and Ohio River valleys and in patients with CD4 counts below 50/mm 3. In a series of 980 patients with AIDS studied by Nightingale et al., those with disseminated histoplasmosis had a median CD4 count of 33/mm 3.22 Aspergillosis is rare and occurs in patients with CD4 counts below 50/mm 3.23 Risk factors for aspergillosis include neutropenia, corticosteroid use, and underlying lung disease. Cryptococcus neoformans can cause pulmonary disease, but more commonly causes meningitis (see Central Nervous System Disease section).
Tuberculosis
Tuberculosis tends to occur at CD4 counts below 500/mm 3. In a series of 193 HIV-infected patients with tuberculosis, only 4 (2.1%) had CD4 counts above 500/mm 3.24 Whether the incidence of tuberculosis increases as the CD4 count declines is unclear.12, 21
Compared with HIV-seronegative patients, HIV-seropositive patients have a greater risk of developing disseminated primary tuberculosis, reactivation of latent tuberculosis, extrapulmonary disease, and adverse reactions to antituberculosis medications.25 Patients infected with HIV and tuberculosis, particularly those with CD4 counts less than 200/mm 3, are also more likely to be anergic.
Patients with advanced immunosuppression may have atypical chest radiographs. Rather than the typical cavitary, upper lobe lesions seen in immunocompetent patients, individuals with AIDS often have lower lobe parenchymal infiltrates, pleural effusions, or mediastinal adenopathy. In Long and colleagues' series of 67 HIV-infected patients with tuberculosis, 80% of those with AIDS had atypical chest radiographs.26 In a study by Keiper et al., 21 (81%) of 26 patients with tuberculosis who had CD4 counts below 200/mm 3 presented with atypical chest radiographs, compared with only 1 (11%) of 9 subjects with CD4 counts above 200/mm 3.27
DERMATOLOGIC DISEASE
HIV-infected individuals are susceptible to a wide range of dermatologic disease. Candidiasis, seborrheic dermatitis, oral hairy leukoplakia, herpes simplex lesions of the mouth and anus, varicella zoster, anal warts, and skin cancers are all more prevalent in HIV-infected individuals.6
Candida
Candida can cause oropharyngeal, vaginal, cutaneous, and esophageal disease. Oropharyngeal candidiasis, often the first sign of HIV infection, is the most prevalent oral lesion in HIV-infected individuals,28 and it tends to occur at CD4 counts less than 500/mm 3.29 Esophageal candidiasis occurs at CD4 counts below 100/mm 3 and is usually accompanied by odynophagia. In a study by Imam et al., vaginal candidiasis occurred at a mean CD4 count of 506/mm 3, oropharyngeal candidiasis occurred at a mean CD4 count of 230/mm 3, and esophageal candidiasis occurred at a mean CD4 count of 30/mm 3.30
Viral Infections
Recurrent varicella-zoster virus infection is an early opportunistic infection that occurs more frequently in HIV-infected individuals than in HIV-seronegative individuals and tends to occur at CD4 counts less than 400/mm 3.31
Incidence and recurrence of oral and genital herpes simplex virus (HSV) infections may increase as immunosuppression increases.32 In a study by Crowe et al., all nine cases of anogenital HSV infection occurred at CD4 counts less than 300/mm 3.29 In advanced AIDS, perirectal HSV may present as large, confluent, nonhealing, ulcerations reminiscent of decubitus ulcers.
