Abstract
OBJECTIVE
To assess the effect of a physician and pharmacist teamwork approach to uncontrolled hypertension in a medical resident teaching clinic, for patients who failed to meet the recommended goals of the fifth Joint National Commission on Detection, Evaluation and Treatment of High Blood Pressure.
HYPOTHESIS
Physician and pharmacist teamwork can improve the rate of meeting national blood pressure goals in patients with previously uncontrolled hypertension.
DESIGN
A single-blinded randomized controlled trial lasting 6 months.
SETTING
A primary care outpatient teaching clinic.
PATIENTS
A sample of 95 adult hypertensive patients who failed to meet national blood pressure goals based on three consecutive visits over a 6-month period.
INTERVENTION
Patients were randomly assigned to a control arm of standard medical care or to an intervention arm in which a physician and pharmacist worked together as a team.
MAIN RESULTS
At study completion, the percentage of patients achieving national goals due to intervention was more than double the percentage in the control arm (55% vs 20%, p < .001). Systolic blood pressure declined 23 mm Hg in the intervention arm versus 11 mm Hg in the control arm (p < .01). Diastolic blood pressure declined 14 and 3 mm Hg in the intervention and control arms, respectively (p < .001). The intervention worked equally as well in men and women and demonstrated noticeable promise in a minority of mixed-ancestry Hawaiians in whom hypertension is of special concern.
CONCLUSIONS
Patients who fail to achieve national blood pressure goals under standard outpatient medical care may benefit from a program that includes a physician and pharmacist teamwork approach.
Keywords: blood pressure, coronary heart disease, risk factor, pharmacist, ambulatory care
Guidelines from the fifth report of the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure (JNC-V) recommend prescribing pharmacologic intervention for the treatment of patients with hypertension when 3 months of lifestyle modification fails to lower systolic or diastolic blood pressure below 140 or 90 mm Hg, respectively.1 Published recommendations also provide for physician discretion to withhold drug therapy from patients with diastolic blood pressure less than 95 mm Hg or systolic blood pressure less than 150 mm Hg in the absence of target organ damage and other cardiovascular risk factors.
According to the JNC-V criteria, up to 50 million Americans are estimated to be hypertensive. Among those being medically treated for hypertension, it is further estimated that 71% fail to achieve JNC-V goals.1, 2 A third (36%) are thought to have blood pressures that exceed even higher thresholds of 160 mm Hg for systolic blood pressure and 95 mm Hg for diastolic blood pressure.2
Because of the widespread failure to reduce the prevalence of hypertension and to reach the goals established by the JNC-V, arguments have been made for the development and implementation of focused programs to effectively lower blood pressure at the local level.3–5 The purpose of this report is to describe such an effort that was undertaken to evaluate the benefits of a coordinated interaction between a physician and a pharmacist consultant in controlling hypertension in patients who failed to meet the goals defined by the JNC-V.
METHODS
Patient Enrollment
This single-blinded clinical trial was performed at the Queen Emma Clinic, a teaching clinic associated with the John A. Burns School of Medicine at the University of Hawaii. The clinic, located at The Queen's Medical Center, serves approximately 10,000 mostly indigent patients from the metropolitan area of Honolulu.
Study enrollment occurred over a 1-year period beginning in October 1993 in an unselected sample of patients who visited the Queen Emma Clinic. During this time, patients were interviewed and asked to participate in the study if they had uncontrolled hypertension during treatment on three consecutive visits to the clinic in the previous 6 months. Here, hypertension was diagnosed according to JNC-V guidelines. In the absence of target organ damage and cardiovascular risk factors, hypertension was defined as including systolic blood pressures at or above 150 mm Hg or diastolic blood pressures at or above 95 mm Hg. When target organ damage or cardiovascular risk factors were present, hypertension was defined as including systolic blood pressures exceeding 140 mm Hg or diastolic blood pressures exceeding 90 mm Hg. The JNC-V guidelines for the definition of hypertension are further described elsewhere.1
Patients were not asked to participate in the study if they had medical conditions that would prevent them from receiving standard medical care or if they were unable to provide informed written consent. Procedures followed were in accordance with institutional guidelines and approved by The Queen's Medical Center Institutional Review Committee. Written informed consent was obtained from all study participants. During recruitment to the study, patients were informed that the purpose of the study was to gauge the effect of pharmacy personnel on their hypertension. Patients were informed that they would be assigned to a study group or a control group. Patients were asked to permit a pharmacist to speak to them about their medications and treatment in the event of their assignment to the treatment group. They were informed that the pharmacist might or might not speak to them. They were not told when the pharmacist would speak to them during the course of the study. They were informed that if they were assigned to the control group, they would continue to see their doctor (or doctors) and receive their treatments as usual. After enrollment, patients were not informed whether they were enrolled in the intervention or control arm. Patients assigned to the control group were told that a pharmacy clerk would be available to answer their questions, and that if they had questions, they could speak to the clerk.
