Abstract
OBJECTIVE
To determine patient knowledge about life-sustaining treatments and physician understanding of patient preferences for proxies and treatments after outpatient discussions about advance directives.
DESIGN
Cross-sectional interview-based and questionnaire-based survey.
SETTING
Two university general internal medicine practices, two Department of Veterans Affairs general internal medicine practices, and one university-based geriatrics practice, in two different cities.
PATIENTS
Fifty-six patients of primary care internists.
INTERVENTION
Physicians discussed “advance directives” (ADs) with one randomly selected patient during an outpatient visit.
MEASUREMENTS AND MAIN RESULTS:
After the discussions, physicians identified the patient's proxy and predicted the patient's preferences for treatment in 20 scenarios. Patients provided treatment preferences in the 20 scenarios, the name of their preferred surrogate decision maker, and their understanding of cardiopulmonary resuscitation and mechanical ventilation. Of the 39 patients who discussed resuscitation, 43% were able to identify two important characteristics; 26% identified none; 66% did not know that most patients need mechanical ventilation after undergoing resuscitation. None of the 43 patients who had a discussion about mechanical ventilation had a good understanding of it; 67% did not know that patients generally cannot talk while on ventilators; 46% expressed serious misconceptions about ventilators. There was poor agreement between physicians and their patients regarding treatment preferences in 18 of 20 scenarios (κ−0.04 to 0.31). Physicians correctly identified the proxy 89% of the time (κ 0.78).
CONCLUSIONS
Patients leave routine AD discussions with serious misconceptions about life-sustaining treatments. Physicians are unable to predict treatment preferences but do learn about patients' preferences for surrogate decision makers.
Keywords: advance directives, patient-doctor communication, medical ethics
Advance care planning offers patients an opportunity to gain control over their medical care should they ever lose decision-making capacity.1 Ideally, this involves discussions with a primary physician that result in the physician's understanding and documentation of the patient's informed decisions regarding life-sustaining treatment in the even of a future medical crisis.
Many physicians and medical ethicists publicly advocate outpatient discussions between primary care physicians and their patients for advance care planning. 2–6 The Joint Commission for the Accreditation of Healthcare Organizations guidelines include a requirement to make advance directives (ADs) available to all patients in hospital-affiliated outpatient clinics.7 Furthermore, many patients desire the opportunity to discuss advance care plans with their physicians while they are still relatively healthy.8–15
Nevertheless, enthusiasm for ADs has waned recently. Studies have called into question the impact that completion of AD forms has on care.16–19 Although the quality of the physician-patient discussions about ADs presumably affects the utility of these documents, the discussions themselves have received little attention.
The prevailing view in the literature is that the process of advance care planning ought to parallel the process of informed consent.20 In this model, just as patients choosing between therapeutic options need to understand their diagnosis, prognosis, and the proposed treatments' risks and benefits, patients making prospective decisions about future care need to understand the medical situations, treatment possibilities, and their risks and benefits. Furthermore, physicians must understand what treatments the patient would or would not accept in potential illness scenarios. A model for advance care planning in the nursing home setting, based on the principles of prospective informed consent and described by Miles et al., is well suited for adaptation to the outpatient setting.21 In this model, the physician explains the purpose of the discussion, provides medical information to the patient to inform patient decision making, and gains knowledge about the patient's treatment goals, preferences for life-sustaining treatment in various possible future conditions, and preferred proxy decision maker.
A few small studies suggest that advance care planning conversations, as they are currently carried out, do not meet the criteria described above. However, these studies were conducted under simulated conditions, 21, 22 or by observing residents discussing do-no-resuscitate orders with acutely ill hospitalized patients.23 They also did not assess physician knowledge of patient preferences or patient understanding of relevant medical information after the discussions. Furthermore, a cross-sectional study showed that doctors who had had discussions about cardiopulmonary resuscitation (CPR) or mechanical ventilation with their patients were no better and sometimes worse at predicting their patients' treatment preferences in five scenarios than doctors who had not had such discussions.24 No information was available about the actual content of the discussions.
The purpose of this study is to determine the level of patients' understanding of important concepts involved in end-of-life decision making and physicians' understanding of patients' preferences for care after routine outpatient discussions about ADs. By audiotaping these discussions, we were able to look for correlations between these outcomes and the conversations' content.
