Abstract
OBJECTIVE
To examine physician and patient characteristics related to the ordering of imaging studies in a general medicine practice and to determine whether physician gender influences ordering patterns.
DESIGN
Retrospective cohort study.
SETTING
Hospital-based academic general medicine practice of 29 attending physicians.
PATIENTS
All 8,203 visits by 5,011 patients during a 6-month period.
METHODS
For each visit the following variables were abstracted from the electronic patient record: patient age, patient gender, visit urgency, visit type, and physician seen. All diagnostic imaging studies performed within 30 days of each outpatient visit were identified from the hospital’s Radiology Information System. Screening mammography was not included in the analysis. Physician variables included gender and years since medical school graduation. Logistic regression analysis was used to evaluate the effect of various patient, physician, and visit characteristics on the probability of a diagnostic imaging study being ordered.
RESULTS
Patient age, urgent visits, visit frequency, and the gender of the physician were all significantly related to the ordering of an imaging study. Correcting for all other factors, the ordering of an imaging study during an outpatient medical visit was 40% more likely if the physician was female (odds ratio = 1.40; 95% confidence interval [CI] 1.01, 1.95). Female physicians were 62% more likely (95% CI 0.99, 2.64) than male physicians to order an imaging study for a male patient and 21% more likely (95% CI 0.87, 1.69) to order an imaging study for a female patient.
CONCLUSIONS
Physician gender is a predictor of whether an outpatient medical visit generates an imaging study. Reasons for this observation are unclear, but may be the result of different practice styles of male and female physicians or unmeasured patient characteristics.
Keywords: physician gender, outpatients, diagnostic imaging, physician practice patterns
During the past few years there has been growing interest in the analysis of physician practice patterns and the role that the gender of the physician and the gender of the patient play in the delivery of health care. Studies have addressed the different utilization rates by male and female physicians of gender-specific screening tests,1–3 gender-neutral screening tests,2,4 and hormone replacement therapy.5 These studies suggest that female physicians provide more preventive services than male physicians.
To our knowledge no study has examined the role that the physician’s gender plays in the utilization of diagnostic imaging studies. Although the gender of the physician should not influence what imaging test a patient needs, studies have found that a number of non-illness-related factors influence resource utilization, including geographic region,6 patient race,7 and patient socioeconomic status.8
The purpose of our study was to examine the role that the gender of the physician plays in the utilization of diagnostic imaging studies (plain film “x-rays,” computed tomography [CT scan], magnetic resonance imaging [MRI], ultrasonography, and diagnostic mammography) in a hospital-based outpatient medicine practice.
METHODS
Setting
The study site was an urban, hospital-based, adult medicine practice with more than 40,000 visits annually. Approximately 30% of patients in this practice come from medically underserved areas and are covered by Medicaid or free care, and 13% are not English speaking. The hospital is served by an integrated clinical computing system that has been described previously.9,10 The outpatient medical record and the Radiology Information System are two components of the electronic patient record. Order entry through the computing system provides the only means for ordering radiographic procedures at the hospital.
Study Design
Every outpatient visit to an attending physician (16 male, 7 female) or a general medicine fellow (4 male, 2 female) in the hospital-based general internal medicine practice between January 1 and June 30, 1994 was included in the study. Data abstracted from the outpatient medical record for each of these visits included patient age, the gender of the patient, visit urgency, visit type, and physician seen. We also determined the number of outpatient visits each patient made to the practice during the 6-month study period. A visit was classified as urgent if it occurred within 2 days of the time the visit was scheduled. Visit type was categorized as either “new,” if the patient had not been seen previously in the practice; or “repeat” if the patient had been seen previously in the practice. Information related to the physician seen included the gender of the physician, years since graduation from medical school, and an indicator of discordance between the gender of the physician and that of the patient.
The hospital’s Radiology Information System was then searched to determine if the outpatient medical visit had generated an imaging study. All imaging studies ordered by the study physicians were ordered through the hospital’s Radiology Information System. An imaging study was determined to be generated by the outpatient visit if the physician who saw the patient ordered a study within 30 days of the outpatient visit. The 30-day period following the outpatient visit was defined as the inclusion “window.” If the patient was admitted to the hospital within 30 days of the outpatient visit, the inclusion window was “closed” on the day before admission. If the patient had another outpatient visit within 30 days, the initial inclusion window was closed on the day before the subsequent outpatient visit and a new 30-day inclusion window was opened.
