Abstract
OBJECTIVE
To assess the effect of a screen for problem drinking on medical residents and their patients.
DESIGN
Descriptive cohort study.
SETTING
Veterans Affairs Medical Clinic.
PATIENTS
Patients were screened 2 weeks before a scheduled visit (n=714). Physicians were informed if their patients scored positive.
MEASUREMENTS AND MAIN RESULTS
Physician discussion of alcohol use was documented through patient interview and chart review. Self-reported alcohol consumption was recorded. Of 236 current drinkers, 28% were positive for problem drinking by the Alcohol Use Disorders Identification Test (AUDIT). Of 58 positive patients contacted at 1 month, 78% recalled a discussion about alcohol use, 58% were advised to decrease drinking, and 9% were referred for treatment. In 57 positive patient charts, alcohol use was noted in 33 (58%), and a recommendation in 14 (25%). Newly identified patients had fewer notations than patients with prior alcohol problems. Overall, 6-month alcohol consumption decreased in both AUDIT-positive and AUDIT-negative patients. The proportion of positive patients who consumed more than 16 drinks per week (problem drinking) decreased from 58% to 49%. Problem drinking at 6 months was independent of physician discussion or chart notation.
CONCLUSIONS
Resident physicians discussed alcohol use in a majority of patients who screened positive for alcohol problems but less often offered specific advice or treatment. Furthermore, residents were less likely to note concerns about alcohol use in charts of patients newly identified. Finally, a screen for alcohol abuse may influence patient consumption.
Keywords: alcohol abuse, problem drinking, screening, brief interventions
A lcohol problems are a serious medical and public health issue. Ninety percent of U.S. adults currently drink or have drunk alcohol, and as many as 14% report a history of abuse or dependence.1 Alcohol is a major contributor to hospital and emergency department visits, accidents, and lost productivity.2–4 Trauma, usually of a greater severity and with a higher mortality, is increasingly associated with alcohol use.3, 5
Problem drinkers are patients whose pattern of alcohol consumption does not fulfill DSM-IV criteria for alcohol abuse or dependence but is characterized by a sufficiently large intake to have associated problems of health and social functioning.6 Problem drinkers develop minor medical problems that they present to primary care providers.7, 8 It is in this setting that early treatment of alcohol problems has been recommended.8 Results of previous studies provide evidence that simple and early intervention can persuade problem drinkers to reduce their intake to low-risk levels and use fewer medical resources.9–12
The U.S. Preventive Services Task Force has recommended screening for alcohol abuse by health care workers.13 However, primary care providers often fail to recognize alcohol problems especially in problem drinkers.14, 15 This failure has led to recent efforts focusing on improving the early detection of patients with alcohol problems by students, residents, and primary care providers.16–19
Identification of alcohol problems in primary care patients is a first step in dealing with this prevalent problem. Many physicians, however, feel they do not possess the skills necessary to initiate management in this setting.20–22 We were interested in how residents in a Veterans Affairs (VA) primary care clinic would respond when their patients screen positive with the Alcohol Use Disorders Identification Test (AUDIT), a screen for problem drinking as well as more severe alcohol problems. We also examined the impact of the program on their patients.
METHODS
Patients were recruited from the Pittsburgh/Oakland VA Medical Center, a major medical and surgical tertiary care center for Western Pennsylvania, Ohio, and West Virginia and a major teaching affiliate of the University of Pittsburgh. The Institutional Review Boards of both the Pittsburgh VA and the University of Pittsburgh approved the protocol. Before instituting the screening program, we obtained informed consent from residents to allow screening of their patients.
We randomly telephoned one of every four patients scheduled to see a second- or third-year internal medicine resident from April 1 through October 31, 1992, two weeks prior to their clinic visit. We included patients able to be contacted by telephone, who were planning to keep their appointment, and who were able to complete the interview. If the telephone service was disconnected, or if the patient could not be contacted after three attempts at three different times, then the interviewer proceeded to the next fourth patient in sequence. After each subject agreed to participate in the study, audiotaped informed consent was obtained.
