Abstract
OBJECTIVE
To provide estimates of physical abuse and use of health services among depressed women in order to inform efforts to increase detection and treatment of physical abuse.
DESIGN
Retrospective assessment of abuse and health services use over 1 year in a cohort of depressed women.
SETTING
Statewide community sample from Arkansas.
PARTICIPANTS
We recruited 303 depressed women through random-digit-dial screening.
MEASUREMENTS AND MAIN RESULTS
Exposure to physical abuse based on the Conflict Tactics Scale, multi-informant estimate of health and mental health services. Over half of the depressed women (55.2%) reported experiencing physical abuse as adults, with 14.5% reporting abuse during the study year. Women abused as adults had significantly more severe depressive symptoms, more psychiatric comorbidity, and more physical illnesses than nonabused women. After controlling for sociodemographic and severity-of-illness factors, recently abused, depressed women were much less likely to receive outpatient care for mental health problems as compared to other depressed women (odds ratio [OR] 0.3;p = .013), though they were more likely to receive health care for physical problems (OR 5.7, p = .021).
CONCLUSIONS
Because nearly all depressed women experiencing abuse sought general medical rather than mental health care during the year of the study, primary care screening for physical abuse appears to be a critical link to professional help for abused, depressed women. Research is needed to inform primary care guidelines about methods for detecting abuse in depressed women.
Keywords: physical abuse, depression, health services use, mental health services use
Despite the growing recognition that physical abuse affects physical and mental health,1–4 events of abuse usually remain unreported by women 5–7 and unrecognized by medical professionals.6, 8, 9 Community surveys have estimated that between 18.1% and 36.4% of women have been physically abused as adults, with 1-year prevalence rates ranging between 8.0% and 14.4%.10–13 Physical abuse is associated with important problems for women's physical and mental health. A number of studies have documented higher rates of depressive disorders and mental health problems among abused women.13–15 Despite evidence linking depression and physical abuse, surprisingly little is known about the prevalence of physical abuse among depressed women.
In addition to its etiologic importance, physical abuse may play a role in whether depressed women seek treatment for depression. Although physical abuse increases women's need for both physical and mental health services,2–4 it is often accompanied by other coercive behaviors that may prevent women from seeking help. Perpetrators of physical abuse may restrict an abused woman's contact with other people, her access to family resources such as money and transportation,16 or her ability to make independent decisions about what she needs.17 Abused women who visit a physician may not be able to use the encounter to obtain the help they need. A national survey found that abused women reported greater unmet health needs, despite their higher levels of health care use.2
The purpose of this study was to document the prevalence of physical abuse by partners or family members among a population-based sample of depressed women and to examine the relation between physical abuse and use of services for emotional problems. We hypothesized that abused, depressed women would have more severe physical and emotional illness when compared with nonabused, depressed women. In addition, we hypothesized that depressed women who were experiencing ongoing abuse would be less likely to seek treatment for their emotional problems than women who had experienced abuse in the past or never.
METHODS
Subject Recruitment
Data for this report were taken from a study of rural-urban differences in mental health treatment among a community-based sample of depressed persons. We completed the first stage of depression screening via telephone interviews. The intent of this phone call was explained to interviewees as, “We want to learn more about the health care needs of people living in Arkansas.” We sampled adults aged 18 years and older in 11,078 randomly selected Arkansas households with listed and unlisted telephone numbers, using a stratified sampling design to oversample nonmetropolitan counties. Recruitment began in April 1991 and continued for 16 months. The screened households represented 70.5% of the 15,721 households attempted; of the remaining households, 6.5% refused to participate and 23.5% did not complete the screening interview. Nine percent (n= 998) of household members screened positive for substantial symptoms of depression—face-to-face interviews have shown that our depression screener has an 89% sensitivity, a 95% specificity, and a 23% positive predictive value when compared to a “gold standard,” the Diagnostic Interview Schedule (DIS).18 There were 713 women in this group. Excluded were 228 bereaved, 39 manic, and 10 acutely suicidal women who were immediately referred to treatment, in addition to 3 subjects who reported no symptoms of depression at the in-person interview.