Imaging studies were defined as “plain film” radiographs, any ultrasound, CT or MRI study, or diagnostic mammogram. Screening mammograms were excluded because these studies are ordered according to standardized guidelines. Nuclear medicine studies were not included, as this information was not available from our database.
Statistical Methods
Logistic regression analysis was used to evaluate the effect of various patient, physician, and visit characteristics on the probability of a diagnostic imaging study being ordered as the result of an outpatient visit. Our primary interest was in determining the importance of the gender of the physician as it relates to the use of outpatient diagnostic imaging. The unit of analysis used in our study was the physician. In order to account for the within-physician correlation, the generalized estimating equation (GEE) approach11 was used for estimation. This method is appropriate for an analysis of this type of repeated measures study.12
Odds ratios (ORs) and associated 95% confidence intervals (CIs) calculated from the logistic regression parameter estimates are reported as measures of effect size. Factors included as potential confounders in the analysis were patient age and gender, the logarithm of the number of times the patient was seen in 6 months, the gender of the physician, years since graduation from medical school, gender discordance between physician and patient, new versus repeat patient visit, and whether the visit was urgent (defined as a visit that occurred within 2 days of the time it was scheduled). Bivariable analyses were performed for each of the variables. A multivariable model was fit with all of the covariates in order to evaluate the effect of the gender of the physician after correcting for all potentially confounding factors.
RESULTS
A total of 8,203 visits by 5,011 patients to the 29 physicians were made during the study period. Patient, physician, and visit characteristics related to the gender of the physician are shown in Table 1. Of visits to female physicians, 11.3% generated an imaging study, compared with 8.5% of visits to male physicians (p < .0001). The proportion of patient visits to each individual physician that generated an imaging study is provided in Figure 1.
Table 1.
Patient, Physician and Visit Characteristics Related to the Gender of the Physician
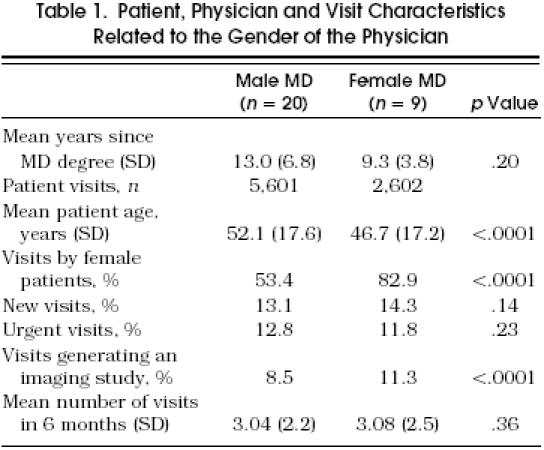
Figure 1.
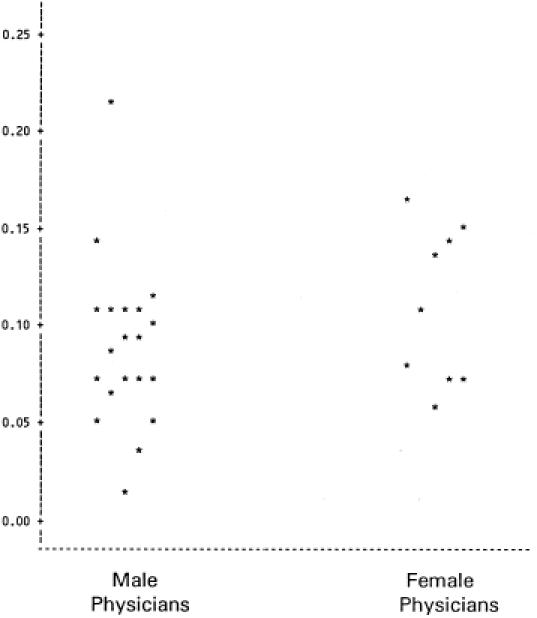
Proportion of patient visits to each physician resulting in an imaging study.
Results from the logistic regression models are presented in Table 2. Bivariable analyses indicated that urgent visits, increasing patient age, and visit frequency had the strongest association with the ordering of an imaging study. The gender variables (female physician, female patient, and physician-patient gender discordance) each were related to an increase in the probability of an imaging study being ordered. The ORs for the gender variables were all approximately 1.2, but only physician-patient gender discordance was significant at the 5% level. New patient visits and more years since the physician graduated from medical school were both associated with decreased probability of ordering an imaging study, but neither of these factors was statistically significant.
