Abstract
OBJECTIVE
To determine the value of conjunctival pallor in ruling in or ruling out the presence of severe anemia (hemoglobin ≤ 90 g/L) and to determine the interobserver agreement in assessing this sign.
DESIGN
Patients were prospectively assessed for pallor by at least one of three observers. All observations were made without information of the patient's hemoglobin value or of another observer's assessment.
SETTING
Tertiary–care, university-affiliated teaching hospital.
PATIENTS
Three hundred and two medical and surgical inpatients.
MEASUREMENTS AND MAIN Results
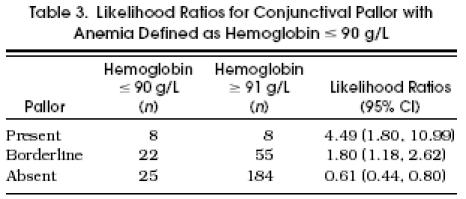
Likelihood ratios (LRs) calculated for conjunctival pallor present, borderline, and absent were as follows: pallor present, LR 4.49 (95% confidence interval [CI] 1.80, 10.99); pallor borderline, LR 1.80 (95% CI 1.18, 2.62); pallor absent, LR 0.61 (95% CI 0.44, 0.80). Kappa scores of interobserver agreement between paired observers were 0.75 and 0.54.
CONCLUSIONS
The presence of conjunctival pallor, without other information suggesting anemia, is reason enough to perform a hemoglobin determination. The absence of conjunctival pallor is not likely to be of use in ruling out severe anemia. With well-defined criteria, interobserver agreement is good to very good.
Keywords: conjunctival pallor, anemia, physical diagnosis, likelihood ratios
When an internist evaluates a patient in an ambulatory setting, anemia may be considered in a variety of clinical scenarios. In this context, a physical finding that would alert the physician that the patient is very likely to have severe anemia would be valuable. If such a finding were present, the clinician would most certainly obtain a laboratory determination of the hemoglobin level. Conversely, if such a finding were absent, the clinician may be able to conclude, on the basis of physical examination alone, that severe anemia need not be considered further.
The precise level of hemoglobin that would be considered severe or would warrant more urgent investigation depends on a number of factors including the chronicity of the anemia and the presence of comorbid conditions such as coronary artery disease. A hemoglobin level of 90 g/L or below might warrant such attention.
Signs traditionally used in the physical diagnosis of anemia are pallor of the conjunctivae, nail beds, face, palms, and palmar creases.1 Of these, only pallor of the conjunctivae, nail beds, and palms can be used in patients of any race. Current evidence suggests that conjunctival pallor may be a more accurate indicator of the presence or absence of anemia than pallor of the palms or nail beds.2 In addition, conjunctival pallor has been documented to appear more frequently in patients with severe anemia, and hence may be more sensitive than other signs.3
Previous studies, however, are limited by small sample sizes, examining only white males, reporting results without confidence intervals (CIs), and preselecting patients to ensure that there were equal numbers with and without anemia.2,3 In a previous prospective study with a larger sample size, the various signs in the clinical diagnosis of anemia were considered as an aggregate and results were not reported for individual signs.4 Furthermore, conjunctival pallor has been considered as a dichotomous variable—that is, either present or absent—when in fact there may be cases in which pallor is neither clearly present nor absent.
Therefore, there were two principal objectives of this study. First, we sought to determine the value of the presence of conjunctival pallor in ruling in, and the value of the absence of conjunctival pallor in ruling out, the presence of severe anemia defined as a hemoglobin concentration of 90 g/L or less. Second, we sought to determine the interobserver agreement in assessing this sign. Also, we were interested in exploring how the operating characteristics of conjunctival pallor varied for different hemoglobin level cutoffs.