Molluscum contagiosum is a cutaneous poxvirus infection that leads to formation of characteristic, umbilicated skin lesions. In HIV-seronegative adults, lesions arise in genital regions, whereas in HIV-seropositive adults, lesions more commonly involve the face and trunk. In a series of 10 patients with mollusca, Koopman et al. found that all had CD4 counts below 100/mm 3.33 In a review of 27 patients with mollusca, Schwartz et al. found a mean CD4 count of 85.7/mm 3, and there was an inverse relation between CD4 count and number of lesions. Giant mollusca developed in three patients, all of whom had profound immunosuppression and CD4 counts under 10/mm 3.34
The occurrence of oral hairy leukoplakia is not clearly related to CD4 count, but it is a marker for progression to AIDS.35 In a retrospective and prospective cohort study of 434 HIV-infected men, Holmberg et al. found that those with oral hairy leukoplakia had a mean CD4 count of 340/mm 3.6
Folliculitis
Folliculitis occurs frequently in HIV-infected individuals. In can occur at any CD4 count and is usually caused by Staphylococcus aureus. At CD4 counts below 300/mm 3, patients can develop eosinophilic folliculitis, a clinical entity unique to HIV-infected individuals 36 that is characterized by discrete, pruritic, erythematous, follicular papules on the trunk or face and is associated with eosinophilia and increased serum IgE levels.37
Kaposi's Sarcoma
Kaposi's sarcoma is the most common tumor and the fourth most common dermatologic condition (after candidiasis, seborrheic dermatitis, and folliculitis) seen in HIV-infected individuals. The suspected etiologic agent is Kaposi's sarcoma–associated herpes virus (human herpes virus 8).38 An infectious etiology may explain why Kaposi's sarcoma is most common in homosexual and bisexual men, especially those with a history of oral or anal sexual contacts. In a series of 130 cases, 75% had CD4 counts less than 200/mm 3. However, low CD4 counts were not a prerequisite for the development of Kaposi's sarcoma, as 10% of the patients in this series had CD4 counts greater than 500/mm 3.39 Painless, violaceous skin lesions are typical, but they may progress to painful, indurated lesions. In advanced HIV disease, they may also involve the oral mucosa, gastrointestinal tract, and lungs.
Bacillary Angiomatosis
Bacillary angiomatosis causes angiomatous skin lesions that may mimic Kaposi's sarcoma. It occurs at CD4 counts less than 100/mm 3 and is caused by Bartonella henslaeB. quintana. In a review of patients with bacillary angiomatosis, Koehler and Tappero found the average CD4 count was 57/mm 3.40
CENTRAL NERVOUS SYSTEM DISEASE
HIV-infected individuals are susceptible to the same viral and bacterial CNS infections as immunocompetent hosts. In addition, HIV-infected individuals may develop HIV meningitis at any CD4 count. Classically, this occurs at the time of seroconversion. In contrast, most HIV-related diseases that affect the CNS occur in advanced stages of AIDS. AIDS dementia occurs when the CD4 count is below 200/mm 3.41 Cryptococcal meningitis, toxoplasmosis, and progressive multifocal leukoencephalopathy occur when the CD4 count is below 100/mm 3. Central nervous system lymphoma occurs even later when the CD4 count is below 50/mm 3.
Toxoplasmosis
Toxoplasmosis is the most common opportunistic infection of the CNS in patients with AIDS. It occurs when the CD4 count is below 100/mm 3 and frequently presents with subacute onset of focal neurologic deficits with or without evidence of generalized cerebral dysfunction.42
Cryptococcal Meningitis
Cryptococcal meningitis is caused by Cryptococcus neoformans, an encapsulated yeast found worldwide, and is most likely to occur at CD4 counts less than 100/mm 3. Symptoms are often indolent and nonspecific. Fever is the most common symptom and occurs in 62% to 88% of patients. The most common nonmeningeal site of involvement is the lung. However, dissemination often occurs by the time pulmonary disease is diagnosed, and meningitis is found in 60% to 70% of patients with primary pulmonary symptoms.43
Cytomegalovirus Retinitis
Cytomegalovirus (CMV) retinitis develops in 7.5% to 30% of AIDS patients during the course of their illness. It usually occurs at CD4 counts less than 50/mm 3. In one series of 26 patients with CMV retinitis, the mean CD4 count was 15.6/mm 3.44 Patients present with painless visual disturbances including floaters, blurred vision, decreased visual acuity, and visual field deficits. Visual loss progresses rapidly over days to weeks, and retinal detachment may occur as a late complication.45
Progressive Multifocal Leukoencephalopathy
Progressive multifocal leukoencephalopathy occurs at CD4 counts less than 100/mm 3. In a review of 15 cases, the mean CD4 count was 84/mm 3. This disease is caused by a ubiquitous papovavirus, the JC virus, which infects myelin-producing oligodendrocytes and causes cell lysis and demyelinization. Patients can present with focal neurologic deficits or with a rapid decline in mental status.46
Central Nervous System Lymphoma
After toxoplasmosis, CNS lymphoma 47 is the second leading cause of intracerebral masses in HIV-infected patients and usually occurs when the CD4 count is below 50/mm 3. Patients present with headaches, seizures, and cranial neuropathies. Diagnosis is by computed tomography or magnetic resonance imaging and biopsy, since malignant cells are found in the cerebrospinal fluid in only 15% to 25% of patients.
