Abstract
OBJECTIVE
The movement for advance planning of end-of-life care was motivated in part by the assumption that medical intervention for terminally ill patients varies from what these patients would prefer. We examined the validity of this assumption by comparing actual life-sustaining treatment practices for patients in critical illness scenarios and surveyed patients' advance care preferences.
MEASUREMENTS AND MAIN RESULTS
We selected at random and reviewed 7,400 inpatient medical records from a single urban teaching hospital during the period just prior to the Patient Self-Determination Act. Records of 198 patients with conditions that matched advance directive scenarios were examined, and practices to withhold or withdraw seven life-sustaining treatments were documented. Practices were compared with surveyed preferences of 102 members of the general public and 495 outpatients who were followed by the same physicians as the 198 patients. Concordance of practices and preferences for the 19 surveyed outpatients who eventually fell into one of the scenarios was also evaluated. One hundred sixty-seven inpatient cases met review criteria for the scenario coma with a small chance of recovery. Hospital patients received medical interventions that were not consistently greater or less than the preferences of the surveyed outpatients or members of the general public. Resuscitation, the most frequently withheld treatment (94% of cases), was withheld more often than surveyed preferences to decline it (56% of outpatients, p < .001). Four treatments—mechanical breathing, artificial nutrition, major surgery, and hemodialysis—were utilized comparably to surveyed outpatients' preferences (range p=.704 –.055). Antibiotics and artificial hydration were withheld (9% and 6%, respectively) less often than surveyed outpatient's prior preferences to decline them (48% and 52%, respectively, p < .001 for each). Conversely, treatments given to the 19 surveyed patients who subsequently developed one of the illness scenarios were often incongruent with the patients' prior preferences. Again, in some cases more interventions were provided (26 of 63 declined treatments were given), and in some cases less (10 of 21 desired treatments were withheld).
CONCLUSIONS
This study does not support the assumption that, collectively, patients' advance care preferences are less interventionist than actual practices for patients in corresponding scenarios. Nevertheless, these results do support the assumption that life-sustaining treatment decisions do not conform well to individual patients' specific preferences. Progress in end-of-life care should focus on shared decision making at the patient-proxy-physician level rather than on overall life-sustaining treatments utilization.
Keywords: advance directives, life support care, critical care, patient participation, treatment refusal
Life-sustaining treatment decisions made for unconscious patients in the absence of advance directives are often assumed, first, to be discordant with individuals' prior preferences,1 and second, to result in more treatments at the end of life than patients would have wanted.2–5 Actual data on life-sustaining treatment practices have not been available to challenge or support either of these assumptions.
Surrogate decisions about eventual end-of-life care often differ from patients' own stated preferences,6, 7 which is indirect evidence that the first assumption is valid. A more definitive assessment could be obtained by directly measuring the concordance between actual treatment practices and individuals' own advance preferences for care. The few studies in which patients' preferences and their eventual treatments were examined prospectively came to differing conclusions.8, 9 One reported about overtreatment, but not about undertreatment.9 No study has prospectively followed a full range of life-sustaining treatment preferences and eventual treatments.
It could also be informative to compare preferences with practices over a range of life-sustaining treatments to estimate the effect that advance directives might have on resource utilization. Treatment preferences of surveyed populations, physicians, nurses, patients and their families and proxies, medical students, and the general public are available.6, 7,10–18 Although data exist on life-sustaining treatments for certain diagnoses and among deceased patients, these are less suited for investigating utilization in common advance directive scenarios. The present study compares preferences selected in a general advance directive survey and actual treatment practices for patients with conditions described in the advance directive scenarios.
We documented the life-sustaining treatment practices at an urban teaching hospital where outpatients and members of the general public in the vicinity had been surveyed with an advance directive.13 For each of seven life-sustaining treatments, we asked whether it was provided more than, less than, or the same as surveyed preferences for that treatment in advance directive scenarios. The period of study was just prior to the Patient Self-Determination Act, when care was virtually uninfluenced by advance directives.18
We also followed the surveyed patients prospectively to compare their advance care preferences with the actual treatments they received when in one of the scenarios. The overall aim was to find evidence supporting or refuting the stated common assumptions about advance care planning.