METHODS
We prospectively assessed 302 medical and surgical inpatients at The Toronto Hospital, a tertiary-care teaching hospital, for conjunctival pallor. Patients were included in the study if they were over 18 years of age, able to consent, and willing to participate. Patients were excluded if they had not had a laboratory measurement of hemoglobin level within 3 days of our clinical assessment or had a transfusion between their last blood sample and our clinical assessment. The study was approved by The Toronto Hospital Research Ethics Committee, and informed written or verbal consent was obtained from all participants.
At the outset, 25 patients were seen by three observers together to standardize assessments. Pallor was classified as being present, borderline, or absent. Subsequent patients were assessed by at least one of three observers, without information of the patient's hemoglobin value or of another observer's assessment (in cases in which there were more than one observer). Observers A and B were medical students at various stages of training, and observer C was an experienced general internist. Pale conjunctivae were those with very little or no evidence of red color on the anterior rim, which matched the fleshy color of the posterior aspect of the palpebral conjunctiva, as seen in Figure 1. Conjunctivae that were normal had full or nearly full redness of the anterior rim, as seen in Figure 2. Borderline conjunctivae were those with neither clearly red nor clearly pale anterior rims or those in which one conjunctiva was pale and the other was normal.
FIGURE 1.

Pale conjunctiva. Note that the color of the pale anterior rim and the posterior part of the conjunctiva are the same.
FIGURE 2.

Normal conjunctiva. Note the full reddness of the anterior rim and its dissimilarity to the posterior aspect of the conjunctiva.
Before examination, the patients’ age, gender, date of last blood sample, and date of last transfusion (if received) were obtained. Conjunctivae were examined under as much natural light as possible. When natural light was insufficient, a small pen flashlight was used. For the 150 cases in which two observers assessed the same patient, observations were made within 30 minutes of each other. When the observers disagreed, the patient was reexamined and a consensus assessment was obtained. This consensus assessment was used in data analysis.
After examination, patients’ charts were reviewed for admitting diagnosis and the presence of HIV, malignancy, or sickle cell anemia. Hemoglobin levels were determined by an individual other than the observers.
To analyze the accuracy of conjunctival pallor, we used a Bayesian conceptual framework.5 This approach involves the incorporation of new information, “the test result,” into risk information that is known before the test is done, “the pretest probability.” To convey the degree of added information used in revising the pretest probabilities when the physical diagnosis results are known, we used the method of likelihood ratios.6 That is, each level of the sign (pale, borderline, and normal) is associated with a specific likelihood ratio, which, when applied to the pretest probability, revises it to a posttest probability in either the upward or downward direction.
Likelihood ratios have two advantages over sensitivity and specificity, which are the traditional approaches to describing test characteristics. Likelihood ratios do not require that test results be divided simply into positive and negative, and one can use a simple nomogram to convert pretest probability into posttest probability without referring to Bayesian formulas.7 For a test with several types of results (for example, conjunctival pallor absent, borderline, and present), one would like to see a progression of likelihood ratios that starts very close to 0, virtually ruling out disease, and goes above 10, virtually ruling in disease.
In the present study, likelihood ratios with confidence intervals were determined using version 6 of Centor's receiver-operating characteristic (ROC) curve analyzer.8 Reliability was measured by a κ score of agreement between paired observers.9
RESULTS
Of the 338 patients who were approached, 10 refused to participate, and 23 were unable to consent due to language barriers or limitations imposed on them by their medical condition. Of the 305 patients remaining, 3 were excluded because they had not had a blood sample within 72 hours of clinical assessment. Therefore, 302 patients were included in the data analysis. Of these, 171 were male and 131 were female.