From the 3,434 scheduled visits, we telephoned 779 veterans. Sixty-five (8.3%) of the patients refused to participate because they were unwilling to perform the telephone survey. We administered a lifestyle risk assessment that included the AUDIT, a measure of alcohol consumption, and other questions on lifestyle habits (smoking, exercise, and diet). The AUDIT is a 10-item questionnaire measuring alcohol consumption, dependence symptoms, and personal and social problems associated with alcohol misuse.23, 24 The AUDIT identifies a current, alcohol-related problem in patients who score 8 or more of a possible 40 points with a sensitivity of 96% and a specificity of 96%.25 We measured alcohol consumption by self-report asking separate questions for quantity and frequency in the consumption of beer, wine, and spirits. This method of reporting alcohol consumption possesses good agreement with other methods such as drinking diaries and allows for direct conversion to standard drinks (1.5 oz of spirits, 12 oz of beer, or 5 oz of wine).26
Patients were analyzed by degree of consumption in two ways. First, we classified patients as problem drinkers based on weekly consumption of more than 16 drinks per week as reported by Sanchez-Craig et al.27 This is similar to the 14 drinks per week recommended in the National Institute on Alcohol Abuse and Alcoholism guideline entitled The Physicians' Guide to Helping Patients with Alcohol Problems.28 We further subdivided patients as those who drank more or less than 35 drinks per week, which is the level of consumption used to validate the AUDIT screen.24
The principal investigator (JC) notified the residents of all AUDIT-positive patients through a letter placed on the chart at the time of the clinic appointment. The letter included information regarding the AUDIT. No information regarding study hypothesis was included. Sixty-one patients (94%) kept their clinic appointments, and only their data were used in the follow-up analyses. We interviewed 58 (91%) of the AUDIT-positive patients by telephone 1 month after the index clinic visit to assess whether any discussion of alcohol problems took place, if any intervention was planned, and if so, whether it was implemented. We resurveyed 215 (91%) of the original current drinkers by telephone at 6 months. We collected self-report data on number of emergency department visits, and number of inpatient hospital days over the last 6 months and also asked patients to specify if the visits or hospital days were alcohol related.
We reviewed patient charts to establish if an alcohol-related diagnosis existed prior to the index visit, and whether an alcohol problem and treatment were noted at the index visit. A patient was considered to have a history of alcohol-related diagnosis if there was any notation of alcoholism, alcohol abuse, or admission for an alcohol-related problem such as alcoholic hepatitis in the chart prior to the index visit. In addition, we searched the VA Patient Treatment File for diagnosis codes associated with alcohol in the last 5 years. Finally, we recorded the number of medical diagnoses in each problem list. Number of medications, gamma glutamyl transferase (GGT), hemoglobin, and mean corpuscular volume (MCV) measured over the past 2 years were obtained from a hospital computerized database.
Statistical Analyses
Differences in demographics, clinical factors, and drinking behavior between AUDIT-positive and AUDIT-negative drinkers, problem drinkers, and nonproblem drinkers, and those with and without a prior history of alcohol abuse were measured with χ2 for categorical variables and Mann-Whitney U tests for continuous measures. Comparisons across time were done with McNemar's test for categorical variables, Wilcoxon signed-rank, Friedman's test for continuous measures and repeated measures analysis of variance (ANOVA) of the ranks of total consumption across time. Nonparametric tests were used for measures of consumption because of the highly skewed nature of the data.
RESULTS
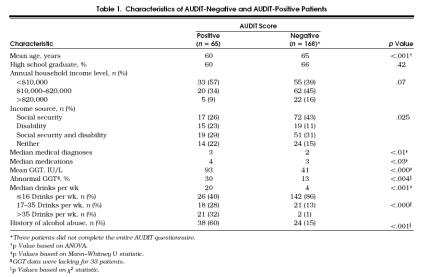
Of the 714 patients who completed the questionnaire, 236 (33%) reported current drinking. Sixty-five of the current drinkers (28%) were AUDIT-positive, representing 9% of those who completed the survey. Demographic and clinical characteristics of AUDIT-positive and AUDIT-negative patients are displayed in Table 1. Positive patients were younger, more often received disability income, had more medical comorbid conditions, were on more medications, and had higher GGT levels than negative patients. Thirty percent of patients in the positive group had GGT levels in the abnormal range (>64 IU/L) compared with 13% in the negative group. They also consumed more alcohol, were more likely to drink more than 16 drinks per week, and to have a prior alcohol-related diagnosis. At the 1 month interview, 45 (78%) of the AUDIT-positive patients recalled at least some discussion about alcohol by their physician at the index visit. Thirty-four (58%) of these patients specifically recalled being told to “cut down,” and 5 (9%) reported being referred for outside intervention. Chart review was possible for 57 (89%) of the positive patients. Residents noted the results of the screen of the current alcohol problem in 33 (58%) of these charts and a specific recommendation in 14 (25%) of the charts.