Enrollment was limited to 100 patients who were randomized with equal allocation to one of two physician group practices. One physician group comprised the treatment or intervention group and the other physician group comprised the control or standard medical care group. Patients were allocated to treatment or control group using the last digit of their social security numbers. Patients with even numbers were assigned to the study group practice. Patients with odd numbers were assigned to the control group practice. Within each group practice, there were five attending physicians, five third-year medical residents, four second-year medical residents, and six medical interns. Patients were treated exclusively by the physicians from the group practice to which they were assigned. During the course of the study, physicians did not migrate between the group practices. Assignment to the treatment or control arm occurred at the time of the initial patient interview, and follow-up within each arm lasted for 6 months.
Twenty-three patients in the study group and 13 patients in the control group were entered in a similar study to determine the effect of a physician-pharmacist team in the management of hypercholesterolemia, which has been previously described.6
Intervention Arm
In the intervention arm, a pharmacist interacted with physicians and patients on each visit to optimize antihypertensive pharmacologic therapy. During such visits, patients in the intervention arm met with the pharmacist for half an hour before seeing their physician (a resident or intern). At that time, the pharmacist took a medication history, answered questions, and encouraged compliance. The pharmacist did not refer the patient to other health care professionals or offer instruction in self-monitoring of blood pressure.
After meeting with the patient, the pharmacist reviewed pertinent laboratory data with the resident or intern who would be seeing the patient. The pharmacist attached recommendations to the front of the patient chart regarding the least costly antihypertensive regimen likely to be effective. The resident or intern then saw the patient, formulated a treatment plan, and discussed proposed strategies with a supervising attending physician. The resident and attending physician also discussed the pharmacist's recommendations and whether to accept or reject them as part of an overall treatment plan. The physicians also considered secondary causes of hypertension, the presence of other cardiovascular risk factors, individual patient circumstances and preferences, lifestyle and dietary patterns, health conditions unrelated to hypertension, and possible referral to other health care professionals.
Control Arm
Patients in the control arm received the same medical care as those in the intervention arm with the exception of the coordinated input from the pharmacist. Such care defines the standard medical practice that was observed at the Queen Emma Clinic during the time of the study. Standard medical practice in either arm, however, included patient access to a pharmacy clerk to answer questions about medication. Unlike the intervention arm, access to the pharmacy clerk in the control arm needed to be initiated by the patient.
Blood Pressure Determinations
Blood pressure levels were measured at the beginning and end of the 6 months of the study by nurses who were blinded to the patient's treatment assignment. Patients were not allowed to smoke or ingest caffeine within 30 minutes before the measurement. Care was taken to ensure that the bladder of the blood pressure cuff encircled the arm by at least 80%. On each occasion, two blood pressure measurements were taken from the right arm with a standard mercury sphygmomanometer after the patient had been sitting quietly for 5 minutes. The results were averaged to give a final blood pressure value that is used in this report.
Outcome Measures
The primary outcome measure after 6 months of follow-up was the percentage of patients who reached blood pressure goals established by the JNC-V.1 Here, a goal was achieved if the average of two systolic blood pressures fell below 140 mm Hg and the average of two diastolic blood pressures fell below 90 mm Hg. Other outcome measures included the absolute change in the average of two systolic and diastolic blood pressures measurements made at the time when the study began and 6 months later.
Statistical Methods
When examining the effect of treatment on the percentage of patients who achieved JNC-V blood pressure goals, comparisons between the control and the intervention arms were based on analyses of 2 × 2 contingency tables (including χ2and Fisher's Exact tests).7 Two-sample Student's t tests were used to compare absolute changes in systolic and diastolic blood pressures between the study groups.7 Contingency table methods and two-sample t tests were also used to evaluate the effect of randomization on producing control and intervention groups that were similar when the study began. To determine if baseline levels of systolic or diastolic blood pressure levels could account for any effects that might be observed within or between groups, logistic regression and analysis of covariance models were used.8 All hypothesis testing was conducted at a two-sided level of significance.