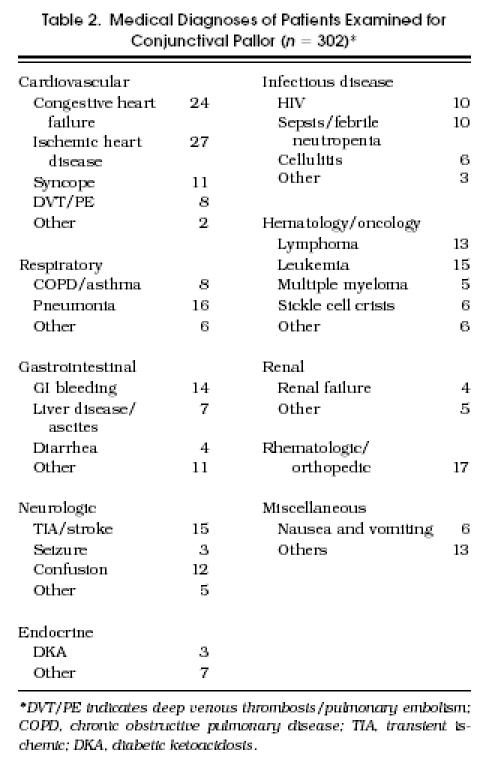
Some characteristics of the study participants are presented in Table 1. The medical diagnoses of the patients are shown in Table 2. HIV was present in 8%, malignancy in 19%, and sickle cell anemia in 2% of patients.
Table 1.
The Ages of Patients with and Without Severe Anemia
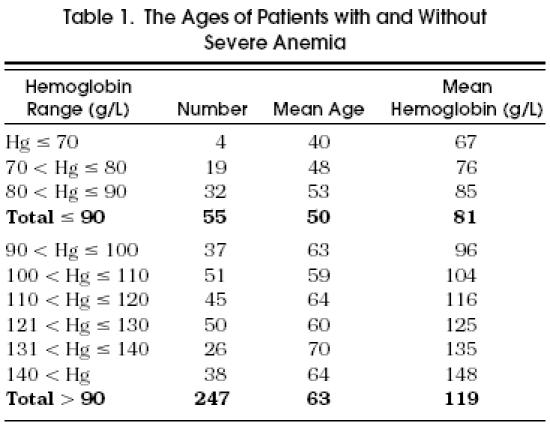
Table 2.
Medical Diagnoses of Patients Examined for Conjunctival Pallor (n = 302)*
Likelihood ratios with 95% CIs are presented in Table 3. For pallor present, the likelihood ratio was 4.49 for a hemoglobin less than or equal to 90 g/L. For borderline cases, the likelihood ratio was 1.80. For pallor absent, the likelihood ratio was 0.61. The area under the ROC curve was 0.70 ± 0.05.
Table 3.
Likelihood Ratios for Conjunctival Pallor with Anemia Defined as Hemoglobin ≤ 90 g/L
Scores for agreement between paired observers were κ = 0.75 between observers A and B and κ = 0.54 between observers A and C. Observers B and C did not see patients together.
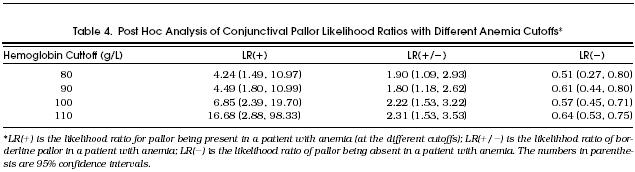
Post hoc analysis of the operating characteristics of conjunctival pallor at different hemoglobin cutoffs are presented in Table 4. For higher cutoff levels of anemia (100 g/L and 110 g/L), the positive likelihood ratio increases significantly. There is little change for the lower cutoff level of 80 g/L. The likelihood ratio for pallor absent does not vary significantly for the different hemoglobin cutoffs.
Table 4.
Post Hoc Analysis of Conjunctival Pallor Likelihood Ratios with Different Anemia Cutoffs*
DISCUSSION
Although the accuracy of conjunctival pallor in the diagnosis of anemia has been examined by others, those studies had several important limitations. Our study is different in that the sample was substantially larger, and patients of both genders were drawn from a racially heterogeneous population. Patients were not preselected for the study, and their medical diagnoses (Table 2) were those that the internist would be likely to encounter in an ambulatory setting. The larger sample allowed us to calculate likelihood ratios with smaller CIs. In addition, we defined pallor as a three-level variable, which we believe better reflects the spectrum of conjunctivae likely to be encountered.
