Abstract
OBJECTIVE
To assess health-related quality of life (HRQOL) in men with erectile dysfunction.
DESIGN
Descriptive survey with general and disease-specific measures. The instrument contained three established, validated HRQOL measures, a validated comorbidity checklist, and sociodemographics. The RAND 36-Item Health Survey 1.0 (SF-36) was used to assess general HRQOL. Sexual function and sexual bother were assessed using the UCLA Prostate Cancer Index. The marital interaction scale from the Cancer Rehabilitation Evaluation System Short Form (CARES-SF) was used to assess each patient's relationship with his sexual partner.
SETTING
Urology clinics at a university medical center and the affiliated Veterans Affairs (VA) Medical Center.
PARTICIPANTS
Thirty-five (67%) of 54 consecutive university patients presenting for erectile dysfunction and 22 (42%) of 52 VA patients who were awaiting a previously prescribed vacuum erection device participated.
MAIN RESULTS
The university respondents scored slightly lower than population normals in social function, role limitations due to emotional problems, and emotional well-being. The VA respondents scored lower than expected in all eight domains. Scores for the VA population were significantly lower than those for the university population in physical function, role limitations due to physical problems, bodily pain, and social function. A significant correlation was seen between marital interaction and sexual function (r = −.33, p = .01) but not between marital interaction and sexual bother (r = −.15, p = .26) in the total sample. Sexual function also correlated significantly with general health perceptions (r = .34, p = .01), role limitations due to physical problems (r = .29, p = .03), and role limitations due to emotional problems (r = .30, p = .03). Sexual bother did not correlate with any of the general HRQOL domains. Affluent men reported better sexual function (p = .03).
CONCLUSIONS
The emotional domains of the SF-36 are associated with more profound impairment than are the physical domains in men with erectile dysfunction. Erectile dysfunction and the bother it causes are discrete domains of HRQOL and distinct from each other in these patients. With increased attention to patient-centered medical outcomes, greater emphasis has been placed on such variables as HRQOL. This should be particularly true for a patient-driven symptom, such as erectile dysfunction.
Keywords: erectile dysfunction, impotence, health-related quality of life, medical outcomes
A lthough erectile dysfunction commands a great deal of attention in medical care, research seldom focuses on assessing health related quality of life (HRQOL) in men with this complaint. The majority of published reports in this area concern the evaluation of specific diagnostic and therapeutic strategies.1–6 Indeed, the field has advanced significantly in recent years with the advent of intracavernosal injection 7–10 and intraurethral therapy.11 As health care increasingly moves to the primary care setting, generalists must be more attuned to the pathophysiology, treatments, and psychosocial impacts of erectile dysfunction in their patients. The impact of erectile dysfunction on HRQOL is of particular concern to primary care physicians as they work to balance a variety of conditions and treatments, all of which may affect HRQOL.
Erectile function may be impaired by a number of conditions, both physical and psychological, and is a well-documented potential outcome of treatment for prostate cancer. Sexual function also declines with advancing years. The Massachusetts Male Aging Study demonstrated that rates of complete erectile dysfunction triple from 5% to 15% between ages 40 and 70.12 Despite these expected decreases in function, sexual interest persists. In a sample of 427 veterans, Mulligan and Moss found that although sexual function declined, sexual interest remained present, albeit diminished, among older veterans.13 As the U.S. population continues to age, erectile dysfunction is likely to become an even more prevalent issue for patients. Although much is known about the pathophysiology of erectile dysfunction,14 relatively little is known about how it affects men's daily lives.15, 16 In this study we sought to describe the impact of erectile dysfunction on HRQOL.
METHODS
Subjects
Patients were recruited both from the urology clinic at our university medical center and from the urology clinic at our affiliated Veterans Affairs (VA) Medical Center. Fifty-four consecutive men who scheduled appointments in the private university urology clinic for a primary complaint of erectile dysfunction from July through October 1994 were recruited to enter the study. Patients were mailed a letter of introduction along with the HRQOL questionnaire and a stamped return envelope 1 week prior to their scheduled appointment. Twelve patients scheduled their appointment less than 1 week in advance and were verbally recruited, then hand-delivered the letter of introduction, questionnaire, and return envelope. Patients in the VA population were recruited from a list of 52 men who had previously been prescribed a vacuum erection device for erectile dysfunction but were awaiting shipment of the device as of July 1994. A letter of introduction was mailed to each patient along with the HRQOL questionnaire and a stamped return envelope. Telephone reminders were used for all patients not responding within 4 weeks. Patient selection criteria were designed to capture the largest possible group of men who had initiated medical care for their chief complaint of erectile dysfunction. Because care is accessed and administered so differently in the populations from which we could recruit, we structured our study to cast the widest possible net.
