Abstract
OBJECTIVE
Little is known about the significance of patient-perceived overmedication. We sought to determine its prevalence and relation to medication compliance, adverse drug reactions, health-related quality of life (HRQOL), and burden of illness.
DESIGN
Analysis of self-reported questionnaire data.
PATIENTS/PARTICIPANT
There were 1,648 participants in a longitudinal study of male veterans.
INTERVENTION
Participants listed each of their medications with indication, missed doses, adverse reactions, and whether their amount of medication was “too much, the right amount, or too little.” The survey included questions about medication adherence, “problems with medications,” common symptoms, and screening questions for a number of chronic conditions. We assessed HRQOL with the Multiple Outcomes Study 36-Item Short Form Health Study (SF-36).
MEASUREMENTS AND MAIN RESULTS
Of the 1,256 respondents, 1,007 (80%) had taken medication within 4 weeks. Forty (4%) thought they were taking too much. They reported a 1.6-fold increase in prescription medications, a 5-8 fold increase in adverse effects, a 1.5-2 fold decrease in compliance, an increase in each of seven measured symptoms, and a decrease in six of eight SF-36 domains (p < .05 for all comparisons), the exceptions being the mental health and role-emotional scales. There was also a slight increase in the report of any chronic illness (95% vs 86%, p >.05).
CONCLUSIONS
Patient perception of overmedication correlates with self-report of decreased compliance, adverse drug reactions, decreased HRQOL, and an increase in symptomatology that is compatible with unrecognized side effects of medication. Such patients warrant careful evaluation.
Keywords: patient attitudes, drug therapy, questionnaires, patient compliance, quality of life
Prescription of medicine is almost certainly the most widespread of medical interventions and lies at the heart of clinical practice. Not surprisingly, its risks and benefits are much studied, as are relevant patient behaviors such as compliance with medication regimens.1–3 Patients' attitudes about their medicines are less well explored, however, and we have found no studies that examine the extent to which patients feel they are overmedicated. This is particularly surprising given the frequency with which practicing physicians encounter patients who would prefer fewer medications or who are resistant to taking more.
Patient perception of overmedication might be important in a number of ways. First, patients may be correct in their assumption. Second, patients who feel that they are taking too many medications may be less adherent to their medical regimens. Third, their attitude about the amount of their medication might reflect the presence of adverse drug reactions, including symptoms not recognized as being related to medication by either the physician or the patient. Finally, it is possible that patient perception of overmedication is a manifestation of psychoneurosis and a marker for more general difficulties in the care of such patients.
We hypothesized that patient perception of overmedication would correlate with medication problems. To explore this possibility, we used data from a large survey of older men to examine how patient perception of overmedication relates to self-reported measures of compliance and to perceived adverse drug reactions. We also characterized such patients in terms of their health-related quality of life (HRQOL), illness burden, and medication use.
METHODS
Study Sample
The Normative Aging Study has followed a cohort of 2,280 healthy male veterans since 1963.4 The participants were originally selected for good health, based on laboratory tests and self-report. Those in the current study continue to reside in the community and few receive care from the VA system. Questionnaires were mailed to the 1,648 surviving participants of the Normative Aging Study in 1992, when their median age was 68 years. Those who did not respond were sent a reminder postcard at 4 weeks. Those who still did not respond were mailed a second copy of the questionnaire after another 4 weeks. Of the 1,648 participants, 1,256 (76%) completed and returned the questionnaire.
Fifty-three percent of respondents were retired, compared with 46% of nonrespondents (p= .05), and their average age was 1.4 years older (p= .002). They did not differ significantly in the proportion that reported a physical problem or condition (47% vs 46%), or worsening health (15% vs 17%), or in rating their health on a 5-point scale (4.2 vs 4.0, with 5 being excellent).
Medication Use
We asked participants to report the total number of different medications used (prescription and over-the-counter) and their perception of the amount of medication (“too much, the right amount, or too little”). We then asked participants to list all of their medications individually (prescription and over-the-counter) using information from containers if possible. For each entry we requested additional information about the indication and dosage regimen, number of missed doses in the last week, and perception of any adverse reactions. The latter two items were used as measures of compliance and adverse drug reactions, respectively. They were supplemented by four questions about medication adherence,5 as well as a single question about their perception of any “problems with medications.” We asked respondents to report prescription medicines separately from nonprescription medicines. To identify the latter we asked, “How many different non-prescription (over-the-counter) medicines or supple-ments did you take? (include medicines like aspirin, Tylenol, Advil).”
Health Status
We assessed HRQOL using the 36-Item Short Form Health Study (SF-36),6, 7 a well-validated 36-item questionnaire. It assesses eight domains of functional status and well-being: physical function, limitations of role due to physical problems, bodily pain, vitality, general health perceptions, social function, limitations of role due to emotional problems, and mental health. Each of these is scored from 0 to 100, with 100 being the best health. Participants also completed a brief medical history, including previously validated screening measures for a number of chronic conditions, as well as various signs and symptoms of illness and its treatment.8
Data Analysis
The data were analyzed using PC SAS (SAS Institute, Cary, NC). We used Mantel-Haenszel χ2 tests to evaluate differences in proportions, and two-tailed Student's t tests were used to evaluate differences in means. No corrections were made for multiple comparisons.