METHODS
Data Collection
We collected data on life-sustaining treatments provided between February 1987 and June 1989, corresponding to the time period of two advance directive surveys.13 One survey had been administered to a convenience sample of outpatients drawn from the waiting rooms of all the physicians in practice at an urban teaching hospital's ambulatory care unit and AIDS clinic. There were five interviewers: a physician, a nurse, and three research assistants trained in the interview process. Only patients with a major psychiatric diagnosis or a language barrier were excluded. A separate telephone survey had been administered by a survey research facility to members of the general public drawn at random from the hospital's vicinity.
Subjects were read the texts of four illness scenarios and 11 treatment options for each scenario, with repeated readings if requested. Outpatients' and the public's treatment options were identical except that artificial hydration was not offered as an option in the public's survey. The scenarios are referred to as coma with a small chance of recovery, dementia, dementia with a terminal illness, and persistent vegetative state. The first reads: “If, in the opinion of my physician and two consultants, I am in a coma, with a small and uncertain chance of regaining higher mental functions, and a greater chance of recovering with some residual damage, and a much greater chance of not recovering at all, then my wishes, if medically reasonable, for this and any additional illness would be:” The text of each scenario is available.19 Respondents were asked which they would want from the list of possible medical interventions and for each treatment in each of the scenarios they were asked to choose from the following: “I want”;“I want treatment tried. If no clear improvement, stop”;“I am undecided”; or “I do not want.”
With Human Studies Review Board approval, we reviewed randomly selected charts of patients who had been admitted to the hospital in the designated time period by the same private physicians whose ambulatory patients were surveyed. We used specific criteria, developed by four physicians, for identifying scenarios and recognizing whether treatments were given (see Appendix A). They consisted of signs, symptoms, and test results normally recorded in medical charts, and they included alternatives where applicable. We classified each of the treatments as having been given, witheld(medically indicated and not received), withdrawn(medically indicated and received, but later withdrawn and patient allowed to die), or not medically indicated.
Each chart was reviewed according to the criteria to determine if the patient's condition corresponded to one of the four scenarios. We screened 7,400 charts, and 198 cases were identified. We also reviewed the charts of all 495 patients who had been surveyed. For each case, we recorded patient's age, gender, attending physician, primary diagnosis, any corresponding advance directive scenario, and use of any of seven life-sustaining treatments (cardiopulmonary resuscitation, mechanical ventilation, artificial hydration, artificial nutrition, major surgery, hemodialysis, and antibiotics) while in the scenario. Sociodemographic data of inpatients and outpatients (age, gender, marital status, place of residence, and health insurance) were obtained from the hospital administrative record.
Three trained reviewers applied the criteria to 50 randomly selected charts to assess interrater reliability for identifying cases and to 49 randomly selected charts to assess interrater reliability for determining treatment utilization.
Data Analyses
Analyses focused on the scenario coma with a small chance of recovery because it accounted for 84% of the cases identified. Contingency table analyses and Pearson's χ2 statistic were used for discrete comparisons among surveyed preferences, utilization rates, and sociodemographic features. The Bonferroni adjustment was made for multiple comparisons.20 Logistic regression was used to determine whether utilization differed overall from surveyed preferences, accounting for age, gender, specific treatment type, and scenario.
Separate logistic regression models compared practices with surveyed preferences of either outpatients or the general public. The treatment decision made, either surveyed preference or actual practice, was the dependent variable in each of the models. This variable was defined in two alternative ways. One modeled actual withholding of treatment and preferences to decline the treatment, and the other modeled the broader category of limiting(withholding or withdrawing) the treatment and preferences to either decline or accept a limited trial of the treatment. We assumed that requests for treatment trials are analogous to providing and later withdrawing treatments, and that actions guided by “uncertain” treatment preferences would usually lead initially to a treatment trial. The main independent variable tested in the regressions was whether the observation was a surveyed preference or a documented treatment practice.
Six dummy variables representing the seven treatments were introduced in the regressions so that comparisons between practices and preferences could be made for each treatment. Each subject therefore generated six observations. Huber's formula for estimates of maximum likelihood standard errors was used to account for correlation between these multiple observations per subject.21
The κ statistic, a measure of agreement that adjusts for chance, was used to assess interrater reliability.22(κ is given by [po−pe]/[1 −pe], where pois the observed proportion of agreement, and peis the proportion of agreement expected by chance.) Statistical analyses were performed with STATA Statistical Software (Release 4.0. College Station, Tex: Stata Corp.; 1995).