METHODS
Subjects
All primary care internists at five practice sites in two cities were eligible for the study. The sites included two university-based general internal medicine practices, two Department of Veterans Affairs (VA) general internal medicine practices, and one university-based geriatrics practice.
Patients were eligible if they were at least 65 years old or suffered from a serious medical illness, such as HIV infection, cancer, renal insufficiency (creatinine level>3 or chronic dialysis), history of cardiac arrest, or had chronic obstructive pulmonary disease, cirrhosis, or congestive heart failure requiring at least two hospitalizations in the last year. In addition, patients were excluded if they did not speak English, were judged incompetent to make medical decisions by their physician, or had previously discussed ADs with their physician.
We asked each physician to discuss “advance directives” with one of their regular patients chosen randomly from a list of eligible patients scheduled to see the physician on a selected clinic day. We included one patient per physician. Physicians had the opportunity to refuse to enroll a patient if they thought an AD discussion would be inappropriate with that patient for any reason. Six physicians (11%) who exercised this option cited reasons such as concerns about the emotional state of the patient. After the physician consented, patients were reached by telephone. The study was explained to them, and consent was obtained. Patients signed a consent form on the day of their visit.
Measurements
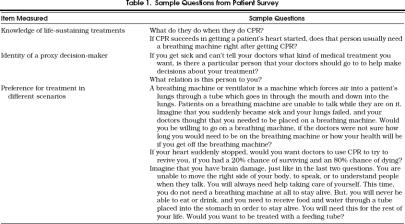
Each patient participated in a face-to-face interview after the audiotaped physician encounter. The interview was conducted immediately after the office visit in 93% of cases and always occurred within 48 hours of the encounter. The survey measured knowledge about life-sustaining treatments in a series of open-ended and multiple-choice questions. The survey also elicited the presence and identity of the preferred health care proxy decision maker. Finally, patients responded to questions about whether they would want treatment in 20 different illness scenarios. The scenarios were described in detail, and any medical terms used were defined. The context of the questions made it clear that the alternative to treatment was death. Patients were given an opportunity to ask questions about the scenarios if they did not understand them. In the six scenarios involving permanent unconsciousness and three involving severe mental disability, patients were asked about different interventions, such as tube feeding and mechanical ventilation. In the remaining 11 questions involving mechanical ventilation or CPR, the chance of complete recovery to the patient's current state of health was varied. When numeric probabilities were used, patients were shown a pie chart depicting the probability. For the scenarios involving permanent unconsciousness, the interviewer coded patients' spontaneous answers to whether they would want treatment as “yes,”“no,”“unsure,” or “whatever my doctor thinks is best.” For the other scenarios, patients chose from the following options: “definitely,”“probably,”“probably not,” and “definitely not.” Interviewers also noted when patients responded that they were unsure or that they wanted their doctor to make the decision.Table 1)contains examples of survey questions and scenarios. (Copies of the survey instrument can be obtained from the corresponding author.)
Table 1.
Sample Questions from Patient Survey
Physicians completed a self-administered questionnaire after the patient encounter. The questionnaire asked the physician to identify the surrogate preferred by the patient and to predict the patient's preferences for treatment in the scenarios contained in the patient survey. Physicians also responded to questions about the patient's medical conditions and the probability that the patient would survive a CPR attempt.
Data Analysis
Patient Knowledge of Life-Sustaining Treatments.
Two evaluators read the answers to the open-ended questions and rated them according to predetermined criteria. Understanding of mechanical ventilators was rated as “good,”“fair,” or “poor,” and the presence of specific misconceptions was noted. Patients had a “good understanding” if they knew that a ventilator forces air into the lungs, patients generally cannot speak while on a ventilator, and other abilities (to see, to communicate) depend on other aspects of the patient's medical condition. They had a “fair understanding” if they understood that a ventilator is used to help a patient breathe, but did not meet the criteria for a good understanding. Patients who thought that people on ventilators were necessarily comatose could qualify for this category, but patients harboring other major misconceptions, such as the belief that a ventilator is a “heart monitor” or the belief that it directly makes the heart continue to beat, were coded as having a “poor understanding.” For CPR, the evaluators noted whether specific features of the process, such as chest compressions and artificial respiration, were mentioned by the patient. We checked interrater reliability using the κ statistic.25 Kappa was greater than 0.6 (range 0.66–1.00) for all items except understanding of mechanical ventilators, where it was 0.53. Disagreements were resolved by consensus between the evaluators. Physician and patient estimates of chance of survival after receiving CPR were compared using the Wilcoxon Rank-Sum Test.