Of the 433 eligible depressed women, 317 (73.2%) agreed to participate in a 3-hour, face-to-face, baseline interview, which 90.4% of subjects completed within a month after the telephone interview. Women participants did not differ significantly from nonparticipants in race, marital status, income, employment, education, and residence; however, there were differences in age. Women participants were younger (mean age 45.9 vs 56.9 years, p < .0001) and more likely to reside in metropolitan areas (27% vs 16%, p < .02) than nonparticipants.
This study was approved by our institutional review board. Written informed consent was obtained at the baseline interview. Participants were paid $100 for participating in the study. Persons who were acutely suicidal at the screening or baseline interview were referred to the nearest mental health provider and excluded from the study. Participants who reported acute suicidal symptoms in subsequent contacts were immediately referred to treatment and dropped from subsequent waves of the study. All subjects were extensively debriefed at the end of the 12-month study, educated that their symptoms were part of a treatable disease, and either referred to their usual providers or given information on how to obtain services. Subjects who reported physical abuse within the study period were offered information on where to seek help for domestic violence.
Data Collection
We conducted telephone interviews with 307 (96.8%) of the original 317 women subjects at 6 months and with 303 (95.6%) at 12 months. The research team collected and reliably abstracted essentially complete medical, pharmacy, and insurance records for the year following baseline on all 303 women. Records were judged to be essentially complete when diagnostic and billing information was available from either the provider or the insurer (for subjects with insurance).
Measures
Physical Abuse.
The Conflict Tactics Scale (CTS) was used at the 12-month interview to measure exposure to physical abuse.19 The CTS is the most widely used measure of domestic violence in survey studies.20 Subjects are asked about a list of actions that a person might experience in a conflict, from items low in coerciveness (for example, sulking and/or refusing to talk about an issue) to items high in coerciveness and aggression (kicking, biting, or hitting with a fist). Women were asked whether a family member or someone they knew well, such as a boyfriend, had committed these actions against them in a conflict. We coded physical abuse and severe physical abuse using the CTS authors' methods.19 Severe abuse included choking, burning, or threatening with a knife or gun, while physical abuse included severe abuse items plus other items such as throwing something, pushing, or slapping. Respondents were asked about their experiences before the age of 16, between age 16 and the time they entered the study, and during the study year (between the baseline interview and the 12-month follow-up). The age 16 was used because women can consent to marriage at 16 years of age in Arkansas.
We categorized women into three mutually exclusive groups according to the recency of abuse: women who reported abuse in the study year were considered to have recent abuse, women who were abused as adults but not in the study year were grouped as previous adult abuse, and women with no abuse histories as adults were the third category. We used this coding scheme so that we could separate women who were experiencing ongoing abusive situations from women who had previously experienced abuse in adulthood. We treated childhood abuse as an independent predictor of abuse in adulthood.
Women who reported physical abuse at any time during their lifetime were asked whether they had ever reported such an incident to a doctor, psychiatrist, or other health or mental health professional.
Health Care Utilization.
Health care services were coded as treating physical or mental health problems by trained raters who reviewed medical charts and insurance records during the year following baseline using an explicit protocol that attempted to correct for the undercoding of treated emotional problems (M. Zhang et al. Estimating health care utilization and charges: a protocol for requesting and abstracting subject records. A copy of this protocol can be obtained by contacting the corresponding author). A visit was considered to be for a mental health problem if the patient identified it as such, if a mental health diagnosis was listed on the insurance claim or medical chart, or if notes in the medical chart indicated that a mental health problem was addressed (i.e., psychiatric symptoms noted, psychotropic medication prescribed). All other services were considered to be for physical health concerns. We calculated subjects' use of inpatient admissions, emergency department (ED) visits, general medical provider visits, and mental health specialist visits for mental health problems. In addition, we calculated use of inpatient admissions, ED visits, and visits to general medical providers for physical health problems. Use of psychotropic medications was identified from pharmacy records and patient report.
Social and Demographic Factors.
Sociodemographic factors were coded based on responses during the baseline interview. Age was used as a continuous variable, race was identified as minority or white. Education was coded in three categories (less than high school, high school graduate, and any college). Urban residence was coded if the respondent lived in a metropolitan statistical area with all other locations considered rural. Marital status was dichotomized as married (or living as married) versus not married. A dichotomous variable was used to indicate whether the respondent had health insurance coverage. Women who indicated that they had worked full-time at any point during the previous year were considered to be employed. Household income was adjusted for the number of persons supported by the income and expressed as the ratio of the annual income to the poverty level, with higher values indicating higher income.21 Social support was measured at baseline by the number of persons the subject felt she could confide in.22
Severity of Mental and Physical Health Problems.
