Abstract
OBJECTIVE
Although physical function is believed to be an important predictor of outcomes in older people, it has seldom been used to adjust for prognosis or case mix in evaluating mortality rates or resource use. The goal of this study was to determine whether patients’ activity of daily living (ADL) function on admission provided information useful in adjusting for prognosis and case mix after accounting for routine physiologic measures and comorbid diagnoses.
SETTING
The general medical service of a teaching hospital.
PARTICIPANTS
Medical inpatients (n = 823) over age 70 (mean age 80.7, 68% women).
MEASUREMENTS
Independence in ADL function on admission was assessed by interviewing each patient’s primary nurse. We determined the APACHE II Acute Physiology Score (APS) and the Charlson comorbidity score from chart review. Outcome measures were hospital and 1-year mortality, nursing home use in the 90 days following discharge, and cost of hospitalization. Patients were divided into four quartiles according to the number of ADLs in which they were dependent.
MAIN RESULTS
ADL category stratified patients into groups that were at markedly different risks of mortality and higher resource use. For example, hospital mortality varied from 0.9% in patients dependent in no ADL on admission, to 17.4% in patients dependent in all ADLs. One-year mortality ranged from 17.5% to 54.9%, nursing home use from 3% to 33%, and hospital costs varied by 53%. In multivariate analyses controlling for APS, Charlson scores, and demographic characteristics, compared with patients dependent in no ADL, patients dependent in all ADLs were at greater risk of hospital mortality (odds ratio [OR] 13.7; 95% confidence interval [CI] 3.1–58.8), 1-year mortality (OR 4.4; 2.7–7.4), and 90-day nursing home use (OR 14.9; 6.0–37.0). The DRG-adjusted hospital cost was 50% higher for patients dependent in all ADLs. ADL function also improved the discrimination of hospital and 1-year mortality models that considered APS, or Charlson scores, or both.
CONCLUSIONS
ADL function contains important information about prognosis and case mix beyond that provided by routine physiologic data and comorbidities in hospitalized elders. Prognostic and case–mix adjustment methods may be improved if they include measures of function, as well as routine physiologic measures and comorbidity.
Keywords: prognosis, case mix, activities of daily living, severity, functional status
Physical function is believed to be an important predictor of hospital outcomes in older people, yet it has not been used extensively to adjust for prognosis or case mix in evaluating mortality rates or resource use. Most methods of adjusting for prognosis or case mix consider either measures of internal physiologic function, such as laboratory values and vital signs, or principal and comorbid diagnoses. However, measures of integrative functioning, such as physical, emotional, and cognitive functioning, may also be useful for prognostic and case–mix adjustment. The purpose of this study was to test the hypothesis that one example of integrative functioning, physical function, is useful as a measure of prognosis and case mix in elders hospitalized with acute medical illness. Although this hypothesis is supported by previous work demonstrating a relation between functional status and mortality,–10 measures of physical function have seldom been used to adjust for prognosis and case mix.
We tested the hypothesis in three steps using dependence in activities of daily living (ADL) as our measure of physical function.11 For outcomes, we used two measures of mortality (hospital and 1-year), as well as two measures of resource use (hospitalization cost and nursing home use). First, we tested whether the level of ADL function stratifies patients into groups with different risks of mortality and levels of resource use. Second, we assessed whether ADL function is predictive of mortality and resource use after adjusting for indices based on standard physiologic measures and comorbidities or diagnoses. Third, we assessed whether ADL function improves the ability of these other indices to discriminate patients at risk of mortality.
METHODS
Patients
This analysis includes subjects enrolled in two related longitudinal studies of functional change in older general medical patients hospitalized at University Hospitals of Cleveland, Ohio. The inclusion and exclusion criteria for these studies have been described previously.12 The first study enrolled patients aged 75 years or older admitted between March and July 1990. The second study, a controlled trial of an intervention to improve functional outcomes, enrolled patients aged 70 years or older admitted between November 1990 and March 1992. Patients admitted to intensive care units or subspecialty services were excluded. Of the 824 patients enrolled in the two studies, one patient was excluded from this analysis because of missing functional status information.