Our rationale for choosing these study populations was to begin to collect descriptive data from as divergent a group of subjects as we could find, most of whom have until now been largely overlooked in HRQOL research because of the elective nature of their condition. We excluded patients who could not read and write English and those who did not wish to participate in the study. We did not exclude or attempt to stratify patients based on the etiology of their erectile dysfunction. Our study was approved by our institution's Human Subjects Protection Committee.
Outcome Measures
Both general and disease-specific measures were included in the questionnaire. The instrument contained three established, validated HRQOL measures, a medical comorbidity checklist, a sociodemographic section. The RAND 36-Item Health Survey (SF-36) was used to assess general HRQOL.17–19 This previously validated, self-administered, 36-item questionnaire addresses eight domains of quality of life: physical function, bodily pain, vitality, role limitations due to physical problems (role-physical), general health perceptions, emotional well-being, social function, and role limitations due to emotional problems (role-emotional). The first four domains are considered the physical domains and the last four are considered the emotional domains. The eight domains are scored separately from 0 to 100 with higher scores representing better HRQOL. Patient scores were compared with age-matched population normals presented in the SF-36 manual.20
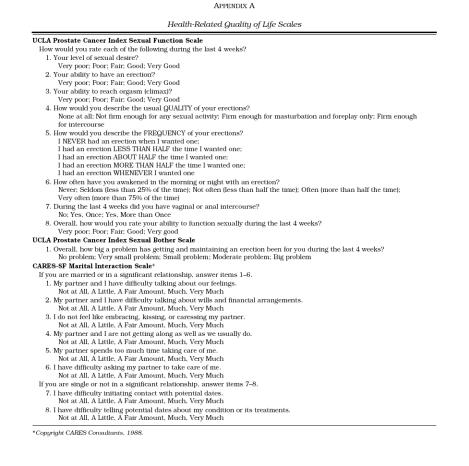
Sexual function and sexual bother were assessed using the UCLA Prostate Cancer Index.21 This previously validated, self-administered instrument was designed to measure disease-specific HRQOL in sexual function, sexual bother, urinary function, urinary bother, bowel function, and bowel bother. Only those seven questions relating to sexual function and bother were included in our questionnaire. Guyatt et al. have emphasized the importance of including global assessment items in HRQOL scales,22 and the UCLA Sexual Function scale includes such an item. This instrument employs 0 –100 scales with higher scores representing better HRQOL. It was validated in patients with and without cancer, many of whom had erectile dysfunction; hence, it was thought to be appropriate for men with a chief complaint of erectile dysfunction.
The marital interaction scale from Cancer Rehabilitation Evaluation System Short Form (CARES-SF) was used to assess each patient's relationship with his sexual partner.23–26 This scale includes a set of items for those in significant relationships and an alternative set of items for those not in such relationships. The CARES-SF has been validated in a variety of clinical settings and is scored from 0 to 4 with lower scores representing better HRQOL. It has not been routinely used in noncancer patients.
Medical comorbidity was elicited using a 12-item medical checklist, developed from an established comorbidity rating scale, the Incidence of Coexistent Disease (ICED).27 Sociodemographic questions included items on race, gender, age, smoking history, marital and employment status, education and income.
The survey instrument took approximately 25 minutes to complete. The marital interaction, sexual function, and sexual bother scales are included in Appendix A.
Statistical Analysis
Descriptive statistics for sociodemographic and comorbidity data are presented. Scale scores for HRQOL are presented as means and standard errors. Results from the two populations were not statistically compared in this analysis because of the great underlying differences between the two samples. Rather, HRQOL data from several other populations are presented for comparison. Sociodemographic variables were compared using χ2 analysis. Pearson product-moment correlation coefficients were calculated among the HRQOL scales and between the continuous sociodemographic variables and HRQOL scales using SAS (SAS User's Guide, Statistics. 5th ed. Cary, NC: SAS Institute; 1985). Bivariate analyses were performed for categorical sociodemographic variables with sexual function and sexual bother using Student's t test with α = 0.05.
