Abstract
OBJECTIVE
To determine the preferences of nursing home residents regarding the use of tube feedings and to characterize the clinical, functional, and psychosocial factors that are associated with preferences.
DESIGN
In-person survey.
SETTING
Forty-nine randomly selected nursing homes.
PATIENTS/PARTICIPANTS
Three hundred seventy-nine randomly selected, decisionally capable, nursing home residents.
MAIN RESULTS
Thirty-three percent of participants would prefer tube feedings if no longer able to eat because of permanent brain damage. Factors positively associated with preferences for tube feedings include male gender, African-American race, never having discussed treatment preferences with family members or health care providers, never having signed an advance directive, and believing that tube feeding preferences will be respected by the nursing home staff. Twenty-five percent of the participants changed from preferring tube feedings to not preferring tube feedings on learning that physical restraints are sometimes applied during the tube feeding process.
CONCLUSIONS
Demographic and social factors are associated with preferences for tube feedings. The provision of information about the potential use of physical restraint altered a proportion of nursing home residents' treatment preferences.
Keywords: nursing home residents, life-sustaining treatment preferences, tube feedings, advance directives
Clinical decisions to initiate or withhold artificial feedings for profoundly brain damaged patients are morally troubling at best. Increasingly, clinicians are being urged to turn to their patients for guidance in making these decisions before the point of a health care crisis.1–4 Decisions regarding tube feeding may be even more crucial to nursing home residents than are decisions regarding whether or not to withhold cardiopulmonary resuscitation (CPR). Few nursing home residents are known to survive CPR, but tube feedings have been shown to forestall death for long periods in patients with advanced dementia or debilitating stroke.5 The long-term use of feeding tubes is associated with use of physical restraints to prevent the feeding tube from becoming dislodged. Such immobilization has been shown to cause substantial physical and psychological damage leading to even further diminution of health and quality of life.6
Little is known about nursing home residents’ preferences regarding tube feedings.7–9 Even less is known about the individual factors that are associated with these preferences. Previous surveys usually addressed single nursing home populations and provided inconsistent findings.7–12 To our knowledge, this in-person survey is the first population-based survey that includes randomly selected nursing home residents from a large number of nursing homes.
METHODS
This study analyzes part of a previously described comprehensive survey.13 The sample was drawn from the Philadelphia Consolidated Metropolitan Statistical Area as defined by the U.S. Bureau of the Census. All licensed nursing homes and their residents were considered potentially eligible for inclusion in the study. The sample population was drawn from 294 nursing homes comprising 37,652 licensed nursing home beds. The survey design used a probability-based, stratified, two-stage probability-proportional-to-size cluster design in which the number of licensed beds was used as the measure of size for nursing homes.14 All nursing homes located within the sampling frame were first sorted by state, corporate status (government, not-for-profit, or for-profit), county, and number of beds. In the first stage of sampling, a random sample of 57 nursing homes was drawn with a probability proportional to the number of beds. In the second stage, the number of residents randomly selected from each sampled facility’s bed roster was maintained constant at 30.
Study Subjects and Recruitment
Institutional review board approval was obtained from the University of Pennsylvania’s Human Subjects Committee and each participating nursing home. Of the 57 nursing homes randomly selected, 49 (86%) agreed to participate and 8 (14%) refused. The smallest participating facility had 35 beds, and the largest had 911 beds. Twenty-eight nursing homes were for-profit institutions, 16 were not-for-profit, and 5 were government-sponsored. The distributions of corporate status (e.g., for-profit, not-for-profit, government), size, and location were not statistically different among institutions recruited for study participation and those that refused.
Randomly selected residents were interviewed between September 1992 and November 1993. Eligibility required that residents be able to comprehend the purpose of the study well enough to meet the standards of informed consent.15 To assess comprehension, residents were asked to describe the study purpose in their own words after being read a standardized study description. Residents were required to be verbal, English-speaking, and able to hear, and their responses had to include “my opinion” or “how I feel about medical treatments for life-threatening problems,” or alternatively, they had to offer a statement of their own preferences regarding the use of life-sustaining treatments. All resident responses were transcribed verbatim by the nurse interviewer. Eligibility required that a blinded off-site physician investigator, using predetermined guidelines, had to agree independently with the nurse interviewer that the resident met the standards for informed consent.
