Abstract
OBJECTIVE
To assess the effectiveness of brief interventions in heavy drinkers by analyzing the outcome data and methodologic quality.
DESIGN
(1) Qualitative analysis of randomized control trials (RCTs) using criteria from Chalmers’ scoring system; (2) calculating and combining odds ratios (ORs) of RCTs using the One-Step (Peto) and the Mantel-Haenszel methods.
STUDY SELECTION AND DATA ANALYSIS
A MEDLINE and PsycLIT search identified RCTs testing brief interventions in heavy alcohol drinkers. Brief interventions were less than 1 hour and incorporated simple motivational counseling techniques much like outpatient smoking cessation programs. By a single-reviewer, nonblinded format, eligible studies were selected for adult subjects, sample sizes greater than 30, a randomized control design, and incorporation of brief alcohol interventions. Methodologic quality was assessed using an established scoring system developed by Chalmers and colleagues. Outcome data were combined by the One-Step (Peto) method; confidence limits and ξ2 test for heterogeneity were calculated.
RESULTS
Twelve RCTs met all inclusion criteria, with an average quality score of 0.49 ± 0.17. This was comparable to published average scores in other areas of research (0.42 ± 0.16). Outcome data from RCTs were pooled, and a combined OR was close to 2 (1.91; 95% confidence interval 1.61–2.27) in favor of brief alcohol interventions over no intervention. This was consistent across gender, intensity of intervention, type of clinical setting, and higher-quality clinical trials.
CONCLUSIONS
Heavy drinkers who received a brief intervention were twice as likely to moderate their drinking 6 to 12 months after an intervention when compared with heavy drinkers who received no intervention. Brief intervention is a low-cost, effective preventive measure for heavy drinkers in outpatient settings.
Keywords: meta-analysis, qualitative analysis, randomized control trial, heavy drinking, brief clinical interventions
A significant number of North Americans drink excessive amounts of alcohol. Although excessive alcohol use is often socially accepted behavior, there is a notable increased risk of workforce dysfunction, motor vehicle accidents, injuries, marital discord, family dysfunction, alcohol-related disease, and death.1 Average daily alcohol consumption above two or three drinks has been shown to result in subjective complaints, physical findings, alcohol-related problems, and alcohol dependence.2,3 These consequences of excessive alcohol use are seen in the primary care and hospital settings with prevalence rates approaching 20% to 40%.4–8
Excessive drinking behavior, often described as problem drinking, heavy drinking, or at-risk drinking, is generally not associated with alcohol dependence such as major withdrawal symptoms, tolerance, complete loss of control, or preoccupation with drinking.9 The definition of excessive or problem drinking is imprecise and often depends on not only quantity and frequency of alcohol consumed but also individual characteristics such as gender, age, weight, and comorbid conditions.10 The Institute of Medicine reports that up to 20% of the U.S. population are problem drinkers as compared with only 5% who are severely dependent alcoholics.11 Survey data comparing problem drinkers with more severely alcohol-dependent individuals suggest that problem drinkers are generally younger, have a shorter problem drinking history, are better educated, have greater employment stability and social resources, and consist of a greater proportion of women.12
In response to a high degree of alcohol-related morbidity and mortality, the medical profession has focused primarily on the medical sequelae of patients with significant alcohol dependence. In addition, traditional intensive alcohol inpatient programs were the mainstay in the treatment of most alcohol disorders. Little attention was given to early intervention programs and treatment of nondependent or mildly dependent drinkers.13 This has led to efforts in earlier identification and intervention, as well as expansion of techniques and goals. Brief interventions as short as 10 to 15 minutes have been introduced as viable treatment options. These types of interventions incorporate simple motivational techniques much like outpatient smoking-cessation programs. In addition, treatment goals consisting of controlled, moderate drinking instead of alcohol abstinence have reportedly become viable options and outcomes in treatment of nondependent heavy or problem drinkers.14,15
This review critiques and summarizes randomized control trials (RCTs) testing brief alcohol interventions. A standardized method is used to grade methodologic strengths and weaknesses of selected trials included in the analysis. Outcome data are pooled using statistical methods.
METHODS
Identification and Selection of Articles
Computer-based bibliographic databases (MEDLINE and PsycLIT) were accessed and searched in years 1966 to 1995. MeSH headings (alcoholism or alcohol drinking) and title words (problem drinking, intervention, clinical trials, treatment, and outcome) were used interchangeably. Numerous combinations were searched including alcoholism and intervention, alcohol drinking and intervention, problem drinking and intervention, alcoholism and clinical trials, and alcohol drinking and clinical trials. Bibliographies of relevant articles and of research experts in the field (Drs. Thomas Babor and William Miller) were reviewed.
After titles and abstracts were reviewed by a single-reviewer format, all articles with the following parameters were retrieved: (1) clear focus on alcohol abuse or dependence or on heavy drinking; (2) focus on intervention and outcome; (3) publication in English; (4) human subjects, aged 19 to 65 years and older; and (5) the study design of a prospective clinical trial. If the abstract and title were unclear as to the study design used, the article was retrieved for clarification.
Retrieved articles were evaluated to determine eligibility for qualitative and quantitative analyses. Inclusion criteria included a study design that is truly a randomized trial, a control group that receives no alcohol-related treatment or intervention, a sample size greater than 30, and a brief intervention that is motivational with a self-help orientation. Articles that did not include original clinical data, such as reviews or editorials, were excluded.
Qualitative Analysis of Articles
The quality of selected RCTs was assessed using a scoring method previously reported by Chalmers and colleagues,16 and previously applied to a number of studies of different chronic diseases.17–20 Among the categories included in the scoring system were selection criteria, rejection log (patients screened and rejected), testing of randomization, blinding of assessors, biological equivalents (γ-glutamyltransferase [GGT] aspartate amino transferase, and mean corpuscular volume blood levels and blood pressure), statistical analyses, handling of withdrawals, and data presentation. Certain categories were excluded owing to the nature of brief alcohol interventions such as blinding of patients to the intervention, controlling placebo appearance and taste, testing compliance, and statistical discussion of side effects.
Scores assigned to each item were judgmental approximations as suggested by Chalmers (see Appendix A). The scoring method has been applied to more than 400 articles with a reported mean score of 0.42 ± 0.16 (SD) out of a possible 1.00.21 Therefore, the qualitative analysis in this article allowed for subgroup quantitative analysis of selected RCTs that achieved an equal or greater score.