Table 2.
Predictors of an Outpatient Visit Generating an Imaging Study
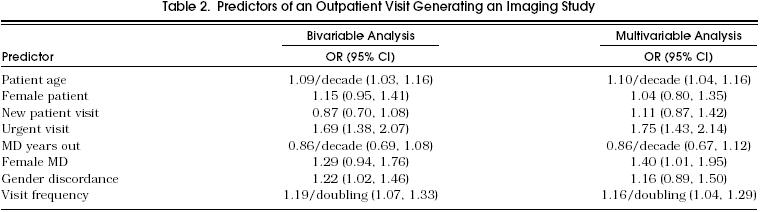
In the multivariable model using GEE (to account for within-physician correlation while using the physician as the unit of analysis), urgent visits, increasing patient age, visit frequency, and the gender of the physician were the only factors that reached statistical significance. Correcting for all other factors considered, the ordering of an imaging study was 75% more likely for an urgent visit than for a nonurgent visit; 10% more likely for each additional decade of patient age; 16% more likely for each doubling of visit frequency; and 40% more likely if the ordering physician was female.
To further investigate the role of gender discordance between patients and physicians, we fit another multivariable model replacing the discordance indicator with a standard interaction term for the gender of the physician and the gender of the patient. This analysis showed similar results in general, but also allowed examination of the effect of the gender of the physician on the ordering of imaging studies for male and female patients. For male patients, a visit to a female physician was 62% (95% CI 0.99, 2.64) more likely to generate an imaging study than a visit to a male physician. For female patients, a visit to a female physician was 21% (95% CI 0.87, 1.69) more likely to generate an imaging study than a visit to a male physician.
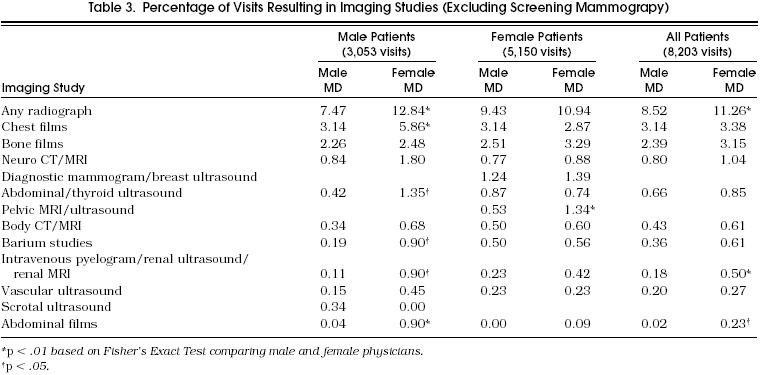
A detailed breakdown of all imaging studies ordered is provided in Table 3. These data are reported as a function of the gender of the patient and the gender of the physician. For male patients, female physicians were more likely to order each type of imaging study except scrotal ultrasound. These differences were statistically significant for chest films, abdominal or thyroid ultrasound, barium studies, intravenous pyelogram, renal ultrasound or renal MRI, and abdominal films. For female patients, female physicians were significantly more likely to order pelvic MRI or pelvic ultrasound than male physicians.
Table 3.
Percentage of Visits Resulting in Imaging Studies (Excluding Screening Mammograpy)
DISCUSSION
The gender of the physician was a significant predictor of whether an outpatient visit generated an imaging study. Our model controlled for multiple other variables including patient age and gender, years of physician experience, concordance or discordance between the gender of the physician and the gender of the patient, visit frequency, visit urgency, and visit type. Many of these variables serve as surrogate measures of illness severity.
Other factors influencing the ordering of an imaging study are consistent with conventional expectations. For example, older patients, patients seen for an urgent visit, and frequently seen patients would be expected to be sicker and more in need of diagnostic imaging than younger patients and those seen less frequently. In addition, patients seen urgently are more likely to be seen by a physician other than their primary care provider who may not be familiar enough with the patient to forgo diagnostic imaging.
