Abstract
OBJECTIVE
To assess the long-term impact of headache on labor force participation among primary care patients with headache.
DESIGN
A 2-year cohort study comparing employment status of primary care patients with headache and that of patients with back pain.
PARTICIPANTS
Patients with headache (n=662) or back pain (n=1,024) sampled from persons visiting a primary care physician who completed baseline, 1-year and 2-year follow-up interviews.
MEASUREMENTS AND MAIN RESULTS
The percentage of subjects unemployed at baseline, 1 year or 2 years was determined, excluding the retired and homemakers. Among all patients, the percentage unable to obtain or keep full-time work in the year prior to each interview because of headache or back pain was also assessed. Over the 3-year period covered by the study interviews, 13% of headache and 18% of back pain patients were unable to obtain or keep full-time work because of their pain condition. Among those in the labor force, 12% of headache patients and 12% of back pain patients were unemployed for any reason at one or more interviews. Among the one in five headache patients with a poor long-term outcome, 36% were unable to obtain or keep full-time work because of headache at some time compared with 4% of headache patients with a good outcome. Among headache patients, women, persons aged 18 to 24 years, those with lower levels of education, persons with depressive symptoms, and migraineurs were more likely to have reduced labor force participation owing to headache.
CONCLUSIONS
The likelihood of reduced labor force participation among primary care patients with headache was considerable and concentrated among the one in five patients with a poor long-term outcome. Headache patients at a social disadvantage in attaining occupational role stability (e.g., younger women or poorly educated patients) were more likely to report reduced labor force participation.
Keywords: migraine; headache, epidemiology; back pain, epidemiology; unemployment; outcomes
Headache is one of the most common pain conditions in the general population,1, 2 and among the most common conditions seen by providers of ambulatory medical care.3, 4 Because mild, transient headache is a nearly universal experience, differentiating headache's more debilitating forms is essential in assessing its public health significance. Epidemiologic surveys on headache have consistently identified a subset of sufferers who are adversely affected,5–8 but prior research has not described the long-term effect of headache on the performance of major social roles, such as occupation. Understanding the significance of headache as a public health problem requires information concerning its impact on work role disability that is not provided by statistics from worker's compensation programs because headache is rarely identified as a compensatable cause of work disability.
The objectives of this report are to compare reduced labor force participation of primary care headache patients with that of primary care back pain patients; and to identify the characteristics of headache patients at high risk of reduced participation in the labor force. Back pain data will be presented for comparison throughout to give context to the findings in headache patients.
METHODS
Setting and Sample
The methods and description of the study population have been published in detail elsewhere.9 The setting for this research was Group Health Cooperative of Puget Sound (GHC), a Seattle area staff-model health maintenance organization with more than 350,000 enrollees. The majority (85%) of GHC enrollees receive their benefits through their employer, while about 12% of GHC enrollees have purchased family coverage on their own. Compared with other Seattle area residents, GHC enrollees have slightly higher educational attainment but are quite similar in age, gender, racial/ethnic composition, and marital status; GHC enrollees also have similar median income but are less representative of the extremes of income distribution. Differences between the U.S. population and GHC enrollees (fewer African Americans, higher education level at GHC) reflect primarily the differences between the demographics of the GHC catchment area population and the U.S. general population.
Patients visiting participating GHC primary care physicians during 1989 and 1990 for headache or back pain were eligible if they were between the ages of 18 and 75 and had been continuously enrolled at GHC for at least 1 year. Patients were excluded if they planned to disenroll or did not have a telephone. Reason for visit was ascertained from the clinic's appointment log or an encounter form completed by the provider. Visits to emergency department and walk-in facilities were excluded. Thus, the resulting sample was a cross section of headache and back pain patients seen by primary care physicians over a 1-year period, including acute, recurrent, and chronic cases, irrespective of diagnosis.
Data Collection
Three to 6 weeks after the index visit, subjects were contacted and asked to participate in a 30-minute telephone interview. Baseline interviews were conducted for 779 headache patients (78% of eligible) and 1,213 back pain patients (72% of eligible). Twenty-minute follow-up interviews were carried out by telephone 1 year and 2 years later. Patients provided informed consent for all interviews and for abstraction of medical records.