Quantitative Analysis of Articles
To estimate the likelihood that heavy drinkers moderated their drinking after a brief alcohol intervention, odds ratios (ORs) of the individual clinical trials were calculated when possible, and then combined using the One-Step (Peto) method.22 Results are expressed as the OR (treatment to control) for achieving alcohol moderation 6 or 12 months after intervention. In addition, a test-based 95% confidence interval (CI) for each OR was computed. Subgroup analyses of gender, number of intervention sessions, type of clinical setting (outpatient vs inpatient), and high-quality clinical trials were conducted. Because of the potential for bias in the Peto method, all ORs and combined ratios were verified using the Mantel-Haenszel technique. In addition, the χ2 test for heterogeneity23 was performed for all summary OR estimates so that any significant statistical heterogeneity between studies may be detected and addressed. Also, an analysis was done to test the differences between different subgroups of data using the following Z statistic:
![]()
RESULTS
Literature Search
A total of 5,896 articles were initially identified with the greater majority consisting of cross-sectional studies and follow-up studies of individual treatment programs. The list was refined to 99 references, and of these trials, 12 were selected for further analysis.24–35 The remaining 87 trials were rejected for the following reasons: 38 were comparison trials of different types of interventions without control groups 36–73; 21 lacked a control group 74–94 15 incorporated other therapies (intensive inpatient therapy, hypnotic therapy, aversion therapy, biofeedback, aerobic exercise)95–109 ; and the remaining 13 for other reasons (e.g., retrospective analysis, lack of randomization).110–122
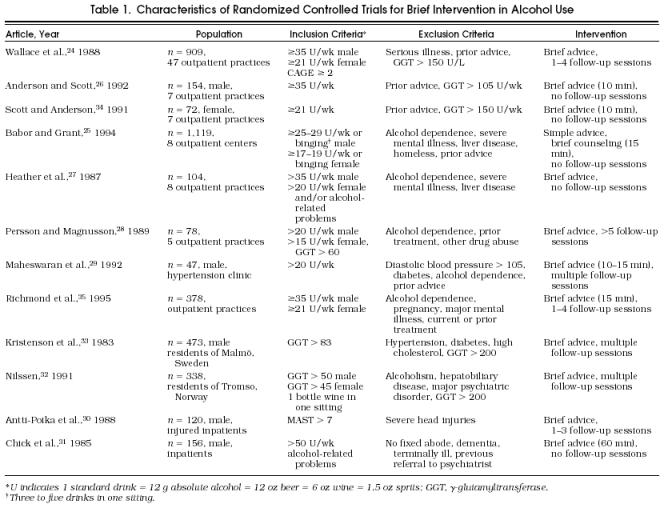
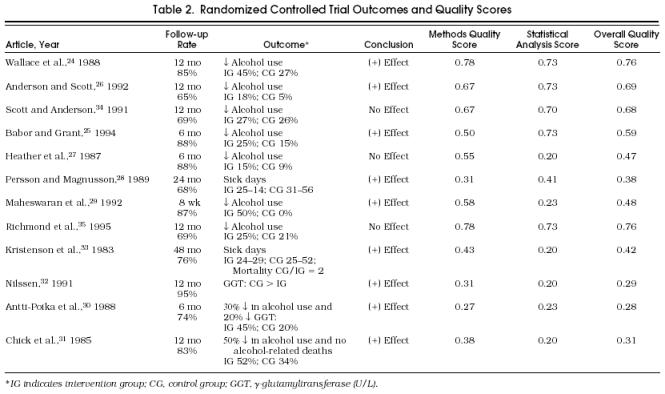
General characteristics of the selected 12 clinical trials, summarized in Tables 1Table 2, reveal diversity in study population, inclusion and exclusion criteria, intervention intensity, follow-up rates, outcome measures, and methodologic quality scores. A total of 3,948 heavy or problem drinkers were randomized to a brief intervention or to no intervention. Overall, sample sizes of individual trials ranged from 47 (single-center study) to 1,119 (multicenter study). Study samples reflected three distinct populations including outpatients,24–29,34,35 inpatients,30,31 and the general population.32,33 Nine studies included patients who were drinking more than 20 to 35 drinks per week. Other inclusion criteria were elevated GGT levels,28,32,33 a positive CAGE (≥2) or MAST questionnaire,24,30 and scales of alcohol-related problems.27,31 Though all trials appeared to target the less severely alcohol-affected population, 5 specifically stated exclusion of patients with severe alcohol dependence; 5 stated exclusion of patients with a previous history of advice to change drinking patterns; and 4 stated exclusion of patients with serious medical and psychiatric disorders.
Characteristics of Randomized Controlled Trials for Brief Intervention in Alcohol Use
Randomized Controlled Trial Outcomes and Quality Scores
The intervention common to all trials was described as short, motivational counseling sessions that included feedback and education in the harm of heavy drinking and advice to moderate drinking to low-risk, problem-free levels. Although the intervention was described as brief, some authors specified 10 to 15 minutes and others as much as 60 minutes. In addition, follow-up sessions after the initial intervention varied from zero to three sessions suggesting differences in intensity of interventions.
Quality Scores Using the Chalmers’ Scoring System
An overall quality score reflecting both methodologic design and statistical analysis of the 12 trials was 0.49 ± 0.17 (range 0–1.0; 1 SD). Quality scores using the same scoring system in other therapeutic clinical trials are comparable.
When specific categories and RCT success in methodologic design and statistical analysis were examined, the majority of RCTs met essential requirements in the following categories: selection criteria (100%), intervention description (100%), and biological equivalents (83%). Half the selected RCTs adequately reported pretreatment variables and rejection logs. Selected RCTs fared less well in categories of reporting withdrawals (25%), randomization methods (42%), blinded assessments (42%), testing adequacy of blinding (17%) and previous estimates of sample size (42%). The majority of trials adequately reported test statistics and probability levels; however, few reported confidence limits and few received credit for proper handling of withdrawals, type II error calculations, and proper retrospective analysis. Complete analysis of withdrawals was reported by four trials in which data were analyzed multiple ways (intention to treat and discarded withdrawals). The remaining studies simply discarded the withdrawals and therefore discounted an end result. Of the two negative trials, one noted type II error and the presence of small sample sizes. However, an estimation of a posterior β value was not done. Half the clinical trials addressed retrospective data analysis that included inadequacies in randomization, dropouts, or presence of selection biases. These areas were discussed to some degree; however, the total determination of these problems and their effect on outcomes was generally incomplete.
Despite the above-mentioned inadequacies, the majority of trials achieved quality scores equivalent to published rates. Selected RCTs that achieved an overall quality score greater than or equal to previously published scores (0.42) were further summarized in the subgroup analysis as higher-quality clinical trials.