Depressive symptoms at baseline were measured using symptom counts of the nine criteria for major depression measured by the Inventory to Diagnose Depression scale.23 Because of its clinical significance, we examined one of the nine criteria, suicidal ideation, separately. Axis I comorbidity was measured at baseline by the number of lifetime psychiatric diagnoses the subject met criteria for using the Quick Diagnostic Interview Schedule (QDIS),24 including generalized anxiety disorder, mania, schizophrenia, obsessive-compulsive disorder, panic disorder, and substance dependence or abuse (including alcohol, marijuana, stimulants, sedatives, cocaine, heroin/opiates, PCP/psychedelics, and inhalants). Lifetime posttraumatic stress disorder, as assessed using the QDIS at the 12-month interview, is reported separately here and is not included in the Axis I comorbidity measure. The number of drinks of alcohol consumed on the occasion of the heaviest drinking during the 12-month period was determined. A separate measure of illicit drug use during the past year was also coded from the QDIS. Axis II comorbidity, operationalized as the probability of personality disorder, was measured by a semistructured interview, the Iowa Personality Disorder Screen.25 Previous hospitalization for mental health problems was measured by a single item at baseline, which asked subjects whether they had previously been admitted to the hospital for any emotional problems. History of childhood abuse was coded as yes or no based on reports from the CTS (see above). Physical comorbidity was measured at baseline by summing the number of 12 chronic physical problems for which the subject reported currently receiving treatment.
Analysis
We weighted the data to represent the age, gender, educational distribution, and regional distribution of the state's population. In the Results section, we present unweighted number values and weighted percentages. We used logistic regression first to identify sociodemographic characteristics related to physical abuse and subsequently to investigate how physical abuse was related to the severity of mental and physical health problems. A similar strategy was used to test the relation between recency of abuse and health services utilization, where covariates included potential sociodemographic confounders as well as indicators of severity of illness. Separate analyses were conducted to compare women abused during adulthood with nonabused women as well as to compare women who experienced recent abuse with all others. We chose this approach so that we could examine two different hypotheses about the relation of abuse history to services use: First, we hypothesized that abused, depressed women would have increased need for health services (thus, we needed to compare women with any adult abuse treatment and those with none). Second, we hypothesized that women with recent abuse would have decreased access to mental health services as compared with other depressed women.
RESULTS
Subjects in Study
The depressed women were on average 45.8 years old (SD 15.9, range 18–86), 82.9% were white, 57.1% were high school educated, and 61.6% were currently married. Subjects had an average of 2.5 physical comorbidities (SD 2.0, range 0–9) and 1.3 other psychiatric comorbidities (SD 1.4, range 0–8). All subjects met criteria for substantial depressive symptoms at baseline at a cutpoint that has been shown to be associated with as much functional impairment as recent major depression or dysthymia.26 One in three women (31.8%) met lifetime criteria for major depression only, 0.7% met lifetime criteria for dysthymia only, and 48.6% met lifetime criteria for major depression and dysthymia.
Prevalence of Domestic Abuse and Associated Factors
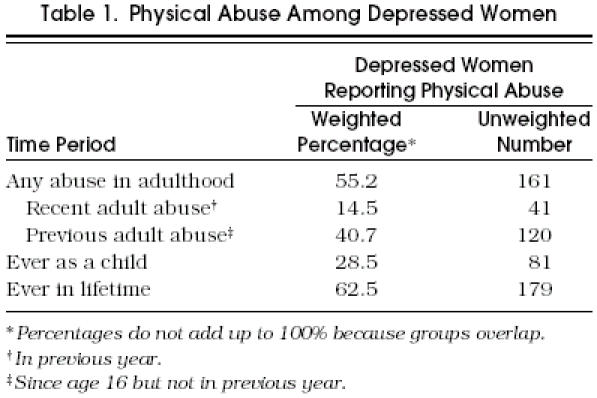
Physical abuse was common in this community sample of depressed women (Table 1). One hundred sixty-one women (55.2%) reported ever experiencing physical abuse as adults (since age 16). Forty-one women (14.5%) reported recent abuse, defined as physical abuse occurring during the course of the yearlong study, and 40.7% reported previous abuse, defined as physical abuse occurring since age 16 but not during the study year. Among the women with recent abuse experience, 42.1% reported severe abuse. Of the depressed women who were physically abused at any time in their lifetime, only 27.9% had reported the abuse to a health or mental health professional.