Data Collection
Within 48 hours of admission, each patient’s primary nurse was asked whether or not the patient was able to perform six different ADLs without assistance on admission. Nurses based their assessments on their experience in caring for the patient. Interrater reliability was not assessed. The six ADLs were bathing, dressing, grooming, transferring, eating, and toileting. A patient who required personal assistance for a particular ADL was classified as dependent in that ADL. We used patient reports about ADL function for the 21 patients (3%) for whom we were unable to interview their nurse. Data collected from chart review included the components of the admission APACHE II Acute Physiology Score (APS),13 the components of the Charlson comorbidity score,14 and demographic information. The APS is a prognostic measure based on laboratory and vital sign abnormalities. Although it was developed for use in the intensive care units (ICU), it is often used in other settings.15 We used the APS instead of the complete APACHE II score because the APS is a purer measure of internal physiologic abnormalities. Results using the entire APACHE II score were generally similar. The Charlson comorbidity score is a weighted prognostic index based on the number and severity of comorbid conditions.
We obtained information about discharge and 1-year mortality through follow-up interviews of patients and family members and a search of the national death index.16 We obtained information about hospital resource use from the hospital’s cost accounting records. Our hospital determines the cost of caring for each patient by using an accounting system that calculates the resource-based cost of each service or procedure a patient receives. We determined whether the patient spent time in a nursing home during the 90 days following discharge by interviewing patients and family members.
Analytic Strategy
We divided patients into four quartiles based on their number of dependent ADLs (0, 1–3, 4–5, or 6 dependent ADLs). The bivariate and multivariate results were similar when using different cutpoints for the ADL categories. We analyzed the relation between ADL quartile and four different outcomes: hospital mortality, 1-year mortality, cost of hospitalization, and nursing home use in the 90 days following discharge. Our analyses of hospitalization costs are based on log transformations of costs because hospital costs are highly skewed. Bivariable associations between mortality, nursing home use, and ADL quartile were assessed using the χ2 test, modified for linear trend. The bivariable association between hospital cost and ADL quartile was assessed using analysis of variance. We standardized the geometric mean cost of the patients dependent in no ADL to 100 units and report the relative costs of the other three function quartiles.
We used logistic regression to determine whether functional status in an independent predictor of mortality and nursing home use and linear regression to determine whether functional status is an independent predictor of hospital cost. For each regression model, the three quartiles representing the worst function were included as indicator variables, with the category of patients dependent in none of the six ADLs as the reference group. All models controlled for APS, Charlson score, and demographic characteristics (age, race, gender, and residence in a nursing home before admission). The hospital cost model also controlled for the Medicare estimate of mean hospital resource use expected for each patient using the diagnosis-related group (DRG) cost weight.17 The DRG cost weight represents the relative payment the hospital received for each patient from Medicare, based on the patient’s primary diagnosis.
Finally, we determined whether ADL function improved the discrimination of hospital and 1-year mortality models based on APS, on Charlson scores, and on both APS and Charlson scores by comparing receiver-operating characteristic (ROC) curve areas, calculated as the c statistic from logistic regression models. These models included ADL function as the number of dependent ADLs and did not include demographic variables. We compared the ROC areas of prognostic models with and without ADL function using the method of Hanley and McNeil.18
RESULTS
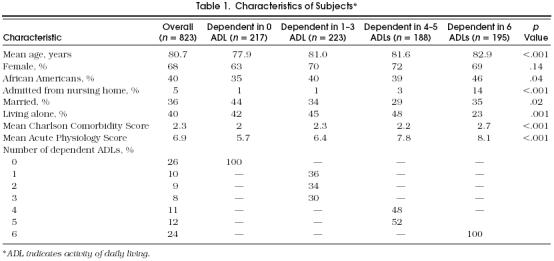
On admission to the hospital, 217 patients were dependent in none of the 6 ADLs, 223 in 1 to 3 ADLs, 188 in 4 or 5 ADLs, and 195 in all 6 ADLs. The mean age of the patients was 80.7 years, and 68% were women (Table 1). Patients with more ADL dependencies were more likely to be older, African American, and admitted from nursing homes. They also had higher Charlson comorbidity and APS scores (Table 1).
Table 1.
Characteristics of Subjects*
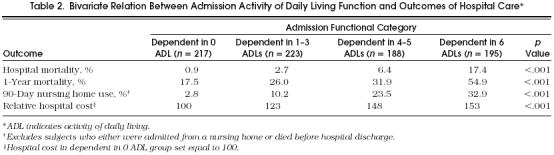
Mortality and resource use increased as function worsened (Table 2). Hospital mortality increased from 0.9% in the patients dependent in no ADL on admission, to 17.4% in patients dependent in all 6 ADLs. One-year mortality increased from 17.5% to 54.9%. The rate of nursing home use increased from 2.8% to 32.9%. Hospital costs were 53% higher for patients dependent in all 6 ADLs than patients dependent in no ADL.