Tabel 1.
Characteristics of AUDIT-Negative and AUDIT-Positive Patients
A comparison of the patient reports and the physician notes was possible for 52 AUDIT-positive patients. There was agreement about the presence or absence of a discussion of alcohol problems in 37 (71%) of these patients. Patients were more likely to remember discussions than physicians were to note discussions (McNemar's test, p= .007). AUDIT-positive patients without previous notation of alcohol problems in the record recalled a discussion about alcohol less often than those with a prior diagnosis (61% vs 88%, χ2= 5.8, p < .05) and were less likely to have had a notation about alcohol abuse in the index visits (17% vs 86% χ2= 26.0, p < .0001). In a logistic regression with AUDIT-positive patients that considered previous mentioning of alcohol problems in the patient chart, number of medical diagnoses, patient age (>60 years), level of current drinking, patient GGT level, patient income, and education levels, only previous notation of an alcohol problem was a significant predictor of current notation (odds ratio [OR] 27.6; 95% confidence interval [CI] 6.6, 115.9).
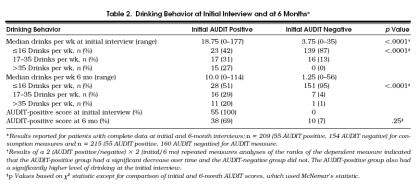
After 6 months, the median number of drinks per week decreased from 4.25 to 2.5 (ANOVA of the ranks, p < .0001) with the proportion of patients drinking more than 16 drinks per week decreasing from 23% to 17% (p= .01, McNemar's test) for all patients who were current drinkers.Table 2 compares patient drinking behavior over 6 months. Significant decreases in consumption were seen in AUDIT-positive patients (p < .0001, for the test of the interaction). The proportion of AUDIT-positive patients who were drinking in the problem drinking range decreased from 58% to 49% at the end of 6 months (McNemar's test, p= .33). AUDIT-negative patients also showed a nonsignificant decrease in their consumption with median number of drinks decreasing from 3.75 drinks per week initially to 1.75 drinks per week at the 6-month interview. The 16 patients who were AUDIT-negative but reported consuming more than 16 drinks per week at enrollment showed a significant decrease in consumption over the 6-month period from a median of 21 drinks per week to 6 drinks per week (p= .0012).
Tabel 2.
Drinking Behavior at Initial Interview and at 6 Months*
The first three AUDIT questions deal specifically with the frequency and quantity of alcohol consumption. When the responses to these questions were studied across time, they indicated that the frequency of drinking decreased slightly for all levels of frequency but quantity of alcohol consumed on each occasion decreased for the lighter drinkers (≤4 drinks per occasion) more than for heavier drinkers (>4 drinks per occasion). On the question of how often 6 or more drinks are consumed, more of those who reported fewer incidents (less than once a month) initially reported a decrease at 6 months than those who initially reported more incidents (once a month or more).
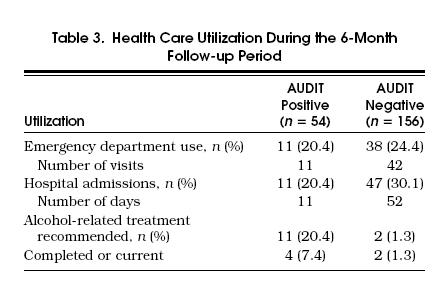
For AUDIT-positive patients, there were no univariate relations between physician notation or patient recall of alcohol discussion and subsequent decreases in consumption. When initial AUDIT status, initial problem drinking status, number of comorbid medical and psychiatric illnesses, previous history of alcohol-related problems, patient recall of advice to decrease drinking, or physician notation of alcohol problem and total quantity of alcohol consumed at enrollment were used in a multivariate logistic regression to model 6-month problem drinking status, only initial AUDIT (OR 8.1; 95% CI 3.0, 21.5) and initial consumption of more than 16 drinks per week (OR 8.8; 95% CI 3.3, 23.6) were significant. When only AUDIT-positive patients were used in the same multivariate model, only the measure of total quantity consumed at enrollment was a significant predictor. As shown in Table 3, there were no differences related to initial AUDIT status in emergency department use or hospital admissions at the 6-month follow-up.