Table 1.
Physical Abuse Among Depressed Women
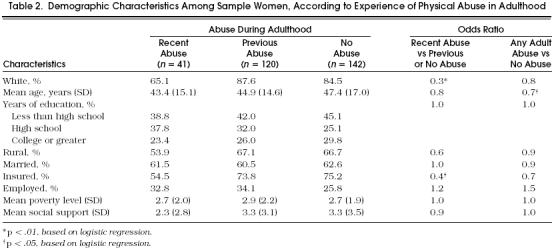
To determine whether demographic characteristics identified women with recent or previous abuse, we ran separate regressions, first comparing women with recent abuse and all others (those with previous abuse and those with no abuse history) and then comparing women with any adult abuse (recent or previous) and those with no adult abuse. Compared with all others, women reporting recent abuse were less likely to be white (odds ratio [OR] 0.3;p= .002) and insured (OR 0.4;p= .012). Compared with nonabused women, women abused in adulthood were younger (OR 0.7;p= .024), but did not differ in other respects including education, rurality, marital status, income, employment, or social support (Table 2). These results indicated that we needed to control for age, race, and insurance in subsequent analyses.
Table 2.
Demographic Characteristics Among Sample Women, According to Experience of Physical Abuse in Adulthood
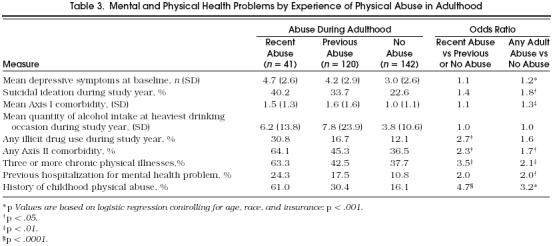
Women who reported recent or previous physical abuse tended to have worse physical and mental health status than the nonabused group. (Table 3) Recently abused women had greater odds of illicit drug use (OR 2.7;p= .02), Axis II comorbidity (OR 2.3;p= .03), childhood physical abuse (OR 4.7;p= .0001), and having three or more chronic physical problems (OR 3.5;p= .002). Compared with nonabused women, women abused in adulthood had more depressive symptoms at baseline (OR 1.2;p= .0007) and were more likely to report suicidal ideation (OR 1.8;p = .04). Abused women also were more likely to report other Axis I comorbidity (OR 1.3;p= .0076), including lifetime posttraumatic stress disorder (OR 3.5;p= .0002). They also were more likely to report any Axis II comorbidity (OR 1.7;p= .04), three or more chronic physical comorbidities (OR 2.1;p= .009), previous mental health hospitalization (OR 2.0;p= .05), and childhood physical abuse (OR 3.2;p= .0002).
Table 3.
Mental and Physical Health Problems by Experience of Physical Abuse in Adulthood
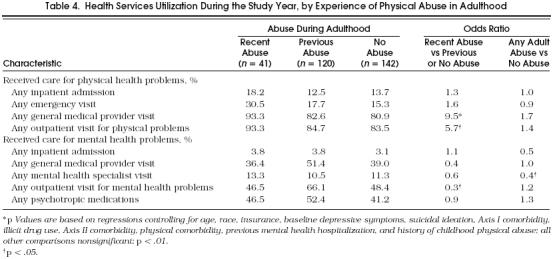
Health Services Utilization
Health services use for physical and mental health problems was examined in the three groups of women using regression models controlling for sociodemographic and severity-of-illness variables (Table 4) Compared with other depressed women, recently abused depressed women had five times the odds of receiving services for physical problems (OR 5.7;p= .021), but only one third the odds of receiving outpatient care for mental health problems during the year following baseline (OR 0.3;p= .013). When compared with nonabused women, abused women were less likely to use specialty mental health services (OR 0.4;p= .05).
Table 4.