Of 1,458 randomly selected nursing home residents who were assessed, 551 (38%) were eligible; 421 (76%) were interviewed as part of the comprehensive survey, and 130 (24%) refused to participate. No significant differences existed between residents who refused and those who participated in terms of gender, age, or location.
Assessment of Tube Feeding Preferences
Eligible nursing home residents were read the following information and were shown the accompanying illustration (Fig. 1):
FIGURE 1.
Tube feeding.
When a person cannot swallow or digest food normally they have to be given food through a tube in the stomach. Tube feeding means that liquid food is poured directly into the stomach through a tube. If someone cannot eat and does not receive tube feedings, they will die. Tube feedings usually do not cause pain.
Each nursing home resident was asked to describe: (1) why someone would need to have tube feedings; (2) how tube feedings are carried out; and (3) what would happen if someone needed to have tube feedings and did not receive them. Only residents able to answer satisfactorily all three questions were asked whether they would want to have tube feedings if they could not eat as a result of permanent brain damage. Brain damage was described as needing help with eating, dressing, bathing, and toileting, and “being unable to recognize anyone that you used to know.” The rationale for this definition was based on our clinical experience; it generally describes the nursing home resident experiencing profound cognitive impairment.
To test whether information about physical restraint alters tube feeding preferences, respondents who either reported preferring tube feedings or were unsure were read the following additional information and were shown the accompanying illustration (Fig. 2):
FIGURE 2.
Tube feeding with physical restraint.
Sometimes people who are confused try to pull the feeding tube out. When this happens, the doctors and nurses sometimes tie the person’s wrists or hands to the bed or chair to prevent the tube from being pulled out. Imagine that you were receiving tube feedings, and you became very confused and began pulling at your feeding tube. If the doctors and nurses had to tie your hands to the bed so you would not pull the tube out, would you want to have the tube feedings?
Individual Factors Assessed
Participants were asked to provide information regarding marital status, religion, number of living children, recent hospitalizations, and whether they had ever experienced a life-threatening illness. Other information gathered included perceptions about whether they believed that most important health care decisions should be made by the doctor, whether they had ever signed a living will or durable power of attorney, and whether they had discussed life-sustaining treatment preferences with their health care providers or family members.
The Nottingham Health Profile was used to assess perceptions of current health status.16 The instrument has 39 yes/no items and addresses the following self-perceived areas of health: physical mobility, energy, pain, emotional reactions, sleep patterns, and social isolation.
The Short Portable Mental Status Questionnaire was used to measure cognitive function.17 The Depression Scale for the Medically Ill was used to measure symptoms of depression.18 The Charlson Comorbidity Index was used to assess severity of current illness.19 The medical record provided age, level of nursing home care, nursing home payment source, and number and type of chronic health conditions.
Statistical Analysis
For dichotomous and nominal variables, responses were characterized in percentage terms after applying appropriate sample weights. Sample weights reflected institution-specific eligibility and refusal rates. Weighting in this manner produced unbiased estimates of population proportions.14 Standard errors of the estimates were calculated to take into account clustering and stratification in the sampling design. To assess the degree of precision in the statistical estimates, 95% confidence intervals (CIs) were computed using standard errors. Similarly, weighted means and appropriately computed errors with 95% CIs were used to summarize the continuous variables.
To analyze the effect of physical restraint information on tube feeding preferences, we calculated the proportion of residents who no longer desired to have tube feedings after receiving the physical restraint information. This proportion was estimated by constructing a CI for the subgroup who changed their preferences from initially preferring tube feedings to not preferring tube feedings by using the appropriate sample weights and an adjusted standard error.
Multivariable logistic regression analyses14 were used to identify a set of factors that were simultaneously significantly associated with preferences for tube feedings. Because of the large number of factors examined, variables were first grouped into domains, including demographic characteristics, clinical characteristics, psychological characteristics, and beliefs regarding personal autonomy in health care decision making. Predictive factors were modeled as interval variables in linear and nonlinear terms, dichotomous variables, or as sets of indicator variables, as appropriate. Backward stepwise algorithms were used to assess the individual variables within each domain. The goal of using these algorithms was to reduce the total number of variables used in the final model-building phase while also minimizing the risk of leaving out important variables. This is an important consideration because of the possibility that marginally significant variables become more significant when controlling for variables in other domains. Thus, the use of a p value equal to .10 served to reduce the risk that important variables were left out.