RESULTS
Subjects
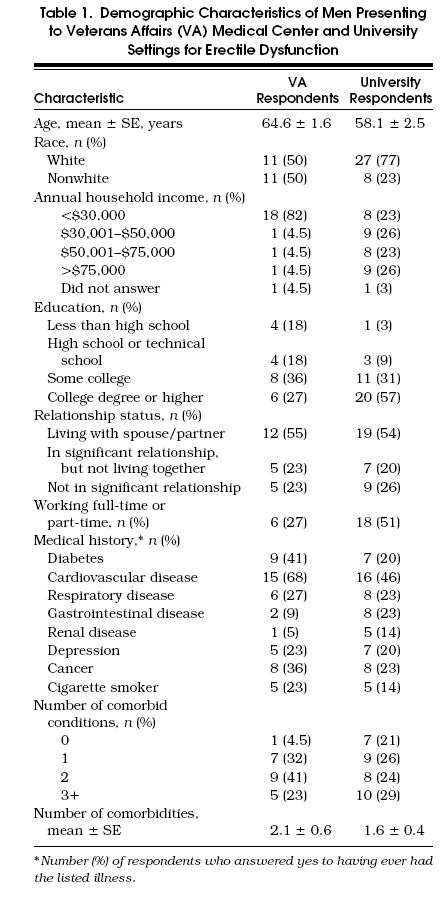
Of 61 men presenting to the private university urology clinic with a chief complaint of erectile dysfunction, 52 kept their appointments and therefore were considered eligible for the study. Thirty-five (67%) of these men completed and returned the survey. This response rate was similar whether men were mailed the survey (27 of 40, 68%) or were given the survey personally (8 of 12, 67%). Telephone reminders yielded no additional surveys. In the VA population, 22 (42%) of the patients recruited returned the initial survey. Of the 30 patients who did not complete the survey, 2 were physically unable to do so secondary to illness and 12 did not have a correct address or telephone number on file at the VA. No other information on the nonrespondents was available. Their results were not included in the study.Table 1 displays the demographic and comorbidity characteristics of the subjects.
Table 1.
Demographic Characteristics of Men Presenting to Veterans Affairs (VA) Medical Center and University Settings for Erectile Dysfunction
Performance of the Instruments
Descriptive statistics and reliability estimates for the HRQOL measures are not shown. There was good internal consistency with Cronbach's α coefficients,28 exceeding 0.79 for all scales. Only three surveys had missing data (each on the marital interaction scale) suggesting that the survey was not difficult to complete. In each of these three cases, at least 50% of the responses were present, and the missing data were replaced by using an average score of the known responses as described in the SF-36 Manual.20
The universally low sexual function and sexual bother scores validate the entry criterion for our study.
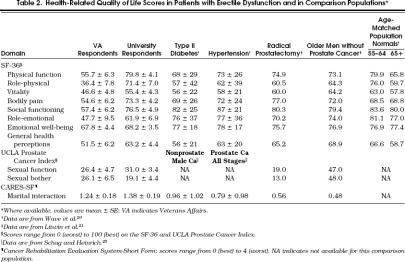
General Health-Related Quality of Life
Table 2 illustrates general HRQOL as measured by SF-36 for the total patient population as well as for the VA and university samples individually. Scores for patients with type II diabetes or hypertension,20 men undergoing radical prostatectomy,21 older men without prostate cancer,21 and age-referenced population normals 20 are presented for comparison. A difference of 6 to 8 points is generally considered to be clinically meaningful.29, 30 The university respondents scored slightly lower than population normals in social function, role-emotional, and emotional well-being. The VA respondents scored lower than expected in all eight domains.
Table 2.