Bivariate Relation Between Admission Activity of Daily Living Function and Outcomes of Hospital Care*
Within each quartile of APS and Charlson score, worsening ADL function was associated with worse outcomes. For example, 1-year mortality in patients dependent in 0, 1–3, 4–5, and 6 ADLs was 7%, 14%, 18%, and 32%, respectively, in patients with Charlson scores of 0 ( p = .008); 11%, 21%, 25%, and 43% respectively, in patients with Charlson scores of 1 (p < .001); 13%, 19%, 30%, and 51%, respectively, in patients with Charlson scores of 2 (p < .001); and 36%, 39%, 48%, and 68%, respectively, in patients with Charlson scores of 3 or more (p < .001).
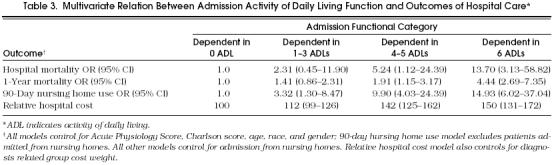
In multivariable models controlling for APS, Charlson comorbidity scores, age, race, and gender, admission ADL function was strongly and independently associated with hospital and 1-year mortality and postdischarge nursing home use (Table 3). ADL function was also an independent predictor of hospital cost in a model that controlled for DRG cost weight as well as the above covariates. Other covariates that were significantly associated (p < .05) with higher hospital mortality were higher APS score (odds ratio [OR] 1.12 per point; 95% confidence interval [CI] 1.05–1.19), higher Charlson score (OR 1.30 per point; 1.15–1.45), and female gender (OR 2.11; 1.01–4.44). Covariates significantly associated with 1-year mortality were higher APS score (OR 1.05 per point, 1.01– 1.09) and higher Charlson score (OR 1.34 per point; 1.25–1.45). The only other covariate significantly associated with nursing home use was age (OR 1.05 per year; 1.02–1.09). Covariates significantly associated with hospital cost (in addition to cost weight) were admission from a nursing home (adjusted cost 24.1% lower, 4.9–39.4%), APS score (adjusted cost 1.2% higher per point, 0.5–2.7%), and white race (adjusted cost 13.6% higher, 3.7–24.5%).
Multivariate Relation Between Admission Activity of Daily Living Function and Outcomes of Hospital Care*
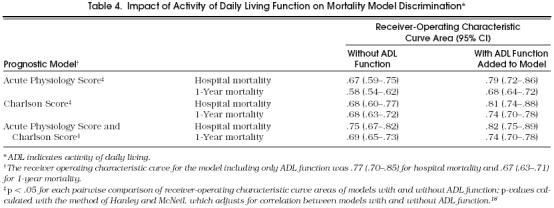
ADL function discriminated hospital and 1-year mortality at least as well as APS and Charlson scores (Table 4). The ROC areas for APS, Charlson scores, and ADL function were .67, .68, and .77, respectively, for hospital mortality, and .58, .68, and .67 for 1-year mortality. ADL function significantly improved the ability of APS, Charlson scores, and APS and Charlson score combined to discriminate among patients according to hospital and 1-year mortality.
Impact of Activity of Daily Living Function on Mortality Model Discrimination*
DISCUSSION
Our results demonstrate that the functional status of older patients on hospital admission, as measured by their ability to perform six ADLs, is an important predictor of outcomes of health care and supplements predictors based on internal physiologic measurements and diagnoses. Three major results support this conclusion. First, ADL function stratified patients into markedly different categories of risk for mortality and higher resource use. Second, ADL function remained highly predictive of mortality and resource use after adjustment for predictive indices based on standard internal physiologic measures or comorbidities and diagnoses. Third, ADL function significantly improved the discrimination of models that considered only these other indices. These findings suggest that incorporating measures of physical function into prognostic and case mix adjustment systems may significantly improve the ability of these systems to predict important health outcomes.
As described by Stein and colleagues,19 measures of integrative functioning, such as ADL function, differ conceptually from more typical measures of prognosis and case mix in that they consider neither the illness itself, nor its impact on internal physiologic parameters, but rather the illness’ impact on the patient’s ability to conduct the normal activities of daily life. They reflect the impact of illness on the whole person and the ability of the individual to function in the external environment, rather than on the internal milieu of an organ or body system. Measures of integrative functioning can add important information about illness severity, beyond that provided by internal physiologic measures and diagnoses, because patients with the same internal physiologic measures and diagnoses can differ widely in their ability to conduct daily life.
