Abstract
OBJECTIVE
Delirium is frequent in elderly hospitalized patients. Many studies have examined its risk factors, but results have been quite variable. Thus, the goal of this study is to identify through systematic literature review the risk factors associated with the development of delirium in hospitalized geriatric patients.
MEASUREMENTS AND MAIN RESULTS
First, medline/current contentsdatabases were screened for relevant articles published from 1966 to December 1995, and from bibliographies of identified articles additional reports were selected. Second, the reports were screened by two different investigators and retained only if meeting the five following criteria: (1) original research in French or English; (2) prospective study; (3) patients over age 50; (4) minimum of one risk factor examined; (5) acceptable definition of delirium. Third, the methodology of each study was graded according to specific criteria for risk factor studies. Fourth, risk factors were identified and tabulated, unadjusted odds ratios (ORs) were computed, and where appropriate a combined OR with the Mantel-Haenszel estimator was calculated. Twenty-seven articles were retained meeting all of the above criteria. Among these studies, 11 were done on medical patients, 9 on surgical patients, 2 on medical and surgical patients, and 5 on psychiatric patients. In total 1,365 subjects with delirium were studied. Sixty-one different risk factors were examined, the five most common being dementia, medication, medical illness, age, and male gender. Mantel-Haenszel estimator was calculated for 10 risk factors, the most strongly associated being dementia (OR 5.2; 95% confidence interval [CI] 4.2, 6.3), medical illness (OR 3.8; 95% CI 2.2, 6.4), alcohol abuse (OR 3.3; 95% CI 1.9, 5.5), and depression (OR 1.9; 95% CI 1.3, 2.6). Methodologic weaknesses were present in many studies.
CONCLUSIONS
Despite methodologic limitations, certain risk factors for delirium seem to be consistent and could help identify high-risk patients. These risk factors include dementia, advanced age, and medical illness. Other risk factors appear to play a contributory role in the development of delirium in elderly hospitalized patients.
Keywords: delirium, risk factors, elderly
Delirium is commonly defined as a transient organic mental disorder characterized by acute onset, altered level of consciousness, fluctuating course, and disturbances in orientation, memory, attention, thought, and behavior.1–2 Etiologic factors for delirium are numerous and include systemic medical illness, metabolic disorders, toxic effects of medications, and a host of other illness and environmental stressors.1 It is common in both elderly medical and surgical patients 1, 2 and is associated with an increase in mortality, morbidity, rate of admission to long-term care institutions, and length of hospitalization.3, 4 Delirium is often not recognized,5–7 and intervention benefits to date have shown to be limited.8–10 Thus, prevention through identification of a high-risk group is indicated.
Many studies have identified different risk factors for delirium 1–11; predictive risk models have been developed for both surgical and medical patients.12, 13 Inconsistent results in the above studies, however, make it difficult to draw conclusions. For example, the presence of dementia was found to be a risk factor in most studies,2, 11–13 but other risk factors such as anticholinergic medications, laboratory abnormalities, and psychiatric disorders, commonly believed to increase the risk of delirium, have shown conflicting results.1, 11, 12 This may be due to varying methods for detection of delirium and identification of risk factors. Also, different risk factors may be particular to the surgical, medical, or psychiatric geriatric population. No study so far has specifically reviewed this literature. Thus, the goal of the present study is to identify the risk factors associated with the development of delirium in hospitalized surgical, medical, and psychiatric geriatric patients through a systematic selection of original research studies, assessment of their validity, and examination of their results
METHODS
Selection of Articles and Data Abstraction
The selection of articles involved three steps. First, medlinewas searched with the use of the key words “delirium,”“risk factors,” and “aged” for all relevant research articles published between January 1966 and December 1995. This was updated by the current contentsdatabase up to December 1995. Second, we identified additional references from the bibliographies of relevant articles. Finally, all the articles were independently screened by two different investigators to meet the following five inclusion criteria: (1) original research in French or English, (2) prospective study, (3) patients over age 50, (4) minimum of one risk factor identified, (5) accepted definition of delirium. Checklists of the inclusion criteria were used for discussion of the results of the screening process and to determine articles to be included in this review.