RESULTS
Demographic Data
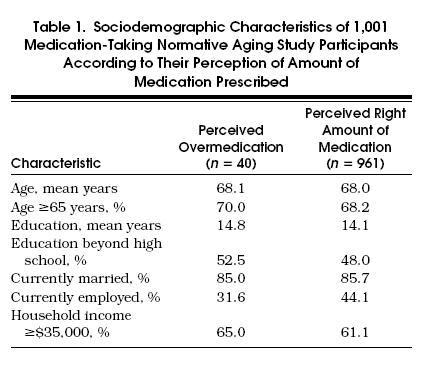
Of the 1,256 respondents, 1,007 (80%) had taken medication in the past 4 weeks. Of these subjects, 40 (4%) felt that they were taking too many medications, 961 (95%) felt that they were taking the right amount, and 6 (1%) felt that they were taking too little. The latter are not considered further. Subjects with perceived overmedication did not differ significantly from those who felt that they were taking the right amount in terms of age, education, income, marital status, or employment (Table 1)
Table 1.
Sociodemographic Characteristics of 1,001 Medication-Taking Normative Aging Study Participants According to Their Perception of Amount of Medication Prescribed
Medication Number, Compliance, and Adverse Drug Reactions
Table 2 shows the reported numbers of medications used, along with the measures of compliance and adverse drug reactions in patients who felt they were taking too many medications and those who felt they were taking the right number. The former reported taking 4.1 prescription medications, versus 2.5 for the others (p < .05). In contrast, there was no significant difference in the mean number of nonprescription medications (0.9 vs 0.8).
Table 2.
Reports of Medication Use, Compliance, and Adverse Drug Reactions According to Perception of Overmedication
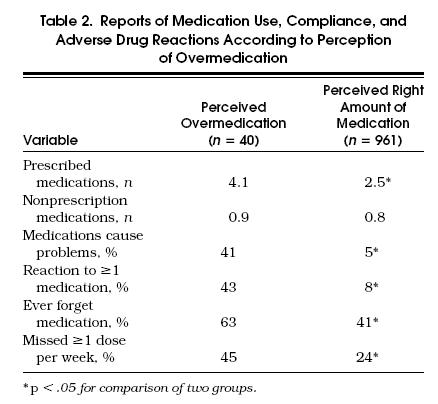
Subjects who said they take too many medications reported more medication problems and worse compliance than patients who said they take the right number of medications. Adverse effects of specific medications were reported 5 to 8 times more often and decreased compliance from 1.5 to 2 times more often (p < .05 for all comparisons). For both groups there was good agreement between general questions about whether medication causes problems and whether one or more specific medications were listed as causing a problem. Likewise, there was good agreement between general and specific questions about medication compliance.
Burden of Illness, Symptoms, and Health-Related Quality of Life
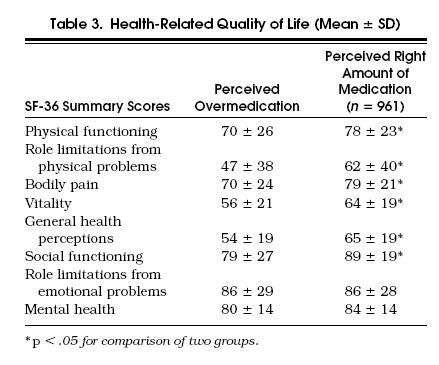
Ninety-five percent of subjects who said that they take too much medication reported having any chronic illness compared with 86% of those reporting taking the right amount, a difference that was not statistically significant (p>.05). We also asked about the presence of nausea, indigestion, headache, blurred vision, dizziness, dry mouth, and itchy skin. Each of these occurred more often in patients with perceived overmedication (p < .05 for each comparison). The health status of patients with self-perceived overmedication was significantly worse for six of the eight SF-36 domains (Table 3) The exceptions were the role-emotional and mental health scales, which were almost identical between the two groups.
Table 3.
Health-Related Quality of Life (Mean ±SD)
DISCUSSION
Four percent of our sample of veterans participating in the Normative Aging Study thought they were taking too many medications. To our knowledge, this is the only report of patient-perceived overmedication in any population. It is surprising that more is not known about perceptions of a treatment modality that is so pervasive. Patients' opinions about the appropriateness of their treatment are important in their own right, but are also likely to influence many aspects of care, medication compliance being but one possibility. Other patient groups should be studied to expand knowledge in this area.
Patients' perception of overmedication appears to reflect reality. On average, these individuals do report taking more medication. This is probably not due to overreporting, as the increase was restricted to prescription drugs and did not extend to those that were over-the-counter. The most likely explanation is their increased number of comorbid illnesses, though this difference did not reach statistical significance. It is also possible that perception of overmedication has a psychological origin, but this is not supported by the mental health and role-emotional SF-36 scores of these patients, which were virtually the same as those of the others.