Health Services Utilization During the Study Year, by Experience of Physical Abuse in Adulthood
DISCUSSION
The 55% prevalence of physical abuse in adulthood reported in this community-based sample of depressed women is much higher than the 18% to 36% lifetime prevalence of physical abuse reported in general population samples.101–12 It is closer to the 54% abuse prevalence rate reported by women emergency department patients,6 than to the 34% to 39% rate reported by women primary care patients.5, 8, 27 In contrast, current physical abuse does not appear to be more common among these depressed women (14%) than it is in the general population (8–14%).2, 5, 8, 10, 11, 13
Although the study design does not allow us to ascertain the direction of the relation, our results suggest that abused depressed women have more severe physical and mental health problems than nonabused depressed women. Exposure to physical abuse also appears to create barriers that limit women's ability to obtain appropriate mental health care. Depressed women in ongoing abusive situations are only one third as likely to obtain mental health care from either a general medical physician or a mental health specialist, while they are five times as likely to seek care for physical problems. This pattern is consistent with other work that suggests abused women may use services at similar rates to nonabused women but continue to have multiple unmet needs for care.2 It is also consistent with the controlling nature of an abusive relationship: men who batter their wives may allow them to seek care for physical symptoms as long as they do not disclose information that would lead to the detection of the abuse.
Nearly all (93%) of the abused depressed women in our sample sought general medical care; thus, effective screening for domestic violence could be an important step in linking women to help they badly need and will not get otherwise given their reticence to seek mental health care. This becomes particularly critical for the 41% of depressed women abused each year who report severe abuse, such as choking, beating, or threatening with a gun. The low rate of detection reported by depressed abused women provides further support for studies which show that women do not volunteer information about the problem,5–7 and providers do not inquire about exposure to violence in effective ways,6, 8, 9, 28–30 despite the encouragement of professional organizations, consensus panels, and others. 1, 31–34 Physicians most commonly attribute failure to detect physical abuse to women's unresponsiveness to inquiries about it as well as to infrequent visits.35 Women's unresponsiveness to physician's inquiries may be related to their fear of further violence, their financial and emotional inability to leave an abusing partner, and feelings of responsibility for the violence.34 Clearly, more effective methods to detect physically abused women during general medical visits need to be developed, evaluated, and disseminated.36 Simple interventions, such as the inclusion of screening questions on a health history form, can increase the identification of physical abuse 37 ; however, the impact of such simple approaches on treatment and outcomes has not been tested.
Given the prevalence of adult physical abuse among depressed women, further study is needed to determine whether the outcomes of care or the effectiveness of widely recommended treatments for depression are influenced by previous or current exposure to abuse.
Best care practices should encourage physicians to use specially tailored interventions for managing the course of care for depressed abused women, including consistent encouragement to take necessary actions to ensure safety. Unfortunately, current guidelines for depression care do not address domestic violence.38
Our findings are strengthened by the study's community-based sample, the high follow-up rate, and the extensive procedures we used to obtain a validated measure of health services use based on patient self-report and medical record review. However, because abuse and services use were both assessed retrospectively, recall bias may have affected the findings. A cohort study with prospective assessment of these key variables is needed to confirm our findings. Such a study would also be useful in untangling the causal relations between abuse and severity of physical and mental illness, which we were not able to address in this study. If social desirability bias led to underreporting of abusive incidents, the odds that recently abused women seek general medical care only for physical problems may be even greater than we report. In addition, we acknowledge limitations to the generalizability of our findings. Because we recruited our cohort using a telephone survey, we eliminated approximately 11% of the state's residents who were without a household telephone, one fourth of households with telephones that did not participate in the screening survey, and one third of eligible persons who screened positive for depression but refused to participate in the longitudinal study. Although the response rate is similar or better to that achieved in other community-based telephone surveys and health services studies, our results are less generalizable to very low income populations (presumably those without telephones) and older women living in nonurban areas.
In conclusion, because nearly all depressed women experiencing physical abuse sought general medical, rather than mental health care during the study year, general medical care screening for physical abuse appears to be a critical link to professional help for abused, depressed women. To aid this screening, research is needed to inform primary care guidelines about methods for increasing detection of abuse in depressed women.
SGIM Website
Please visit the Society of General Internal Medicine on their World-Wide Website. SGIM is located at
Acknowledgments
This research was supported by the National Institute of Mental Health funded grants MH48197 and MH54444 to the University of Arkansas and grant MH53817 to the University of Pittsburgh.