The current literature contains several studies that address the influence of the gender of the physician on preventive care practice styles. In a study based on data from the National Medical Expenditure Survey, Franks and Clancy reported that patients of female physicians were less likely to be deficient for Pap tests and mammograms than patients of male physicians.2 Majeroni et al. reported that female physicians were significantly more likely to give influenza vaccines and to check for fecal occult blood than were male physicians.4 Similarly, Kreuter et al. found that patients of female physicians were 74% more likely to undergo a Pap test and 56% more likely to undergo cholesterol screening than patients of male physicians.1 Lurie et al. also found a greater use of female-specific screening tests by female physicians,13 and Seto et al. recently reported that female physicians were more likely to prescribe hormone replacement therapy than were male physicians.5
Fewer studies have examined the role of the gender of the physician on diagnostic ordering behavior. In a study of gender differences in practice styles among general practitioners in Holland, Bensing et al. reported that female general practitioners ordered more laboratory tests and provided more counseling, but wrote fewer prescriptions and performed fewer technical interventions than their male counterparts.14
The reason that female physicians order more diagnostic imaging studies than male physicians is unclear. One possible explanation is that female physicians see a different patient mix than male physicians. Bensing et al. found that female general practitioners were more likely to see patients with obstetric or gynecologic problems.14 Such bias in patient mix could account for a higher utilization of gender-specific imaging studies. In our study we considered gender-specific imaging studies to be diagnostic mammography, breast ultrasound, pelvic MRI or ultrasound, and scrotal ultrasound. Among outpatient visits that resulted in an imaging study (Table 3), gender-specific studies accounted for an identical proportion of studies ordered by male physicians (2.11 of 8.52, 24.77%) and female physicians (2.73 of 11.26, 24.25%). By factoring the gender of the patient into the multivariable model, we further corrected for any potential bias conferred by the fact that female physicians see a larger percentage of female patients.
Another potential explanation for greater utilization of imaging studies by female physicians is that they care for a sicker population of patients than male physicians. Although we do not know the specific complaints that generated an imaging study, our model controlled for visit frequency and visit urgency as surrogate measures of illness severity. In addition, the average age of patients seen by female physicians was significantly lower (46.7 years) than that of patients seen by male physicians (52.1 years). Presumably, the younger patients seen by female physicians would be less sick than the older patients seen by male physicians.
A third possible explanation for the observed difference in ordering patterns may relate to the health beliefs of patients who seek female physicians or to differences in the practice styles of male and female physicians. Bertakis et al. found that women patients coming for a first visit to a primary care practice reported themselves to be significantly less healthy than male patients coming to the same practice.15 A perception of ill health might result in more patient request for imaging studies. In our study, female physicians did care for a larger percentage of female patients than did male physicians; however, our analysis controlled for the gender of the patient. In addition, most of the additional studies ordered by women physicians in our study were for male patients (Table 3).
Roter et al. analyzed audiotapes of 537 adult visits to primary care physicians and concluded that, compared with male physicians, female physicians engaged in more positive talk, partnership building, question asking, and information giving.16 West, in a study of physician-patient interactions, concluded that male physicians formulate directives as a command in contrast to female physicians who issue directives in the form of a proposal.17 It is possible that patients who consider themselves to be sicker would seek out physicians whom they perceive to have a more collaborative style and that this combination of physician and patient characteristics might result in more diagnostic tests being ordered. Alternatively, women physicians who use a more collaborative interviewing style might uncover more problems that require diagnostic imaging. A final possibility is that female physicians are more uncomfortable with higher levels of uncertainty and seek to reduce uncertainty by performing more diagnostic testing. Our study did not explore patient health beliefs or physician communication styles. However, male patients, for whom most of the additional studies were ordered, have not been reported to consider themselves to be sicker, nor have they been reported to specifically seek out female physicians as providers.
Our study is limited by the fact that it was conducted at a single institution with a relatively small number of female physicians and that we did not have information on the diagnosis or complaint that prompted the patient visit. Although only nine female physicians are included in our study, the utilization rates for each physician, as presented in Figure 1, indicate that it is unlikely that our results were influenced by the ordering patterns of one or two female physicians. Furthermore, the use of the GEE method, which accounts for within-physician correlations, protects against the undue influence of outliers. Surrogate measures of illness severity (patient age, visit frequency, and visit urgency) suggest that our results cannot be explained by female physicians seeing a sicker population of patients.