SYSTEMIC DISEASES
HIV-infected individuals often develop nonspecific symptoms and signs such as fatigue, malaise, anorexia, weight loss, and night sweats. In later stages of immunosuppression, these are frequently caused by opportunistic infections and malignancies.
Non-Hodgkin's Lymphoma
HIV-infected individuals have a 60-fold greater risk of developing non-Hodgkin's lymphoma than the general population. Non-Hodgkin's lymphoma 29 usually occurs at CD4 counts under 200/mm 3 and can present with fevers, weight loss, and night sweats. Compared with non-HIV-infected individuals, those with HIV tend to have more extranodal disease, higher-stage and higher-grade disease, and a poorer response to chemotherapy.
Mycobacterium avium Complex
Mycobacterium avium complex is now one of the most common opportunistic infections associated with AIDS. The incidence of the disseminated complex as the first opportunistic infection has increased from 5.7% of patients from 1985 to 1988 to 23.3% of patients from 1989 to 1990. Mycobacterium avium complex usually occurs in those with CD4 counts below 75/mm 3 and rarely in those with CD4 counts above 100/mm 3. It commonly presents with persistent fever, weight loss, night sweats, and diarrhea.48
SUMMARY
Regardless of their CD4 count, HIV-infected patients are susceptible to sinusitis, community-acquired pneumonia, oral hairy leukoplakia, Kaposi's sarcoma, and HIV meningitis. Once their CD4 counts drop below 500/mm 3, they are at risk of developing tuberculosis, thrush, herpes simplex, and herpes zoster. In advanced HIV, when their CD4 counts are below 200/mm 3, PCP, coccidioidomycosis, bacillary angiomatosis, molluscum contagiosum, cryptococcal meningitis, toxoplasmosis, progressive multifocal leukoencephalopathy, Mycobacterium avium complex, and non-Hodgkin's lymphoma all increase in incidence. In very advanced HIV, when their CD4 counts are below 50/mm 3, they are at risk of pseudomonas pneumonia, CMV retinitis, CNS lymphoma, aspergillosis, and histoplasmosis. By appreciating these characteristic changes in disease incidence, and by knowing a patient's CD4 count, clinicians should be better able to develop differential diagnoses and plans for diagnostic evaluation.