Physician Ability to Predict Treatment Preferences and Proxies.
For each of the 20 scenarios in the survey, we compared physician and patient responses. For this analysis, responses were placed into two categories: “wants treatment” and “does not want treatment.” Percentage of agreement was defined as the percentage of physicians who correctly predicted their patients' preferences for the given scenario. Because percentage of agreement can be misleading in a situation in which a large proportion of the responses falls into one category, we also calculated the proportion of specific agreement, which evaluates agreement for the less commonly chosen option.25 To account for the influence of chance, the κ statistic was computed for each scenario: κ >0.6 indicates good agreement, and κ >0.4 indicates moderate agreement.26 When physicians or patients stated they were “unsure” about their treatment preference, we placed the response in the “treat” category for the analyses presented here, as that reflects actual practice. Results when the “unsure” responses are excluded from the analysis are similar to those when these responses are included in the “treat” category. In seven of the scenarios, there was one patient who wanted the doctor to make the decision. These responses were eliminated from the analysis reported here. If these responses are automatically counted in favor of the physician, it does not affect the results.
The physicians' beliefs about the existence of a proxy and the proxy's identity were compared with the patients' answers to these questions, using percentage of agreement and κ.
Relation of Content of Discussions to Outcomes.
We explored how the actual content of the discussions about ADs influenced the outcomes of patient knowledge and physician ability to predict patient preferences. All audiotapes of the discussions were transcribed and coded. Transcripts were read by two raters. Raters identified each segment of uninterrupted speech that referred to CPR, mechanical ventilation, presentation of quantitative probabilities (i.e., percentages), and presentation of qualitative probabilities (i.e., statements like “a good chance”). Using these codes, we identified which discussions contained some mention of each of these topics. Interrater reliability for these codes, measuring the extent to which raters agreed that a particular code was applicable in a given discussion, was good, with κ >0.6 (range 0.70–0.90). Using a UNIX-based computer program that identifies all text labeled with any given code, we also used the codes to search for characteristics of the conversations that might explain differences in the ability of physicians to predict preferences.
RESULTS
Fifty-six (93%) of 60 eligible physicians participated. The physicians had a mean age of 37 years and a mean of 11 years' experience; 56% were male and 93% were white. They reported spending an average of 20 hours a week in direct patient care (range 2–50), and they knew the patients in this study an average of 2.5 years (range 0.08–12).
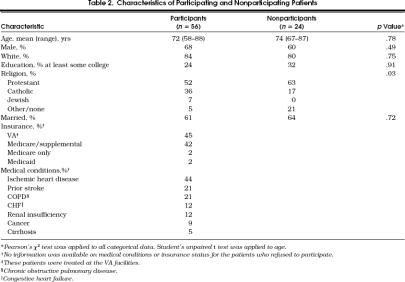
Fifty-six (70%) of 80 patients who were approached agreed to participate. They had a mean age of 72 years; 68% were male, and 84% were white. Their marital status, insurance, religion, and major medical diagnoses are listed in Table 2. Patients who refused to participate were more likely to be Protestant than that those who agreed (p=.03, Table 2). Twenty-three percent already had an AD, unknown to the physicians prior to the study.
Table 2.
Characteristics of Participating and Nonparticipating Patients
Patient Understanding of Topics Discussed
Thirty-nine (70%) of the discussions mentioned CPR. The patients who had these discussions greatly overestimated their chances of survival after an in-hospital cardiopulmonary arrest. The patients' median estimate of the probability of survival to hospital discharge was 70%, compared with a 20% median probability of survival stated by their physicians (p < .0001, Wilcoxon Rank Sum).
