Abstract
OBJECTIVE
To evaluate the accuracy of a preliminary diagnosis based solely on patient history and physical examination in medical outpatients with abdominal or chest pain.
DESIGN
Prospective observational study.
setting
General medical outpatient clinic in a university teaching hospital.
participants
One hundred ninety new, consecutive patients with a mean age of 44 years (SD = 14 years, range 30–58 years) with a main complaint of abdominal or chest pain.
measurements and main results
The preliminary diagnosis, established on the basis of patient history and physical examination, was compared with a final diagnosis, obtained after workup at completion of the chart. A nonorganic cause was established in 66 (59%) of 112 patients with abdominal pain and in 65 (83%) of 78 with chest pain. The preliminary diagnosis of “nonorganic” versus “organic” causes was correct in 79% of patients with abdominal pain and in 88% of patients with chest pain. An “undoubted” preliminary diagnosis predicted a correct assessment in all patients with abdominal pain and in all but one patient with chest pain. Overall, only 4 patients (3%) were initially incorrectly diagnosed as having a nonorganic cause of pain rather than an organic cause. In addition, final nonorganic diagnosis (n = 131) was compared with long-term follow-up by obtaining information from patients and, if necessary, from treating physicians. Follow-up information, obtained for 71% of these patients after a mean of 29 months (range 18–56 months) identified three other patients that had been misdiagnosed as having abdominal pain of nonorganic causes. Compared with follow-up, the diagnostic accuracy for nonorganic abdominal and chest pain at chart completion was 93% and 98%, respectively.
conclusions
A preliminary diagnosis of nonorganic versus organic abdominal or chest pain based on patient history and physical examination proved remarkably reliable. Accuracy was almost complete in patients with an “undoubted” preliminary diagnosis, suggesting that watchful waiting can be recommended in such cases.
Keywords: abdominal pain, chest pain, outpatients, nonorganic diagnosis, patient history
A bdominal and chest pain are among the most frequent main complaints of patients in ambulatory care.1,2 A substantial percentage of these complaints do not have readily discernible organic causes. Nonorganic diagnoses are made in up to 60% of patients in primary care that present with abdominal pain,3 and in approximately 80% of patients with chest pain.1 An extensive workup in patients with abdominal or chest pain suspected of having nonorganic causes may identify only a few patients with organic causes and may therefore have a very low diagnostic yield.4–8 This suggests that additional and sometimes costly investigations might be unnecessary.1,5,9–13
There are a few studies on the diagnostic accuracy of physicians’ initial assessments of nonorganic versus organic diagnoses in patients with abdominal or chest pain in primary care.1,3,13–15 However, most of these studies are not prospective, and none are with patients in general medical clinics that include a long-term follow-up. Furthermore, it is not entirely clear how diagnostic accuracy varies with the degree of certainty that the primary care physician attaches to the initial diagnosis. Consequently, primary care physicians are often mired in doubt about whether to rely on their initial and preliminary diagnosis of a nonorganic cause of pain or whether to initiate more extensive testing.
The aim of this prospective study was to appraise the quality of the physician’s initial diagnostic assessment based on patient history and physical examination for patients presenting in general medical outpatient clinics with abdominal or chest pain. Two comparisons were performed. Initial diagnoses characterized as “undoubted” or “probable” were compared with (1) the final diagnosis established after workup and completion of the chart, and (2) long-term follow-up results.
METHODS
Setting and Medical Staff
The Medical Outpatient Clinic is a division of the Department of Internal Medicine of the University Hospital Basel. This teaching hospital provides primary, secondary, and tertiary care for a region with approximately 200,000 inhabitants. Each year about 20,000 general internal medical consultations for approximately 5,000 new patients are provided by the Medical Outpatient Clinic, which is open to the public without referral. Approximately 80% of the cases are primary care walk-in patients; 20% of the patients are referred to the clinic by physicians of other departments, by general practitioners, or by specialists in town.
The medical staff consists of 14 residents in internal medicine, most of whom have undergone more than 4 years of postgraduate clinical training, and three supervising attending physicians. A recent evaluation at our clinic set the duration of the first consultation at 35 minutes (range 20–75 minutes). This consultation usually consists of taking a careful patient history and a general physical examination.
Patients
All 1,032 new and consecutive general internal medicine outpatients were prospectively evaluated and screened for the study during the 3-month inclusion period from April through June 1992. Outpatients who were seen in subspecialty clinics were not evaluated for inclusion into the study. Of 1,032 patients, 190 fulfilled inclusion criteria; i.e., they had abdominal or chest pain as their main complaint or symptom. These 190 patients were included in the present study.