Factors selected from each domain-specific analysis were then simultaneously entered into a logistic regression model. A backward stepwise algorithm using p less than .05 was used to determine the final model. The use of this more stringent p value serves to ensure that variables in the final model are significant using traditional criteria when assessed on a variable-by-variable basis. All regression analyses were performed using appropriately weighted data. Parameters for the intermediate regression models were estimated using maximum likelihood. Parameters in the final model were re-estimated using SUDAAN software to take into account the stratified sampling design.20,21 This software was used as traditional methods of statistical analysis do not apply to data collected using two-stage sampling (i.e., stratified or cluster) because the assumption that “independent and identically distributed sampling units are drawn from an infinite population” is usually improbable.20 This improbability then typically implies that statistical estimates may be biased and that measures of standard errors (and hence p values) are incorrect. Such biases arise from either planned oversampling of subgroups or unplanned nonresponses (as in this study). SUDAAN uses an approach to produce approximately unbiased estimates with approximately correct standard errors. The SUDAAN approach uses a mathematical technique or Taylor series approximations to obtain parameter estimates and estimates of the standard errors that account for both the intracluster and intercluster variation as well as for planned and unplanned deviations from the desired representativeness.
RESULTS
Of the 421 participants in the comprehensive survey, 379 were able to comprehend the specific questions relating to tube feeding preferences. Of these, 33.4% reported preferring tube feedings, 61.8% reported not preferring tube feedings, and 4.8% reported being unsure.
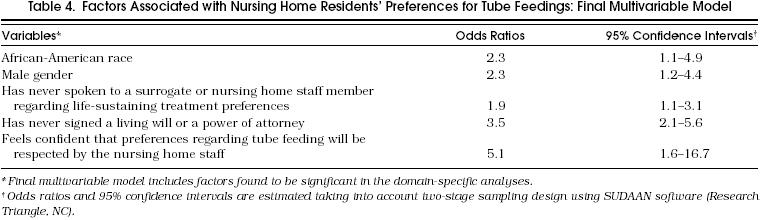
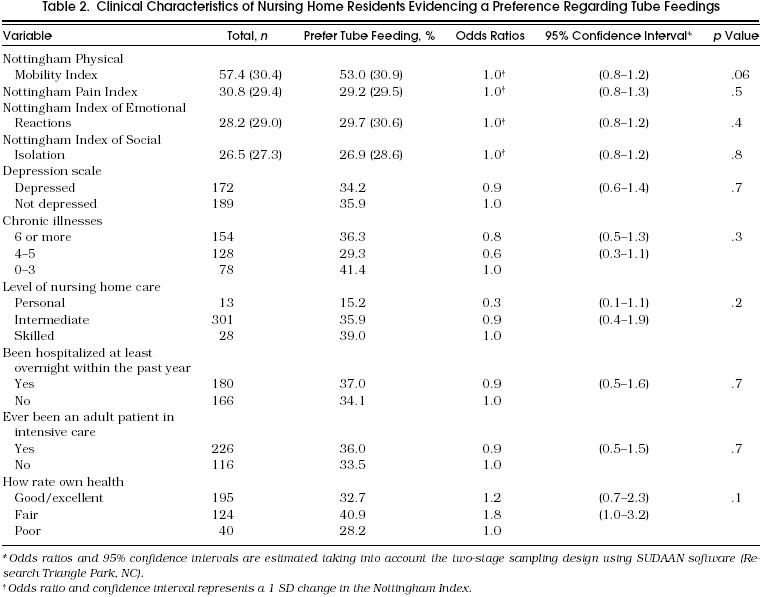
Table 1–Table 3 show the individual factors, 95% CIs, and crude odds ratios (ORs) for each candidate variable, listed by domain, for the 361 study participants who expressed a definite preference either for or against tube feedings. Table 4 shows the ORs for the variables included in the final multivariable logistic regression model. Preferring tube feedings was significantly associated with the following individual factors: male gender, African American race, having never discussed life-sustaining treatment preferences with family members or health care providers, having never signed a living will or durable power of attorney for health care, and believing that tube feeding preferences will be respected by the nursing home staff.