Study Measures
Pain Outcome Assessment
Outcome of headache and of back pain was assessed using a simple, empirically derived and validated grading system.9 At each interview, severity was graded into the following classes: grade 0, no pain in the prior 6 months; grade I, low disability–low intensity pain; grade II, low disability–high intensity pain; grade III, moderate interference with activities; grade IV, severe interference with activities. Grading was based on ratings from 0 to 10 of pain intensity (pain right now, average pain, and worst pain), three ratings from 0 to 10 of interference with activities as a result of pain in daily activities, work activities, and family/social/recreational activities, and the number of days the person was unable to carry out usual activities because of pain in the prior 6 months. The persistence of headache was assessed by the number of days the patient reported having headache in prior 6 months.
Classification of Outcome
Outcomes were classified as good, mixed/fair, or poor according to the following criteria:
Good outcome. Patients reporting low intensity pain (grade I), or who were pain-free (grade 0), at both the 1- and the 2-year follow-up were classified as having a good outcome.
Poor outcome. Patients with moderate to severe pain dysfunction (grades III and IV as defined above) on both of the two follow-up interviews were classified as having a poor outcome, as were patients with moderate to severe pain dysfunction on one of the follow-up interviews and high intensity pain (grade II) on the other.
Mixed or fair outcome. Patients who were placed at grades II–V on one of the follow-up interviews and at grade 0–I on the other were classified as having a mixed outcome, as were those at grade II for both follow-up interviews.
Depressive Symptoms
Depressive symptoms were measured using the depression and vegetative symptom items from the Symptom Checklist 90.10 According to prior GHC data providing population norms,2 persons with a mean raw score of 1.10 or higher were classified as depressed.
Unemployment
Unemployment rates were estimated after excluding persons who were retired or keeping house at every interview. Full-time students were considered employed for this analysis. Persons who reported that they were currently unable to work, unemployed, or looking for work were considered unemployed. Subjects were also asked if they felt that they had been unable to obtain or keep full-time work during the past year specifically because of their headache or back pain.
Headache and Back Pain Diagnosis
Headache diagnoses were derived by algorithm from a fully structured headache questionnaire,11 inclusive of International Headache Society criteria.12 Migraine was defined as headache of unilateral location and pulsating character associated with nausea, vomiting, or photophobia. Migraine headaches with and without aura were differentiated, where aura were defined by spots, lines, or heat waves affecting one or both visual fields before or during a headache. Tension-type headache was defined by bilateral pain with a band-like character. Patients meeting criteria for neither migraine nor tension headache were classified as “other.” According to the resulting diagnostic classification, patients were assigned to one of the following categories: migraine with aura, migraine with tension-type headache only, migraine only, tension-type headache only, and other. Migraine with aura subjects included those with coexisting tension headache. Back pain subjects were defined as any who had made a primary care visit with a complaint of back pain during the enrollment period. There were no exclusions based on the location of the pain (e.g., cervical pain); however, a small number of patients receiving a diagnosis of kyphosis, scoliosis, lordosis, instability, or alignment disorders (n= 27) were excluded.
Statistical Analysis
Only the 662 headache and 1,024 back pain patients with data from all three interviews were included in the analyses reported here. Rates of unemployment across all three waves were compared for patient groups differing in social and clinical variables by χ2 tests (two-sided test with α = 0.05). Variables found to be associated with unemployment in the analysis were considered for inclusion in a multivariate model. These analyses were performed using SAS statistical software (Version 6, 4th ed., 1989; SAS Institute, Inc., Cary, N.C.). Using epidemiologic software (EGRET, 1990; Statistics and Epidemiology Research Corporation, Seattle, Wash.), multivariate analyses were conducted using logistic regression to assess the independent contribution of patient characteristics to unemployment rates while controlling for the effect of the other variables in the model; a likelihood ratio test was performed for each (class) variable.