Preliminary Diagnosis (Initial Assessment)
For all patients, routine patient history and physical examination were performed by one of 14 residents according to standard protocol. When necessary, interpreters helped to obtain the history from patients speaking foreign languages. Patients were subsequently presented to an attending physician (A) who checked directly with patients when necessary to confirm elements of the history or physical examination. Attending physician A and resident together reached a preliminary diagnosis. The preliminary diagnosis was immediately recorded onto a standardized form and was rated as “undoubted” or “probable.” An “undoubted” preliminary diagnosis was based on characteristic and specific findings allowing a diagnosis with a very high level of confidence by the involved physicians. A preliminary diagnosis based on vague or nonspecific findings or a mere suspicion was called “probable.”
Workup
Further workup included routine laboratory testing and all measures deemed necessary to reach a diagnosis that might benefit the patient. Results of the individual diagnostic workup and immediate follow-up visits over a mean duration of 2 weeks were recorded. The most frequently performed investigations in patients with abdominal pain were stool culture for parasites or bacteria, abdominal ultrasound, gastroduodenal endoscopy, and colonic endoscopy. The most frequently performed investigations in patients with chest pain were chest radiography and treadmill ergometry. In addition to treadmill ergometry, myocardial perfusion scintigraphy was done particularly in patients with angina-like chest pain or cardiovascular risk factors.
Based on the diagnosis, reasons for abdominal or chest pain were classified as being of nonorganic versus organic causes. Nonorganic causes of abdominal pain were unspecific pain symptoms such as nonulcer dyspepsia and irritable bowel syndrome. Organic causes of abdominal pain were gastritis, peptic ulcer, parasitoses, enteritis, motility disorders due to alcohol consumption, cholelithiasis, cholecystitis, pancreatitis, and diverticulitis. Nonorganic causes of chest pain were unspecific chest pain symptoms and anxiety disorders. Organic causes of chest pain were coronary heart disease of any stage, pleuritis, tracheobronchitis, esophageal reflux, chest wall trauma, and tumors.
“Gold Standard” Diagnosis
A final diagnosis was established by the resident and attending physician A when patients were discharged from the care of the Medical Outpatient Clinic, i.e., after test results were entered into the chart and a diagnosis was made. Subsequently, all diagnoses were analyzed together by attending physician B and the resident. A second diagnosis was reached, however, because attending physician B was not blinded to the study aims or the preliminary diagnosis; subsequently, another independent attending physician (C), who was blinded to the aims of the study and the preliminary diagnosis, reviewed all charts and made the final diagnosis. The second and third “final” exact diagnoses were compared using the Kappa test.16 Thereafter, final diagnoses were reevaluated and classified as being either nonorganic or organic by consensus between attending physicians B and C. This final consensus decision served as the gold standard to assess sensitivity, specificity, accuracy, and the likelihood ratio of the preliminary diagnosis.
Follow-up of Patients with Nonorganic Causes of Pain at Final Diagnosis
Patients with nonorganic abdominal or chest pain were contacted after a mean of 29 months (range 18–56 months) after their first consultation to verify the diagnosis. Telephone interviews or, if necessary, ambulatory checkup examinations at our institution were executed. To reach as many patients as possible, telephone calls were repeated. When needed, specially trained interpreters helped to recruit as many patients as possible for follow-up. The patients were asked about new complaints, change of complaints, further investigations, intervening treatments, and hospitalizations during the follow-up observation period. In all cases with suspected new diagnoses, the responsible general practitioner was contacted to confirm or reject alternative diagnoses.
RESULTS
Patients
Of 1,032 consecutive new patients in the general Medical Outpatient Clinic screened for the study, 190 fulfilled the inclusion criteria; i.e., they had either abdominal pain (n = 112) or chest pain (n = 78) as their main complaint. The mean age was 44 years (SD = 14); 101 patients were male, and 89 were female.
Definition of the Gold Standard
Interobserver agreement between attending physicians B and C on the final diagnosis as well as separation into nonorganic or organic was excellent, with a κ = 0.95 in both instances. Subsequently, all 190 patients were classified by consensus by the two attending physicians B and C as having a nonorganic (n = 131) or organic (n = 59) final diagnosis.
Accuracy of Preliminary Diagnoses Based on History and Physical Examination Alone
We investigated whether a preliminary diagnosis of nonorganic versus organic cause of pain was reliable, i.e., whether it compared favorably with the diagnosis when the patient’s case was considered closed (see the gold standard above).
Abdominal Pain
Of the 112 patients with abdominal pain as their main complaint, 47 (41%) had upper abdominal pain, 30 (27%) had lower abdominal pain, and 35 (31%) had diffuse nonlocalized abdominal pain. The preliminary diagnosis was nonorganic for 51 patients and organic for 61 patients. After the final diagnosis, an organic cause was found in 46 (41%) of 112 patients (Table 1A). Gastritis (n = 9), peptic ulcer disease (n = 6), and amebiasis (n = 4) were the most frequent organic findings. Sixty-six (59%) of 112 patients were considered to have a nonorganic cause of their pain (Table 1A).