Table 1.
Demographic Characteristics of Nursing Home Residents Evidencing a Preference Regarding Tube Feedings
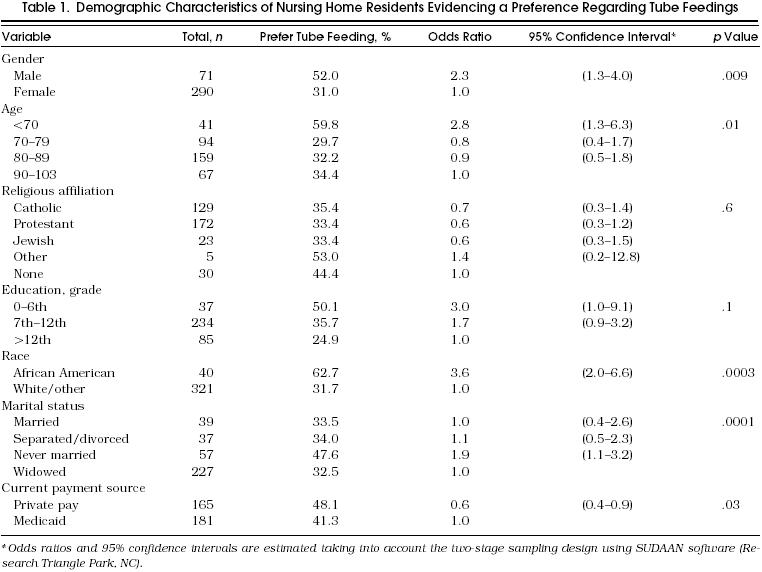
Table 3.
Health Care Decision-Making Characteristics of Nursing Home Residents Evidencing a Preference Regarding Tube Feedings
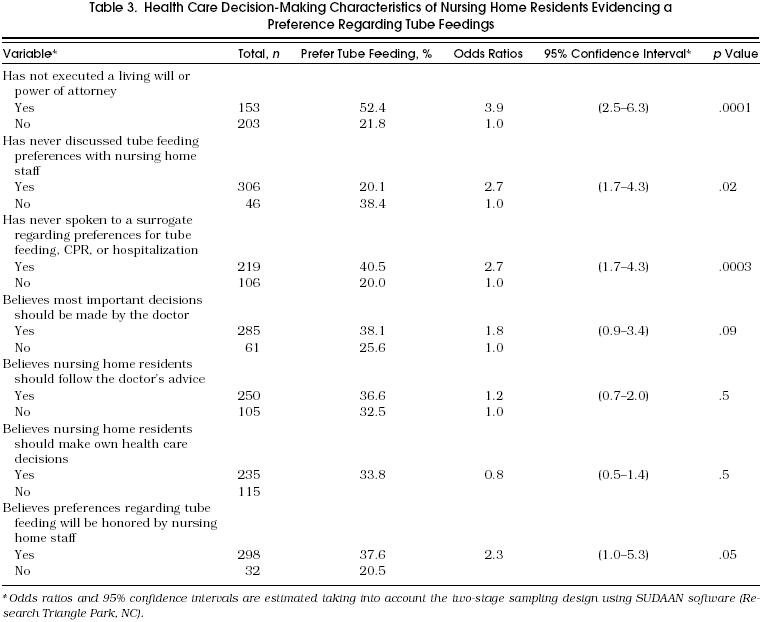
Table 4.
Factors Associated with Nursing Home Residents’ Preferences for Tube Feedings: Final Multivariable Model
Regarding the effect of physical restraint information on preferences for tube feeding, of the 33.4% who initially preferred tube feedings and the 4.8% who were unsure, 25% (95% CI 19%–31%) changed their preference from preferring to not preferring tube feedings after receiving the physical restraint information.