RESULTS
Interrater Reliability
The κ interrater reliability statistics were .89 for identifying cases; .40 to .49 for classifying cases into scenarios and for determining utilization of mechanical breathing, artificial hydration, major surgery, hemodialysis, and antibiotics; .86 for determining utilization of cardiopulmonary resuscitation; and .30 for determining utilization of artificial nutrition. Values of at least .4 are often taken as reasonable agreement beyond the level of chance.
Study Sample
Of 7,400 randomly selected charts, 198 admissions (3%) matched one of the scenarios. Of these, 167 case subjects were in coma with a small chance of recovery, 17 had dementia, 10 had dementia with a terminal illness, and 4 were in a persistent vegetative state. Thirteen case subjects met criteria for more than one scenario and were classified according to the earliest cause of mental incompetence (5 in coma with a small chance of recovery and 8 in one of the remaining scenarios). Case subjects were treated by 109 attending physicians and had 36 primary diagnoses. Only one chart referred to an advance directive, and 68% had any preferences regarding care noted including those of patients or family or proxy. Of these, 123 (91%) were either treatment declines or requests for comfort measures only.
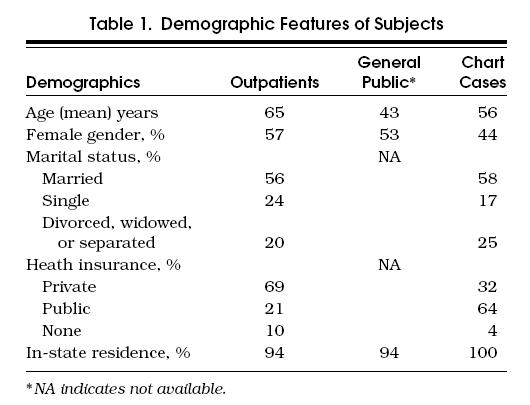
Of an initial pool of 829 outpatients, 495 (60%) responded to the surveys, and 102 (76%) of an initial pool of 135 members of the general public responded.13 Nineteen of the outpatients had subsequently been admitted to the hospital and were in a situation corresponding to one of the scenarios by February 1995, seven years later. Demographic features are displayed in Table 1). Race was not recorded consistently in charts and could not be included.
Table 1.
Demographic Features of Subjects
Demographic Factors
Outpatient and general public prior preferences were previously found not to be associated with health or demographic characteristics.13 Logistic regression analysis confirmed that there was no association between prior preferences (either to decline or to limit any of the treatments) and gender, marital status, health insurance, or place of residence in either group (p>.15 in each instance). Age alone was associated with outpatients' prior preferences to withhold or to limit treatments (p≤ .012) and to withhold hemodialysis among the general public (p= .042), although the effect was small. None of these demographic features was associated with actual practices of withholding or withdrawing treatment (p>.10). The one exception, an association between limiting hemodialysis and health insurance, was not significant after adjusting for multiple comparisons (p= .14).
Life-Sustaining Treatment Utilization and Preferences
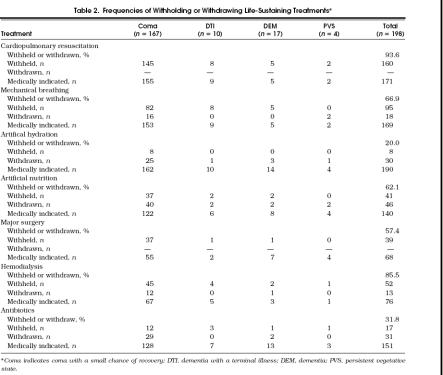
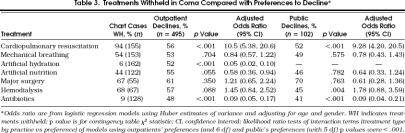
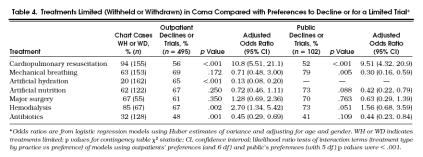
Life-sustaining treatments were limited, with incidences ranging from 20% for artificial hydration to 94% for cardiopulmonary resuscitation (Table 2 Surveyed preferences have been reported.13 Preferences to have a trial of treatment or to decline treatments in coma with a small chance of recovery are shown in Tables 3 and 4 with the frequencies they were found to be actually withheld. Preferences to have a trial only of treatments ranges from 48% to 69% among outpatients and from 41% to 79% among the public.