RESULTS
Response Rates
Baseline interviews were completed by 779 primary care headache patients and 1,213 back pain patients. Follow-up was sought for patients who did not die, become too ill to be interviewed, or move out of the country. One- and 2-year follow-up interviews were completed by telephone with 662 (85%) of the headache patients and 1,024 (84%) of the back pain patients. Of the 779 headache subjects at the baseline visit, 117 were lost to follow-up over 2 years: for 66, the telephone number was not working, only an answering machine was reached, or attempts at recontacting were unsuccessful, 34 refused to comment, 7 moved out of the country, 6 died, 3 were too ill, and 1 subject had language or hearing difficulty. There was no significant difference between those who completed the 2 years of follow-up versus those who did not in the rate of unemployment (5.85% vs 4.21%, χ2 = 0.41, df= 1, p= .523) or the rate of being unable to obtain or keep full-time work (5.89% vs 5.13%, χ2 = 0.11, df= 1, p= .744). The distribution was similar among back pain patients lost to follow-up.
Patient Characteristics
The characteristics of headache patients and back pain patients completing all three study interviews were provided in Table 1). Most patients with headache were between the ages of 25 and 44, were female, and had attended at least some college. Those with back pain were slightly older with approximately equal proportions of men and women. The relatively high educational attainment of the study patients is characteristic of GHC's enrollment.13
Table 1.
Table Characeristicsof the Study Patients Interviewed at Baseline, 1-Year, and 2-Year Follow-ups
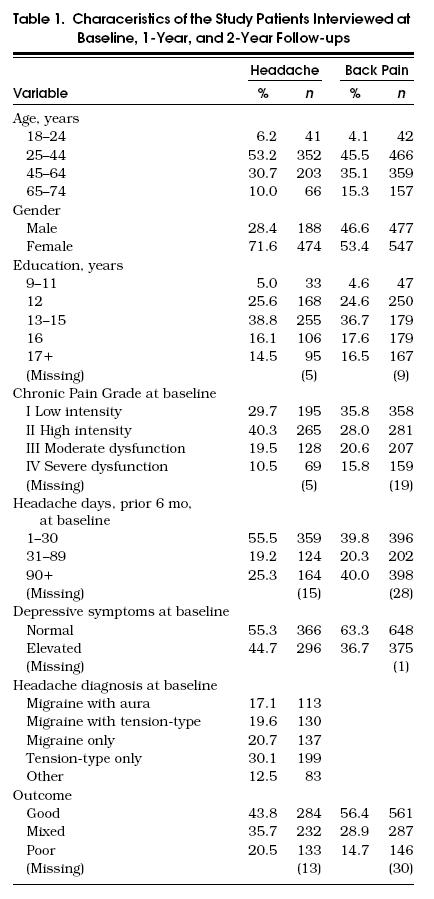
Approximately one in three headache and back pain patients were graded as having moderate to severe pain-related disability (grade III–IV) at baseline. Back pain tended to be more persistent than headache—back pain patients were more likely to report pain on 90 or more days in the prior 6 months than headache patients. The percentage of headache patients with elevated levels of depressive symptoms was greater than observed among the back pain patients, but a large minority of both groups showed elevated depression scores. At baseline, more than half of the headache subjects met criteria for migraine headache (with or without aura or co-occurring tension-type headache), while another 30% met criteria for tension-type headache in the absence of migraine.
Headache and Back Pain Outcomes
Among the primary care headache patients interviewed on all three occasions, one in five had a poor outcome, while two in five had a good outcome (Table 1). Among the primary care back pain patients, approximately one in seven had a poor outcome, while more than half had a good outcome.
Unemployment
For both back pain and headache patients, 12% were unemployed on one or more of the three interviews, excluding from the denominator those retired or keeping house (Table 2. Among patients with a poor long-term outcome, 25% of headache patients and 38% of back pain patients reported being unemployed at one or more interviews.
Table 2.