A physical sign such as conjunctival pallor that can provide information about the presence of anemia during patient evaluation might be helpful. To rule in anemia with confidence, the presence of conjunctival pallor should have a likelihood ratio that is greater than 10 for predicting anemia. For example, typical angina has a likelihood ratio of 115 for predicting greater than 75% coronary artery stenosis,10 and right-lower-quadrant pain has a likelihood ratio of 3 for predicting appendicitis.11 In this study the presence of pallor had a likelihood ratio of only 4.49 for predicting anemia. With this likelihood ratio, when a clinician initially assesses a patient's probability of having anemia as 50% and then finds pale conjunctivae on physical examination, the probability of anemia increases to 82%. Although the finding of pale conjunctivae increases the probability of anemia, it does not permit a diagnosis of anemia, and there are few realistic situations in which the presence of pallor alone would allow the clinician to rule in anemia.
If we had defined anemia as a hemoglobin level less than or equal to 110 g/L, as we did in a post hoc analysis, the positive likelihood ratio would have been 16.68 (Table 4). With this likelihood ratio, when a clinician initially assesses a patient's probability of having anemia as 50% and then finds pale conjunctivae on physical examination, the probability of anemia increases to 94%. This probability may be sufficient to rule in the presence of anemia. This use of our data, however, should be approached with caution because these results were generated in a post hoc analysis and the CIs are wide (2.88, 98.33).
There are situations, however, in which the presence of pallor may be more helpful. For example, clinicians in the office often see patients whose probabilities of anemia are too low to justify ordering a hemoglobin determination to search for it. Even when using a likelihood ratio of 4.49, however, the presence of conjunctival pallor in such a patient can raise the probability of anemia high enough to make a hemoglobin determination worthwhile. For example, when a clinician initially assesses a patient's probability of having anemia as 1% and then finds pale conjunctivae on physical examination, the probability of anemia increases to 5%. Therefore, we conclude that finding pale conjunctivae in a patient without another reason for the patient to be anemic should lead the clinician to order a hemoglobin determination.
To rule out anemia with confidence, conjunctival pallor should have a small likelihood ratio when pallor is absent. For example, a near normal or totally normal lung perfusion scan has a likelihood ratio of 0.19, which decreases the probability of a pulmonary embolism in a clinically meaningful way.12 We found that the absence of pallor had a likelihood ratio of 0.61 when the hemoglobin cutoff level was 90 g/L. When a clinician initially assesses the patient's probability of anemia to be 50%, and then finds normal-colored conjunctivae, application of this likelihood ratio lowers the probability of anemia to 38%. Although the absence of pallor revises the probability of anemia downward, we believe the change is not clinically meaningful because the change is insufficient to rule out disease.
Presumably, a lower cutoff point for defining anemia should lead to a lower likelihood ratio for absent pallor. Although our post hoc analysis did show a decrease in the likelihood ratio from 0.61 to 0.51 when the cutoff point was decreased from 90 to 80 g/L (Table 4), the decrease does not change the probability of anemia enough to be clinically relevant.
Our study does not explain why patients with severe anemia did not always have pale conjunctivae. It is possible that an inflammatory process in the conjunctivae of some patients caused a “falsely” red color. Alternatively, the observers in this study may not have been sufficiently skilled to detect pallor when it was present.
Our scores of κ = 0.75 and 0.54 interobserver agreement about conjunctival pallor were slightly higher than the scores reported by others.2–4 Usually κ scores between 0.4 and 0.6 are interpreted as good agreement and those between 0.6 and 0.8 as very good agreement.6 The higher level of agreement in our study may have been a result of the standardizing examinations we carried out at the onset of the study. Our experience suggests that many conjunctivae are neither clearly pallid nor clearly normal, and it is likely that our three-level classification of pallor also enhanced agreement between observers.