Health-Related Quality of Life Scores in Patients with Erectile Dysfunction and in Comparison Populations*
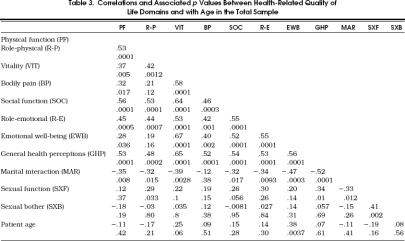
Sexual Function, Sexual Bother, and Marital Interaction
Table 2 also shows the results of the CARES-SF (marital interaction) and UCLA Prostate Cancer Index (sexual function and sexual bother) scales for the VA and university groups, the comparison populations, and two other populations: men with nonprostrate cancers (such as lung and colon) and men with various stages of prostate cancer.25 Correlation coefficients and associated p values between domains are presented in Table 3 for the total sample. A significant correlation was seen between sexual function and marital interaction (r= 2.33, p= .01) although not between sexual bother and marital interaction (r= −.15, p= .26). Note that a higher score on the CARES-SF marital interaction scale represents poorer HRQOL in this domain, hence reversing the sign of the correlation coefficient. Sexual function also correlated significantly with general health perceptions (r= .34, p= .01), role-physical (r= .29, p= .03), and role-emotional (r = .30, p= .03). Sexual bother did not correlate significantly with any of the eight general HRQOL domains. Marital interaction correlated significantly with all of the general HRQOL domains except bodily pain. Of these, general health perceptions (r= −.52, p= .0001) and emotional well-being (r= −.47, p= .0003) had the highest correlation coefficients.
Table 3.
Correlations and Associated pValues Between Health-Related Quality of Life Domains and with Age in the Total Sample
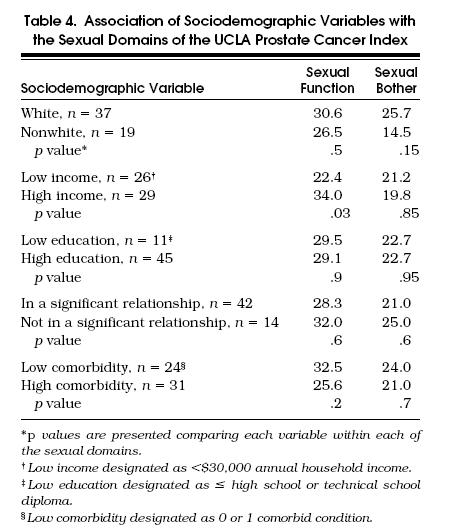
Among the various sociodemographic comparisons in the total sample, shown in Table 4, no racial differences (white vs nonwhite) were seen for sexual function or sexual bother. Despite similar sexual function scores for whites and nonwhites, the latter group trended toward greater sexual bother (p= .15). Neither education level nor relationship status was associated with any difference in the sexual domains. Household income had no association with sexual bother, but more affluent men reported better sexual function (p= .03). No association with the number of comorbidities was seen for either sexual domain.
Table 4.
Association of Sociodemographic Variables with the Sexual Domains of the UCLA Prostate Cancer Index
DISCUSSION
Our study has several important findings. First, the emotional domains of the RAND SF-36 are more profoundly affected by erectile dysfunction than are the physical domains. In both university clinic and VA clinic patients, erectile dysfunction was associated with worse psychosocial function than in population normals. Only the veterans, however, scored worse in the physical domains. This suggests that erectile dysfunction is more likely associated with impairments in mental than in physical HRQOL domains. The observation that veterans scored substantially lower than population normals on the physical domains is consistent with clinical experience regarding the generally poorer physical health of this population.
Second, erectile dysfunction is a component of quality of life distinct from the bother it causes. Indeed, the correlation coefficient of only 0.41 between sexual function and sexual bother indicates that some men with erectile dysfunction are less troubled than others by their dysfunction. Several observations support this conclusion. Among all respondents, sexual function correlated weakly with three of the general HRQOL domains (social function, vitality, and emotional well-being), but sexual bother did not correlate with any. In addition, sexual function demonstrates a weak but significant correlation with marital interaction (r= 2.33, p= .01), but sexual bother does not. This emphasizes that men's spousal relationships may be interdependent with their sexual function, while their sexual bother appears to be independent of this interaction. Finally, despite similar sexual function scores, nonwhites showed a trend toward more bother from their erectile dysfunction than did whites, suggesting that subset analyses in larger samples may illuminate this finding. Hence, when evaluating men with erectile dysfunction, physicians must separate actual sexual performance from its emotional impact.