RESULTS
Fifty-five women and 40 men completed the study. One patient in the intervention arm died. One patient in the control group was lost to follow-up, and three failed to return for a final blood pressure measurement but were known to be alive at the close of the study. The final sample included 46 and 49 subjects in the control and intervention arms, respectively.
Table 1 provides the mean age at the time of study enrollment and the number of subjects with various demographic characteristics in the control and intervention groups. The mean age was nearly identical between the two groups (mean 55 ± SD 13 years). For those in the control arm, ages ranged from 28 to 83 years, and for those in the intervention arm, ages ranged from 22 to 83 years. Except for income, there were no significant differences between patients randomized to either arm of the study. Patients assigned to the control arm tended to fall in the higher income categories (p < .05). Among the other features of the study sample, 25% were mixed-ancestry Hawaiian, 57% were high school graduates, and most (87%) had some form of health insurance.
Table 1.
Mean Age and the Number of Subjects with Various Demographic Characteristics in the Control and Intervention Groups
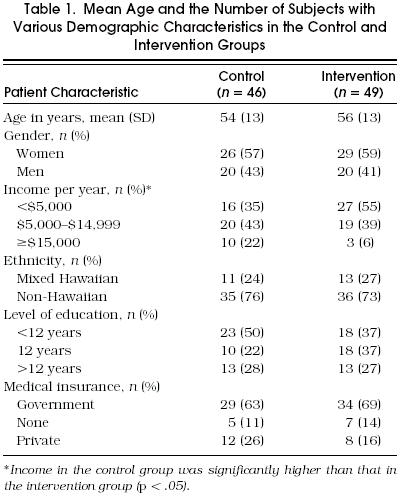
Table 2 provides a summary of baseline health characteristics for the control and intervention arms. Here, there were no significant group differences among the characteristics. Overall, the mean systolic blood pressure ± SD at study enrollment was 155 ± 21 mm Hg, and the starting diastolic blood pressure ± SD was 95 ± 9 mm Hg. Among the 95 patients who completed the study, 72 were receiving hypertensive medication at the outset of the study, 21 smoked cigarettes, and 28 consumed alcohol. Despite having uncontrolled hypertension, 38 considered their health to be excellent or good.
Table 2.
Patient Baseline Health Characteristics in the Control and Intervention Groups*
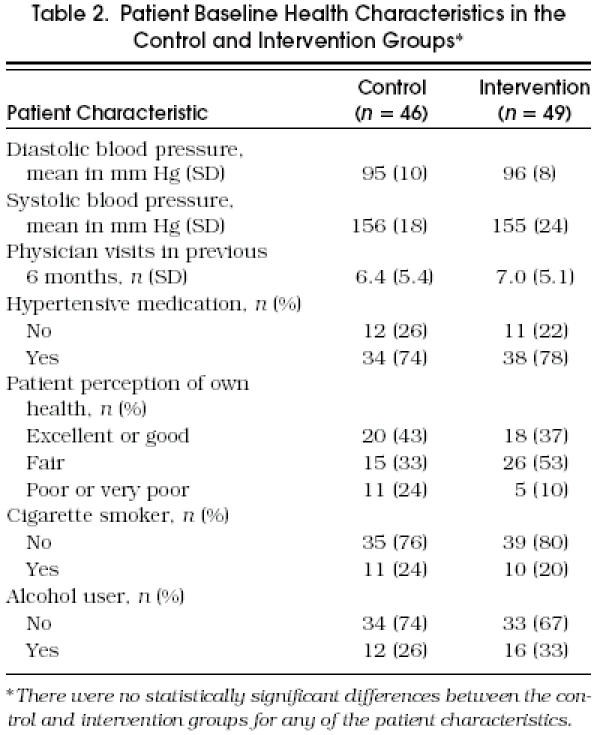
Figure 1 describes the overall rate of success in achieving JNC-V goals. Overall, 55% of the patients in the intervention arm achieved their JNC-V goal as compared with 20% of those in the control arm (p < .001). We also examined the effect of including the five patients who had no evaluable follow-up data by considering a worst-case scenario. Here, we examined the effect of the intervention if the one patient from the intervention arm had failed to achieve his JNC-V goal and if JNC-V goals had been achieved in the four lost to follow-up in the control arm. Even in this situation, the effect of the intervention remained statistically significant (p < .01).