REFERENCES
- 1.Mellors JW, Rinaldo CR, Gupta P, White RM, Todd JA, Kingsley LA. Prognosis in HIV-1 infection predicted by the quantity of the virus in plasma. Science. 1996;272:1167–70. doi: 10.1126/science.272.5265.1167. [DOI] [PubMed] [Google Scholar]
- 2.A study of HIV RNA viral load in AIDS patients with bacterial pneumonia. J Acquir Immune Defic Syndr Hum Retrovirol. 1996;13(1):23–6. doi: 10.1097/00042560-199609000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Baroud JM, Haley L, Montaner JS, Murphy C, Januszewska M, Schechter MT. Quantification of the variation due to laboratory and physiologic sources in CD4 lymphocyte counts of clinically stable HIV-infected individuals. J Acquir Immune Defic Syndr. 1995;10(suppl 2):S67–73. [PubMed] [Google Scholar]
- 4.Hughes MD, Stein DS, Gundacker HM, Valentine FT, Phair JP, Volberding PA. Within-subject variation in CD4 lymphocyte count in asymptomatic human immunodeficiency virus infection: implications for patient monitoring. J Infect Dis. 1994;169:28–36. doi: 10.1093/infdis/169.1.28. [DOI] [PubMed] [Google Scholar]
- 5.Turner BJ, Hecht FM, Ismail RB. CD4+ T-lymphocyte measures in the treatment of individuals infected with human immunodeficiency virus type 1. Arch Intern Med. 1994;154:1561–73. [PubMed] [Google Scholar]
- 6.Holmberg SD, Buchbinder SP, Conley LJ, et al. The spectrum of medical conditions and symptoms before acquired immunodeficiency syndrome in homosexual and bisexual men infected with the human immunodeficiency virus. Am J Epidemiol. 1995;141:395–404. doi: 10.1093/oxfordjournals.aje.a117441. [DOI] [PubMed] [Google Scholar]
- 7.Godofsky EW, Zinreich J, Armstrong M, Leslie JM, Weikel CS. Sinusitis in HIV-infected patients: a clinical and radiographic review. Am J Med. 1992;93:163–70. doi: 10.1016/0002-9343(92)90046-e. [DOI] [PubMed] [Google Scholar]
- 8.Zurlo JJ, Feuerstein IM, Lebovics R, Lane HC. Sinusitis in HIV-1 infection. Am J Med. 1992;93:157–62. doi: 10.1016/0002-9343(92)90045-d. [DOI] [PubMed] [Google Scholar]
- 9.Milgram LM, Rubin JS, Rosenstreich DL, Small CB. Sinusitis in human immunodeficiency virus infection, typical and atypical organisms. J Otolaryngol. 1994;23:450–3. [PubMed] [Google Scholar]
- 10.Tami TA. The management of sinusitis in patients infected with the human immunodeficiency virus (HIV) Ear Nose Throat J. 1995;74:360–3. [PubMed] [Google Scholar]
- 11.Meyer RD, Gaultier CR, Yamashita JT, et al. Fungal sinusitis in patients with AIDS: report of 4 cases and review of the literature. Medicine. 1994;73:69–78. doi: 10.1097/00005792-199403000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Wallace JM, Rao AV, Glassroth J, et al. Pulmonary Complications of HIV Infection Study Group. Respiratory illness in persons with human immunodeficiency virus infection. Am Rev Respir Dis. 1993;148:1523–9. doi: 10.1164/ajrccm/148.6_Pt_1.1523. [DOI] [PubMed] [Google Scholar]
- 13.Hirschtick RE, Glassroth J, Jordan MC, et al. Bacterial pneumonia in persons infected with the human immunodeficiency virus. N Engl J Med. 1995;333:845–51. doi: 10.1056/NEJM199509283331305. [DOI] [PubMed] [Google Scholar]
- 14.Caiaffa WT, Viahov D, Graham NMH, et al. Drug smoking, Pneumocystis carinii pneumonia, and immunosuppression increased risk of bacterial pneumonia in human immunodeficiency virus-seropositive injection drug users. Am J Respir Crit Care Med. 1994;150:1493–8. doi: 10.1164/ajrccm.150.6.7952605. [DOI] [PubMed] [Google Scholar]