Most of these patients were able to describe some specific features of CPR. In response to the open-ended question, “What do they do when they do CPR?,” 71% identified chest compressions, 60% identified some sort of assisted breathing (mouth-to-mouth or intubation), and 23% alluded to defibrillation. One patient identified the use of medications, and one mentioned the possibility of brain damage after resuscitation. Forty-three percent identified two or more of these characteristics, but 26% did not identify any. One response was: “Well, they breathe into your lungs and they try to get your lungs started up again, and that I think is done in the field. Perhaps if it's a heart problem, they pound on your chest, and if they have the facility, I guess they can do shock treatments.”
However, to the question “If CPR succeeds in getting a patient's heart started, does that patient usually need a breathing machine right after CPR?,” 34% answered “yes,” 32% answered “no,” and 34% were unsure. There were no significant differences in responses between patients who had a discussion about CPR and those whose discussions did not include CPR.
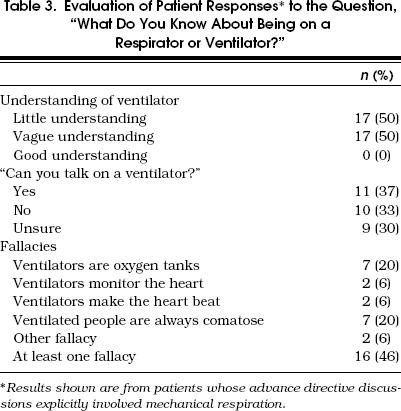
Discussion concerning mechanical ventilation occurred with 43 (77%) of the patients. Patients whose discussions included mechanical ventilation had a poor understanding of what this procedure entails, and a significant number harbored important misconceptions.Table 3 shows these patients' responses to an open-ended question about mechanical ventilation. No subject who discussed ventilators had a good understanding of what they involved, and 50% had a poor understanding. The only subject with a good understanding had an AD discussion that did not explicitly involve mechanical ventilation. Here is an example of a response exhibiting “poor understanding”:
Table 3.
Evaluation of Patient Responses* to the Question, “What Do You Know About Being on a Respirator or Ventilator?”
A breathing machine is one that is the same as, something that looks like a heart machine. It tells you how your heart is beating, and it tells you—a living machine.
Below is an example of a response exhibiting “fair understanding”:
Interviewer: Do you have any idea what it does or how it might work?
Patient: Makes you breathe, and tries to keep you alive, I guess.
Interviewer: Do you know how it works to make you breathe?
Patient: No.
Interviewer: Do you know how it connects to your body?
Patient: No.
Interviewer: What do you think it would be like to be on one?
Patient: Oh, I don't want to be on one.
Interviewer: OK. Do you have any idea what it might be like to be one?
Patient: I don't know.
In response to the question “Can you talk while you are on a ventilator?” 67% either said “yes” or were unsure. Sixteen (46%) of the patients expressed serious misconceptions about ventilators: seven thought they were oxygen tanks, seven assumed that all ventilated patients were comatose, two believed that they were heart monitors, two stated that they helped the heart to beat, and two had other misconceptions (Table 3). There were no significant differences in patients' understanding regardless of whether their discussion included mechanical ventilation.
Participants who had previously written ADs did not have better knowledge of CPR or mechanical ventilation on any of these measures. In fact, those who had ADs were more likely to express the view that ventilators directly kept the heart beating (p= .001).
Physician Understanding of Treatment Preferences
In 13 of the 20 scenarios, there was little variation in treatment preferences among patients: in 4 scenarios, 75% or more patients wanted treatment, and in 9 scenarios, 75% or more patients did not want treatment. The percentage of agreement between doctors and patients ranged from 59% to 83%, and was greater than 75% in 10 of the scenarios. All but two of the scenarios with more than 75% agreement were scenarios in which there was little variation in treatment responses among patients.
The κ statistic indicated moderate agreement between physicians and their patients regarding treatment preferences in only 2 of the 20 scenarios. In the scenario involving severe permanent brain damage with an acute, intercurrent illness requiring a ventilator for only a short amount of time, the agreement was 78% with a κ of 0.47. In the scenario involving the need for a ventilator for an unknown period of time, the agreement was 76% with a κ of 0.44. Interestingly, these were the two scenarios in which there was high percentage of agreement even though there was considerable variation in patient preference. In the remaining 18 scenarios, κ ranged from −0.04 to 0.31 (median 0.15), despite the fact that the median percentage of agreement was 70% (range 59–86%).