The authors acknowledge the contributions of Larry Wissow, Stacey Plichta, Carl Elliott, Jeff Smith, Stacy Fogle, Debbie Hodges, Dan Hoyt, Marki Kimball, Phylis Linkswiller, Cindy Mosley, Blair Tompkins, Ryan Turk, and the women who participated in this study.
References
- 1.Council on Scientific Affairs American Medical Association Violence against women: relevance for medical practitioners. JAMA. 1992;267:3184–9. [PubMed] [Google Scholar]
- 2.Plichta SB, Weisman CS. Spouse or partner abuse, use of health services, and unmet need for medical care in U.S. women. J Women's Health. 1995;4:45–53. [Google Scholar]
- 3.Golding JM. Sexual assault history and medical care seeking: the roles of symptom prevalence and illness behavior. Psychol Health 1996. In press [Google Scholar]
- 4.Golding JM. The cost of domestic violence to the health care system: exploratory paper on mental health consequences. In: Rice DP, Max W, Golding JM, Pinderhughes H, editors. The Cost of Domestic Violence to the Health Care System: Final Report to the Office of the Assistant Planning and Evaluation. Washington, DC: U.S. Department of Health and Human Services; 1996. In. [Google Scholar]
- 5.Gin NE, Rucker L, Frayne S, Cygan R, Hubbell FA. Prevalence of domestic violence among patients in three ambulatory care internal medicine clinics. J Gen Intern Med. 1991;6:317–22. doi: 10.1007/BF02597429. [DOI] [PubMed] [Google Scholar]
- 6.Abbott J, Johnson R, Koziol-McLain J, Lowenstein SR. Domestic violence against women: incidence and prevalence in an emergency department population. JAMA. 1995;273:1763–7. doi: 10.1001/jama.273.22.1763. [DOI] [PubMed] [Google Scholar]
- 7.Drossman DA, Leserman J, Nachman G, et al. Sexual and physical abuse in women with functional or organic gastrointestinal disorders. Ann Intern Med. 1990;113:828–33. doi: 10.7326/0003-4819-113-11-828. [DOI] [PubMed] [Google Scholar]
- 8.Hamberger LK, Saunders DG, Hovey M. Prevalence of domestic violence in community practice and rate of physician inquiry. Fam Med. 1992;24:283–7. [PubMed] [Google Scholar]
- 9.Helton AS, McFarlene J, Anderson ET. Battered and pregnant: a prevalence study. Am J Public Health. 1987;77:1337–9. doi: 10.2105/ajph.77.10.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Straus MA, Gelles RJ. Societal change and change in family violence from 1975 to 1985 as revealed by two national surveys. J Marriage Fam. 1986;48:465–79. [Google Scholar]
- 11.Schulman MA. A Survey of Spousal Violence Against Women in Kentucky. Washington, DC: U.S. Department of Justice, Law Enforcement Assistance Administration; 1979. [Google Scholar]
- 12.Smith MD. The incidence and prevalence of women abuse in Toronto. Violence Victims. 1987;2:173–87. [PubMed] [Google Scholar]
- 13.McCauley J, Kern DE, Kolodner K, et al. The “battering syndrome” prevalence and clinical characteristics of domestic violence in primary care internal medicine practices. Ann Intern Med. 1995;123:737–46. doi: 10.7326/0003-4819-123-10-199511150-00001. [DOI] [PubMed] [Google Scholar]
- 14.Bergman B, Brismar B. Suicide attempts by battered wives. Acta Psychiatr Scand. 1991;83(5):380–4. doi: 10.1111/j.1600-0447.1991.tb05560.x. [DOI] [PubMed] [Google Scholar]
- 15.Ratner PA. The incidence of wife abuse and mental health status in abused wives in Edmonton, Alberta. Can J Public Health. 1993;84:246–9. [PubMed] [Google Scholar]
- 16.Wilson MI, Daly M. Male sexual proprietariness and violence against wives. Cur Directions Psychol Sci. 1996;5:2–7. [Google Scholar]
- 17.Smith PH, Earp JA, DeVellis R. Measuring battering: development of the Women's Experience with Battering (WEB) scale. Women's Health. 1995;1:273–88. [PubMed] [Google Scholar]