Odds Ratios and Pooling of Odds Ratios
Eight RCTs (70% of the total randomized study population) reported outcome data that allowed calculation of individual ORs whose range was 1.09 to 3.20 (Table 3 and Fig. 1). A pooled OR of the eight RCTs showed that heavy drinkers who received brief motivational interventions were close to two times more likely to decrease and moderate their drinking compared with those who received no intervention (OR 1.95; 95% CI 1.66 –2.30). Despite inclusion of low-quality RCTs in the pooled OR no significant heterogeneity was detected (Table 4. A subanalysis of the six high-quality RCTs (scores 0.42 or greater) revealed little difference in the summary OR (1.91; 95% CI 1.61–2.27) and still no significant heterogeneity. Specific subcategories of heavy drinkers were also analyzed and included intensity of intervention, gender, and type of patient population (Fig. 2). Calculated ORs suggest a greater likelihood of alcohol moderation with greater intensity of intervention (OR 2.12 for> 1 session compared with OR 1.83 for 1 session), female gender (OR 2.42 for women compared with OR 1.90 for men), and the intervention in the inpatient setting (OR 2.41 for inpatient compared with OR 1.91 for outpatient), although none of these comparisons was significant by Z statistic (p values .37, .24, and .43, respectively). All OR calculations were repeated using the Mantel-Haenszel method, and results were nearly equal in all analyses.
Table 3.
Randomized Controlled Trials: Percentage Moderation and Odds Ratios in Treatment and Control Groups
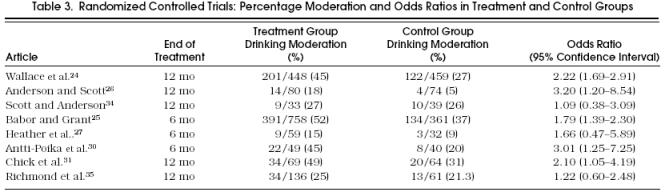
Figure 1.
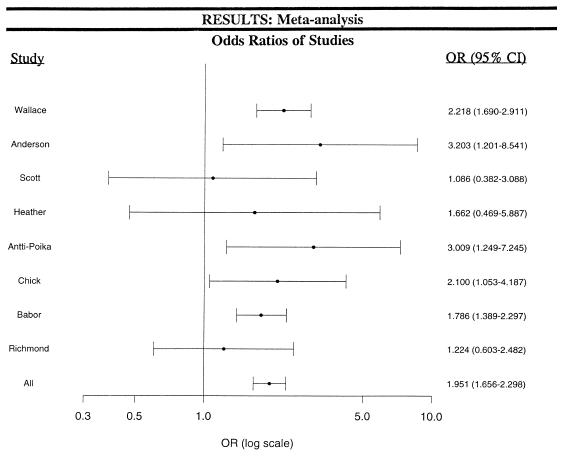
Eight randomized control trials whose outcome data allowed calculation of individual odds ratios.
Table 4.
Benefit of Brief Intervention Versus No Intervention by Combined Ratios According to Gender, Intervention Intensity, and Clinical Setting

Figure 2.

Analysis of specific subcategories of heavy drinkers.
DISCUSSION
We have shown in this meta-analysis of RCTs that heavy drinkers receiving brief interventions were two times more likely to moderate their drinking when compared with drinkers receiving no intervention. To date, the literature has not contained a published meta-analysis of clinical trials in alcohol outcomes research using the described quality scoring system. The pooled ORs calculated from trials were consistently close to 2 and included 70% of all reported randomized heavy drinkers in the 12 selected RCTs. Despite great variation in trial characteristics, there was no statistical evidence of heterogeneity and little difference in ORs when high-quality trials were compared with low-quality trials.
Qualitative analysis of the selected RCTs revealed varying levels of methodologic and analytic rigor. Though mean scores of methodology were comparable to those for previously published clinical reviews and analyses, variability and potentially serious flaws were present in a number of randomized trials. This was especially evident in the randomization process, wherein only one trial received full credit.25 Details of randomization such as measures in concealment of treatment allocation, measures to generate an allocation schedule, and measures to implement blinding were not adequately reported in the remaining trials. Thus, although randomization was key to the strength of these RCTs, authors often provided inadequate details in their assignment of participants to intervention and control groups. Therefore the risk of larger estimates in treatment effects for the majority of trials is relatively high.123,124 Previous reports suggest that ORs of effect can be exaggerated by as much as 17% to 40% depending on the particular methodologic flaw.125 More than half of the selected trials tested the success of their randomization process by comparing baseline variables in control and treatment groups and found insignificant differences. This represents some reassurance of successful randomization, but does not entirely exclude the possibility of exaggerated ORs and treatment effects.
There were potential limitations with regard to the RCT selection process. Though MEDLINE and PsycLIT databases were extensively reviewed back to 1966, unpublished trials would have been missed. In particular, unpublished negative trials could have been excluded for review thus biasing the review to positive outcomes. However, unpublished results may also be less reliable and therefore detrimental to the final analysis. Furthermore, the process of review was limited by a single-reviewer format with no blinding to author or institution.
Generalizability of our results must be limited to less severely affected drinkers who exhibit little or no alcohol dependence. More severely affected individuals with evidence of loss of control, tolerance, or withdrawal symptoms would in fact be at risk for withdrawal, or failure, if brief intervention were the sole treatment. Therefore, brief alcohol interventions must be applied carefully to the drinking population who may exhibit early medical or psychosocial complications but do not have alcohol dependence. To aid the primary care physician in screening and intervening in heavy or problem drinkers, the algorithm in Figure 3 is recommended. Generalizability of results to patients in the United States is perhaps limited by the greater majority of trials conducted in populations outside the United States. Presently, up to five ongoing alcohol brief intervention trials are being conducted in the United States, and results are pending their completion.
Figure 3.

Algorithm for screening problem drinkers. (Adapted from The Physician’s Guide to Helping Patients with Alcohol Problems. Bethesda, Md: National Institute in Alcohol Abuse and Alcoholism; 1995. NIH publication 95-3769.)
Finally, although our results show a strong positive impact of brief alcohol interventions, we are still limited in our knowledge of alcohol treatment outcomes in other significant areas: cost-effectiveness, hard endpoints such as mortality and morbidity, long-term effects of treatment, and health care utilization. Though none of the clinical trials directly addressed cost, brief alcohol intervention compared with all other available alcohol intervention programs has been shown to be the least expensive.126,127 Holder and coworkers estimate that the expense of brief alcohol intervention is somewhat less than $100.126 In regard to mortality and morbidity rates, drinking moderation and problem-free drinking tend to lead to a decrease in alcohol-related disease and improved health and well-being. However, only one RCT reported results suggestive of lower mortality and morbidity rates in the group receiving brief interventions.33 Other outcomes such as work performance, family relationships, and overall quality of life were not consistently addressed and shown to improve with brief interventions. In addition, though collateral data are key to validating self-reported alcohol consumption, biomedical markers (GGT, MCV, AST) do not consistently reflect heavy or severity of drinking. Therefore, other collateral or supporting outcome measures such as the CAGE questionnaire and confirmatory reports by close contacts need to be consistently included.