Another potential limitation is that the inclusion window was closed on the day before an admission. Thus, studies performed within 24 hours of admission were eliminated. This was done to exclude routine preadmission studies from the analysis. The gender differences that we observed would be diminished if patients of male physicians were more likely to be admitted within 24 hours of a diagnostic study than patients of female physicians. However, we have no reason to believe that this is the case.
We did not address the effect that differing utilization rates of diagnostic imaging may have on patient outcomes or on the subsequent utilization of other health care resources. We make no representation as to the appropriateness of the various practice patterns discussed. Further research is needed to better understand the impli-cations of these findings for patient outcome and health care costs.
References
- 1.Kreuter MW, Strecher VJ, Harris R, Kobrin SC, Skinner CS. Are patients of women physicians screened more aggressively? J Gen Intern Med. 1995;10:119–25. doi: 10.1007/BF02599664. [DOI] [PubMed] [Google Scholar]
- 2.Franks P, Clancy CM. Physician gender bias in clinical decision making: screening for cancer in primary care. Med Care. 1993;31:213–8. doi: 10.1097/00005650-199303000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Levy S, Dowling P, Boult L, Monroe A, McQuade W. The effect of physician and patient gender on preventive medicine practices in patients older than fifty. Fam Med. 1992;24:58–61. [PubMed] [Google Scholar]
- 4.Majeroni BA, Karuza J, Wade C, McCreadie M, Calkins E. Gender of physicians and patients and preventive care for community-based older adults. J Am Board Fam Pract. 1993;6:359–65. [PubMed] [Google Scholar]
- 5.Seto TB, Taira DA, Davis RB, Safran C, Phillips RS. Effect of physician gender on the prescription of estrogen replacement therapy. J Gen Intern Med. 1996;11:197–203. doi: 10.1007/BF02642475. [DOI] [PubMed] [Google Scholar]
- 6.Wennberg JE, Freeman JL, Shelton RM, Bubolz TA. Hospital use and mortality among Medicare beneficiaries in Boston and New Haven. N Engl J Med. 1989;321:1168–73. doi: 10.1056/NEJM198910263211706. [DOI] [PubMed] [Google Scholar]
- 7.Wenneker MB, Epstein AM. Racial inequalities in the use of procedures for patients with ischemic heart disease in Massachusetts. JAMA. 1989;261:253–7. [PubMed] [Google Scholar]
- 8.Wenneker MB, Weissman JS, Epstein AM. The association of payer with utilization of cardiac procedures in Massachusetts. JAMA. 1990;264:1255–60. [PubMed] [Google Scholar]
- 9.Bleich HL, Beckley RF, Horowitz GL, et al. Clinical computing in a teaching hospital. N Engl J Med. 1995;312:756–64. doi: 10.1056/NEJM198503213121205. [DOI] [PubMed] [Google Scholar]
- 10.Safran C, Bleich HL, Slack WV. Role of computing in patient care in two hospitals. MD Comput. 1989;6:141–8. [PubMed] [Google Scholar]
- 11.Zeger SL, Liang K-Y. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30. [PubMed] [Google Scholar]
- 12.Lipsitz SR, Fitzmaurice GM, Orav EJ, Laird NM. Performance of generalized estimating equations in practical situations. Biometrics. 1994;50:270–8. [PubMed] [Google Scholar]
- 13.Lurie N, Slater J, McGovern P, Ekstrum J, Quam L, Margolis K. Preventive care for women. Does the sex of the physician matter? N Engl J Med. 1993;329:478–82. doi: 10.1056/NEJM199308123290707. [DOI] [PubMed] [Google Scholar]
- 14.Bensing JM, Brink-Muinen AVD, DeBakker DH. Gender differences in practice styles: a Dutch study of general practice. Med Care. 1993;31:219–29. doi: 10.1097/00005650-199303000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Bertakis KD, Helms J, Callahan EJ, et al. The influence of gender of physician practice styles. Med Care. 1995;33:407–16. doi: 10.1097/00005650-199504000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Roter D, Lipkin M, Korsgaard A. Sex differences in patients’ and physicians’ communication during primary care medicine visits. Med Care. 1991;29:1083–93. doi: 10.1097/00005650-199111000-00002. [DOI] [PubMed] [Google Scholar]
- 17.West C. Reconceptualizing gender in physician-patient relationships. Soc Sci Med. 1993;36:57–66. doi: 10.1016/0277-9536(93)90305-n. [DOI] [PubMed] [Google Scholar]