Each selected article was systematically reviewed by one author using a checklist to outline the following information: type of study, setting, service, type of cases (incident or prevalent), sample size, age range or mean, gender, place of living, number of case and control subjects, exclusion criteria, and criteria used for the definition of delirium.
Study Quality Assessment
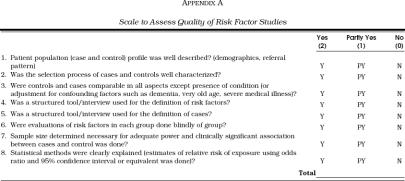
One limitation of systematic review is often the lack of a quality assessment of studies included in the review.14 Because the validity of the estimate of effect sizes depends on both the combinability and the methodologic quality of selected studies, quality assessment is of primary importance.15 Because a review of the literature did not yield a quality assessment scale for studies examining risk factors, we developed such a scale (Appendix A). This scale is derived from the work of Squires, Prendiville, and Macarthur.15–17 It controls for selection bias at entry and after entry, for assessment bias, and for statistical analysis. Each of its eight questions can be rated 2 (complete answer), 1 (partial answer), or 0 (absent) for a maximum score of 16. Each individual selected article was rated with this scale by three different authors. The intraclass correlation coefficient was calculated to assess the interrater reliability. For each study, the average score of the three raters was used as the quality score of the study.
Risk Factor Analysis
All selected articles were screened with a checklist to identify the risk factors studied. Because the statistical analysis varied between studies, the reviewers relied on the reported statistics (odds ratio [OR], relative risk, p values, or others). Risk factors were reported to have a positive correlation or no correlation to the development of delirium and were then tabulated. Comparison of these results provided the qualitative analysis.
A quantitative analysis was done for each risk factor when original data (number of case and control subjects exposed to the risk factor) could be obtained from two or more studies. Unadjusted ORs were calculated from the original data to standardize the results (adjusted OR was often present, but could not be used because it had been adjusted for different variables in different studies). A combined Mantel-Haenszel OR was then calculated.18
RESULTS
Articles Selected and Data
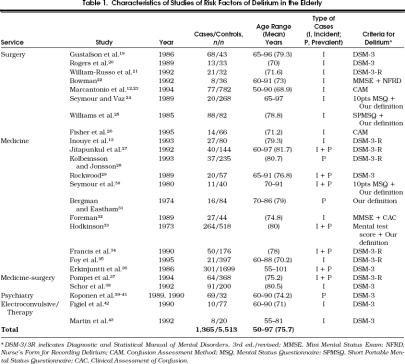
We obtained 101 studies from the online and cross-reference search. Only 27 met all the inclusion criteria (Table 1) Nine were done on surgical patients,12, 19–2611 on medical patients,13, 27–362 on a mixed population of medical and surgical patients,37, 38 and 5 on psychiatric patients.39–43 Two of these latter studies looked at patients receiving electroconvulsive therapy.42, 43
Table 1.
Characteristics of Studies of Risk Factors of Delirium in the Elderly
A total of 1,365 cases of delirium were studied with 5,513 control subjects (Table 1). The subjects in Marcantonio et al.12, 23 and Koponen et al.39–41 were counted only once because the same population of cases was analyzed looking at different risk factors. The number of delirium cases per study varied from 8 to 301 with a mean of 59. Age range was 50 to 97 with a mean of 75.7 years. Fifteen studies looked at incident cases, 5 at prevalent cases, and 7 at both. Most studies used the Diagnostic and Statistical Manual of Mental Disorders, third edition or third edition revised, for diagnostic criteria of delirium. Others used a combination of a structured interview and their own definition.
Study Quality
The intraclass correlation coefficient was 0.70 (95% confidence interval [CI] 0.51, 0.83). Most frequent discrepancies between authors were for criteria 2 and 3 (selection process and adjustment for confounding factors), perhaps from lack of adequate specificity for these questions. The mean quality score of the 27 studies was 9.3 with a minimum of 5 and a maximum of 13. Ten studies scored in the 5- to 8-range, 14 in the 9- to 12-range and 3 in the 13- to 16-range.