It will also be important to test whether health care utilization improves with brief interventions. There is some suggestion in Persson’s trial28 that a subgroup of intervention clients did decrease health care costs; however, the sample size was small in this study. There is a clear need in clinical trials addressing heavy drinking or problem drinking for standardized outcome measures that include function and quality of life, over 5 to 10 years after treatment maneuvers. The measures may include various domains of health status, such as global, physical, social, and psychological health.
In summary, low-cost, brief interventions in heavy drinking within the primary care setting work with twice the likelihood of alcohol moderation. Future studies should focus on training clinicians to alter their interventional behavior, screen carefully for alcoholism, and incorporate brief interventions in patients with heavy or problem drinking but without alcoholism and severe dependence.
Acknowledgments
The authors thank Mark Linzer, MD, MPH, and Michael F. Fleming, MD, MPH, for their invaluable time reviewing the manuscript during its various stages of preparation.
References
- 1.NIAAA National Institute on Alcohol Abuse and Alcoholism. Seventh Special Report to the US Congress. Rockville: Md: Dept of Health and Human Services; 1990. Alcohol and Health. [Google Scholar]
- 2.Miller WR, Heather N, Hall W. Calculating standard drink units: international comparisons. Br J Addict. 1991;86:43–7. doi: 10.1111/j.1360-0443.1991.tb02627.x. [DOI] [PubMed] [Google Scholar]
- 3.Saunders JB, Aasland OG. Geneva, Switzerland: World Health Organization, Division of Mental Health; 1987. WHO Collaborative Project on Identification and Treatment of Persons with Harmful Alcohol Consumption: Report on Phase I—Development of a Screening Instrument. WHO/MNH/DAT/86.3. [Google Scholar]
- 4.Cleary PD, Miller M, Bush BT, Warburg MM, Delbanco TL, Aronson MD. Prevalence and recognition of alcohol abuse in a primary care population. Am J Med. 1988;85:466–71. doi: 10.1016/s0002-9343(88)80079-2. [DOI] [PubMed] [Google Scholar]
- 5.Graham AW. Screening for alcoholism by life-style risk assessment in a community hospital. Arch Intern Med. 1991;151:958–64. [PubMed] [Google Scholar]
- 6.Moore RD, Bone LR, Geller G, Marmon JA, Stokes EJ, Levine DM. Prevalence, detection, and treatment of alcoholism in hospitalized patients. JAMA. 1989;261:403–7. [PubMed] [Google Scholar]
- 7.Sherin KM, Piotrowski ZH, Panek SM, Doot MC. Screening for alcoholism in a community hospital. J Fam Pract. 1982;15:1091–5. [PubMed] [Google Scholar]
- 8.Coulehan JL, Zettler-Segal M, Block M, McClelland M, Schulberg HC. Recognition of alcoholism and substance abuse in primary care patients. Arch Intern Med. 1987;147:349–52. [PubMed] [Google Scholar]
- 9.American Psychiatric Association . 4th ed. Washington, DC: American Psychiatric Association; 1994. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 10.Kendell RE. Drinking sensibly. Br J Addict. 1987;82:1279–88. doi: 10.1111/j.1360-0443.1987.tb00430.x. [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine . Washington, DC: National Academy Press; 1990. Broadening the Base of Treatment for Alcohol Problems. [PubMed] [Google Scholar]
- 12.Sobell MB, Sobell LC. New York, NY: The Guilford Press; 1993. Problem Drinkers Guided Self-Change Treatment. [Google Scholar]
- 13.Skinner HA. Spectrum of drinkers and intervention opportunities. Can Med Assoc J. 1990;143:1054–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Miller WR. Controlled drinking: a history and a critical review. J Stud Alcohol. 1983;44:68–83. doi: 10.15288/jsa.1983.44.68. [DOI] [PubMed] [Google Scholar]
- 15.Sanchez-Craig M. Random assignment to abstinence or controlled drinking in a cognitive-behavioral program: short-term effects on drinking behavior. Addict Behav. 1980;25:35–9. doi: 10.1016/0306-4603(80)90019-2. [DOI] [PubMed] [Google Scholar]
- 16.Chalmers TC, Smith H, Jr, Blackburn B, et al. A method for assessing the quality of a randomized control trial. Control Clin Trials. 1981;2:31–49. doi: 10.1016/0197-2456(81)90056-8. [DOI] [PubMed] [Google Scholar]
- 17.Hine LK, Laird NM, Hewitt P, Chalmers TC. Meta-analysis of empirical long-term antiarrhythmic therapy after myocardial infarction. JAMA. 1989;262:3037–40. [PubMed] [Google Scholar]
- 18.Moskowitz SB, Chalmers TC, Sacks HS, Fagerstrom RM, Smith H., Jr Deficiencies of clinical trials of alcohol withdrawal. Alcohol Clin Exp Res. 1983;7:42–6. doi: 10.1111/j.1530-0277.1983.tb05409.x. [DOI] [PubMed] [Google Scholar]
- 19.Liberati A, Himel HN, Chalmers TC. A quality assessment of randomized control trials of primary treatment of breast cancer. J Clin Oncol. 1986;4:942–51. doi: 10.1200/JCO.1986.4.6.942. [DOI] [PubMed] [Google Scholar]
- 20.Longnecker MP, Berlin JA, Orza MJ, Chalmers TC. A meta-analysis of alcohol consumption in relation to risk of breast cancer. JAMA. 1988;260:652–6. [PubMed] [Google Scholar]
- 21.Reitman D, Sacks HS, Chalmers TC. Technical quality assessment of randomized control trials (RCTs) Control Clin Trials. 1987;8:282. Abstract. [Google Scholar]
- 22.Berlin JA, Laird NM, Sacks HS, Chalmers TC. A comparison of statistical methods for combining event rates from clinical trials. Stat Med. 1989;8:145–51. doi: 10.1002/sim.4780080202. [DOI] [PubMed] [Google Scholar]
- 23.Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10:101–29. [Google Scholar]