Table 1A.
Preliminary Diagnosis of Nonorganic Versus Organic Chest Pain Compared with Final Dignosis
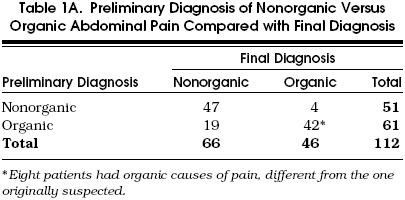
The actual preliminary diagnosis compared with the actual final diagnosis was not correct in 31 (28%) of 112 patients. As many as 19 of these 31 patients were ultimately diagnosed with a nonorganic cause of their pain; i.e., most erroneous judgments occurred in patients that were initially diagnosed as having a pain of organic origin and were ultimately classified as having a pain of nonorganic origin. In 8 other patients an organic cause other than the previously suspected one was discovered, e.g., a peptic ulcer instead of cholelithiasis. Only 4 patients had an organic final diagnosis when a pain of nonorganic origin had originally been supposed (one urinary infection, one appendicitis, one peptic ulcer, and one enteric amebiasis). In 2 of the patients with a wrong preliminary nonorganic diagnosis, the correct diagnosis was made within an hour after the preliminary diagnosis on the basis of routine laboratory testing (diagnosis of acute appendicitis after leukocyte count and abdominal ultrasound, urinary infection after urinalysis). In the remaining 2 patients, a correct diagnosis was made within 2 days; upper endoscopy led to the diagnosis of nonbleeding peptic ulcer, and positive stool tests to the diagnosis of amebiasis.
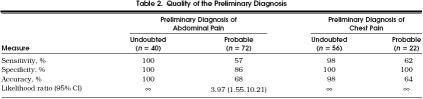
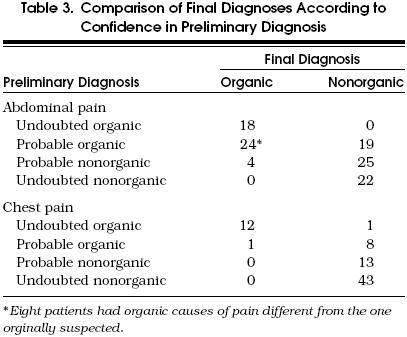
All 31 preliminary diagnoses that turned out to be wrong had been characterized as “probable” by the treating physicians. In other words, the confidence of the treating physicians in the reliability of their diagnosis was low. Consequently, further workup was solicited that resulted in the final, correct diagnosis in all of these cases. In 40 (38%) of 112 cases the preliminary diagnosis had been rated as “undoubted.” In these cases the diagnosis was always correct when compared with the final diagnosis (Table 2 and Table 3. Hence 81 (72%) of all 112 patients with abdominal pain had an exact final diagnosis correctly assessed on the basis of history and physical examination alone (Table 3). The corresponding sensitivity, specificity, and accuracy are excellent for an “undoubted” preliminary diagnosis and intermediate for a “probable” preliminary diagnosis (Table 2
Table 2.
Quality of the Preliminary Diagnosis
Table 3.
Comparison of Final Diagnoses According to Confidence in Preliminary Diagnosis
Chest Pain
Of 78 patients complaining mainly of chest pain, 65 (83%) had unspecific complaints of musculoskeletal origin or other symptoms that were classified as nonorganic in final diagnosis (Table 1B). In one third of these patients further investigations such as treadmill ergometry or chest radiography were used to exclude potential organic causes of chest pain. Only 13 patients with chest pain (17%) received a final diagnosis of organic disease (Table 1B): 4 patients (5%) had symptomatic coronary heart disease, and 9 (12%) had an other organic final diagnosis, most frequently pleuritis (n = 3), tracheobronchitis (n = 2), or esophageal reflux (n = 2).
Table 1B.