- 15.Janoff EN, Breiman RF, Daley CL, Hopewell PC. Pneumococcal disease during HIV infection. Epidemiologic, clinical, and immunologic perspectives. Ann Int Med. 1992;117:314–24. doi: 10.7326/0003-4819-117-4-314. [DOI] [PubMed] [Google Scholar]
- 16.Farizo KM, Buehler JW, Chamberland ME, et al. Spectrum of disease in persons with human immunodeficiency virus infection in the United States. JAMA. 1992;267:1798–1805. [PubMed] [Google Scholar]
- 17.Baron AD, Hollander H. Pseudomonas aeruginosa bronchopulmonary infection in late human immunodeficiency virus disease. Am Rev Respir Dis. 1993;148:992–6. doi: 10.1164/ajrccm/148.4_Pt_1.992. [DOI] [PubMed] [Google Scholar]
- 18.Schuster MG, Norris AH. Community-acquired Pseudomonas aeruginosa pneumonia in patients with HIV infection. AIDS. 1994;8:1437–41. doi: 10.1097/00002030-199410000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Jensen BN, Gerstoft J, Hojlyng N, et al. Pulmonary pathogens in HIV-infected patients. Scand J Infect Dis. 1990;22:413–20. doi: 10.3109/00365549009027072. [DOI] [PubMed] [Google Scholar]
- 20.Masur H, Ognibene FP, Yarchoan R, et al. CD4 counts as predictors of opportunistic pneumonias in human immunodeficiency virus (HIV) infection. Ann Intern Med. 1989;111:223–31. doi: 10.7326/0003-4819-111-3-223. [DOI] [PubMed] [Google Scholar]
- 21.Wheat J. Histoplasmosis and coccidioidomycosis in individuals with AIDS. A clinical review. Infect Dis Clin North Am. 1994;8:467–82. [PubMed] [Google Scholar]
- 22.Nightingale SD, Parks JM, Pounders SM, et al. Disseminated histoplasmosis in patients with AIDS. South Med J. 1990;83:624–30. doi: 10.1097/00007611-199006000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Keating JJ, Rogers T, Petrou M, et al. Management of pulmonary aspergillosis in AIDS: an emerging clinical problem. J Clin Pathol. 1994;47:805–9. doi: 10.1136/jcp.47.9.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Girardi E, Antonucci G, Armignacco O, et al. Tuberculosis and AIDS: a retrospective, longitudinal, multicentre study of Italian AIDS patients. J Infect Dis. 1994;28:261–9. doi: 10.1016/s0163-4453(94)91693-4. [DOI] [PubMed] [Google Scholar]
- 25.Chaisson RE, Schecter GF, Theuer CP, et al. Tuberculosis in patients with the acquired immunodeficiency syndrome. Clinical features, response to therapy, and survival. Am Rev Respir Dis. 1987;136:570–4. doi: 10.1164/ajrccm/136.3.570. [DOI] [PubMed] [Google Scholar]
- 26.Long R, Maycher B, Scalcini M, Manfreda J. The chest roentgenogram in pulmonary tuberculosis patients seropositive for human immunodeficiency virus type 1. Chest. 1991;99:123–7. doi: 10.1378/chest.99.1.123. [DOI] [PubMed] [Google Scholar]
- 27.Keiper MD, Beumont M, Elshami A, et al. CD4 T lymphocyte count and the radiographic presentation of pulmonary tuberculosis. Chest. 1995;107:74–80. doi: 10.1378/chest.107.1.74. [DOI] [PubMed] [Google Scholar]
- 28.Barr CE. Oral diseases in HIV-1 infection. Dysphagia. 1992;7:126–37. doi: 10.1007/BF02493444. [DOI] [PubMed] [Google Scholar]
- 29.Crowe SM, Carlin JB, Stewart KI, Lucas CR, Hoy JF. Predictive value of CD4 lymphocyte numbers for the development of opportunistic infections and malignancies in HIV-infected persons. J Acquir Immune Defic Syndr. 1991;4:770–6. [PubMed] [Google Scholar]
- 30.Imam N, Carpenter CCJ, Mayer KH, et al. Hierarchical pattern of mucosal candida infections in HIV-seropositive women. Am J Med. 1990;89:142–6. doi: 10.1016/0002-9343(90)90291-k. [DOI] [PubMed] [Google Scholar]