Figure 1.
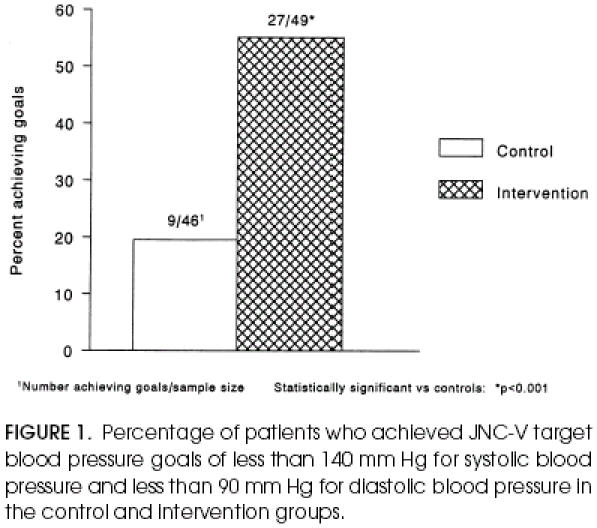
Percentage of patients who achieved JNC-V target blood pressure goals of less than 1 40 mm Hg for systolic blood pressure and less than 90 mm Hg for diastolic blood pressure in the control and intervention groups.
Figure 2 illustrates the absolute mean reduction in systolic and diastolic blood pressures observed over the 6 months of follow-up within the control and intervention groups. Diastolic blood pressure declined an average ± SD of 14 ± 11 mm Hg in the intervention arm and 3 ± 11 mm Hg in the control arm (p < .001). Systolic blood pressure declined an average ± SD of 23 ± 22 mm Hg in the intervention arm and 11 ± 23 mm Hg in the control arm (p < .01).
Figure 2.
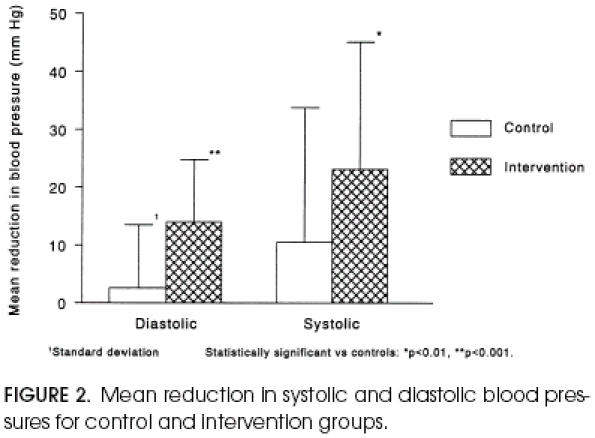
Mean reduction in systolic and diastolic blood pressures for control and intervention groups.
The positive effects of the intervention appeared to be unrelated to age and gender. The intervention was also effective in a minority of mixed-ancestry Hawaiians: 8 (62%) of 13 mixed-ancestry Hawaiians in the intervention arm achieved JNC-V goals, compared with 2 (18%) of 11 in the control arm (p < .05).
The pharmacist made a total of 162 recommendations to physicians. Thirteen were for laboratory monitoring while on medication, 10 were for new (additional) medication to be prescribed, and 34 were for an increase in medication dosage. There were 12 recommendations to discontinue medication and 5 to reduce medication dosage because of untoward effects. In 16 instances, recommendations were made to renew medication at an existing dose. Fifty-two recommendations were made to switch to a less expensive drug or less expensive formulation of the current drug. There were 20 recommendations to switch to a drug or formulation that was felt to be of more potential effectiveness.
Among the 162 recommendations, 12 (7.4%) were declined by physicians: there were 5 refusals to change to a less expensive drug, 2 to increase a drug dose, 2 to start a new medication, 1 to check a serum potassium level, and 2 to decrease medication dosages. Of the patients in whom a recommendation was declined, 5 (63%) of 8 met their JNC-V goal, with a mean drop in the systolic blood pressure of 16.7 mm Hg and a mean drop in the diastolic blood pressure of 8.6 mm Hg.
In all study patients, the pharmacist first emphasized diet, lifestyle modification, and compliance with the prescribed medical regimen. Almost half of the patients (23) in the study group were maintained on the same medication with the same dose or with a dose reduction during the study. Of these, 15 (65%) met JNC-V goals. Five patients had an existing dose of medication increased. Four (80%) of these met JNC-V goals. The remaining 22 patients were switched to a new medication because of side effects, failure to achieve a blood pressure goal, or cost reduction. Of these, 11 (50%) achieved JNC-V goals.