As we expected, the perception of overmedication had a strong association with decreased medication compliance and increased drug reactions. The consistency of answers between the general and specific medication questions supports this conclusion. In addition, it is consonant with the results of other studies, which show that patients who take more medications have decreased compliance and increased drug reactions.9–13 However, it is also true that adverse medication effects, when they do occur, may contribute to patients' perceptions that they are taking too many medications.
Perception of overmedication also showed a strong association with decreased HRQOL in all domains other than mental health and limitations of role due to emotional problems. There was also a parallel increase in symptom reports, which spanned all of those about which we asked. These findings may be the exclusive result of an increased prevalence of physical illness. However, many of the symptoms that were reported are of a type commonly caused by medications, and therefore they could also reflect medication side effects. There is support for this possibility in these patients' reports of an increase of 5- to 8-fold in adverse drug reactions. This suggests that their impaired HRQOL may be partially remediable by alteration of their medication regimens.
Our study relies on patient self-report and demonstrates many of the advantages of this method. We have been able to gather a great deal of information that would have been difficult to obtain by other means. This, in turn, has enabled us to examine relations among patient attitudes, medication problems, mental health, physical illness, and HRQOL. This breadth of scope would have been hard to achieve with any other approach.
Though patient self-report can be a powerful tool, it also has limitations. What patients say about their own attitudes and quality of life usually can be accepted as definitive, but other types of patient reports may be less reliable. Patients probably underreport problems with compliance and overestimate adverse drug reactions.9–13 Although we are satisfied that both are altered in patients who think they are taking too many medications, the magnitude of the difference that we have found must be considered an estimate. In addition, lack of a reference standard for compliance and adverse drug reactions prevents us from estimating the sensitivity and specificity of perceived overmedication as a way to screen for such problems.
In summary, patients' perceptions of overmedication bear a strong relation to their reports of decreased medication compliance and increased drug reactions. This perception is more likely to reflect reality than to result from psychological factors. Such patients report a higher average number of medications and decreased HRQOL, probably resulting from a greater burden of chronic illness. However, there is also an increase in symptomatology that is compatible with unrecognized side effects of medication. Patients who perceive themselves to be overmedicated warrant careful evaluation.
Acknowledgments
The Normative Aging Study is supported by the Health Services Research and Development Service of the U.S. Department of Veterans Affairs.
References
- 1.Caranasos GJ, Stewart RB, Cluff LE. Drug induced illness leading to hospitalization. JAMA. 1974;228:713–7. [PubMed] [Google Scholar]
- 2.Ives TJ, Bentz EJ, Gwyther RE. Drug-related admissions to a family medicine inpatient service. Arch Intern Med. 1987;147:1117–20. [PubMed] [Google Scholar]
- 3.Blackwell B. Patient compliance. N Engl J Med. 1973;289:249–52. doi: 10.1056/NEJM197308022890506. [DOI] [PubMed] [Google Scholar]
- 4.Bossé R, Spiro A., III . The normative aging study. In: Maddox G, editor. Encyclopedia of Aging. 2nd ed. New York, NY: Springer Press; 1996. In. [Google Scholar]
- 5.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 6.McHorney CA, Ware JE, Razcek AE. The Medical Outcomes Study 36-Item Short Form Health Survey (SF-36), II: psychometric and clinical tests of validity in measuring physical and mental health constraints. Med Care. 1993;31:247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. Boston, Mass: Health Assessment Lab, New England Medical Center Health Institute; 1993. [Google Scholar]
- 8.Skinner K, Miller D, Kazis L, et al. The Health Related Quality of Life in Veterans: A Pilot Study. Washington, DC: Health Services Research and Development Service, Veterans Health Administration; 1995. Study design and implementation of the veterans health study. In. Technical report SDR 91006.S. [Google Scholar]
- 9.Norell SE. Methods in assessing drug compliance. Acta Med Scand. 1983;(683):35–40. doi: 10.1111/j.0954-6820.1984.tb08712.x. [DOI] [PubMed] [Google Scholar]
- 10.Haynes BR, Taylor W, Sackett DL, et al. Can simple clinical measurements detect patient noncompliance. Hypertension. 1980;2:757–64. doi: 10.1161/01.hyp.2.6.757. [DOI] [PubMed] [Google Scholar]
- 11.Inui TS, Carter WB, Pecoraro RE. Screening for noncompliance among patients with hypertension: is self-report the best available measure. Med Care. 1981;19:1061–4. doi: 10.1097/00005650-198110000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Karch FE, Lasagna L. Adverse drug reactions: a critical review. JAMA. 1975;234:1236–41. [PubMed] [Google Scholar]
- 13.Kramer MS, Leventhal JM, Hutchinson TA, et al. An algorithm for the operational assessment of adverse drug reactions, i: background, description, and instructions for use. JAMA. 1979;242:623–32. [PubMed] [Google Scholar]