Reduced Labor Force Participation Over Baseline, 1-Year, and 2-Year Interviews Among Patients Seeking Primary Care for Headache or for Back Pain by Long-Term Outcome
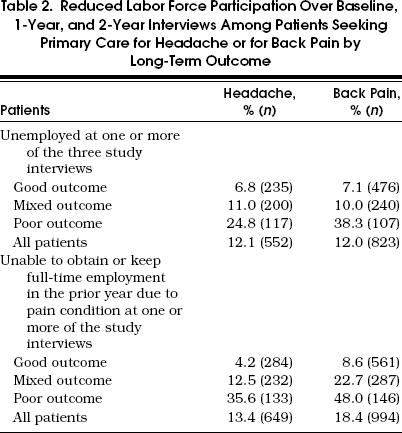
Thirteen percent of the headache patients overall felt they were unable to obtain or keep full-time work on one or more of the study interviews because of their headache (Table 2). However, among headache patients with a poor outcome, 36% reported being unable to obtain or keep full-time work because of headache, compared with 4% of those with a good outcome. Among back pain patients, 18% of all patients, and 48% of those with a poor outcome, reported being unable to obtain or keep full-time work owing to back pain. Because the definition of “poor outcome” incorporates measures of patient functioning, it is not surprising that patients with a poor outcome have reduced labor force participation.
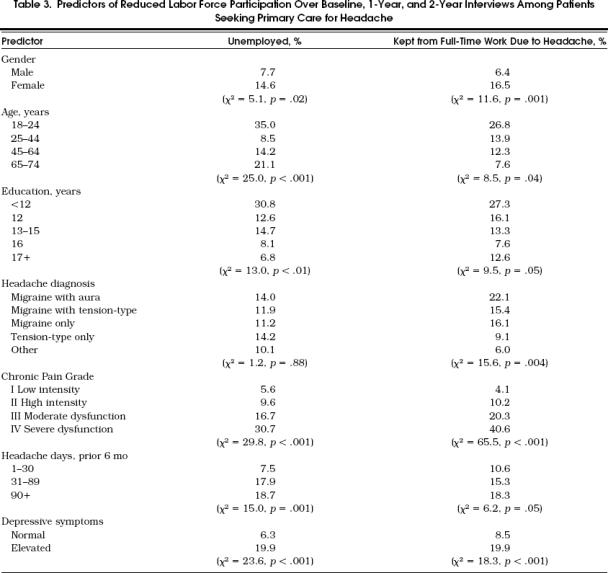
Among primary care headache patients (Table 3), women, younger persons, and persons with lower levels of education were more likely to be unemployed during the study period. Age, gender, and education were also associated with headache-related difficulty in obtaining or keeping full-time work. Headache diagnosis was not a significant predictor of unemployment for any reason, but patients meeting diagnostic criteria for migraine were almost twice as likely as nonmigraine headache patients to report that they were unable to obtain or keep full-time work because of their headache. As might be expected, chronic pain grade (a composite measure of pain intensity and disability) and number of headache days were strong predictors of unemployment rates (Table 3). Headache patients with high levels of depressive symptoms were more than twice as likely to be unemployed and kept from fulltime work by headache than nondepressed patients.
Table 3.
Predictors of Reduced Labor Force Participation Over Baseline, 1-Year, and 2-Year Interviews Among Patients Seeking Primary Care for Headache
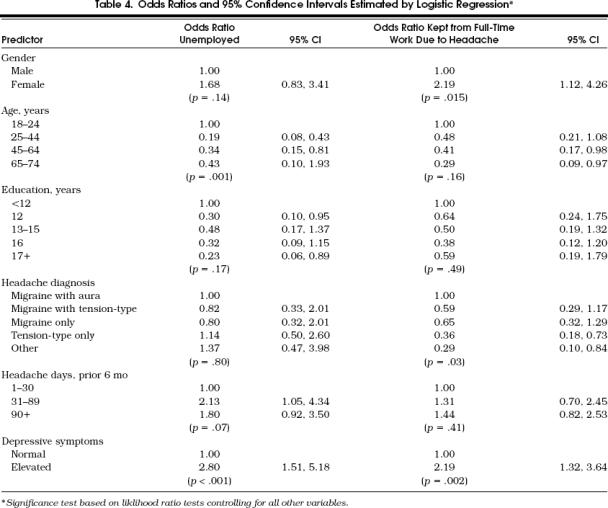
The results of the logistic regression model are reported in Table 4, with the odds ratios for each level of the variables included in the model. Chronic pain grade was not included as a predictor in these multivariate analyses because it incorporates measures of work role disability. In the multivariate analyses of unemployment, age and depressive symptoms emerged as highly significant predictors, while number of headache days was of borderline significance. Female gender, headache diagnosis, and depressive symptoms were significant predictors of being unable to obtain or keep full-time work because of headache.