Third, it is imperative to include disease-specific domains to achieve a fuller picture of HRQOL. The low correlation coefficients between sexual function and bother and the SF-36 domains demonstrate that general HRQOL measures alone do not adequately capture disease-specific impairments in patients' quality of life. Although the low correlations may partially reflect the uniformly low sexual function and bother scores across all our patients, similar low correlations between the SF-36 and sexual domains were also seen in a different population we have studied following treatment for prostate cancer (unpublished data).
Lastly, among the sociodemographic and comorbidity factors, only income was associated with group differences in sexual function (p= .03), while none correlated with sexual bother. That affluent men with erectile dysfunction reported better sexual performance than men with lower incomes, despite similar bother, suggests that they may present for evaluation earlier in the course of their impairment. As most of the lower-income individuals were in the VA population (for which financial status should not limit access to health services), this observation may reflect nonfinancial barriers to access to care. Alternatively, this finding might disappear if corrections were made for multiple comparisons.
Several other investigators have reported the interactions between erectile dysfunction and various HRQOL domains. Recently, Georghiu et al. examined HRQOL in men before and after treatment with intracavernosal injection therapy.15 They used the Duke Health Profile for General Mental Health, Social Health, Self-Esteem, Anxiety, and Depression and an instrument developed at Case Western Reserve University to measure frequency of intercourse, quality of erections, and general sexual satisfaction. Their patients' mean baseline quality of erection score of 3.8 (possible range, 0–8, higher is better) is consistent with our patients' mean score of 45 (possible range, 0–100) on our quality of erection item. Unlike our study, the selection requirements of their study excluded a priori men not in stable relationships and those with known psychiatric disorders. Hence, anxiety and depression were rare in their study group. Despite better mental health in their sample, quality of erections was equally poor in both studies. Our analysis expands the assessment of erectile dysfunction from a single item to two domains, sexual function and sexual bother, capturing a fuller picture of erectile dysfunction.
Helgason et al. developed a scale to examine how sexual function affects HRQOL after pelvic irradiation for prostate cancer.16 This study primarily focused on differences in sexual function and desire before and after treatment, but it did include a global item assessing the extent to which “sexual wishes,”“erectile capacity,” and “orgasm function” affected quality of life. Although the study did not use any general HRQOL scales, half of these patients felt that the decreased erectile function following radiation therapy affected their quality of life “much” or “very much.” This is consistent with our finding that HRQOL is impacted by erectile dysfunction; however, our results suggest that the emotional HRQOL domains are affected more severely than the physical domains. Contrary to the Massachusetts Male Aging Study,12 we found no correlation between erectile function and number of comorbidities or age, although patients' ages in the two studies were fairly uniform.
Any health impairment may provide a source of emotional distress and may in turn manifest as a change in HRQOL. When a man seeks help for erectile dysfunction, he is likely to be particularly sensitive to the distress caused by his problem. Typically, a man lives with his dysfunction for several months or years before seeing a physician for medical attention. The impetus for his visit may be a discussion with his partner, some significant life event, or something as simple as a magazine article. Regardless of what the catalyst is, patients with erectile dysfunction clearly need physicians who are at once compassionate and knowledgeable about the physical and psychosocial effects of this embarrassing clinical entity. It is also clearly difficult to dissect the HRQOL impairment associated with the erectile dysfunction from that which may result from other related conditions such as diabetes or hypertension. It is less clear whether other men do not seek intervention because they are less distressed or more embarrassed. The sensitive clinician may have difficulty sorting out the various potential sources of anxiety in order to intervene successfully. These issues present numerous methodologic challenges when studying HRQOL in men with erectile dysfunction. Certainly, it is challenging for researchers to provide data that can be clinically helpful while provoking innovative thought about this condition. To build a foundation for such work, we must first paint a picture of HRQOL with broad brush strokes, such as those presented here. Subsequent questions can then be addressed at teasing out the fine details of men's life experience with erectile dysfunction.