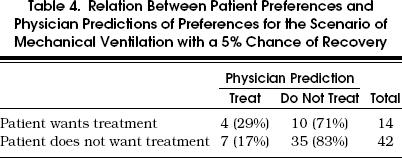
The disparity between the κ values and the percentages of agreement generally resulted from an inability of physicians to predict patients' idiosyncratic preferences. For example, to the question “Would you want to go on a breathing machine if there was a 5% chance of getting off that machine?” 23% of patients answered “yes,” and 77% answered “no.” Physicians accurately identified those patients who did not want a respirator 83% of the time. However, only 17% of physicians whose patients answered “yes” predicted this response (Table 4 A similar pattern was evident in the other scenarios.
Table 4.
Relation Between Patient Preferences and Physician Predictions of Preferences for the Scenario of Mechanical Ventilation with a 5% Chance of Recovery
We analyzed the discussions to determine whether differences in content might explain why some physicians were able to predict correctly patients' idiosyncratic responses in this scenario. Examination of passages that had been coded as relating to respirators or to the probabilities of outcomes revealed important differences.
In the four cases in which the doctor correctly predicted that the patient wanted treatment, either the doctor or the patient explicitly discussed the desire for treatment in the context of low probability of success. For example, one physician asked, “We need to know if you are a five-percenter … If I have to put you on a ventilator and there's a five percent chance of getting you off that ventilator, would you want it …”
In another case, it was the patient who stated his views on reversible illness: “… if there's any chance at all of reviving a sentient, sensible person, for heaven's sake, use it.”
The 10 doctors who incorrectly believed that their patients would not want treatment failed to elicit from the patient a treatment preference in the event of a low probability of success. In most of the conversations, the concept did not arise at all. In two discussions, probability was described in vague terms. For example, one doctor said, “If there's reasonable doubt, we err on the side of going, rather than not going.” The patient agreed, but what constituted “reasonable doubt” was never spelled out.
There was one case in which the likely source of the doctor's mistaken impression of the patient's preferences is evident:
Physician: Because sometimes what happens is that those attempts—tries in getting people well are futile and just prolongs suffering… If people make a decision ahead of time … that if they are ever in a position where they are on a respirator and things look pretty hopeless, that someone would make a decision of basically stopping all treatment. OK. some people even make the decision that they don't even want to be on a respirator.
Patient: I don't want to be on one.
Although the patient may only be responding to the extremely grim scenario that the physician is depicting, his comment can be interpreted to mean that he never wants to be on a respirator. In fact, this physician predicted that the patient would answer “no” to all of the ventilator scenarios that were in the survey, whereas the patient answered “yes” to all of them except two cases: the case in which the doctors are unsure of the prognosis and the case in which the doctors believed that the patient would never come off of the ventilator.
Physicians' Ability to Predict Patient Surrogates
Of those patients who told us that they had a preferred proxy decision maker, 76% of physicians were aware of this fact. Furthermore, physicians who were aware that their patients had a preferred proxy correctly identified the proxy 89% of the time (κ = 0.78).
DISCUSSION
Our results indicate that these discussions fell short of the goals represented by Miles' model of advance care planning discussions.21 It is true that after a discussion about ADs, physicians were able to identify their patients' preferred proxy. However, physicians were unable to predict their patients' specific treatment preferences better than chance in 18 of 20 scenarios, and patients left the conversations with serious misunderstandings about CPR and mechanical ventilation.
One of the most disconcerting findings of this study was that patients expressed strong preferences about treatments that they did not understand. A patient who states that he would never accept artificial ventilation, not recognizing that it sometimes is briefly needed to provide a full recovery, is in danger of being denied a treatment that he would want if he understood it better. Conversely, a patient who wants CPR, believing that she would have a 70% chance of full recovery, is in danger of being subjected to an intervention she might not want if she understood the true likelihood of success.27
Our patients generally believed that they would have a 70% chance of recovery to hospital discharge after CPR, which is remarkably close to the survival rate of CPR in television programs,28 but far above that predicted by their physicians and far above the actual survival rate (9–16%).29, 30 Other studies have also reported that patients do not understand terms commonly used in living wills 11 and do not have a good understanding of CPR.13 Clearly, if these discussions are to meet the requirements of prospective informed consent, physicians will need to be aware of prior misconceptions that patients may have about life-sustaining treatments, and will have to ensure that they come away with an understanding of the treatments that are being discussed.