The importance of physical function as a predictor of mortality and resource use has important implications for users of prognostic and case-mix adjustment methods. For example, prognostic and case-mix adjustment methods are increasingly being used to compare outcomes across providers and institutions.20 In these cases, the purpose of these methods is to level the playing field by accounting for baseline differences in risk of outcome. Our results suggest that considering physical function may allow for more accurate risk comparisons. Institutions and providers that care for frailer patients may be inappropriately penalized by systems that fail to measure this frailty. For example, our results show that the DRG-based risk adjustment system used by Health Care Financing Administration (HCFA) to reimburse hospitals will penalize hospitals taking care of more frail patients. Prognostic and case mix adjustment is also often used to compare outcomes in clinical trials. Our findings suggest that collecting information on baseline physical function will improve these comparisons.
Relationship to Previous Studies
Others have demonstrated correlations between ADL function and mortality in community-dwelling older patients, though most of these studies did not control for validated measures of illness severity.1–2 Several studies have measured the prognostic significance of function in hospitalized patients with specific illnesses. For example, ADL function discriminated hospital mortality in AIDS patients better than CD4 counts, diagnoses, or laboratory measures.3 Function in specific ADLs has been demonstrated to be strongly correlated with hospital mortality after adjustment for routine laboratory measurements in patients with pneumonia and congestive heart failure,4 and Karnofsky Performance Status score has been shown to predict outcomes in patients with cancer5 or acute myocardial infarction.6
The number of studies on the relation between function and outcomes in general medical patients is limited. In one example, the Nursing Severity Index, a prognostic index that included measures of functional impairment, discriminated hospital mortality as well as Medis-Groups, a prognostic system based on diagnoses and laboratory measures.7 Other studies have demonstrated that physical function in hospitalized elders is correlated with mortality and other outcomes at and after discharge, but none of these studies adjusted for other validated measures of prognosis or case mix.8–10
Our results extend those of previous studies by demonstrating that function is a strong predictor of both mortality and resource use in older hospitalized patients after adjustment for validated predictors of mortality and resource use. We also demonstrate that adding functional information significantly improves the discrimination of two systems that only consider internal physiologic measures and diagnoses.
Methodologic Considerations
Strengths of this study are the use of a diverse population of patients, the consideration of both early and late mortality, and the consideration of both patient and economic outcomes. However, several limitations should be recognized.
First, the relative performance of the three adjustment methodologies we used most likely would have been different in different populations. For example, in our patient population, APS did not consistently significantly improve the discrimination of models that included both Charlson comorbidity scores and ADL function. However, APS was initially designed for ICU patients, who were not included in our sample. We think it is likely that in a sample that had more variability in physiologic derangements, APS would have significantly improved the discrimination of Charlson scores and ADL function. We believe the major message of our results is not the relative performance of each methodology, but rather that considering physical function can improve existing prognostic and case mix adjustment methods. More comprehensive and disease-specific measures of integrative function may have even greater potential as adjustment methodologies.
Second, although our results suggest function should be incorporated into prognostic and case-mix adjustment indices, such an index remains to be developed and tested. Third, our study population was limited to older general medical patients. Physical function may have been a less useful adjustment method in younger patients or surgical patients. Fourth, actually incorporating measures of physical function into prognostic and case-mix methods requires further study of several methodologic issues including reliability, measurement method (for example, observer vs patient, interview vs performance based), and the potential for biased reporting or gaming of the measurements when used to compare outcomes across providers.
Conclusions
Functional status is an important predictor of hospital outcomes in older patients, with respect to both mortality and resource use. ADL function contains important information about illness severity beyond that provided by laboratory data and comorbidities. Severity adjustment methods may be improved if they include measures of physical function, in addition to measures of physiology and comorbidity. The inclusion of functional information may allow for more accurate outcomes comparisons and risk stratification.
JOURNAL OF GENERAL INTERNAL MEDICINE SUBSCRIBERS
Do we have your new address?
Send us your new address three months before it becomes effective, so we will have time to get it into our computer system and ensure that your copies of JGIM continue to arrive uninterrupted. Send your old mailing label, your new address with zip code, the effective date of your new address, and your current telephone number.
Nonmember subscribers notify:
Tina Lynch
Blackwell Science, Inc.
Commerce Place, 350 Main St.