Risk Factor Analysis
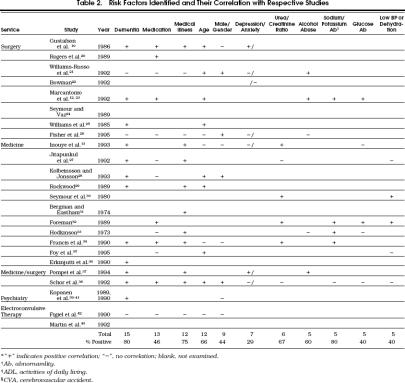
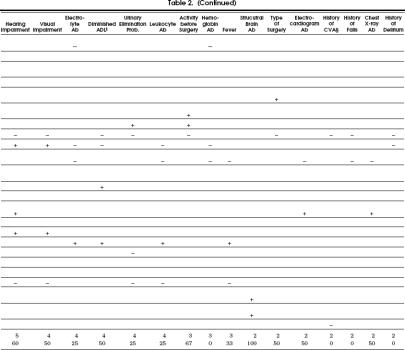
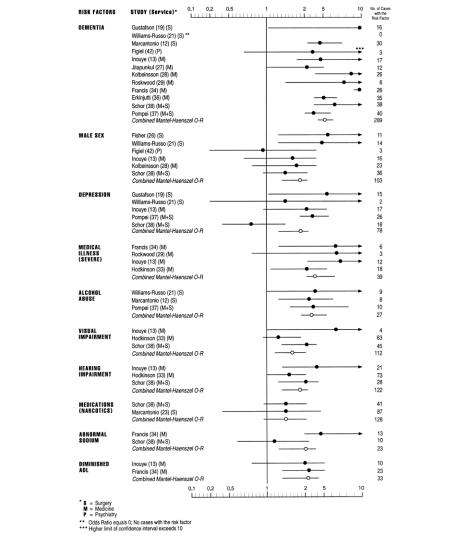
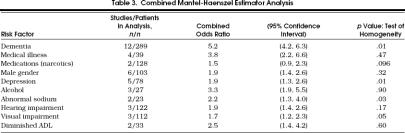
Sixty-one different risk factors were identified. Twenty-seven were studied in two or more articles as illustrated in Table 2). Thirty-four other risk factors were studied in only one article and will be mentioned in the text. The unadjusted OR for each study and the combined Mantel-Haenszel unadjusted OR 18 were calculated on 10 risk factors (Fig. 1, Table 3 Unadjusted here refers to an OR not corrected for other possible confounding or risk factors. Weighted averages of the unadjusted log ORs were also calculated using fixed and random effects models with (1) the inverse of the variance of the log OR as weight and (2) the quality score multiplied by the inverse of the variance as a weight to adjust for the effect of the study quality score on the overall combined estimate.18 For each risk factor, a test of homogeneity of the log OR across studies was also performed (Table 3).18 The results of these different combining methods were very similar to the combined Mantel-Haenszel OR and for this are not reported here. All the statistical analyses were done with the SAS software for Windows version 6.12. The following descriptions combine the results of both the qualitative and quantitative analyses.
Table 2.
Risk Factors Identified and Their Correlation with Respective Studies
Figure 1.
Individual and combined odds ratio analysis.
Table 3.
Combined Mantel-Haenszel Estimator Analysis
Demographics.
Advanced age was significantly associated with the development of delirium. Male gender was found to be a risk factor in only four of nine studies, but the combined OR of 1.9 was statistically significant (95% CI 1.4, 2.6). Schor et al.38 and Bergmann and Eastham,31 respectively, found living in an institution and having little contract with relatives to be risk factors. Race,34 marital status,34 education,26 and first language other than English 26 had no association.
Mental Status.
Dementia was the most studied risk factor and the most strongly associated with delirium. Twelve of 15 studies showed a positive correlation. The cumulative OR was 5.2 (95% CI 4.2, 6.3). Clock-drawing abnormality, to a certain extent a reflection of cognitive impairment, also was shown in one study to predict development of delirium.26 History of nocturnal confusion,26 history of delirium,13, 26 and a preoperative measure of anxiety 22 showed no association. Depression was found to have an association in only two of six studies, but the combined OR of 1.9 was statistically significant (95% CI 1.3, 2.6).
Medical Illness and Medications.