Our study has several specific limitations. The relatively small sample sizes may not have provided sufficient power to identify differences with comparison populations. The lower response rate in the VA patients may also have introduced systematic errors in reported HRQOL scores (higher or lower). In our sociodemographic data, we cannot exclude the potential problem of multiple comparisons as an explanation for the statistically significant difference in sexual function between the low- and high-income patients. In addition, the two patient groups were very distinct from each other in many ways, potentially limiting the generalizability of our findings. The retrospective, cross-sectional nature of the study design may have introduced still other biases. Conversely, the fact that 50% of the sample was nonwhite adds an important dimension to the interpretation of our results.
With increased attention to patient-centered medical outcomes in recent years, greater emphasis has been placed on such variables as HRQOL. This should be particularly true for a patient-driven symptom such as erectile dysfunction. Hence, generalists and urologists should be especially cognizant not only of the physical problems associated with erectile dysfunction, but also with the impact it has on men's daily quality of life. Our study documents profound impairment in many domains of HRQOL among men with erectile dysfunction. Not surprisingly, the emotional issues raised by this problem appear to be significant. To provide helpful diagnostic and therapeutic interventions for these patients, we must remain aware of the myriad ways in which erectile dysfunction can alter men's HRQOL. This has clinical relevance in patient care and in investigational protocols. Armed with a richer database that includes HRQOL as well as the more familiar pathophysiologic measures, we can then provide better care for men with erectile dysfunction.
Acknowledgments
Supported by a New Investigator Award from the American Foundation for Urologic Disease.
Appendix A
Health-Related Quality of Life Scales
References
- 1.Althof S, Turner L, Levine S, et al. Why do so many people drop out from auto-injection therapy for impotence? J Sex Marital Ther. 1989;15:121–9. doi: 10.1080/00926238908403816. [DOI] [PubMed] [Google Scholar]
- 2.Bechara A, Casabe A, Cheliz G, Romano S, Fredotovich N. Prostaglandin E1versus mixture of prostaglandin E1papaverine and phentolamine in nonresponders to high papaverine plus phentolamine doses. J Urol. 1996;155:913–4. [PubMed] [Google Scholar]
- 3.Gee WF, Holtgrewe HL, Albertson PC, et al. Practice trends of American urologists in the treatment of impotence, incontinence, and infertility. J Urol. 1996;156:1778–80. [PubMed] [Google Scholar]
- 4.Hollander JB, Gonzalez J, Norman T. Patient satisfaction with pharmacologic erection program. Urology. 1992;39:439–41. doi: 10.1016/0090-4295(92)90242-o. [DOI] [PubMed] [Google Scholar]
- 5.Irwin MB, Kata EJ. High attrition rate with intracavernous injection of prostaglandin E1for impotency. Urology. 1994;43:84–7. doi: 10.1016/s0090-4295(94)80272-6. [DOI] [PubMed] [Google Scholar]
- 6.Turner LA, Althof SE, Levin SB, Bodner DR, Kursh ED, Resnick MI. Twelve-month comparison of two treatments for erectile dysfunction: self-injection versus external vacuum devices. Urology. 1992;39:139–44. doi: 10.1016/0090-4295(92)90270-7. [DOI] [PubMed] [Google Scholar]
- 7.Godschalk M, Gheorghiu D, Chen J, Katz PG, Mulligan T. Long-term efficacy of a new formulation of prostaglandin E1as treatment for erectile dysfunction. J Urol. 1996;155:915–7. [PubMed] [Google Scholar]
- 8.Hedlund H, Anderson K-E. Contraction and relaxation induced by some prostenoids in isolated human penile erectile tissue and cavernous artery. J Urol. 1985;134:1245–50. doi: 10.1016/s0022-5347(17)47704-4. [DOI] [PubMed] [Google Scholar]
- 9.Porst H. The rationale for prostaglandin E1in erectile failure: a survey of worldwide experience. J Urol. 1996;155:802–15. [PubMed] [Google Scholar]