Table 2.
Frequencies of Withholding or Withdrawing Life-Sustaining Treatments*
Table 3.
Treatments Withheld in Coma Compared with Preferences to Decline*
Table 4.
Treatments Limited (Withheld or Withdrawn) in Coma Compared with Preferences to Decline or for a Limited Trial*
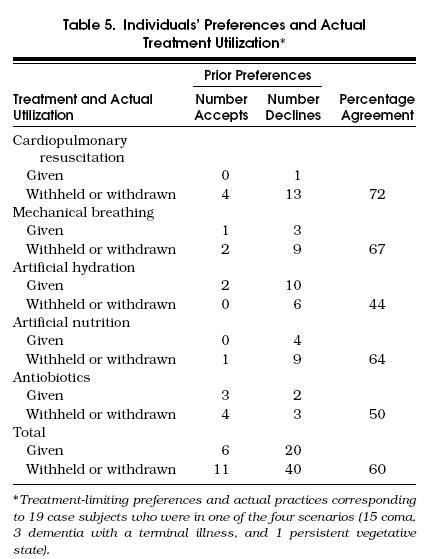
Treatments Received by Outpatients Who Entered a Described Scenario
Nineteen (4%) of the outpatients surveyed were eventually hospitalized at the study site and faced with one of the four scenarios. Fifteen cases subjects were classified as in coma with a small chance of recovery, three as having dementia with a terminal illness, and one was in a persistent vegetative state. Treatments given or limited are shown in Table 5 together with the patients' prior surveyed preferences. There were few indications for major surgery and hemodialysis in these patients.
Table 5.
Individuals' Preferences and Actual Treatment Utilization*
DISCUSSION
This study documents utilization patterns of a wide range of life-sustaining treatments and compares these practices with surveyed preferences for advance directive scenarios.
Patterns of withholding or limiting life-sustaining treatments exhibited wide variation. This wide variation contrasted with the relative homogeneity in patients' surveyed preferences and may reflect less discrimination between treatments among patients and members of the general public than among physicians.23–25 Cardiopulmonary resuscitation was usually withheld from patients, and artificial hydration was usually provided. Hemodialysis and mechanical breathing were withheld frequently, but withdrawn infrequently. These observations are consistent with those from other studies that indicate that withholding resuscitation is generally the first step in decisions to limit aggressive treatment, whereas intravenous fluids are forgone relatively rarely.26, 27
Although the observation that cardiopulmonary resuscitation was withheld more often than surveyed preferences would have dictated is consistent with other data, this finding may obscure the likelihood that many patients wanting no resuscitation receive it and many patients wanting resuscitation do not receive it.8, 28
Artificial hydration and antibiotics were given to patients more often than prior preferences would have directed. These findings are consistent with the view that physicians may find their administration routine and less subject to withdrawal or withholding.
These data are limited in that the surveyed patients are not the same as the observed inpatients. Nevertheless, given these limitations, these data do not support the common view that patients receive more intervention than they would wish. Three of the seven treatments investigated were withheld or limited at rates comparable to outpatients' and the public's surveyed preferences. The four for which practices and preferences differed were not consistent in the direction of either overtreatment or undertreatment.
Among the 19 subjects who later found themselves in surveyed scenarios, prior preferences and later treatments were often incongruent. Overtreatment and undertreatment patterns were approximately similar to the collective level, but correspondence of practices with individuals' wishes was poor for all treatments.
It is not yet clear what is required to attain congruence between individuals' prior preferences and practices. One possibility is that surveyed preferences may not be stable. However, a follow-up study of the same cohort of outpatients demonstrated reasonable stability.29 Another possibility is that family members or the physician may have been unaware of, or overrode the patient's preferences.7, 14, 15 Some patients may wish to allow their physicians latitude when acting on their preferences, as other commentators have suggested.30 These possibilities are best studied prospectively, as evidence of conflicting judgment is not often found in the medical record.