DISCUSSION
One third of the nursing home residents reported preferring tube feedings in the event of no longer being able to eat due to permanent brain damage. This percentage is slightly larger than those reported by previous investigators. In those studies, 16% of subjects “unable to eat,” reported preferring tube feedings if becoming “permanently unconscious,” and 25% of subjects preferred tube feedings if becoming “persistently vegetative.”8,9 Previous studies have shown that the desire for tube feedings tends to decrease as the hypothetical degree of cognitive impairment increases.22–24 This may explain why a larger percentage (53%) of the subjects in another nursing home study opted for tube feedings when provided the hypothetical scenario of being “unable to eat” with no mention of associated cognitive status.7 Likewise, preferences for tube feedings among elderly outpatients has been shown to vary according to hypothetical scenario, with 50% of subjects opting for tube feedings in the event of “severely impaired health,”25 while 2.4% in another study opted for tube feedings if having “Alzheimer’s disease.”26 As few studies have investigated preferences for tube feedings using comparable hypothetical scenarios; it is difficult to draw conclusions about whether the preferences of nursing home residents and elderly outpatients’ vary substantially.
Our study did not specifically investigate the relation between tube feeding preferences and varying levels of cognitive impairment; however, it is clear that a substantial number of nursing home residents would prefer to have tube feedings despite having irreversible brain damage. There are a number of potential reasons why decisions regarding the use of tube feedings are particularly difficult for both patients and caregivers.27 Perhaps study participants fear that withholding food and water leads to a painful death. Several reports have attempted to address this misdirected fear.28,29 Clinical literature purports that terminal patients may not benefit at all from artificial hydration.29–33 Many individuals may also have difficulty conceptualizing the provision of food and hydration as a medical treatment rather than a basic life necessity. Historically, the provision of food and water has been equated with caring and conjures up images of nurturing. Thus, for some, forgoing food and hydration may be equated with neglect and abandonment. Future research needs to investigate individuals’ attitudes toward the symbolic meanings of food and water and the role of beliefs in decisions regarding tube feedings.
We also found it somewhat surprising that information about the potential use of physical restraint did not alter more patients’ preferences. This, too, seems to indicate a certain perception that the benefits of food and water outweigh the risks and potential indignities of physical restraint.
The individual factors found to be associated with a preference for tube feedings (male gender, African-American race, and having never discussed life-sustaining treatment preferences with others) are consistent with those found in previous studies. For instance, it had previously been reported that men tend to opt for life-sustaining treatments in scenarios of terminal illness more often than do women.22 Garrett et al. reported similar findings in relation to race, with African-Americans preferring the use of life-sustaining treatments more frequently than white counterparts.26 Possible explanations are concerns regarding access to appropriate care, and variations in cultural beliefs regarding the meaning of suffering and the dying process. Blackhall et al. reported that significant differences may exist among elderly individuals from differing ethnic backgrounds regarding disclosure of terminal diagnoses and end-of-life medical decisions.34 Similarly, Klessig reported variations among different cultural groups regarding the role of patient autonomy and the withholding and withdrawing of life-sustaining treatments.35
The finding that nursing home residents who have not signed advance directives are more likely to prefer tube feedings might be explained by the common impression that advance directives are primarily mechanisms for refusing medical intervention rather than for requesting it. A general confidence seems to prevail that even if one has never communicated treatment preferences, one’s health care wishes will, nonetheless, be followed. Many patients rely on the assumption that family and health care providers intuitively know their treatment preferences and will make concordant decisions when the time arrives. Such beliefs may be ill-founded, however, as previous studies have shown that health care providers and family members are frequently unable to predict patient preferences in the absence of explicit discussions.36–38
The fact that 62% of the nursing home residents were unable to participate in this survey due to cognitive impairment does not result in study bias. It does, however, require that these study results be regarded as applying only to decisionally capable nursing home residents.
In conclusion, our results have shown that one third of nursing home residents prefer tube feedings despite a dismal long-term clinical outlook. Such findings have profound implications for a rapidly aging society. Further qualitative research is sorely needed to assess the role of human values, religious beliefs, and cultural variations underlying individual preferences regarding life-sustaining treatments.
Table 2.