There are several limitations to this study. First, although the population was racially heterogeneous, data on ethnic and racial background were not recorded and analyzed. Second, inexperienced medical students were among the evaluators in this study, although training and standardization were used to minimize their inexperience. Third, we studied only one possible sign for pallor. Pallor of the nail beds and palms are other signs that might have been studied. Fourth, we studied only inpatients, and our principal conclusion is directed at outpatients, although we do not know any reason why this discrepancy should be important.
We conclude that when anemia is defined as a hemoglobin concentration less than or equal to 90 g/L, conjunctival pallor adds information to the clinical decision-making process, although it cannot lead to a confident diagnosis in common clinical situations. This sign, however, without other information suggesting anemia, should be reason enough to order a hemoglobin determination. The absence of conjunctival pallor does not allow the clinician to rule out anemia, which means that physical diagnosis is not sufficient to exclude even severe anemia from consideration. Finally, with defined criteria, interobserver agreement for conjunctival pallor is good to very good.
REFERENCES
- 1.Bunn HF, Anemia . Harrison's Principles of Internal Medicine. In: Isselbacher KT, et al., editors. 13th ed. New York, NY: McGraw-Hill; 1994. p. 313. [Google Scholar]
- 2.Nardone DA, Roth KM, Mazur DJ, McAfee JM. Usefulness of physical examination in detecting the presence or absence of anemia. Arch Intern Med. 1990;150:201–4. [PubMed] [Google Scholar]
- 3.Strobach RS, Anderson SK, Doll DC, Ringenberg S. The value of the physical examination in the diagnosis of anemia. Arch Intern Med. 1988;148:831–2. [PubMed] [Google Scholar]
- 4.Gjorup T, Rugge PM, Hendriksen C, Jensen AM. A critical evaluation of the clinical diagnosis of anemia. Am J Epidemiol. 1986;124:657–65. doi: 10.1093/oxfordjournals.aje.a114438. [DOI] [PubMed] [Google Scholar]
- 5.Wong T, Detsky AS. Preoperative cardiac risk assessment for patients having peripheral vascular surgery. Ann Intern Med. 1992;116:743–53. doi: 10.7326/0003-4819-116-9-743. [DOI] [PubMed] [Google Scholar]
- 6.Sackett DL, Haynes RB, Guyatt GH, Tugwell P. Clinical Epidemiology: A Basic Science for Clinical Medicine. Boston, Mass: Little Brown and Co; 1991. [Google Scholar]
- 7.Fagan TL. Nomogram for Bayes's theorem. N Engl J Med. 1975;293:257. doi: 10.1056/NEJM197507312930513. [DOI] [PubMed] [Google Scholar]
- 8.Centor RM. A Visicalc program for estimating the area under a receiver operating characteristics (ROC) curve. Med Decis Making. 1985;5:139–48. doi: 10.1177/0272989X8500500203. [DOI] [PubMed] [Google Scholar]
- 9.Fleiss JL. 2nd ed. New York, NY: Wiley; 1981. Statistical Methods for Rates and Proportions; pp. 217–34. [Google Scholar]
- 10.Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary artery disease. N Engl J Med. 1979;300:1350–8. doi: 10.1056/NEJM197906143002402. [DOI] [PubMed] [Google Scholar]
- 11.Clinical Epidemiology Rounds The interpretation of diagnostic data, 5: how to do it with a simple math. Can Med Assoc J. 1983;129:947–54. [PMC free article] [PubMed] [Google Scholar]
- 12.PIOPED Value of the ventilation/perfusion scan in acute pulmonary embolism. JAMA. 1990;263:2753–9. doi: 10.1001/jama.1990.03440200057023. [DOI] [PubMed] [Google Scholar]