- 18.Burnam MA, Wells KB, Leake B, Landsverk J. Development of a brief screening instrument for detecting depressive disorders. Med Care. 1988;26:775–89. doi: 10.1097/00005650-198808000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Straus MA. Measuring intrafamily conflict and violence: the Conflict Tactics (CT) Scales. J Marriage Fam. 1979;February:75–88. [Google Scholar]
- 20.Straus MA. The Conflict Tactics Scales and its critics: an evaluation and new data on validity and reliability. In: Straus MA, Gelles RJ, editors. Physical Violence in American Families: Risk Factors and Adaptation to Violence in 8,145 Families. New Brunswick, NJ: Transaction; 1996. 49–73. [Google Scholar]
- 21.U.S. Department of Commerce . Statistical Abstract of the U.S. Washington, DC: U.S. Department of Commerce; 1994. [Google Scholar]
- 22.Sherbourne CD, Stewart AL. The MOS Social Support Survey. Soc Sci Med. 1991;32:705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 23.Zimmerman M. A self-report scale to diagnose major depressive disorder. Arch Gen Psychiatry. 1986;43:1076–81. doi: 10.1001/archpsyc.1986.01800110062008. [DOI] [PubMed] [Google Scholar]
- 24.Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38:381–9. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 25.Pfohl B, Langdehn D. Iowa Personality Disorder Screen: Version 1.1. Ames. Iowa: University of Iowa, Department of Psychiatry; 1993. [Google Scholar]
- 26.Wells KB, Stewart A, Hays RD, et al. The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA. 1989;262:914–9. [PubMed] [Google Scholar]
- 27.Elliott BA, Johnson MMP. Domestic violence in a primary care setting: patterns and prevalence. Arch Fam Med. 1995;4:113–9. doi: 10.1001/archfami.4.2.113. [DOI] [PubMed] [Google Scholar]
- 28.Saunders DG, Kindy P. Predictors of physicians' responses to woman abuse: the role of gender, background, and brief training. J Gen Intern Med. 1993;8:606–9. doi: 10.1007/BF02599714. [DOI] [PubMed] [Google Scholar]
- 29.Friedman LS, Samet JH, Roberts MS, Hudlin M, Hans P. Inquiry about victimization experiences: a survey of patient preferences and physician practices. Arch Intern Med. 1992;152:1186–90. doi: 10.1001/archinte.152.6.1186. [DOI] [PubMed] [Google Scholar]
- 30.Currier GW, Barthauer LM, Begier E, Bruce ML. Training and experience of psychiatric residents in identifying domestic violence. Psychiatr Serv. 1996;47:529–30. doi: 10.1176/ps.47.5.529. [DOI] [PubMed] [Google Scholar]
- 31.Randall T. ACOG renews domestic violence campaign, calls for changes in medical school curricula. JAMA. 1992;267:3131. [PubMed] [Google Scholar]
- 32.Novello AC, Rosenberg M, Saltzman L, Shosky J. From the Surgeon General, U.S. Public Health Service: a medical response to domestic violence. JAMA. 1992;267:3132. doi: 10.1001/jama.267.23.3132. [DOI] [PubMed] [Google Scholar]
- 33.Kellermann AL. Domestic violence and the internist's response: advocacy or apathy. J Gen Intern Med. 1990;5:89–90. doi: 10.1007/BF02602317. [DOI] [PubMed] [Google Scholar]
- 34.Alpert EJ. Violence in intimate relationships and the practicing internist: new “disease” or new agenda? Ann Intern Med. 1995;123:774–81. doi: 10.7326/0003-4819-123-10-199511150-00006. [DOI] [PubMed] [Google Scholar]
- 35.Ferris LE. Canadian family physicians' and general practitioners' perceptions of their effectiveness in identifying and treating wife abuse. Med Care. 1994;32:1163–72. doi: 10.1097/00005650-199412000-00001. [DOI] [PubMed] [Google Scholar]
- 36.National Academy of Sciences. Violence in Families: Assessing Prevention and Treatment Programs. Washington, DC: National Academy Press; 1998. [Google Scholar]
- 37.Freund KM, Bak SM, Blackhall L. Identifying domestic violence in primary care practice. J Gen Intern Med. 1996;11:44–6. doi: 10.1007/BF02603485. [DOI] [PubMed] [Google Scholar]
- 38.Depression Guideline Panel. Depression in Primary Care: Volume 2. Treatment of Major Depression. Clinical Practice Guideline, Number 5. Rockville, Md: Public Health Service, Agency for Health Care Policy and Research; 1993. [Google Scholar]