Clinical Characteristics of Nursing Home Residents Evidencing a Preference Regarding Tube Feedings
References
- 1.Emanuel LL, Barry MJ, Stoeckle JD, Emanuel EJ. Advance directives for medical care—a case for greater use. N Engl J Med. 1991;324:889–95. doi: 10.1056/NEJM199103283241305. [DOI] [PubMed] [Google Scholar]
- 2.Orentlicher D. Advance medical directives. JAMA. 1990;263:2365–7. doi: 10.1001/jama.263.17.2365. [DOI] [PubMed] [Google Scholar]
- 3.Singer PA. Advancing the cause of advance directives. Arch Intern Med. 1992;152:22–4. [PubMed] [Google Scholar]
- 4.Finucane TE, Shumway JM, Powers RL, D’Alessandri RM. Planning with elderly outpatients for contingencies of severe illness. J Gen Intern Med. 1988;3:322–5. doi: 10.1007/BF02595788. [DOI] [PubMed] [Google Scholar]
- 5.Tresch DD, Neahring JM, Duthie EH, Mark DH, Kartes SK, Aufderheide TP. Outcomes of cardiopulmonary resuscitation in nursing homes: can we predict who will benefit? Am J Med. 1993;95:123–30. doi: 10.1016/0002-9343(93)90252-k. [DOI] [PubMed] [Google Scholar]
- 6.Evans LK, Strumpf NE. Tying down the elderly: a review of the literature on physical restraint. J Am Geriatr Soc. 1989;38:65–74. doi: 10.1111/j.1532-5415.1989.tb01571.x. [DOI] [PubMed] [Google Scholar]
- 7.Kayser-Jones J. The use of nasogastric feeding tubes in nursing homes—patient, family and health care provider perspectives. Gerontologist. 1990;30:469–79. doi: 10.1093/geront/30.4.469. [DOI] [PubMed] [Google Scholar]
- 8.Gerety MB, Chiodo LK, Kanter DN, Tuley MR, Cornel JE. Medical treatment preferences of nursing home residents. Relationship to function and concordance with surrogate decision-makers. J Am Geriatr Soc. 1993;141:953–60. doi: 10.1111/j.1532-5415.1993.tb06761.x. [DOI] [PubMed] [Google Scholar]
- 9.Danis M, Southerland LI, Garrett JM, et al. A prospective study of advance directives for life-sustaining care. N Engl J Med. 1991;324:882–8. doi: 10.1056/NEJM199103283241304. [DOI] [PubMed] [Google Scholar]
- 10.Wetle T, Levkoff S, Cwikel J, Rosen A. Nursing home resident participation in medical decisions: perceptions and preferences. Gerontologist. 1988;28(6):32–8. [PubMed] [Google Scholar]
- 11.Ouslander JG, Tymchuk AJ, Rahban B. Health decisions among elderly long-term care residents and their potential proxies. Arch Intern Med. 1989;149:1367–72. [PubMed] [Google Scholar]
- 12.Michelson C, Mulvihill M, Hsu M, Olson E. Eliciting medical care preferences from nursing home residents. Gerontologist. 1991;31:358–63. doi: 10.1093/geront/31.3.358. [DOI] [PubMed] [Google Scholar]
- 13.O’Brien LA, Grisso JA, Maislin G. Nursing home residents’ preferences for life-sustaining treatments. JAMA. 1995;274:1775–9. [PubMed] [Google Scholar]
- 14.Kish L. New York, NY: John Wiley and Sons; 1965. Survey Sampling; pp. 230–1–424–7. [Google Scholar]
- 15.Jonsen AR, Siegler M, Winslade WJ. 2nd ed. New York, NY: Macmillan Publishing Co; 1986. Clinical Ethics: A Practical Approach to Ethical Decisions in Clinical Medicine; pp. 52–65. [Google Scholar]
- 16.Hunt SM, McEwen J, McKenna SP. Measuring health status: a new tool for clinicians and epidemiologists. JR Coll Gen Pract. 1985;35:185–8. [PMC free article] [PubMed] [Google Scholar]
- 17.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;25:433–41. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 18.Koenig HG, Cohen HJ, Blazer DG, Meador KG, Westlund R. A brief depression scale for use in the medically ill. Int J Psychiatr Med. 1992;22:183–95. doi: 10.2190/M1F5-F40P-C4KD-YPA3. [DOI] [PubMed] [Google Scholar]
- 19.Charlson ME, Pompei P, Ales KL, MacKenzi CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 20.LaVange LM, Stearns SC. Innovative strategies using SUDAAN for analysis of health surveys with complex samples. Stat Methods Med Res. 1996;5:311–29. doi: 10.1177/096228029600500306. [DOI] [PubMed] [Google Scholar]
- 21. SUDAAN version 6.33. Research Triangle Park, NC: Research Triangle Institute; 1993.