- 31.Conant MA. Fungal infections in AIDS and other immunocompromised patients. J Am Acad Dermatol. 1994;31:S47–50. doi: 10.1016/s0190-9622(08)81267-4. [DOI] [PubMed] [Google Scholar]
- 32.Drew WL, Buhles W, Erlich KS. Herpesvirus infections (cytomegalovirus, herpes simplex virus, varicella zoster virus). How to use gancyclovir (DHPG) and acyclovir. Infect Dis Clin North Am. 1988;2:495–509. [PubMed] [Google Scholar]
- 33.Koopman RJJ, van Merriènboer FCJ, Vreden SGS, Dolmans WMV. Molluscum contagiosum; a marker for advanced HIV infection. Br J Dermatol. 1992;126:528. doi: 10.1111/j.1365-2133.1992.tb11835.x. . Letter. [DOI] [PubMed] [Google Scholar]
- 34.Schwartz JJ, Myskowski PL. Molluscum contagiosum in patients with human immunodeficiency virus infection: a review of twenty-seven patients. J Am Acad Dermatol. 1992;27:583–8. doi: 10.1016/0190-9622(92)70226-6. [DOI] [PubMed] [Google Scholar]
- 35.Itin PH. Oral hairy leukoplakia-10 years on. Dermatology. 1993;187:159–163. doi: 10.1159/000247233. [DOI] [PubMed] [Google Scholar]
- 36.Rosenthal D, LeBoit PE, Klumpp L, Berger TG. Human immunodeficiency virus-associated eosinophilic folliculitis. A unique dermatosis associated with advanced human immunodeficiency virus infection. Arch Dermatol. 1991;127:206–9. [PubMed] [Google Scholar]
- 37.Khorenian SD, Lebwohl M. New cutaneous manifestations of systemic disease. Am Fam Phys. 1995;51:625–30. [PubMed] [Google Scholar]
- 38.Schatz O, Bogner JR, Goebel FD. Kaposi's sarcoma: is the hunt for the culprit now over? J Mol Med. 1997;75(1):28–34. doi: 10.1007/s001090050083. [DOI] [PubMed] [Google Scholar]
- 39.Orfanos CE, Husak R, Wölfer U, Garbe C. Kaposi's sarcoma: a reevaluation. Recent Results Cancer Res. 1995;139:275–96. [PubMed] [Google Scholar]
- 40.Koehler JE, Tappero JW. Bacillary angiomatosis and bacillary peliosis in patients infected with human immunodeficiency virus. Clin Infect Dis. 1993;17:612–24. doi: 10.1093/clinids/17.4.612. [DOI] [PubMed] [Google Scholar]
- 41.Bacellar H, Muñoz A, Miller EN, et al. Temporal trends in the incidence of HIV-1-related neurologic diseases: multicenter AIDS cohort study, 1985–1992. Neurology. 1994;44:1892–1900. doi: 10.1212/wnl.44.10.1892. [DOI] [PubMed] [Google Scholar]
- 42.Mariuz P, Bosler EM, Luft BJ. Toxoplasmosis in individuals with AIDS. Infect Dis Clin North Am. 1994;8:365–81. [PubMed] [Google Scholar]
- 43.Powderly WG. Cryptococcal meningitis and AIDS. Clin Infect Dis. 1993;17:837–42. doi: 10.1093/clinids/17.5.837. [DOI] [PubMed] [Google Scholar]
- 44.Pertel P, Hirschtick R, Phair J, et al. Risk of developing cytomegalovirus retinitis in persons infected with the human immunodeficiency virus. J Acquir Immune Defic Syndr. 1992;5:1069–74. [PubMed] [Google Scholar]
- 45.Smith MA, Brennessel DJ. Cytomegalovirus. Infect Dis Clin North Am. 1994;8:427–38. [PubMed] [Google Scholar]
- 46.Von-Einsiedel RW, Tomiyasu U, Itabashi HH, Vinters HV. Progressive multifocal leukoencephalopathy in AIDS: a clinicopathologic study and review of the literature. J Neurol. 1993;240(7):391–406. doi: 10.1007/BF00867351. [DOI] [PubMed] [Google Scholar]
- 47.Mcarthur JC. Neurologic manifestations of AIDS. Medicine. 1987;6:407–35. doi: 10.1097/00005792-198711000-00001. [DOI] [PubMed] [Google Scholar]
- 48.Rubin DS, Rahal JJ. Mycobacterial avium complex. Infect Dis Clin North Am. 1994;8:413–26. [PubMed] [Google Scholar]