- 24.Wallace P, Cutler S, Haines A. Randomised controlled trial of general practitioner intervention in patients with excessive alcohol consumption. BMJ. 1988;297:663–8. doi: 10.1136/bmj.297.6649.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Babor TF, Grant M. Report on Phase II: A Randomized Clinical Trial of Brief Interventions in Primary Health Care. eds. Geneva, Switzerland: World Health Organization; 1992. Project on Identification and Management of Alcohol-Related Problems. [Google Scholar]
- 26.Anderson P, Scott E. The effect of general practitioner’s advice to heavy drinking men. Br J Addict. 1992;87:891–900. doi: 10.1111/j.1360-0443.1992.tb01984.x. [DOI] [PubMed] [Google Scholar]
- 27.Heather N, Campion PD, Neville RG, Maccabe D. Evaluation of a controlled drinking minimal intervention for problem drinkers in general practice (the DRAMS scheme) J R Coll Gen Pract. 1987;37:358–63. [PMC free article] [PubMed] [Google Scholar]
- 28.Persson J, Magnusson P. Early intervention in patients with excessive consumption of alcohol: a controlled study. Alcohol. 1989;6:403–8. doi: 10.1016/0741-8329(89)90011-6. [DOI] [PubMed] [Google Scholar]
- 29.Maheswaran R, Beevers M, Beever DG. Effectiveness of advice to reduce alcohol consumption in hypertensive patients. Hypertension. 1992;19:79–84. doi: 10.1161/01.hyp.19.1.79. [DOI] [PubMed] [Google Scholar]
- 30.Antti-Poika I, Karaharju E, Roine R, Salaspuro M. Intervention of heavy drinking—a prospective and controlled study of 438 consecutive injured male patients. Alcohol Alcohol. 1988;23:115–21. [PubMed] [Google Scholar]
- 31.Chick J, Lloyd G, Crombie E. Counselling problem drinkers in medical wards: a controlled 6–31 study. BMJ. 1985;290:965–7. doi: 10.1136/bmj.290.6473.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nilssen O. The Tromso study: identification of and a controlled intervention on a population of early-stage risk drinkers. Prev Med. 1991;20:518–28. doi: 10.1016/0091-7435(91)90049-a. [DOI] [PubMed] [Google Scholar]
- 33.Kristenson H, Ohlin H, Hultén-Nosslin M-B, Trell E, Hood B. Identification and intervention of heavy drinking in middle-aged men: results and follow-up of 24–60 months of long-term study with randomized controls. Alcohol Clin Exp Res. 1983;7:203–9. doi: 10.1111/j.1530-0277.1983.tb05441.x. [DOI] [PubMed] [Google Scholar]
- 34.Scott E, Anderson P. Randomized controlled trial of general practitioner intervention in women with excessive alcohol consumption. Drug Alcohol Rev. 1991;10:313–21. doi: 10.1080/09595239100185371. [DOI] [PubMed] [Google Scholar]
- 35.Richmond R, Heather N, Wodak A, Kehoe L, Webster I. Controlled evaluation of a general practice–based brief intervention for excessive drinking. Addiction. 1995;90:119–32. doi: 10.1046/j.1360-0443.1995.90111915.x. [DOI] [PubMed] [Google Scholar]
- 36.Sanchez-Craig M, Spivak K, Davila R. Superior outcome of females over males after brief treatment for the reduction of heavy drinking: replication and report of therapist effects. Br J Addict. 1991;86:867–76. doi: 10.1111/j.1360-0443.1991.tb01842.x. [DOI] [PubMed] [Google Scholar]
- 37.Caddy GR, Addington HJ, Jr, Perkins D. Individualized behavior therapy for alcoholics: a third year independent double-blind follow-up. Behav Res Ther. 1978;16:345–62. doi: 10.1016/0005-7967(78)90004-9. [DOI] [PubMed] [Google Scholar]
- 38.Miller WR, Gribskov CJ, Mortell RL. Effectiveness of a self-control manual for problem drinkers with and without therapist contact. Int J Addict. 1981;16:1247–54. doi: 10.3109/10826088109039178. [DOI] [PubMed] [Google Scholar]
- 39.Galanter M, Castaneda R, Salamon I. Institutional self-help therapy for alcoholism: clinical outcome. Alcohol Clin Exp Res. 1987;11:424–8. doi: 10.1111/j.1530-0277.1987.tb01916.x. [DOI] [PubMed] [Google Scholar]
- 40.Walsh DC. A randomized trial of treatment options for alcohol-abusing workers. N Engl J Med. 1991;325:775–82. doi: 10.1056/NEJM199109123251105. [DOI] [PubMed] [Google Scholar]
- 41.Romelsjo A, Andersson L, Barrner H, et al. A randomized study of secondary prevention of early stage problem drinkers in primary health care. Br J Addict. 1989;84:1319–27. doi: 10.1111/j.1360-0443.1989.tb00733.x. [DOI] [PubMed] [Google Scholar]
- 42.Chick J, Ritson B, Connaughton J, Stewart A, Chick J. Advice versus extended treatment for alcoholism: a controlled study. Br J Addict. 1988;83:159–70. doi: 10.1111/j.1360-0443.1988.tb03977.x. [DOI] [PubMed] [Google Scholar]
- 43.Smith JW, Frawley PJ, Polissar L. Six- and twelve-month abstinence rates in inpatient alcoholics treated with aversion therapy compared with matched inpatients from a treatment registry. Alcohol Clin Exp Res. 1991;15:862–70. doi: 10.1111/j.1530-0277.1991.tb00614.x. [DOI] [PubMed] [Google Scholar]
- 44.Keso L, Salaspuro M. Inpatient treatment of employed alcoholics: a randomized clinical trial on hazeldon-type and traditional treatment. Alcohol Clin Exp Res. 1990;14:584–9. doi: 10.1111/j.1530-0277.1990.tb01206.x. [DOI] [PubMed] [Google Scholar]
- 45.Miller WR, Baca LM. Two-year follow-up of bibliotherapy and therapist-directed controlled drinking training for problem drinkers. Behav Ther. 1983;14:441–8. [Google Scholar]
- 46.Drummond DC. A controlled trial of cue exposure treatment in alcohol dependence. J Consult Clin Psychol. 1994;62:809–17. doi: 10.1037//0022-006x.62.4.809. [DOI] [PubMed] [Google Scholar]
- 47.Goldberg HI, Mullen M, Ries RK. Alcohol counseling in a general medicine clinic: a randomized controlled trial of strategies to improve referral and show rates. Med Care. 1991;29:Suppl. [PubMed] [Google Scholar]
- 48.Chapman PL, Huygens I. An evaluation of three treatment programmes for alcoholism: an experimental study with 6- and 8-month follow-ups. Br J Addict. 1988;83:61–81. doi: 10.1111/j.1360-0443.1988.tb00454.x. [DOI] [PubMed] [Google Scholar]
- 49.Chick J, Ritson B, Connaughton J, Stewart A, Chick J. Advice versus extended treatment for alcoholism: a controlled study. Br J Addict. 1988;83:159–70. doi: 10.1111/j.1360-0443.1988.tb03977.x. [DOI] [PubMed] [Google Scholar]