Medical illness was the second most strongly associated risk factor with delirium development. Nine of 12 studies found an association. The statistical analysis, limited to four articles looking at severe illness, produced a combined OR of 3.8 (95% CI 2.2, 6.6). Medication use was the second most studied risk factor. Less than 50% (6 of 13 studies) found an association. Diverse measurement of this variable between studies limited the quantitative analysis to narcotics exposure, which produced a nonsignificant cumulative OR of 1.5 (95% CI 0.9, 2.3).
Physical Status.
Fever and low blood pressure showed some association, whereas abnormal heart rate,27 high blood pressure,38 dyspnea,27 and pain 38 did not. One study identified physical findings (enlarged liver and palpable bladder) as risk factors.31 Both hearing and visual impairment were moderate risk factors and produced combined ORs of 1.9 (95% CI 1.4, 2.6) and 1.7 (95% CI 1.2, 2.3), respectively. Diminished activities of daily living (combined OR 2.5, 95% CI 1.4, 4.2) and decreased activity before surgery increased risk of delirium, but a history of falls did not. Most studies found no association between urinary or fecal incontinence and delirium.26
Laboratory Findings.
Of the 12 biochemical parameters studied, blood urea nitrogen/creatinine ratio and sodium or potassium abnormalities were significant risk factors most often. The sodium abnormality combined OR was 2.2 (95% CI 1.3, 4.0). Foy et al.35 and Koponen et al.41 provided isolated results of association for hypoxia and abnormal cerebrospinal fluid, respectively. Other electrolyte derangements and abnormal glucose or leukocytes demonstrated a weak association, whereas abnormal hemoglobin, albumin,27 calcium,13 liver function tests,13 or presence of leukocytes in the urine 27 did not. Bergmann and Eastham found both abnormal electrocardiogram and chest x-ray findings to be risk factors,31 but this finding was not reproduced by Jitapunkul et al.27 Two studies of psychiatric patients noted structural brain abnormalities as risk factors 39, 42; however, history of cerebrovascular accident did not show such an association.
Surgery and Anaesthesia.
Marcantonio et al. demonstrated noncardiac thoracic surgery and aortic aneurysm surgery to be risk factors.12 Fisher et al. found no difference between hip and knee surgery.26 Other surgical risks were unplanned surgery 22 and low mobility after surgery.25 Not shown to have an influence on the development of delirium were surgical technique,19 number of previous surgeries,26 time between surgeries,19 type of anesthesia,19 and surgery duration.19 Furthermore, Schor et al. did not find surgery in itself a risk factor for their mixed medical-surgical population.37
Other Risk Factors.
Alcohol abuse was identified as having a strong association, being positive in three of five studies and yielding a cumulative OR of 3.3 (95% CI 1.9, 5.5). Presence of a fracture at admission,38 increased number of admissions in the previous 2 years,27 and urgent admission 34 were all found to be risk factors. Neither type (unilateral vs bilateral)43 nor number 42 of electroconvulsive treatments was significant. Finally, presence of more orienting objects was surprisingly associated with delirium development.32
DISCUSSION
This review has limitations at several levels. First, a search involving different databases and the use of different key words might have resulted in a different group of articles, especially since delirium has often changed name over time.44 Second, we tried to control for publication bias (i.e., the tendency for reports with positive findings to be published) by obtaining unpublished data; we had limited success with this. Nevertheless, we believe that most large studies represent enough investment to warrant some effort to publish, independent of results, and that most valid work is published.45 Finally, more strict inclusion criteria, such as a minimum number of cases per study and specific definition of delirium, could have been used.