Twelve patients in the control group were not treated with a drug at the time of enrollment. Six (50%) of these were started on antihypertensive medications during the course of the study. There were 11 patients in the study group who were not treated with a drug initially, and 5 (45%) were started on antihypertensive medications during the course of the study.
Among factors affecting costs in the current study, mean medication charges dropped $6.80 per patient from the first month in the intervention group. There was a $6.50 increase in the control group. Physician visits during the course of the study, referral to a dietitian, emergency department visits, and hospitalizations were nearly identical in the intervention and control arms.
There were 13 patients in the control group and 23 in the study group who were entered in a similar study to ascertain the effect of a physician-pharmacist team in the management of hypercholesterolemia.6 The effects of the intervention on achieving JNC-V goals were nearly identical in those enrolled and those not enrolled in this study (p < .05 in each instance). Effects on reducing systolic and diastolic blood pressure were also similar, although reductions in systolic blood pressure were no longer statistically significant when analyzed separately for each group, presumably owing to a loss of power. In contrast, the intervention continued to have a significant effect on reducing diastolic blood pressure (p < .01) in those enrolled as well as those not enrolled in the cholesterol study.
DISCUSSION
In addition to the findings reported here, others have shown similar effects involving increased patient and physician interaction with a pharmacist in approaching uncontrolled hypertension. One group demonstrated the effectiveness of a consulting clinical pharmacist in an unblinded clinical trial.9 Patients were described as mostly noncompliant at the time of study enrollment with blood pressures exceeding 160 mm Hg for systolic blood pressure or 90 mm Hg for diastolic blood pressure. Working semiautonomously, the pharmacist saw patients without a physician, encouraged compliance, answered questions, managed mild drug reactions without consultation, and referred patients to other specialized personnel when necessary. The system resulted in improvement in patient knowledge about hypertension, compliance with therapy, and more frequent control of blood pressure. In another report, the effect of a pharmacist intervention for the control of resistant hypertension was also shown to have benefits in lowering blood pressure,10 although reported findings were criticized because of the absence of a control group.11
To our knowledge, the current study is the first that is based on findings from a controlled clinical trial in which efforts were made to mask patients to treatment assignment. Unlike earlier reports, the current study suggests that a physician-pharmacist team approach to uncontrolled hypertension can work equally well in men and women. Positive effects also appeared to be unrelated to age. In addition, the intervention demonstrated noticeable promise in a minority of mixed-ancestry Hawaiians. Here, 8 (62%) of 13 in the intervention arm achieved JNC-V goals as compared with 2 (18%) of 11 in the control arm (p < .05). Although this is a small series of patients, the result suggests that a team approach between physicians and pharmacists may have positive effects even in high-risk minorities in whom control of hypertension is especially difficult to achieve.12, 13
We attempted to design and conduct a controlled randomized clinical trial; however, the process used for patient allocation cannot be considered random in a strict sense. Patients were entered in the study group if their social security number was even, and into the control group if it was odd. The nature of this system raises the possibility that the person entering patients could figure out the system and deliberately withhold patients from entry if their social security number was “wrong.” However, we believe that this type of selection did not occur, as the protocol required that all patients were asked to enter when they came to the clinic if they met explicit entry criteria without meeting explicit exclusion criteria. Baseline characteristics were analyzed after all patients were entered, and the intervention and control groups of patients were found to be comparable.
Blinding was also difficult to guarantee, although patient access to a clerk pharmacist as part of standard medical care might have helped make it difficult for patients to distinguish between the control and intervention arms.
The intervention was conducted in a resident teaching clinic, and the results may not be generalizable to nonteaching practices. The success of an intervention program is bound to depend on how aggressively it is implemented. With considerable emphasis on levels of personal interaction in the intervention arm in the current study, sustained positive rapport among physicians, pharmacist, and patient is likely to be an important factor in achieving success in similar intervention strategies. As the physician and pharmacist were aware of their roles in the current study, it is possible that they were also more eager to cooperate and respect opposing opinions more often than would be the case in a general day-to-day setting.