Table 4.
Odds Ratios and 95% Confidence Intervals Estimated by Logistic Regression*
DISCUSSION
Recent studies of work disability among headache patients have found that persons with severe headache contribute a large number of lost work days. However, the impact of headache on labor force participation has not been extensively studied. In this sample, the unemployment rate and the extent of being unable to obtain or keep full-time work among headache patients approached those reported by back pain patients. This is surprising as headache, especially migraine, is an intermittent disorder while back pain is more persistent. Among the one in five primary care headache patients with a poor long-term outcome, the risks of unemployment were substantial. This suggests the need for further research to understand the extent, causes, and amelioration of work-role disability among primary care headache patients with a poor outcome.
Pain can impair work performance through its impact on physical capacities such as the ability to lift, to walk, to sit, or to perform movements required by a work task. Pain can also impair work performance through its effects on cognitive, emotional, and interpersonal capacities required to be effective at work such as concentration, motivation, energy, and ability to engage in positive interaction with others. In addition, migraine can impair work through specific symptoms that interfere with work task performance, such as nausea and vomiting. Unfortunately little is known about the specific cognitive, emotional, and interpersonal capacities that are affected by severe headache in the work setting and how they interfere with performance of work role. Given the strong association of poor headache outcome with reduced labor force participation, more information on the work impairments associated with headache is needed.
Social characteristics most strongly associated with reduced labor force participation as a result of headache included young age, female gender, and lower levels of education. The presence of a severe headache disorder may exacerbate difficulties in attaining stable labor force participation among persons at social disadvantage in the labor force for other reasons (e.g., young age, female gender, low levels of education). Epidemiologic studies have reported a higher prevalence of migraine among subjects of lower socioeconomic status.6, 7 It has been proposed that the effects of severe headache may produce a downward drift in social status and an inability to earn a consistent income. As problems in obtaining and keeping full-time work because of headache were most often reported by the young, the female, and the less well educated, hypothesis that severe headache has the potential for a long-lasting adverse effect on social status and income deserves further study. Few headache patients in this study reported seeking or obtaining worker's compensation for headache. This study was not designed to test causal hypotheses about the determinants of reduced labor force participation among headache patients, but these high-risk patients deserve further study.
The study patients were consecutive pain patients, not a cohort of patients seeking treatment for the first time. A cohort of patients identified at the inception of illness, or the inception of treatment, would most likely have more favorable outcomes than the consecutive pain patients enrolled in this study. At the same time, this study was conducted in an HMO serving a relatively highly educated and typically employed population. In a more socially disadvantaged population, the extent of reduced labor force participation among persons of a poor headache outcome could be greater.
In part of this analysis, we relied on patients' attributions of the relation between difficulty obtaining or keeping full-time work and their headache. It is possible that work difficulties, or underlying psychosocial problems that impair work performance, cause or exacerbate a headache disorder. Although this possibility deserves research attention, the perceptions of persons experiencing work difficulties should not be dismissed. The widely held assumption that headaches were caused by underlying psychosocial conflicts or psychological disorder is an unproven hypothesis. It is plausible that psychological distress and difficulties in work role performance are directly caused by a headache disorder. It is also possible that severe, chronic headache and psychosocial problems are mutually reinforcing.