The generalizability of results as reported in Table 2 is limited by diverse methods for risk factor measurement, heterogeneous statistical analyses, and distinct patient populations found between studies. This also limited our quantitative analysis. For example, measurement of medication use varied from type to number or dose of medication. Thus, of 13 articles looking at this risk factor, only 2 presented data we could cumulate for a combined OR. Similarly measurement of medical illness varied from type to number or severity of medical illness. Thus, of 12 studies looking at this risk factor, only the 4 looking at severity of medical illness could be combined. Three of these four studies used the Charlson scale.46 Dementia (structured instrument used in 11 of 12 studies combined), depression (Geriatric Depression Scale 47 used in 3 of 5 studies), abnormal sodium (set values in 2 of 2 studies), and activities of daily living (Katz scale 48 in 2 of 2 studies) were the best characterized risk factors in the quantitative analysis. In only one of three articles was a structured instrument present for analysis of alcohol abuse and visual or hearing impairment. Lack of a common definition for old age and measurement for blood urea nitrogen/creatinine ratio prevented quantitative analysis. Finally, authors of these studies may have preferably reported statistically significant risk factors, omitting to report risk factors with no significant associations. This raises the concern that specific unpublished results (even though the study is published) may be different from the published results for a given risk factor.
Oxman et al.49 and Macarthur 15 stressed the importance of evaluating the quality of studies involved in reviews. As described above, we developed a scale to examine this (Appendix A). Agreement between the authors was good, but this scale could have taken into account the study design (e.g., prospective cohort vs case-control) and the type of cases studied (incident vs prevalent). Overall, study quality was moderate (mean = 9.3/16). Only three studies scored above 13, and more than one third (37%) scored less than 9. Most frequent weaknesses were inadequate sample size necessary for significant association, lack of blind evaluation of risk factors, poor statistical analysis, and poor control of confounding factors. In any case, the calculation of the combined OR using the study quality score as a weighting factor did not change the results.
Despite the above methodologic weaknesses, some variables are convincing risk factors for delirium: for example, dementia and medical illness. The negative results of Figiel et al.,42 Fisher and Flowerdew,26 and Williams-Russo et al.21 could be explained by the healthier and less-demented population they studied. Other probable risk factors include advanced age, abnormal blood urea nitrogen/creatinine ratio, abnormal sodium or potassium level, alcohol abuse, sensory impairment, and medications. The latter gains importance, particularly in the surgical group, if the three above-mentioned studies are excluded. Unfortunately, lack of systematized data for this risk factor precludes further analysis of hypothesized contributory drug effect, such as anticholinergic effect.50 Other possible risk factors include male gender, depression, and low levels of activity. No conclusions can be drawn for a large number of risk factors studied.
Analysis of risk factors by service yielded no marked differences. However, certain variables (medical illness, electrolyte abnormalities, sensory impairment) remain much less studied in surgical patients and require further examination. Because studies of prevalent cases could include variables that did not precede onset of delirium, we also analyzed the data by type of cases (incident or prevalent). There was no difference in either the qualitative or quantitative analysis. Levkoff et al., however, analyzed case subjects by their residency status (i.e., living in the community or in an institution).2 They found no effect for advanced age, cognitive impairment, or illness severity in the institutionalized group, whereas analysis of the group as a whole had shown an association for these variables.38
The following recommendations should be considered in new studies of risk factors for delirium: first, the eight criteria in Appendix A should be included in the study methodology; second, only incident cases, in which the risk factors can clearly be shown to have preceded the onset of delirium, should be included; third, risk factors should be examined by service (surgical, medical, or psychiatric).
To conclude, this review has attempted to identify risk factors for development of delirium in the elderly to better identify high-risk patients. Even with the methodologic limitations mentioned above, certain risk factors seem consistent. Some are fixed (age, gender, and dementia), but others are potentially modifiable (medical illness, biochemical abnormalities, and medication use) and could permit a clinical intervention to prevent development of this disorder. Certain risk factors (e.g., medication use) will require further study to better define their role. Clearly more research is needed.
Acknowledgments
The authors thank Brigitte Beaudet, Audiovisual Department, and Dr. Jane McCusker, Department of Clinical Epidemiology, for their assistance in completing this article.