An important limitation of this study is the comparability of the chart-reviewed and surveyed patients, although the groups came from the same region and did not differ in sociodemographic characteristics. Another limitation is the use of scenarios, which may not capture all elements of patients' preferences.
This study challenges the common assumption that collectively treatments are not withheld or limited as much as patients would prefer. It does support the notion that, at least in the absence of advance directives, specific treatment practices deviate from individuals' prior preferences. An important implication of these findings is that if advance directives are regularly completed and followed, utilization of some treatments might increase, and others might decrease or remain the same. To improve congruence between preferences and practice, research and programs should target communication at the patient-proxy-physician level.
Acknowledgments
Supported by grants from the William F. Milton Fund and the Decamp Foundation.
The authors thank Susan Orb, Barbara Redman, and Melissa Bottrell for help with chart reviews; and Lynn Peterson, Gwendolyn Zahner, Gary Fischer, Janice Weinberg, Daniel Q. Naiman, , and Jennifer Chyet for their advice and suggestions.
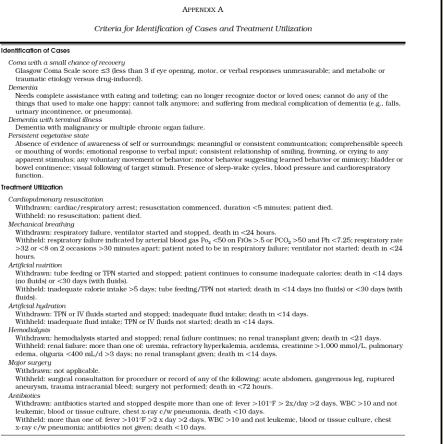
Appendix A
Criteria for Identification of Cases and Treatment Utilization
References
- 1.Kassirer JP. Adding insult to injury: usurping patients' prerogatives. N Engl J Med. 1983;308:898–901. doi: 10.1056/NEJM198304143081511. [DOI] [PubMed] [Google Scholar]
- 2.Renick O, Hanson S, Nelson M. Advance patient directives: are they worth it? Med Interface. 1994;7:149–52. [PubMed] [Google Scholar]
- 3.Weeks WB, Kofoed LL, Wallace AE, Welch HG. Advance directives and the cost of terminal hospitalization. Arch Intern Med. 1994;154:207–8. [PubMed] [Google Scholar]
- 4.Levinsky NG. The purpose of advance medical planning—autonomy for patients or limitation of care? N Engl J Med. 1996;335:741–3. doi: 10.1056/NEJM199609053351012. [DOI] [PubMed] [Google Scholar]
- 5.Callahan D. Controlling the costs of health care for the elderly—fair means, and foul. N Engl J Med. 1996;335:744–6. doi: 10.1056/NEJM199609053351013. [DOI] [PubMed] [Google Scholar]
- 6.Emanuel EJ, Emanuel LL. Proxy decision-making for incompetent patients: an ethical and empirical analysis. JAMA. 1992;267:2067–71. [PubMed] [Google Scholar]
- 7.Seckler AB, Meier DE, Mulvihill M, Paris BEC. Substitute judgement: how accurate are proxy predictions? Ann Intern Med. 1991;115:92–8. doi: 10.7326/0003-4819-115-2-92. [DOI] [PubMed] [Google Scholar]
- 8.Danis M, Southerland LI, Garrett JM, et al. A prospective study of advance directives for life-sustaining care. N Engl J Med. 1991;324:882–8. doi: 10.1056/NEJM199103283241304. [DOI] [PubMed] [Google Scholar]
- 9.Knaus WA and the SUPPORT investigators. A controlled trial to improve care for seriously ill hospitalized patients. JAMA. 1995;274:1591–8. [PubMed] [Google Scholar]
- 10.Fischer G, Alpert H, Stoeckle JD, Emanuel LL. Comparison of physician and patient choices and stability in the medical directive. J Gen Intern Med. 1994;9:93. [Google Scholar]
- 11.Gillick MR, Hesse K, Mazzapica N. Medical technology at the end of life—what would physicians and nurses want for themselves? Arch Intern Med. 1993;153:2542–7. [PubMed] [Google Scholar]
- 12.Solomon MZ, O'Donnell L, Jennings B, et al. Decisions near the end of life: professional views on life-sustaining treatments. Am J Public Health. 1993;83:14–23. doi: 10.2105/ajph.83.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Emanuel LL, Barry MJ, Stoeckle JD, Ettelson LM, Emanuel EJ. Advance directives for medical care—a case for greater use. N Engl J Med. 1991;324:889–95. doi: 10.1056/NEJM199103283241305. [DOI] [PubMed] [Google Scholar]