- 50.Zweben A, Pearlman S, Li S. A comparison of brief advice and conjoint therapy in the treatment of alcohol abuse: the results of the Marital Systems Study. Br J Addict. 1988;83:899–916. doi: 10.1111/j.1360-0443.1988.tb01583.x. [DOI] [PubMed] [Google Scholar]
- 51.Skutle A, Berg G. Training in controlled drinking for early-stage problem drinkers. Br J Addict. 1987;82:493–501. doi: 10.1111/j.1360-0443.1987.tb01506.x. [DOI] [PubMed] [Google Scholar]
- 52.Robertson I, Heather N, Dzialdowski A, Crawford J, Winton M. A comparison of minimal vs intensive controlled drinking treatment interventions for problem drinkers. Br J Clin Psychol. 1986;25(5):185–94. doi: 10.1111/j.2044-8260.1986.tb00694.x. [DOI] [PubMed] [Google Scholar]
- 53.Sanchez-Craig M. Brief didactic treatment for alcohol and drug-related problems: an approach based on client choice. Br J Addict. 1990;85:169–77. doi: 10.1111/j.1360-0443.1990.tb03068.x. [DOI] [PubMed] [Google Scholar]
- 54.Kuchipudi V, Hobein K, Flickinger A, Iber FL. Failure of 2-hour motivational intervention to alter recurrent drinking behavior in alcoholics with gastrointestinal disease. J Stud Alcohol. 1990;51:356–60. doi: 10.15288/jsa.1990.51.356. [DOI] [PubMed] [Google Scholar]
- 55.Bowers TG, Al-Redha MR. A comparison of outcome with group/marital and standard/individual therapies with alcoholics. J Stud Alcohol. 1990;51:301–9. doi: 10.15288/jsa.1990.51.301. [DOI] [PubMed] [Google Scholar]
- 56.Edwards G, Guthrie S. A controlled trial of inpatient and outpatient treatment of alcohol dependency. Lancet. 1967;1:555–9. doi: 10.1016/s0140-6736(67)92129-0. [DOI] [PubMed] [Google Scholar]
- 57.Daniels V, Somers M, Orford J, Kirby B. How can risk drinking amongst medical patients be modified? The effects of computer screening and advice and self-help manual. Behav Psychother. 1992;20:47–60. [Google Scholar]
- 58.Harris KB, Miller WR. Behavioral self-control training for problem drinkers: components of efficacy. Psych Addict Behav. 1990;4:82–90. [Google Scholar]
- 59.Heather N, Kissoon-Singh J, Fenton GW. Assisted natural recovery from alcohol problems: effects of a self-help manual with and without supplementary telephone contact. Br J Addict. 1990;85:1177–85. doi: 10.1111/j.1360-0443.1990.tb03443.x. [DOI] [PubMed] [Google Scholar]
- 60.Miller WR, Taylor CA. Relative effectiveness of bibliotherapy, individual and group self-control training in the treatment of problem drinkers. Addict Behav. 1980;5:13–24. doi: 10.1016/0306-4603(80)90017-9. [DOI] [PubMed] [Google Scholar]
- 61.Miller WR, Taylor CA, West JC. Focused versus broad spectrum behavior therapy for problem drinkers. J Consult Clin Psychol. 1980;48:590–601. doi: 10.1037//0022-006x.48.5.590. [DOI] [PubMed] [Google Scholar]
- 62.Miller WR. Behavioral treatment of problem drinkers: a comparative outcome study of three controlled drinking therapies. J Consult Clin Psychol. 1978;46:74–86. doi: 10.1037//0022-006x.46.1.74. [DOI] [PubMed] [Google Scholar]
- 63.Petersson B, Kristenson H, Trell E, Hood B. Screening and intervention for alcohol-related disease in middle-aged men: the Malmö Preventive Programme. Ciba Foundation Symposium. 1985;110:143–63. doi: 10.1002/9780470720912.ch10. [DOI] [PubMed] [Google Scholar]
- 64.Sannibale C. A prospective study of treatment outcome with a group of male problem drinkers. J Stud Alcohol. 1989;50:236–44. doi: 10.15288/jsa.1989.50.236. [DOI] [PubMed] [Google Scholar]
- 65.Rahav M, Rivera JJ, Nuttbrock L, et al. Characteristics and treatment of homeless, mentally ill, chemical-abusing men. J Psychoactive Drugs. 1995;27:93–103. doi: 10.1080/02791072.1995.10471677. [DOI] [PubMed] [Google Scholar]
- 66.Longabaugh R, Wirtz PW, Beattie MC, Noel N, Stout R. Matching treatment focus to patient social investment and support: 18-month follow-up results. J Consult Clin Psychol. 1995;63:296–307. doi: 10.1037//0022-006x.63.2.296. [DOI] [PubMed] [Google Scholar]
- 67.Heather N, Robertson I, MacPherson B. Effectiveness of a controlled drinking self-help manual: one-year follow-up results. Br J Clin Psychol. 1987;26(5):279–87. doi: 10.1111/j.2044-8260.1987.tb01361.x. [DOI] [PubMed] [Google Scholar]
- 68.Nickel WR. A five-year follow-up of treatment for DWI recidivists in the Federal Republic of Germany. Alcohol Drugs Driving. 1990;6:119–32. [Google Scholar]
- 69.Foy DW, Nunn BL, Rychtarik RG. Broad-spectrum behavioral treatment for chronic alcoholics: effects of training controlled drinking skills. J Consul Clin Psychol. 1984;52:218–30. doi: 10.1037//0022-006x.52.2.218. [DOI] [PubMed] [Google Scholar]
- 70.Dahlgren L, Willander A. A controlled 2-year follow-up study from a specialized female unit (EWA) versus mixed male/female treatment facility. Alcohol Clin Exp Res. 1989;13:499–504. doi: 10.1111/j.1530-0277.1989.tb00366.x. [DOI] [PubMed] [Google Scholar]
- 71.Strickler DP, Bradlyn AS, Maxwell WA. Teaching moderate drinking behaviors to young adult heavy drinkers. The effects of three training procedures. Addict Behav. 1981;6:355–64. [Google Scholar]
- 72.Oei TP, Jackson P. Long-term effects of group and individual social skills training with alcoholics. Addict Behav. 1980;5:129–36. doi: 10.1016/0306-4603(80)90030-1. [DOI] [PubMed] [Google Scholar]
- 73.Baer JS, Marlatt A, Kivlahan DR, Fromme K, Larimer ME, Williams E. An experimental test of three methods of alcohol risk reduction with young adults. J Consult Clin Psychol. 1992;60:974–9. doi: 10.1037//0022-006x.60.6.974. [DOI] [PubMed] [Google Scholar]