Agreement between the physician and pharmacist on a strategy to lower blood pressure is also likely to be critical in avoiding conflicting messages of importance on blood pressure management to a patient. In the current study, agreement appeared to be high. Here, 145 (92%) of the 157 recommendations made by the pharmacist were accepted by the physician. Among the recommendations, most were for suggestions to switch to a less expensive or better drug or formulation (72) or for increases in the dose of a drug (24). Of the recommendations that were denied, no single type of recommendation appeared to dominate.
Although the benefits of increased teamwork between physicians and pharmacists seem promising in improving patient management of hypertension, implementation of such intervention programs in a general clinic setting is not without cost. Despite the modest and possibly favorable effect of the intervention on the cost of monthly medication observed in this study, the greatest burden in implementing an intervention program similar to the one considered in this report is in directing physician and pharmacist time away from other activities to more concerted efforts of teamwork and patient interaction. Although difficult to measure, decreases in the risk of cardiovascular morbidity and mortality that would accompany the anticipated declines in the prevalence of hypertension could result in substantial savings that would warrant implementation of coordinated efforts to lower blood pressure by physicians, pharmacists, and possibly other health care personnel.
Finally, it is intriguing to speculate why the intervention worked even in patients who had no change or a decrease in their blood pressure medication. In these patients, compliance, changes in diet, reduction in alcohol consumption, and weight reduction may have been important. To affect these variables, the discipline of the nonphysician team member might not matter as much as the time invested in increased individualized attention to patients. Further research is needed to clarify what sort of team member could provide the most cost-effective improvements in the control of hypertension.
Acknowledgments
This work was supported by a grant from the Queen's Medical Center, Honolulu, Hawaii and by a Research Centers in Minorities Institutions Award (P20 RR 11091) from the National Institutes of Health.
References
- 1.The Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure. The fifth report of the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure (JNC V) Arch Intern Med. 1993;153:154–83. [PubMed] [Google Scholar]
- 2.Trends in the prevalence, awareness, treatment and control of hypertension in the adult US population Data from the health examination surveys, 1960 to 1991. Hypertension. 1995;26:60–9. doi: 10.1161/01.hyp.26.1.60. [DOI] [PubMed] [Google Scholar]
- 3.Kosecoff J, Kanouse DE, Rogers WH, et al. Effects of the National Institutes of Health Consensus Development Program on physician practice. JAMA. 1987;258:2708–13. [PubMed] [Google Scholar]
- 4.Lomas J, Anderson GM, Domnick-Pierre K, et al. Do practice guidelines guide practice? N Engl J Med. 1989;321:1306–11. doi: 10.1056/NEJM198911093211906. [DOI] [PubMed] [Google Scholar]
- 5.Avorn J, Soumerai SB. Improving drug therapy decisions through educational outreach: a randomized controlled trial of academically based “detailing.”. N Engl J Med. 1983;308:1457–63. doi: 10.1056/NEJM198306163082406. [DOI] [PubMed] [Google Scholar]
- 6.Bogden P, Koontz L, Williamson P, Abbott R. The physician and pharmacist team: an effective approach to cholesterol reduction. J Gen Intern Med. 1997;12:158–64. doi: 10.1007/s11606-006-5023-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Netter J, Wasserman W. Applied Linear Statistical Models. Homewood, Ill: Richard D. Irwin; 1974. [Google Scholar]
- 8.Rosner B. Fundamentals of Biostatistics. Boston, Mass: PWS Kent Publishing Co; 1993. [Google Scholar]
- 9.Morse GD, Douglas JB, Upton JH, et al. Effect of pharmacist intervention on control of resistant hypertension. Am J Hosp Pharm. 1986;43:905–9. [PubMed] [Google Scholar]
- 10.Monteagudo FSE, Robins AH, Barnett L. Questioning the proof for effectiveness of pharmacist intervention in blood pressure control. Am J Hosp Pharm. 1987;44:69–70. [PubMed] [Google Scholar]
- 11.McKenney JM, Slining JM, Henderson HR, et al. Effect of clinical pharmacy services on patients with essential hypertension. Circulation. 1973;48:1104–11. doi: 10.1161/01.cir.48.5.1104. [DOI] [PubMed] [Google Scholar]
- 12.Curb JD, Aluli NE, Kautz JA, et al. Cardiovascular risk factor levels in ethnic Hawaiians. Am J Public Health. 1991;81:164–7. doi: 10.2105/ajph.81.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Braun KL, Look MA, Tsark JA. High mortality rates in Native Hawaiians. Hawaii Med J. 1995;54:723–9. [PubMed] [Google Scholar]