- 14.Zweibel NR, Cassel CK. Treatment choices at the end of life: a comparison of decisions by older patients and their physician-selected proxies. Gerontologist. 1989;29:615–21. doi: 10.1093/geront/29.5.615. [DOI] [PubMed] [Google Scholar]
- 15.Ouslander JG, Tymchuk AJ, Rahbar B. Health care decisions among elderly long-term care residents and their potential proxies. Arch Intern Med. 1989;149:1367–72. [PubMed] [Google Scholar]
- 16.Fried TR, Stein MD, O'Sullivan PS, Brock DW, Novack DH. Limits of patient autonomy: physician attitudes and practices regarding life-sustaining treatments and euthanasia. Arch Intern Med. 1993;153:722–8. doi: 10.1001/archinte.153.6.722. [DOI] [PubMed] [Google Scholar]
- 17.Caralis PV, Hammond JS. Attitudes of medical students, housestaff, and faculty physicians toward euthanasia and termination of life-sustaining treatment. Crit Care Med. 1992;20:683–90. doi: 10.1097/00003246-199205000-00023. [DOI] [PubMed] [Google Scholar]
- 18.Brennan TA. Ethics committees and decisions to limit care: the experience at the Massachusetts General Hospital. JAMA. 1988;260:803–7. [PubMed] [Google Scholar]
- 19.Emanuel L. The Health Care Directive: learning how to draft advance care documents. J Am Geriatr Soc. 1991;39:1221–8. [PubMed] [Google Scholar]
- 20.Miller RG., Jr . Simultaneous Statistical Inference. New York, NY: Springer-Verlag; 1981. [Google Scholar]
- 21.Huber PJ. The behavior of maximum likelihood estimates under non-standard conditions. In: LeCam LM, Heyman J, Scott EL, editors. Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability. Vol. 1. Berkeley: University of California Press; 1967. pp. 221–33. editors. [Google Scholar]
- 22.Fleiss JL. Statistical Methods for Rates and Proportions. 2nd ed. New York, NY: John Wiley and Sons; 1981. [Google Scholar]
- 23.Asch DA, Christakis NA. Why do physicians prefer to withdraw some forms of life support over others? Med Care. 1996;34:103–11. doi: 10.1097/00005650-199602000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Christakis NA, Asch DA. Medical specialists prefer to withdraw familiar technologies when discontinuing life-support. J Gen Intern Med. 1995;10:491–4. doi: 10.1007/BF02602399. [DOI] [PubMed] [Google Scholar]
- 25.Alpert HR, Hoijtink H, Fischer GS, Emanuel L. Psychometric analysis of an advance directive. Med Care. 1996;34:1057–65. doi: 10.1097/00005650-199610000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Faber-Langendoen K, Bartels DM. Process of forgoing life-sustaining treatment in a university hospital: an empirical study. Crit Care Med. 1992;20:570–7. doi: 10.1097/00003246-199205000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Smedira NG, Evans BH, Grais LS, et al. Withholding and withdrawal of life support from the critically ill. N Engl J Med. 1990;322:309–15. doi: 10.1056/NEJM199002013220506. [DOI] [PubMed] [Google Scholar]
- 28.Emanuel L. Structured deliberation to improve decisionmaking for the seriously ill. Hastings Center Rep. 1995;(25):S14–8. [PubMed] [Google Scholar]
- 29.Emanuel LL, Emanuel EJ, Stoeckle JD, Hummel LR, Barry MJ. Advance directives: stability of patients' treatment choices. Arch Intern Med. 1994;154:209–17. doi: 10.1001/archinte.154.2.209. [DOI] [PubMed] [Google Scholar]
- 30.Sehgal A, Galbraith A, Chesney M, Schoenfeld P, Charles G, Lo B. How strictly do dialysis patients want their advance directives followed? JAMA. 1991;267:59–63. [PubMed] [Google Scholar]