Appendix A
Scale to Assess Quality of Risk Factor Studies
References
- 1.Francis J. Delirium in older patients. J Am Geriatr Soc. 1992;40:829–38. doi: 10.1111/j.1532-5415.1992.tb01859.x. [DOI] [PubMed] [Google Scholar]
- 2.Levkoff SE, Evans DA, Liptzin B, et al. Delirium: the occurrence and persistence of symptoms among elderly hospitalized patients. Arch Intern Med. 1992;152:334–40. doi: 10.1001/archinte.152.2.334. [DOI] [PubMed] [Google Scholar]
- 3.Cole MG, Primeau FJ. Prognosis of delirium in elderly hospitalized patients. Can Med Assoc J. 1993;149:41–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Thomas RI, Cameron DJ, Fahs MC. A prospective study of delirium and prolonged hospital stay. Arch Gen Psychiatry. 1998;45:937–40. doi: 10.1001/archpsyc.1988.01800340065009. [DOI] [PubMed] [Google Scholar]
- 5.Lewis LM, Miller DK, Morley JE, Nork MJ, Lasater LC. Unrecognized delirium in ED geriatric patients. Am J Emerg Med. 1995;13:142–5. doi: 10.1016/0735-6757(95)90080-2. [DOI] [PubMed] [Google Scholar]
- 6.Rockwood K, Cosway S, Stolee P, et al. Increasing the recognition of delirium in elderly patients. J Am Geriatr Soc. 1994;42:252–6. doi: 10.1111/j.1532-5415.1994.tb01747.x. [DOI] [PubMed] [Google Scholar]
- 7.Gustafson Y, Brannstrom B, Norbeg A, Butch G, Winblab B. Underdiagnosis and poor documentation of acute confusional states in elderly hip fracture patients. J Am Geriatr Soc. 1991;39:760–5. doi: 10.1111/j.1532-5415.1991.tb02697.x. [DOI] [PubMed] [Google Scholar]
- 8.Cole MG, Primeau FJ, Bailey RF, et al. Systematic intervention for elderly inpatients with delirium: a randomized trial. Can Med Assoc J. 1994;151(7):965–70. [PMC free article] [PubMed] [Google Scholar]
- 9.Williams MA, Campbell EB, Raynar WJ, et al. Reducing acute confusional states in elderly patients with hip fractures. Res Nurs Health. 1985;8:329–37. doi: 10.1002/nur.4770080405. [DOI] [PubMed] [Google Scholar]
- 10.Wanich CK, Sullivan-Marx FM, Gottlieb G, et al. Functional status outcomes of a nursing intervention in hospitalized elderly. Image. 1992;24:201–7. doi: 10.1111/j.1547-5069.1992.tb00719.x. [DOI] [PubMed] [Google Scholar]
- 11.Dyer CB, Ashton CM, Teasdale TA. Postoperative delirium, a review of 80 primary data-collection studies. Arch Intern Med. 1995;155:461–5. doi: 10.1001/archinte.155.5.461. [DOI] [PubMed] [Google Scholar]
- 12.Marcantonio ER, Goldman L, Mangione CM, et al. A clinical prediction rule for delirium after elective noncardiac surgery. JAMA. 1994;271:134–9. [PubMed] [Google Scholar]
- 13.Inouye SK, Viscoli CM, Horwitz RI, Hurst LD, Tinetti ME. A predictive model for delirium in hospitalized elderly medical patients based on admission characteristics. Ann Intern Med. 1993;119:474–81. doi: 10.7326/0003-4819-119-6-199309150-00005. [DOI] [PubMed] [Google Scholar]
- 14.Eysenck HJ. Meta-analysis and its problems. BMJ. 1994;309:789–92. doi: 10.1136/bmj.309.6957.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Macarthur C, Foran PJ, Boilar JC., III Qualitative assessment of studies included in a meta-analysis: DES and the risk of pregnancy loss. J Clin Epidmiol. 1995;48(6):739–47. doi: 10.1016/0895-4356(94)00190-2. [DOI] [PubMed] [Google Scholar]
- 16.Squires BP, Elmslie TJ. Reports of case-control studies: what editors want from authors and peer reviewers. Can Med Assoc J. 1989;141:17–9. [PMC free article] [PubMed] [Google Scholar]