- 22.Frankl D, Dye RK, Bellamy PE. Attitudes of hospitalized patients towards life support: a survey of 200 medical inpatients. Am J Med. 1989;86:645–8. [PubMed] [Google Scholar]
- 23.Cohen-Mansfield J, Droge JA, Billig N. Factors influencing hospital patients’ preferences in the utilization of life-sustaining treatment. Gerontologist. 1992;32:89–95. doi: 10.1093/geront/32.1.89. [DOI] [PubMed] [Google Scholar]
- 24.Cohen-Mansfield JC, Rabinovich BA, Lipson S, et al. The decision to execute a durable power of attorney for health care and preferences regarding the utilization of life-sustaining treatments in nursing home residents. Arch Intern Med. 1991;151:289–94. [PubMed] [Google Scholar]
- 25.Ouslander JG, Tymchuk AJ, Krynski MD. Decisions about enteral tube feeding among the elderly. J Am Geriatr Soc. 1993;41:70–7. doi: 10.1111/j.1532-5415.1993.tb05951.x. [DOI] [PubMed] [Google Scholar]
- 26.Garrett JM, Harris RP, Norburn JK, et al. Life-sustaining treatments during terminal illness: who wants what? J Gen Intern Med. 1993;8:361–8. doi: 10.1007/BF02600073. [DOI] [PubMed] [Google Scholar]
- 27.Slomka J. What do apple pie and motherhood have to do with feeding tubes and caring for the patients? Arch Intern Med. 1995;155:1258–63. [PubMed] [Google Scholar]
- 28.Sullivan RG. Accepting death without artificial nutrition or hydration. J Gen Intern Med. 1993;8:220–7. doi: 10.1007/BF02599271. [DOI] [PubMed] [Google Scholar]
- 29.Ahronheim JC. ‘Starvation’ a misnomer—a physician’s view Soc Right to Die Newsletter. Spring. 1989;1:7. [Google Scholar]
- 30.Billings JA. Philadelphia, Pa: JB Lippincott Co; 1985. Outpatient management of advanced cancer. In: Symptom Control, Support, and Hospice-in-the-Home. pp. 58–68. [Google Scholar]
- 31.Andrews MR, Levine AM. Dehydration in the terminal patient: perception of hospice nurses. Am J Hospice Care. 1989;6:31–4. doi: 10.1177/104990918900600112. [DOI] [PubMed] [Google Scholar]
- 32.Cox SS. Is dehydration painful? Ethics Medics. 1976;12:1–2. [PubMed] [Google Scholar]
- 33.Miller RJ, Albright PG. What is the role of nutritional support and hydration in the terminal cancer patient? Am J Hospice Palliative Care. 1989;6(6):33–8. [Google Scholar]
- 34.Blackhall LJ, Murphy ST, Fran KG, et al. Ethnicity and attitudes toward patient autonomy. JAMA. 1995;274:820–5. [PubMed] [Google Scholar]
- 35.Klessig J. The effect of values and culture on life-support decisions in cross-cultural medicine—a decade later. West J Med. 1992;157:316–22. . Special issue. [PMC free article] [PubMed] [Google Scholar]
- 36.Zweibel NR, Cassel CK. Treatment choices at the end of life: a comparison of decisions by older patients and their physician-selected proxies. Gerontologist. 1989;29:615–21. doi: 10.1093/geront/29.5.615. [DOI] [PubMed] [Google Scholar]
- 37.Ebell MH, Doukas DJ, Smith MA. The do-not-resuscitate order: a comparison of physician and patient preferences and decision-making. Am J Med. 1991;91:255–60. doi: 10.1016/0002-9343(91)90124-g. [DOI] [PubMed] [Google Scholar]
- 38.Allison B, Seckler AB, Meler DE, Mulvihill M, Paris BE. Substitute judgment: how accurate are proxy predictions? Ann Intern Med. 1991;115:92–8. doi: 10.7326/0003-4819-115-2-92. [DOI] [PubMed] [Google Scholar]