We also found that physicians were unable to predict treatment preferences better than chance, despite high percentages of agreement for most scenarios. One may ask if physicians have a 70% or 80% chance of correctly predicting a patient's treatment preference, does the low κ value matter? We believe it does. Physicians generally have a high degree of accuracy only in cases in which large majorities of patients have the same treatment choice. However, physicians have low accuracy for patients with idiosyncratic preferences. This implies that physicians are expressing preexisting conceptions of what patients want in general, rather than using information gathered from a particular patient to predict that person's true wishes.
The discussions provide some clues on how physicians might identify idiosyncratic preferences. In the case we examined in depth, the physicians who incorrectly believed that their patient would not want treatment failed to elicit their patient's preference when success is very unlikely. This suggests physicians should ask a series of questions about the patient's views on treatment in the face of uncertainty and different probabilities of success. This might be accomplished either by using very specific numeric descriptions of probabilities or by exploring patients' underlying values and goals in more detail. Further research is needed to determine other factors that may cause patient preferences to vary and to develop methods to discuss these topics efficiently.
There are a number of suggestions in the literature about how to conduct advance care planning discussions effectively. The model proposed by Miles involves having practitioners concentrate on eight specific content points, and represents an effort to meet the criteria of prospective informed consent.21 Interestingly, after hearing a 90-minute lecture on the content areas, physicians still exhibited serious deficiencies in their conversations 21 indicating the need to teach physicians not just what to discuss, but how to discuss it. Emanuel et al. recommend a five-step process, which includes allocating portions of three different visits to introducing the topic, facilitating a structured discussion, and actually completing and recording an AD.31 This model gives the patient time to read informational materials, talk to family members, assimilate difficult information, and ask questions, and may overcome some of the shortcomings observed in our discussions. Finally, Patrick et al. endorse asking patients to rate health states and to state treatment preferences, allowing physicians to explore any discrepancies between the two approaches.32 This may help physicians to discover patient misunderstandings and also to better understand patients' values and preferences. We need empiric studies to determine whether these approaches would enhance patient understanding of important concepts and physician understanding of patient preferences.
This study has several limitations. The sample size was small, limiting our ability to quantitatively determine differences between groups. However, the study included five separate sites in two cities, and nearly all of the eligible physicians participated, which decreases the chances that our physicians differ from other practitioners. The small sample size allowed us to scrutinize qualitatively the content of the discussions and answers to open-ended interview questions.
Because we have no information about patient knowledge or physician understanding of patient preferences prior to the discussion, this study cannot tell us how the discussions affected these variables. It is possible, for example, that the discussions increased or even decreased patient knowledge. We were concerned that surveying the patients and doctors prior to the discussions would alter the content of the discussions and bias our results. Nevertheless, the principal findings of this study, that patient knowledge and physician understanding are inadequate following a discussion about ADs, remain true, even in the absence of knowledge of their quality beforehand.
There are methodologic concerns with using scenarios to assess patient preferences. If patients do not understand the scenario, for example, their answers mean little. To ensure validity, our questions were framed to help patients understand what the experience would be like. We avoided technical terms and explained interventions, and we presented probabilities in visual form.33
Finally, people who believe that these discussions should focus more on values and goals than on specific scenarios might object that we are measuring the wrong outcomes. Nevertheless, in-depth, qualitative analysis of these discussions shows that patient values and goals were rarely discussed in depth (unpublished observations).
Many influential individuals and organizations advocate outpatient discussions about ADs. Nevertheless, these conversations, as currently conducted, do not further the goals of ADs. Better communication regarding these issues is critical if ADs are to promote patients' values during critical illness.
Acknowledgments
Financial support was provided in part by the R. K. Mellon Foundation, the National Institute on Aging Claude D. Pepper Older Americans Independence Center, grant 5-P60-AG11268, VA HSR&D Service, and the John A. Hartford Foundation.