- 74.Ben-Arie O, Swartz L, George GC. The compulsory treatment of alcoholic drunken drivers referred by the courts: a 7 to 9 years outcome study. Int J Law Psychiatry. 1986;8:229–35. doi: 10.1016/0160-2527(86)90037-3. [DOI] [PubMed] [Google Scholar]
- 75.Rychtarik RG, Foy DW, Scott T, Lokey L. Five–six-year follow-up of broad spectrum behavioral treatment for alcoholism: effects of training controlled drinking skills. J Consult Clin Psychol. 1987;55:106–8. doi: 10.1037//0022-006x.55.1.106. [DOI] [PubMed] [Google Scholar]
- 76.Booth PG, Dale B, Slade PD, Dewey ME. A follow-up study of problem drinkers offered a goal choice option. J Stud Alcohol. 1992;53:594–600. doi: 10.15288/jsa.1992.53.594. [DOI] [PubMed] [Google Scholar]
- 77.Corrigan EM, Butler S, Camasso MJ. Outcome of treatment for Irish alcoholic women. Ir J Psych Med. 1995;12:48–52. [Google Scholar]
- 78.Savage SA, Hollin CR, Hayward AJ. Self-help manuels for problem drinking: the relative effects of their educational and therapeutic components. Br J Clin Psychol. 1990;29:373–82. doi: 10.1111/j.2044-8260.1990.tb00900.x. [DOI] [PubMed] [Google Scholar]
- 79.Miller WR, Hedrick KE, Taylor CA. Addictive behaviors and life problems before and after behavioral treatment of problem drinkers. Addict Behav. 1983;8:403–12. doi: 10.1016/0306-4603(83)90041-2. [DOI] [PubMed] [Google Scholar]
- 80.Miller WR, Leckman AL, Delaney HD, Tinkcom M. Long-term follow-up of behavioral self-control training. J Stud Alcohol. 1992;53:249–61. doi: 10.15288/jsa.1992.53.249. [DOI] [PubMed] [Google Scholar]
- 81.Wright C, Grodin DM, Harig PT. Occupational outcome after military treatment for alcoholism. J Occup Med. 1990;32:24–32. doi: 10.1097/00043764-199001000-00009. [DOI] [PubMed] [Google Scholar]
- 82.Liskow B, Powell BJ, Nickel EJ, Penick E. Diagnostic subgroups of antisocial alcoholics: outcome at 1 year. Compr Psychiatry. 1990;3:549–56. doi: 10.1016/0010-440x(90)90069-5. [DOI] [PubMed] [Google Scholar]
- 83.Finney JW. The long-term course of treated alcoholism, i: mortality, relapse and remission rates and comparisons with community controls. J Stud Alcohol. 1991;52:44–54. doi: 10.15288/jsa.1991.52.44. [DOI] [PubMed] [Google Scholar]
- 84.Miller WR, Benefield RG, Tonigan JS. Enhancing motivation for change in problem drinking: a controlled comparison of two therapist styles. J Consult Clin Psychol. 1993;61:455–61. doi: 10.1037//0022-006x.61.3.455. [DOI] [PubMed] [Google Scholar]
- 85.Edwards G, Orford J, Ehert S, et al. Alcoholism: a controlled trial of “treatment” and “advice.”. J Stud Alcohol. 1977;38:1004–31. doi: 10.15288/jsa.1977.38.1004. [DOI] [PubMed] [Google Scholar]
- 86.Baggaley MR, Morgan-Jones D. Long-term follow-up study of military alcohol treatment programs using post-treatment career as an outcome. J R Army Med Corps. 1993;139:46–8. doi: 10.1136/jramc-139-02-03. [DOI] [PubMed] [Google Scholar]
- 87.Seppa K. Intervention in alcohol abuse among macrocytic. Scand J Prim Health Care. 1992;10:217–22. doi: 10.3109/02813439209014064. [DOI] [PubMed] [Google Scholar]
- 88.Heather N, Whitton B, Robertson I. Evaluation of self-help manual for media-recruited problem drinkers: six-month follow-up results. Br J Clin Psychol. 1986;25(5):19–34. doi: 10.1111/j.2044-8260.1986.tb00667.x. [DOI] [PubMed] [Google Scholar]
- 89.Booth BM, Russell DW. Social support & outcomes of alcoholism treatment: an exploratory analysis. Am J Drug Alcohol Abuse. 1992;18:87–101. doi: 10.3109/00952999209001614. [DOI] [PubMed] [Google Scholar]
- 90.Farragher A, Webb M. Eight-year outcome of problem-drinking among medical inpatients. Alcohol Alcohol. 1991;26(5):635–8. doi: 10.1093/oxfordjournals.alcalc.a045167. [DOI] [PubMed] [Google Scholar]
- 91.Collins GB, Janesz JW. The Cleveland Clinic Alcohol Rehabilitation Program. Clevel Clin Q. 1985;52:245–51. doi: 10.3949/ccjm.52.2.245. [DOI] [PubMed] [Google Scholar]
- 92.Heok KE, Meng KS, Sing TC, Yeo B, Halstead S, Mahendran R. A follow-up study of Asian problem drinkers. Br J Addict. 1990;85:1261–4. doi: 10.1111/j.1360-0443.1990.tb01602.x. [DOI] [PubMed] [Google Scholar]
- 93.McLatchie BH, Lomp KGE. Alcoholics Anonymous affiliation and treatment outcome among a clinical sample of problem drinkers. Am J Drug Alcohol Abuse. 1988;14:309–24. doi: 10.3109/00952998809001553. [DOI] [PubMed] [Google Scholar]
- 94.Miller NS, Veriris JS. Treatment outcome for impoverished alcoholics in an abstinence-based program. Int J Addict. 1995;30:753–63. doi: 10.3109/10826089509048757. [DOI] [PubMed] [Google Scholar]
- 95.Eriksen L, Bjornstad S, Gotestam KG. Social skills training in group for alcoholics: one-year treatment outcome for groups and individuals. Addict Behav. 1986;11:309–29. doi: 10.1016/0306-4603(86)90058-4. [DOI] [PubMed] [Google Scholar]
- 96.Murphy TJ, Pagano RR, Marlatt GA. Lifestyle modification with heavy alcohol drinkers: effects of aerobic exercise and meditation. Addict Behav. 1986;11:175–86. doi: 10.1016/0306-4603(86)90043-2. [DOI] [PubMed] [Google Scholar]
- 97.Gordon AJ, Zrull M. Social networks and recovery: one year after inpatient treatment. J Subst Abuse Treat. 1991;8:143–52. doi: 10.1016/0740-5472(91)90005-u. [DOI] [PubMed] [Google Scholar]
- 98.Burton LC, Paglia MJ, German PS, Shapiro S, Damiano AM. The effect among older persons of a general preventive visit on three health behaviors: smoking, excessive alcohol drinking, and sedentary lifestyle. Prev Med. 1995;24:492–7. doi: 10.1006/pmed.1995.1078. [DOI] [PubMed] [Google Scholar]
- 99.Denney MR, Baugh JL. Sobriety outcome after alcoholism treatment with biofeedback participation: a pilot inpatient study. Int J Addict. 1991;26:335–41. doi: 10.3109/10826089109058889. [DOI] [PubMed] [Google Scholar]