Tabel 3.
Health Care Utilization During the 6-Month Follow-up Period
DISCUSSION
We found that a majority of AUDIT-positive patients recalled a discussion about alcohol problems by their resident physician. The majority of the discussions consisted of advice to decrease use and much less often involved a specific recommendation for more traditional treatment. Nevertheless, there appeared to be a modest reduction in patient alcohol consumption over 6 months.
Our finding of a 78% discussion rate in screen-positive patients was comparable to that in a previous study. Schorling et al. screened patients of categorical internal medicine, primary care internal medicine, and family medicine residents for alcohol abuse using the Michigan Alcoholism Screening Test and showed that 60% to 80% of positive patients recalled a discussion of alcohol abuse by their physician in the past year.29 In our study, resident intervention consisted mostly of advice to “cut down” in 58% of AUDIT-positive patients, but referral to other therapy occurred in less than 25%. This finding is lower than that found in the inpatient setting, where Moore noted that when the diagnosis of alcohol abuse was made, treatment was instituted 50% to 75% of the time.30 If outpatients are more likely problem drinkers, then they may lack clinical evidence of an alcohol-related problem and physicians might be less likely to offer other, more intensive traditional treatment.
Newly diagnosed patients in our study were less likely to recall a discussion, and physicians were less likely to note an alcohol-related problem. These patients may be problem drinkers who lack the “clinical” evidence of an alcohol-related problem. In a similar study, Buchsbaum et al. administered the alcohol module of the Diagnostic Interview Schedule to patients in a medical clinic at an urban university teaching hospital staffed by interns and residents and studied patient and physician characteristics that influence detection of problem drinking.15 Resident physicians, unaware of the interview results, noted alcohol problems in the chart of 49% of patients who met criteria for current alcohol abuse or dependence. Previous medical record reference of alcohol problems, number of concurrent medical problems, patient gender, and gastrointestinal problems were associated with detection of alcohol problems by residents. Our notation rate of 58% resulted when physicians were made aware of a current problem. We also found that prior medical record notation was the strongest predictor of current notation in the chart. The association of prior medical record notation in both studies support the theory that residents depend on prior labeling with alcohol diagnoses in making current alcohol-related diagnoses.
Six months after screening, patients reported a decrease in alcohol consumption and were less likely to drink in the problem range. This was due primarily to decreased consumption among the AUDIT-positive group and problem drinkers. However, screen-positive patients who recalled a discussion about alcohol with their doctor or for whom physicians made a note in the chart had a similar decrease in their alcohol consumption compared with those without a reported discussion or notation. The rate of utilization of alcohol-related and non-alcohol-related health care services was low in all patients and did not explain the decrease in consumption.
These overall findings suggest that a simple screening program may act as a brief intervention for problem drinkers. A simple screen or reminder has been shown to reduce consumption and adverse outcomes from drinking in a number of studies.31 Wallace et al., screening general practitioners' practices, found an overall reduction of 24% in the proportion of patients who reported excessive levels of consumption at 12 months.10 Most recently, Fleming et al. reported a 20% reduction in alcohol use among control patients in a study evaluating the efficacy of brief physician advice in reducing alcohol use and health care utilization in problem drinkers.12 Patients in our study who were AUDIT-negative but consumed alcohol in the problem range also had a significant decrease in their consumption although we did not specifically identify them to their physicians. The reasons for these reductions include regression to the mean, historical changes in alcohol use, and the intervention effect of the screen and the data collection procedures independent of physician involvement.
There are several limitations to our study. First, the patient sample was derived from a single VA hospital, which may limit the generalizability of our results. Veterans may possess unique medical and psychosocial comorbidities that increase the prevalence of alcohol problems or make their diagnosis difficult to establish. Our prevalence, although low, is in the range of earlier studies, as is our rate of physician recognition.14, 28 Our lower rate of alcohol problems and higher rate of nondrinkers may be a reflection of the older age of our population. Patients who were heavier drinkers may have succumbed from complications associated with drinking or other comorbid conditions. Residents cared for the patients in our study so these results may not be applicable to other health care providers. The issue of alcohol abuse and early treatment, however, should be more salient during training and thus resident rates of discussion might be higher than with physicians in practice. Residents are also caring for fewer patients per clinical session.