The authors thank Esther Shaw for technical support on the computer and the 112 patients and physicians who graciously allowed us to observe them.
References
- 1.Teno JM, Nelson HL, Lynn J. Advance care planning: priorities for ethical and empirical research. Hastings Cent Rep. 1994;24:S32–6. [PubMed] [Google Scholar]
- 2.Emanuel LL, Barry MJ, Stoeckle JD, Ettelson LM, Emanuel EJ. Advance directives for medical care—a case for greater use. N Engl J Med. 1991;324:889–95. doi: 10.1056/NEJM199103283241305. [DOI] [PubMed] [Google Scholar]
- 3.Layson RT, Adelman HM, Wallach PM, Pfeifer MP, Johnston S, McNutt RA. Discussions about the use of life-sustaining treatments: a literature review of physicians' and patients' attitudes and practices. J Clin Ethics. 1994;5:195–203. [PubMed] [Google Scholar]
- 4.Loewy EH, Carlson RW. Talking, advance directives, and medical practice. Arch Intern Med. 1994;154:2265–7. [PubMed] [Google Scholar]
- 5.President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Patients who lack decision-making capacity . In: Deciding to Forgo Life-Sustaining Treatment: A Report on the Ethical, Medical, and Legal Issues in Treatment Decisions. Washington, DC: President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research; 1983. pp. 121–70. [Google Scholar]
- 6.American College of Physicians Ethics Manual Part 2: The physician and society; research; life-sustaining treatment; other issues. Ann Intern Med. 1989;111:327–35. doi: 10.7326/0003-4819-111-4-327. [DOI] [PubMed] [Google Scholar]
- 7.Joint Commission on Accreditation of Healthcare Organizations . 1996 Comprehensive Accreditation Manual for Ambulatory Care. Oakbrook Terrace, Ill: Joint Commission on Accreditation of Healthcare Organizations; 1995. pp. 79–80. [Google Scholar]
- 8.Haas JS, Weissman JS, Cleary PD, et al. Discussion of preferences for life-sustaining care by persons with AIDS: predictors of failure in patient-physician communication. Arch Intern Med. 1993;153:1241–8. [PubMed] [Google Scholar]
- 9.Johnston SC, Pfeifer MP, McNutt RA. The discussion about advance directives: patient and physician opinions about when and how it should be conducted. Arch Intern Med. 1995;155:1025–30. doi: 10.1001/archinte.155.10.1025. [DOI] [PubMed] [Google Scholar]
- 10.Edinger W, Smucker DR. Outpatients' attitudes regarding advance directives. J Fam Pract. 1992;35:650–3. [PubMed] [Google Scholar]
- 11.Joos SK, Reuler JB, Powell JL, Hickam DH. Outpatients' attitudes and understanding regarding living wills. J Gen Intern Med. 1993;8:259–63. doi: 10.1007/BF02600093. [DOI] [PubMed] [Google Scholar]
- 12.Gamble ER, McDonald PJ, Lichstein PR. Knowledge, attitudes, and behavior of elderly person regarding living wills. Arch Intern Med. 1991;151:277–80. [PubMed] [Google Scholar]
- 13.Shmerling RH, Bedell SE, Lilienfeld A, Delbanco TL. Discussion cardiopulmonary resuscitation: a study of elderly outpatients. J Gen Intern Med. 1988;3:317–21. doi: 10.1007/BF02595786. [DOI] [PubMed] [Google Scholar]
- 14.Steinbrook R, Lo B, Moulton J, Saika G, Hollander H, Volberding PA. Preferences of homosexual men with AIDS for life-sustaining treatment. N Engl J Med. 1986;314:457–60. doi: 10.1056/NEJM198602133140730. [DOI] [PubMed] [Google Scholar]
- 15.Lo B, McLeod GA, Saika G. Patient attitudes to discussion life-sustaining treatment. Arch Intern Med. 1986;146:1613–5. [PubMed] [Google Scholar]
- 16.The SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients: the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT) JAMA. 1995;274:1591–8. [PubMed] [Google Scholar]