- 17.Prendiville W, Elbourne D, Chalmers I. The effects of routine oxytocic administration in the management of the third stage of labour: an overview of the evidence from controlled trials. Br J Obstet Gynaecol. 1988;95:3–16. doi: 10.1111/j.1471-0528.1988.tb06475.x. [DOI] [PubMed] [Google Scholar]
- 18.Cooper H, Hedges L. The Handbook of Research Synthesis. New York, NY: Russell Sage Foundation; 1994. Combining estimate of effect size. In. [Google Scholar]
- 19.Gustafson Y, Berggen D, Brannstrom B, et al. Acute confusional states in elderly patients treated for femoral fracture. J Am Geriatr Soc. 1988;36:525–30. doi: 10.1111/j.1532-5415.1988.tb04023.x. [DOI] [PubMed] [Google Scholar]
- 20.Rogers MP, Liang MH, Daltroy LH, et al. Delirium after elective orthopedic surgery: risk factors and natural history. Int J Psychiatr Med. 1989;19(2):109–21. doi: 10.2190/2q3v-hyt4-nn49-bpr4. [DOI] [PubMed] [Google Scholar]
- 21.Williams-Russo P, Urquhart BL, Sharrock NE, Charlson ME. Post-operative delirium: predictors and prognosis in elderly orthopedic patients. J Am Geriatr Soc. 1992;40:759–67. doi: 10.1111/j.1532-5415.1992.tb01846.x. [DOI] [PubMed] [Google Scholar]
- 22.Bowman AM. The relationship of anxiety to development of postoperative delirium. J Gerontol Nurs. 1992;18(1):24–30. doi: 10.3928/0098-9134-19920101-07. [DOI] [PubMed] [Google Scholar]
- 23.Marcantonio ER, Juarez G, Goldman L, et al. The relationship of postoperative delirium with psychoactive medications. JAMA. 1994;272:1518–22. [PubMed] [Google Scholar]
- 24.Seymour DG, Vaz FC. A prospective study of elderly general surgical patients, II: post-operative complications. Age Ageing. 1989;18:316–26. doi: 10.1093/ageing/18.5.316. [DOI] [PubMed] [Google Scholar]
- 25.Williams M, Campbell EB, Raynor WJ, Musholt MA, Mlynarczyk SM, Crane LF. Predictors of acute confusional states in hospitalized elderly patients. Res Nurs Health. 1985;8:329–37. doi: 10.1002/nur.4770080107. [DOI] [PubMed] [Google Scholar]
- 26.Fisher BW, Flowerdew G. A simple model for predicting postoperative delirium in older patients undergoing elective orthopedic surgery. J Am Geriatr Soc. 1995;43:175–8. doi: 10.1111/j.1532-5415.1995.tb06385.x. [DOI] [PubMed] [Google Scholar]
- 27.Jitapunkul S, Pilloy I, Ebrahim S. Delirium in newly admitted elderly patients: a prospective study. Q J Med. 1992;83:307–14. [PubMed] [Google Scholar]
- 28.Kolbeinsson H, Jonsson A. Delirium and dementia in acute medical admissions of elderly patients in Iceland. Acta Psychiatr Scand. 1993;83:123–7. doi: 10.1111/j.1600-0447.1993.tb03342.x. [DOI] [PubMed] [Google Scholar]
- 29.Rockwood K. Acute confusion in elderly medical patients. J Am Geriatr Soc. 1989;37:150–4. doi: 10.1111/j.1532-5415.1989.tb05874.x. [DOI] [PubMed] [Google Scholar]
- 30.Seymour DG, Henschke RD, Cape T, Campbell AJ. Acute confusional states and dementia in the elderly: the role of dehydration/volume depletion, physical illness and age. Age Ageing. 1980;9:137–46. doi: 10.1093/ageing/9.3.137. [DOI] [PubMed] [Google Scholar]
- 31.Bergmann K, Eastham EJ. Psychogeriatric ascertainment and assessment for treatment in an acute medical ward setting. Age Ageing. 1974;3:174–88. doi: 10.1093/ageing/3.3.174. [DOI] [PubMed] [Google Scholar]
- 32.Foreman MD. Confusion in the hospitalized elderly: incidence, onset and associated factors. Res Nurs Health. 1989;12:21–9. doi: 10.1002/nur.4770120105. [DOI] [PubMed] [Google Scholar]
- 33.Hodkinson HM. Mental impairment in the elderly. J R Coll Physicians Lond. 1973;7:305–17. [PMC free article] [PubMed] [Google Scholar]