The results of this study are consistent with prior research indicating that severe, chronic headache may significantly affect the economic productivity and quality of life of afflicted persons. The risk of reduced labor force participation doubled with each increase in level of pain-related disability as reflected in the Chronic Pain Grade, a relation that persisted across unemployment in general and headache-specific unemployment. Although number of headache days was a strong risk indicator of unemployment in our model, headache diagnosis was a stronger risk indicator of headache-related labor difficulty. Further research is needed to clarify the specific effects of chronicity and diagnostic signs and symptoms on labor force participation. Given the significant effects of loss of employment on household income, access to medical insurance, family functioning, and personal self-esteem, the impact of headache on employment status merits further study.
In conclusion, the one in five primary care headache patients with a poor outcome are at substantial risk of reduced labor force participation. Given that headache is among the most common reasons for visiting primary care physicians, the development and evaluation of interventions appropriate for primary care to improve psychosocial functioning and sustain labor force participation among patients with severe, disabling headache deserves increased attention. Improving functional outcomes of primary care headache patients is a public health concern deserving attention commensurate with the extent of work role disability in this patient population.
Acknowledgments
Supported by grants from the Agency for Health Care Policy and Research (RO1 HS06168) and the National Institute of Dental Research (PO1 DE08773), and Glaxo Research Institute. The contributions of Kathleen Saunders to this research are gratefully acknowledged.
REFERENCES
- 1.Sternbach RA. Survey of pain in the United States: the Nuprin pain report. Clin J Pain. 1986;2:49–53. doi: 10.1016/0304-3959(86)90224-1. [DOI] [PubMed] [Google Scholar]
- 2.Von Korff M, Dworkin SF, Le Resche L, Kruger A. An epidemiologic comparison of pain complaints. Pain. 1988;32:173–83. doi: 10.1016/0304-3959(88)90066-8. [DOI] [PubMed] [Google Scholar]
- 3.American Academy of Family Physicians . Kansas City, Kan: American Academy of Family Physicians; 1987. Facts About: Family Practice. [Google Scholar]
- 4.Schappert SW. National Ambulatory Medical Care Survey: 1989 Summary. National Center for Health Statistics. Vital Health Stat. 1992;13:110. [PubMed] [Google Scholar]
- 5.Osterhaus JT, Gutterman DL, Plachetka JR. Health care resource use and lost labour costs of migraine headache in the US. Pharmaco-Economics. 1992;2(1):67–76. doi: 10.2165/00019053-199202010-00008. [DOI] [PubMed] [Google Scholar]
- 6.Stang PE, Osterhaus JT. Impact of migraine in the United States: data from the National Health Interview Survey. Headache. 1993;33:29–35. doi: 10.1111/j.1526-4610.1993.hed3301029.x. [DOI] [PubMed] [Google Scholar]
- 7.Stewart WF, Lipton RB, Celentano DD, Reed ML. Prevalence of migraine headache in the US. JAMA. 1992;267:64–9. [PubMed] [Google Scholar]
- 8.Rasmussen BK, Jensen R, Olesen J. Impact of headache on sickness, absence and utilization of medical services: a Danish population survey. J Epidemiol Commun Health. 1992;46:443–6. doi: 10.1136/jech.46.4.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50:133–49. doi: 10.1016/0304-3959(92)90154-4. [DOI] [PubMed] [Google Scholar]
- 10.Derogatis LR. Towson, Md: Clinical Psychometric Research; 1983. SCL-90-R: Administration, Scoring and Procedures Manual-II for the Revised Version. [Google Scholar]
- 11.Linet MS, Stewart WF, Celentano DD, et al. An epidemiologic study of headache among adolescents and young adults. JAMA. 1989;261:2211–6. [PubMed] [Google Scholar]
- 12.Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias, and facial pain. Cephalalgia. 1988;8(suppl 7):19–28. [PubMed] [Google Scholar]
- 13.Saunders KW, Stergachis A, Von Korff M. Group Health Cooperative of Puget Sound. In: Strom BL, editor. Pharmacoepidemiology. New York, NY: John Wiley and Sons; 1994. in: ed. [Google Scholar]