- 10.Sidi AA, Reddy PK, Chen KK. Patient acceptance of and satisfaction with vasoactive intracavernous pharmacotherapy for impotence. J Urol. 1988;140:293–4. doi: 10.1016/s0022-5347(17)41586-2. [DOI] [PubMed] [Google Scholar]
- 11.Padma-Nathan H, Hellstrom WJ, Kaiser FE, et al. Treatment of men with erectile dysfunction with transurethral alprostadil. N Engl J Med. 1997;336:1–7. doi: 10.1056/NEJM199701023360101. [DOI] [PubMed] [Google Scholar]
- 12.Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151:54–61. doi: 10.1016/s0022-5347(17)34871-1. [DOI] [PubMed] [Google Scholar]
- 13.Mulligan T, Moss CR. Sexuality and aging in male veterans: a cross-sectional study of interest, ability, and activity. J Arch Sex Behav. 1991;20:17–25. doi: 10.1007/BF01543004. [DOI] [PubMed] [Google Scholar]
- 14.Carrier S, Brock G, Kour NW, Lue TF. Pathophysiology of erectile dysfunction. Urology. 1993;42:468–81. doi: 10.1016/0090-4295(93)90391-m. [DOI] [PubMed] [Google Scholar]
- 15.Gheorghiu S, Godschalk M, Gemtili A, Mulligan T. Quality of life in patients using self-administered intracavernous injections of prostaglandin E1for erectile dysfunction. J Urol. 1996;156:80–1. [PubMed] [Google Scholar]
- 16.Helgason A, Fredrikson M, Adolfsson J, Steineck G. Decreased sexual capacity after external radiation therapy for prostate cancer impairs quality of life. Int J Radiat Oncol Biol Phys. 1995;32:33–9. doi: 10.1016/0360-3016(95)00542-7. [DOI] [PubMed] [Google Scholar]
- 17.Litwin MS. Measuring health-related quality of life in men with prostate cancer. J Urol. 1994;152:1882–7. doi: 10.1016/s0022-5347(17)32407-2. [DOI] [PubMed] [Google Scholar]
- 18.Ware JE, Sherbourne CD. The MOS 36-Item short-form health survey (RAND 36-Item Health Survey), I: conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 19.Stewart AL, Greenfield S, Hays RD, et al. Functional status and well-being of patients with chronic conditions: results from the Medical Outcomes Study. JAMA. 1989;262:907–13. [PubMed] [Google Scholar]
- 20.Ware JE, Snow KK, Kosinski M, et al. RAND 36-Item Health Survey: Manual and Interpretation Guide. Boston, Mass: The Health Institute, The New England Medical Center; 1993. [Google Scholar]
- 21.Litwin MS, Hays RD, Fink A, et al. Quality of life outcomes in men treated for localized prostate cancer. JAMA. 1995;273:129–35. doi: 10.1001/jama.273.2.129. [DOI] [PubMed] [Google Scholar]
- 22.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118:622–9. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- 23.Ganz PA, Schag CAC, Lee JJ, et al. The CARES: a generic measure of health-quality of life for patients with cancer. Qual Life Res. 1992;1:19–29. doi: 10.1007/BF00435432. [DOI] [PubMed] [Google Scholar]
- 24.Schag CAC, Ganz PA, Heinrich RL. Cancer Rehabilitation Evaluation System Short Form (CARES-SF): a cancer-specific rehabilitation and quality of life instrument. Cancer. 1991;68:1404–13. doi: 10.1002/1097-0142(19910915)68:6<1406::aid-cncr2820680638>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 25.Schag CAC,, Heinrich RL. Cancer Rehabilitation Evaluation System (CARES) Manual. Los Angeles, Calif: CARES Consultants; 1988. [Google Scholar]
- 26.Schag CAC, Heinrich RL. Development of a comprehensive quality of life measurement tool: CARES. Oncology. 1990;4:135–8. [PubMed] [Google Scholar]
- 27.Greenfield S, Apolone G, McNeil BJ, Cleary PD. The importance of coexistent disease in the occurrence of post-operative complications and one-year recovery in patients undergoing total hip replacement: comorbidity and outcomes after hip replacement. Med Care. 1993;31:141–54. doi: 10.1097/00005650-199302000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 29.Ware JE, Kosinski M, Keller SK. SF-36 Physical and Mental Health Summary Scales: A User's Manual. Boston, Mass: The Health Institute, New England Medical Center; 1994. [Google Scholar]
- 30.Testa MA, Simonson DC. Assessment of quality-of-life outcomes. N Engl J Med. 1996;334:835–40. doi: 10.1056/NEJM199603283341306. [DOI] [PubMed] [Google Scholar]