Malden, MA 02148
SGIM members notify:
Elnora Rhodes
Society of General Internal Medicine
700 13th Street, NW, Suite 250
Washington, DC 20005
REFERENCES
- 1.Corti-Maria C, Guralnik JM, Salive ME, Sorkin JD. Serum albumin and physical disability as predictors of mortality in older persons. JAMA. 1994;272:1036–42. [PubMed] [Google Scholar]
- 2.Reuben DB, Rubenstein LV, Hirsch SH, Hays RD. Value of functional status as a predictor of mortality: results of a prospective study. Am J Med. 1992;93:663–9. doi: 10.1016/0002-9343(92)90200-u. [DOI] [PubMed] [Google Scholar]
- 3.Justice AC, Aiken LH, Smith HL, Turner BJ. The role of functional status in predicting inpatient mortality with AIDS: a comparison with current predictors. J Clin Epidemiol. 1996;49:193–201. doi: 10.1016/0895-4356(95)00546-3. [DOI] [PubMed] [Google Scholar]
- 4.Davis RB, Iezzoni LI, Phillips RS, Reiley P, Coffman GA, Safran C. Predicting in-hospital mortality: the importance of functional status information. Med Care. 1995;33:906–21. doi: 10.1097/00005650-199509000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Grabowski C, Unger J, Potish R. Factors predictive of completion of treatment and survival after palliative radiation therapy. Radiology. 1992;184:329–32. doi: 10.1148/radiology.184.2.1377829. [DOI] [PubMed] [Google Scholar]
- 6.Brezinski D, Stone P, Muller J, et al. Prognostic significance of the Karnofsky Performance Status score in patients with acute myocardial infarction: comparison with the left ventricular ejection fraction and the exercise treadmill test performance. Am Heart J. 1991;121:1374–81. doi: 10.1016/0002-8703(91)90141-4. [DOI] [PubMed] [Google Scholar]
- 7.Rosenthal GE, Halloran EJ, Kiley M, Pinkley C, Landefeld CS. Development and validation of the Nursing Severity Index: a new method of measuring severity of illness using nursing diagnoses. Med Care. 1992;30:1127–41. doi: 10.1097/00005650-199212000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Narain P, Rubenstein LZ, Wieland GD, et al. Predictors of immediate and 6-month outcomes in hospitalized elderly patients: the importance of functional status. J Am Geriatr Soc. 1988;36:775–83. doi: 10.1111/j.1532-5415.1988.tb04259.x. [DOI] [PubMed] [Google Scholar]
- 9.Cohen HJ, Saltz CC, Samsa G, McVey L, Davis D, Feussner JR. Predictors of two-year post-hospitalization mortality among elderly veterans in a study evaluating a geriatric consultation team. J Am Geriatr Soc. 1992;40:1231–5. doi: 10.1111/j.1532-5415.1992.tb03648.x. [DOI] [PubMed] [Google Scholar]
- 10.Winograd CH, Gerety MD, Chung M, Goldstein MK, Dominguez F, Vallone R. Screening for frailty: criteria and predictors of outcomes. J Am Geriatr Soc. 1991;39:778–84. doi: 10.1111/j.1532-5415.1991.tb02700.x. [DOI] [PubMed] [Google Scholar]
- 11.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 12.Landefeld CS, Palmer RM, Kresevic DM, Fortinsky RH, Kowal J. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338–44. doi: 10.1056/NEJM199505183322006. [DOI] [PubMed] [Google Scholar]
- 13.Knaus WA, Draper EA, Wagner WP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 15.MacKenzie TA. Baltimore, Md: Report to the Health Care Financing Administration; 1991. Patient Classification Systems: An evaluation of the State of the Art. NTIS document PB92-123405. [Google Scholar]
- 16.Rich-Edwards JW, Corsano KA, Stampfer MJ. Test of the National Death Index and Equifax Nationwide Death Search. Am J Epidemiol. 1994;140:1016–9. doi: 10.1093/oxfordjournals.aje.a117191. [DOI] [PubMed] [Google Scholar]
- 16.Lorenz EW, Jones MK, Lawson KH, LeBlond J. Washington, DC: St. Anthony Hospital Publications; 1989. The Physician’s DRG Working Guidebook. [Google Scholar]
- 18.Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148:839–43. doi: 10.1148/radiology.148.3.6878708. [DOI] [PubMed] [Google Scholar]
- 19.Stein REK, Perrin EC, Pless IB, et al. Severity of illness: concepts and measurements. Lancet. 1987;2:1506–9. doi: 10.1016/s0140-6736(87)92633-x. [DOI] [PubMed] [Google Scholar]
- 20.Rosenthal GE, Harper DL. Cleveland Health Quality Choice: a model for collaborative community-based outcomes assessment. Jt Comm J Qual Improv. 20;8:425–42. doi: 10.1016/s1070-3241(16)30088-8. [DOI] [PubMed] [Google Scholar]