- 34.Francis J, Martin D, Kapoor WN. Prospective study of delirium in hospitalized elderly. JAMA. 1990;263:1097–1101. [PubMed] [Google Scholar]
- 35.Foy A, O'Connell D, Henry D, Kelly J, Cocking S, Halliday J. Benzodiazepine use as a cause of cognitive impairment in elderly hospital inpatients. J Gerontol Med Sci. 1995;50A:M99–106. doi: 10.1093/gerona/50a.2.m99. [DOI] [PubMed] [Google Scholar]
- 36.Erkinjuntti T, Wirstrom J, Palo J, Autio L. Dementia among medical inpatients: evaluation of 2000 consecutive admissions. Arch Intern Med. 1986;146:1923–6. [PubMed] [Google Scholar]
- 37.Pompei P, Foreman M, Rudberg MA, Inouye SK, Braund V, Cassel CK. Delirium in hospitalized older persons: outcomes and predictors. J Am Geriatr Soc. 1994;42:809–15. doi: 10.1111/j.1532-5415.1994.tb06551.x. [DOI] [PubMed] [Google Scholar]
- 38.Schor J, Levkoff SE, Lipsitz LA, et al. Risk factors for delirium in hospitalized elderly. JAMA. 1992;267:827–31. [PubMed] [Google Scholar]
- 39.Koponen H, Hurri L, Stenback U, Mattila E, Soininen H, Riekkinen PJ. Computed tomography findings in delirium. J Nerv Ment Dis. 1989;177:226–31. doi: 10.1097/00005053-198904000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Koponen H, Stenback V, Mattila E, Soininen H, Reinikainen K, Riekkinen PJ. Delirium among elderly persons admitted to a psychiatric hospital: clinical course during the acute stage and one year follow-up. Acta Psychiatr Scand. 1989;79:579–85. doi: 10.1111/j.1600-0447.1989.tb10306.x. [DOI] [PubMed] [Google Scholar]
- 41.Koponen H, Riekkinen PJ. A longitudinal study of cerebrospinal fluid beta-endorphin-like, immunoreactivty in delirum: changes at the acute stage and at one year follow-up. Acta Psychiatr Scand. 1990;82:323–6. doi: 10.1111/j.1600-0447.1990.tb01394.x. [DOI] [PubMed] [Google Scholar]
- 42.Figiel GS, Coffey CE, Djang WT, Doraiswamy PM. Brain magnetic resonance imaging findings in ECT-induced delirium. J Neuropsychiatry Clin Neurosci. 1990;2:53–8. doi: 10.1176/jnp.2.1.53. [DOI] [PubMed] [Google Scholar]
- 43.Martin M, Figiel GS, Mattingly G, Zorumski CF, Jarvis MR. ECT-induced interictal delirium in patients with a history of a CVA. J Geriatr Psychiatry Neurol. 1992;5:149–55. doi: 10.1177/002383099200500304. [DOI] [PubMed] [Google Scholar]
- 44.Lipowski ZJ. Delirium in the elderly patient. N Engl J Med. 1989;320:578–81. doi: 10.1056/NEJM198903023200907. [DOI] [PubMed] [Google Scholar]
- 45.Angell M. Negative studies. N Engl J Med. 1989;321:464–6. doi: 10.1056/NEJM198908173210708. [DOI] [PubMed] [Google Scholar]
- 46.Charlson ME, Sax FL, MacKenzie R, et al. Assessing illness severity: does clinical judgment work? J Chronic Dis. 1986;39:439–52. doi: 10.1016/0021-9681(86)90111-6. [DOI] [PubMed] [Google Scholar]
- 47.Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1983;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 48.Katz S, Ford AG, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL, a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 49.Oxman AD, Cook DJ, Guyatt GH. User's guide to the medical literature, VI: how to use an overview. JAMA. 1994;272:1367–71. doi: 10.1001/jama.272.17.1367. [DOI] [PubMed] [Google Scholar]
- 50.Mach JR, Dysken MW, Kuskowski M, et al. Serum anticholinergic activity in hospitalized older persons with delirium: a preliminary study. J Am Geriatr Soc. 1995;43:491–5. doi: 10.1111/j.1532-5415.1995.tb06094.x. [DOI] [PubMed] [Google Scholar]