- 100.Feuerlein W, Kufner H. A prospective multicentre study of in-patient treatment for alcoholics: 18- and 48-month follow-up (Munich Evaluation for Alcoholism Treatment, MEAT) Eur Arch Psychiatr Neurol Sci. 1989;239:144–57. doi: 10.1007/BF01739647. [DOI] [PubMed] [Google Scholar]
- 101.Kivlahan DR, Marlatt GA, Fromme K, Coppel DB, Williams E. Secondary prevention with college drinkers: evaluation of an alcohol skills training program. J Consult Clin Psychol. 1990;58:805–10. doi: 10.1037//0022-006x.58.6.805. [DOI] [PubMed] [Google Scholar]
- 102.Smith DI. Evaluation of a residential AA program. Int J Addict. 1986;21:33–49. doi: 10.3109/10826088609063436. [DOI] [PubMed] [Google Scholar]
- 103.Darkes J, Goldman MS. Expectancy challenge and drinking reduction: experimental evidence for a mediational process. J Consult Clin Psychol. 1993;61:344–53. doi: 10.1037//0022-006x.61.2.344. [DOI] [PubMed] [Google Scholar]
- 104.Murphy TJ, Pagano RR, Marlatt GA. Lifestyle modification with heavy alcohol drinkers: effects of aerobic exercise and meditation. Addict Behav. 1986;11:175–86. doi: 10.1016/0306-4603(86)90043-2. [DOI] [PubMed] [Google Scholar]
- 105.Jacobson NO, Silverskiold NP. A controlled study of hypnotic method in the treatment of alcoholism. Br J Addict. 1973;68:25–31. doi: 10.1111/j.1360-0443.1973.tb01218.x. [DOI] [PubMed] [Google Scholar]
- 106.Elvy GA, Wells JE, Baird KA. Attempted referral as an intervention for problem drinking in the general hospital. Br J Addict. 1988;83:83–9. doi: 10.1111/j.1360-0443.1988.tb00455.x. [DOI] [PubMed] [Google Scholar]
- 107.Carpenter RA, Lyons CA, Miller WR. Peer-managed self-control program for prevention of alcohol abuse in American Indian JS students: a pilot evaluation. Int J Addict. 1985;20:299–310. doi: 10.3109/10826088509044912. [DOI] [PubMed] [Google Scholar]
- 108.Brown JM, Miller WR. Impact of motivational interviewing on participation and outcomes in residential alcoholism treatment. Psychology of Addictive Behaviors. 1993;7:211–8. [Google Scholar]
- 109.Miller WR, Dougher MJ. Covert sensitization: alternative treatment procedures for alcoholism. Behav Psychother. 1989;17:203–20. [Google Scholar]
- 110.Timko C, Finney JW, Moos RH, Moos BS. The process of treatment selection among previously untreated help-seeking problem drinkers. J Subst Abuse. 1993;5:203–20. doi: 10.1016/0899-3289(93)90064-i. [DOI] [PubMed] [Google Scholar]
- 111.Telch MJ, Hannon R, Telch CF. A comparison of cessation strategies for the outpatient alcoholic. Addict Behav. 1984;9:103–9. doi: 10.1016/0306-4603(84)90014-5. [DOI] [PubMed] [Google Scholar]
- 112.Alden LE. Behavioral self-management controlled-drinking strategies in a context of secondary prevention. J Consult Clin Psychol. 1988;56:280–6. doi: 10.1037//0022-006x.56.2.280. [DOI] [PubMed] [Google Scholar]
- 113.Donovan DM, Salzberg PM, Chaney EF, Queisser HR. Prevention skills for alcohol-involved drivers. Alcohol Drugs Driving. 1990;6:169–88. [Google Scholar]
- 114.Reynolds KD, Coombs DW, Lowe JG, Peterson PL, Gayoso E. Evaluation of a self-help program to reduce alcohol consumption among pregnant women. Int J Addict. 1995;30:427–43. doi: 10.3109/10826089509048735. [DOI] [PubMed] [Google Scholar]
- 115.Ueshima H, Mikawa K, Baba S, et al. Effect of reduced alcohol consumption on blood pressure in untreated hypertensive men. Hypertension. 1993;21:248–52. doi: 10.1161/01.hyp.21.2.248. [DOI] [PubMed] [Google Scholar]
- 116.Malla A. An outcome study comparing refusers and acceptors of treatment for alcoholism. Can J Psychiatry. 1988;33:183–7. doi: 10.1177/070674378803300304. [DOI] [PubMed] [Google Scholar]
- 117.Saunders JB. The WHO Project on early detection and treatment of harmful drinking. Aust Drug Alcohol Rev. 1987;6:303–8. [Google Scholar]
- 118.Wells-Parker E, Anderson BJ, Landrum JW, Snow RW. Long-term effectiveness of probation, short-term intervention and administration for reducing recidivism. Br J Addict. 1988;83:415–21. doi: 10.1111/j.1360-0443.1988.tb00488.x. [DOI] [PubMed] [Google Scholar]
- 119.Gillet C, Pailli F, Wahl D, Aubin HJ, Pirollet P, Prime T. Outcome of treatment in alcoholic women. Drug Alcohol Depend. 1991;29:189–94. doi: 10.1016/0376-8716(91)90048-4. [DOI] [PubMed] [Google Scholar]
- 120.Smith DI. Evaluation of a residential AA programme for women. Alcohol Alcohol. 1985;20:315–27. [PubMed] [Google Scholar]
- 121.Willenbring ML, Olson DH, Bielinski J. Integrated outpatients treatment for medically ill alcoholic men: results from a quasi-experimental study. J Stud Alcohol. 1995;56:337–43. doi: 10.15288/jsa.1995.56.337. [DOI] [PubMed] [Google Scholar]
- 122.Agostinelli G, Brown JM, Miller WR. Effects of normative feedback on consumption among heavy drinking college students. J Drug Educ. 1995;25:31–40. doi: 10.2190/XD56-D6WR-7195-EAL3. [DOI] [PubMed] [Google Scholar]
- 123.Chalmers TC, Celano P, Sacks HS, Smith H. Bias in treatment assignment in controlled clinical trials. N Engl J Med. 1983;309:1358–61. doi: 10.1056/NEJM198312013092204. [DOI] [PubMed] [Google Scholar]
- 124.Gillman MW, Runyan DK. Bias in treatment assignment in controlled clinical trials. N Engl J Med. 1984;310:1610–1. doi: 10.1056/nejm198406143102419. [DOI] [PubMed] [Google Scholar]
- 125.Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273(5):408–12. doi: 10.1001/jama.273.5.408. [DOI] [PubMed] [Google Scholar]
- 126.Holder H, Longabaugh R, Miller WR, Rubonis AV. The cost effectiveness of treatment for alcoholism: a first approximation. J Stud Alcohol. 1991;52:517–40. doi: 10.15288/jsa.1991.52.517. [DOI] [PubMed] [Google Scholar]
- 127.Rundell OH, Paredes A. Benefit-cost methodology in the evaluation of therapeutic services for alcoholism. Alcohol Clin Exp Res. 1979;3:324–30. doi: 10.1111/j.1530-0277.1979.tb05331.x. [DOI] [PubMed] [Google Scholar]