- 17.The SUPPORT Principal Investigators. Do formal advance directives affect resuscitation decisions and the use of resources for seriously ill patients? J Clin Ethics. 1994;5:23–30. [PubMed] [Google Scholar]
- 18.Virmani J, Schneiderman LJ, Kaplan RM. Relationship of advance directives to physician-patient communication. Arch Intern Med. 1994;154:909–13. [PubMed] [Google Scholar]
- 19.Danis M, Southerland LI, Garrett JM, et al. A prospective study of advance directives for life-sustaining care. N Engl J Med. 1991;324:882–8. doi: 10.1056/NEJM199103283241304. [DOI] [PubMed] [Google Scholar]
- 20.Olick RS. Approximating informed consent and fostering communication: the anatomy of an advance directive. J Clin Ethics. 1991;2:181–9. [PubMed] [Google Scholar]
- 21.Miles SH, Bannick-Mohrland S, Lurie N. Advance-treatment planning discussions with nursing home residents: pilot experience with simulated interviews. J Clin Ethics. 1990;1:108–12. [PubMed] [Google Scholar]
- 22.Miller A, Lo B. How do doctors discuss do-not-resuscitate orders? West J Med. 1985;143:256–8. [PMC free article] [PubMed] [Google Scholar]
- 23.Tulsky JA, Chesney MA, Lo B. How do medical residents discuss resuscitation with patients? J Gen Intern Med. 1995;10:436–42. doi: 10.1007/BF02599915. [DOI] [PubMed] [Google Scholar]
- 24.Uhlmann RF, Pearlman RA, Cain KC. Physicians' and spouses' predictions of elderly patients' resuscitation preferences. J Gerontol. 1988;43:M115–21. doi: 10.1093/geronj/43.5.m115. [DOI] [PubMed] [Google Scholar]
- 25.Fleiss JL. Statistical Methods for Rates and Proportions. 2nd ed. New York, NY: John Wiley & Sons; 1981. The measurement of interrater reliability; pp. 211–36. [Google Scholar]
- 26.Seckler AB, Meier DE, Mulvihill M, Cammer Paris BE. Substituted judgement: how accurate are proxy predictions? Ann Intern Med. 1991;115:92–8. doi: 10.7326/0003-4819-115-2-92. [DOI] [PubMed] [Google Scholar]
- 27.Forrow L. The green eggs and ham phenomena. Hastings Cent Rep. 1994;24:S29–32. [PubMed] [Google Scholar]
- 28.Diem SJ, Lantos JD, Tulsky JA. Cardiopulmonary resuscitation on television. Miracles and misinformation. N Engl J Med. 1996;334:1578–82. doi: 10.1056/NEJM199606133342406. [DOI] [PubMed] [Google Scholar]
- 29.Schultz SC, Cullinane DC, Pasquale MD, Magnant C, Evans SR. Predicting in-hospital mortality during cardiopulmonary resuscitation. Resuscitation. 1996;33:13–7. doi: 10.1016/s0300-9572(96)00986-0. [DOI] [PubMed] [Google Scholar]
- 30.Bailecki L, Woodward RS. Predicting death after CPR. Experience at a nonteaching community hospital with full-time critical care staff. Chest. 1995;108:1009–17. doi: 10.1378/chest.108.4.1009. [DOI] [PubMed] [Google Scholar]
- 31.Emanuel LL, Danis M, Pearlman RA, Singer PA. Advance care planning as a process: structuring the discussions in practice. J Amer Geriatr Soc. 1995;43:440–6. doi: 10.1111/j.1532-5415.1995.tb05821.x. [DOI] [PubMed] [Google Scholar]
- 32.Patrick DL, Pearlman RA, Starks HE, Cain KC, Cole WG, Uhlmann RF. Validation of preferences for life-sustaining treatment: implications for advance care planning. Ann Intern Med. 1997;127:509–17. doi: 10.7326/0003-4819-127-7-199710010-00002. [DOI] [PubMed] [Google Scholar]
- 33.Murphy DJ, Burrows D, Santilli S, et al. The influence of the probability of survival on patients' preferences regarding cardiopulmonary resuscitation. N Engl J Med. 1994;330:454–9. doi: 10.1056/NEJM199402243300807. [DOI] [PubMed] [Google Scholar]