We used a quantity-frequency method to assess average level of consumption. Such methods may underestimate consumption especially when patients have days of excessive or heavy alcohol use that deviate substantially from their average daily consumption.32 However, when average consumption was sought, this method produced results similar to those of a study using a more sensitive time-line method.32 Finally, we used a telephone-based screen that may have biased patient responses. Prior comparisons between telephone interviews and face-to-face interviews found that women tended to underreport consumption in face-to-face interviews, but no difference was seen in men.33
Despite these limitations, we believe our study has important implications. First, we showed that given the knowledge of a positive alcohol screen, residents discussed alcohol problems in a majority of patients, however, this occurred less often for patients without a prior history of alcohol abuse. Second, a simple screen for alcohol problems may be enough of an intervention to decrease alcohol consumption in patients. This last finding contributes to the growing body of literature supporting the importance of a brief intervention. Given these findings, clinic directors should consider implementing a systematic screening program to identify alcohol problems and decrease overall drinking rates in their patients.
Acknowledgments
The authors thank Jeff Whittle, MD, MPH, for providing data from the VA Patient Treatment File and Jeannette Gibbon for performing the interviews.
References
- 1.Robins LN, Helzer JE, Weissman MM, et al. Lifetime prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry. 1984;41:949–58. doi: 10.1001/archpsyc.1984.01790210031005. [DOI] [PubMed] [Google Scholar]
- 2.Adams WL, Yuan Z, Barboriak JJ, Rimm AA. Alcohol-related hospitalization of elderly people. JAMA. 1993;270:1222–5. [PubMed] [Google Scholar]
- 3.Jurkovich GJ, Rivara FP, Gurney JG, et al. The effect of acute alcohol intoxication and chronic alcohol abuse on outcome from trauma. JAMA. 1993;270:51–6. [PubMed] [Google Scholar]
- 4.Harford TC, Parker DA, Grant BF, Dawson DA. Alcohol use and dependence among employed men and women in the United States in 1988. Alcohol Clin Exp Res. 1992;16:146–8. doi: 10.1111/j.1530-0277.1992.tb01357.x. [DOI] [PubMed] [Google Scholar]
- 5.Evans L. The fraction of traffic fatalities attributable to alcohol. Accid Anal Prev. 1990;22:587–602. doi: 10.1016/0001-4575(90)90030-o. [DOI] [PubMed] [Google Scholar]
- 6.Rinaldi RC, Steindler EM, Wilford BB, Goodwin D. Clarification and standardization of substance abuse terminology. JAMA. 1988;259:555–7. [PubMed] [Google Scholar]
- 7.Sobell LC, Sobell MB. Problem Drinkers. New York, NY: The Guilford Press; 1993. [Google Scholar]
- 8.Institute of Medicine . Broadening the Base of Treatment for Alcohol Problems. Washington, DC: National Academy Press; 1990. [PubMed] [Google Scholar]
- 9.Chick J. Brief interventions for alcohol misuse: effective, but not for all alcohol misusers. BMJ. 1993;307:1374. doi: 10.1136/bmj.307.6916.1374. Editorial. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wallace P, Cutler S, Haines A. Randomized controlled trial of general practitioner intervention in patients with excessive alcohol consumption. BMJ. 1988;297:663–8. doi: 10.1136/bmj.297.6649.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson P, Scott E. The effect of general practitioners' advice to heavy drinking men. Br J Addict. 1992;87:891–900. doi: 10.1111/j.1360-0443.1992.tb01984.x. [DOI] [PubMed] [Google Scholar]
- 12.Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers: a randomized controlled trial in community-based primary care practices. JAMA. 1997;277:1039–45. [PubMed] [Google Scholar]
- 13.U.S. Preventive Services Task Force. Screening for alcohol and other drug abuse . In: Guide to Clinical Preventive Services: An Assessment of the Effectiveness of 169 Interventions. Report of the U.S. Preventive Services Task Force. Fisher M, editor. Baltimore, Md: Williams and Wilkins; 1989. pp. 277–86. [Google Scholar]
- 14.Coulehan JL, Zettler-Segal M, Block M, McClelland M, Schulberg HC. Recognition of alcoholism and substance abuse in primary care patients. Arch Intern Med. 1987;147:349–52. [PubMed] [Google Scholar]
- 15.Buchsbaum DG, Buchanan RG, Poses RM, Schnoll SH, Lawton MJ. Physician detection of drinking problems in patients attending a general medicine practice. J Gen Intern Med. 1992;7:517–21. doi: 10.1007/BF02599456. [DOI] [PubMed] [Google Scholar]
- 16.Screening. In: Eighth Special Report to the U.S. Congress on Alcohol and Health. Rockville, Md: Dept. of Health and Human Services; 1993. pp. 297–311. NIH Publication 94-3699. [Google Scholar]
- 17.Graham AW. Screening for alcoholism by life-style risk assessment in a community hospital. Arch Intern Med. 1991;151:958–64. [PubMed] [Google Scholar]
- 18.Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA. 1984;252:1905–7. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 19.Bush B, Shaw S, Cleary P, Delbanco TL, Aronson MD. Screening for alcohol abuse using the CAGE questionnaire. Am J Med. 1987;82:231–5. doi: 10.1016/0002-9343(87)90061-1. [DOI] [PubMed] [Google Scholar]
- 20.Rohman ME, Cleary PD, Warburg M, Delbanco TL, Aronson MD. The response of primary care physicians to problem drinkers. Am J Drug Alcohol Abuse. 1987;13:199–209. doi: 10.3109/00952998709001509. [DOI] [PubMed] [Google Scholar]
- 21.Rush B, Bass M, McCracken E, LaBreque M, Bondy S. Detecting, preventing, and managing patients' alcohol problems. Can Fam Physician. 1994;40:1557–66. [PMC free article] [PubMed] [Google Scholar]
- 22.Rush B, Ellis K, Crowe T, Powell L. How general practitioners view alcohol abuse: clearing up the confusion. Can Fam Physician. 1994;40:1570–9. [PMC free article] [PubMed] [Google Scholar]
- 23.Babor TF, De La Fuente, JR, Saunders J, Grant M. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care. Geneva, Switzerland: World Health Organization; 1989. [Google Scholar]
- 24.Saunders JB, Aasland OG, Babor TF, Fuente De La, JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 25.Isaacson JH, Butler R, Zacharek M, Tzelepis A. Screening with the Alcohol Use Disorders Identification Test (AUDIT) in an inner city population. J Gen Intern Med. 1994;9:550–3. doi: 10.1007/BF02599279. [DOI] [PubMed] [Google Scholar]
- 26.Flegal KM. Agreement between two dietary methods in reported intake of beer, wine, and liquor. J Stud Alcohol. 1991;52:174–9. doi: 10.15288/jsa.1991.52.174. [DOI] [PubMed] [Google Scholar]
- 27.Sanchez-Craig M, Wilkinson DR, Davilla R. Empirically based guidelines for moderate drinking: one year results from three studies with problem drinkers. Am J Pub Health. 1995;85:823–8. doi: 10.2105/ajph.85.6.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bethesda, Md: National Institute on Alcohol Abuse and Alcoholism; NIH publication; 1995. The Physicians' Guide to Helping Patients with Alcohol Problems; pp. 95–3769. [Google Scholar]
- 29.Schorling JB, Klas PT, Willems JP, Everett AS. Addressing alcohol use among primary care patients: differences between family medicine and internal medicine residents. J Gen Intern Med. 1994;9:248–54. doi: 10.1007/BF02599649. [DOI] [PubMed] [Google Scholar]
- 30.Moore RD, Bone LR, Geller G, Mamon JA, Stokes EJ, Levine DM. Prevalence, detection, and treatment of alcoholism in hospitalized patients. JAMA. 1989;261:403–7. [PubMed] [Google Scholar]
- 31.Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction. 1993;88:315–36. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- 32.Sobell LC, Cellucci T, Nirenberg TD, Sobell MB. Do quantity-frequency data underestimate drinking-related health risks? Am J Public Health. 1982;72:823–8. doi: 10.2105/ajph.72.8.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hochstim JR. Comparison of three information-gathering strategies in a population study of sociomedical variables. Proc Soc Stat Sect Am Stat Assoc. 1962:154. [Google Scholar]