Preliminary Diagnosis of Nonorganic Versus Organic Chest Pain Compared with Final Dignosis
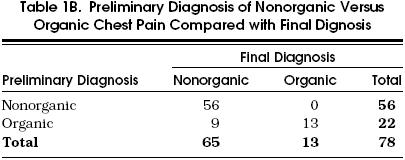
Of the 78 patients, 69 (88%) had a correct preliminary diagnosis on the basis of history and physical examination alone. In 55 (80%) of these patients, the preliminary diagnosis had been considered “undoubted,” and in 14 (20%) “probable.” Final diagnosis did not correspond to preliminary diagnosis in only 9 (12%) of the patients (Table 3). In 8 of these 9 patients, preliminary diagnosis was made with little confidence, analogous to the results in patients with abdominal pain. Thus, the preliminary diagnosis was rated as “probable” organic disorder, mostly angina pectoris, in these patients. These 8 patients received a final diagnosis of nonorganic chest pain. A single patient received an “undoubted” preliminary diagnosis of angina pectoris based on the patient’s history of myocardial infarction and a history of percutaneous transluminal coronary angioplasty (PTCA). However, thallium scintigraphy did not reveal any ischemia, which led to a final diagnosis of nonorganic cause of pain despite the patient’s history of coronary heart disease. Interestingly, this patient was later found to have coronary pain (successful PTCA, see below) in the follow-up investigation.
Thus, all nonorganic preliminary diagnoses were correct in 56 of 78 patients with chest pain (Tables 2 and Table 3). No organic cause of pain was missed. This means a specificity of nonorganic preliminary diagnosis of 100% (Table 2). Similar to abdominal pain, an exceedingly high specificity and sensitivity was reached when the treating physicians rated the cause of chest pain as “undoubted” organic or nonorganic (Table 2).
Follow-up Examination of Patients with Nonorganic Abdominal or Chest Pain
Missing an organic cause of pain that is not immediately apparent on standard workup might have dire consequences for a patient. It would therefore be of great advantage to know whether a first clinical judgment of a nonorganic cause of pain is reliable in the long term. To that end and to assess the final diagnosis serving as gold standard, we conducted a long-term follow-up of 131 patients with a nonorganic abdominal or chest pain at final diagnosis gold standard.
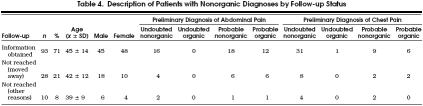
Thirty-eight patients (29%) could not be reached for follow-up investigation. Most of these predominantly young patients (e.g., students and expatriates) had moved away. Their diagnostic and demographic characteristics are given in Table 4. Of 131 patients, 93 (71%) could be reached for a follow-up examination after a mean of 29 months (range 18–56 months). Of these patients, 46 had nonorganic abdominal pain and 47 had nonorganic chest pain as their final diagnosis (Table 5 Patients had a telephone interview or checkup investigation at our institution. They were asked about new diagnoses and about the evolution of their pain symptoms.
Table 4.
Description of Patients with Nonorganic Diagnoses by Follow-up Status
Table 5.
Outcome at Long-Term Follow-up of 93 Patients with Nonorganic Abdominal or Chest Pain
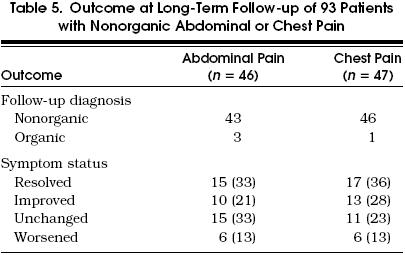
Nonorganic Abdominal Pain
Of the 46 patients that could be followed, pain had resolved completely in 15 (33%), improved in 10 (21%), remained unchanged in 15 (33%), and worsened in 6 (13%) (Table 5). In three patients who originally had a final diagnosis of nonorganic abdominal pain, the follow-up investigation revealed an organic diagnosis. Two patients had gastric ulcer, and one underwent surgery for diverticulosis of the colon. Thus, accuracy in patients diagnosed as having nonorganic abdominal pain at final diagnosis was 92% when compared with long-term follow-up.
Nonorganic Chest Pain
Of the 47 patients with chest pain that could be followed, pain had resolved completely in 17 (36%), improved in 13 (28%), remained unchanged in 11 (23%), and worsened in 6 (13%) (Table 5). The gold standard and diagnosis was correct in 98%. In one patient a final diagnosis of nonorganic chest pain had been made because of a negative result on thallium scintigraphy. A month later coronary heart disease was detected at coronary angiography, and PTCA abrogated the pain. Interestingly, the preliminary diagnosis was “undoubted” organic cause of pain.
DISCUSSION
Abdominal pain, chest pain, fatigue, back pain, headache, and dyspnea are the most frequent symptoms in medical outpatients.1 In the collective patients screened for our study, abdominal pain and chest pain were the most common complaints. This case mix of outpatients compares well with general internal practitioners in the local region,17 and other regions.1 In outpatients, 40% to 85% of complaints have no discernible organic cause; i.e., they are “nonorganic” in origin.1,3,18–21 It may be crucial to diagnose a nonorganic cause of pain early in order to prevent unnecessary workup and cost.1,13 It matters whether patients can be diagnosed reliably and early with a nonorganic cause of pain, although this may be more difficult than in pain of organic origin. To appraise whether a nonorganic diagnosis can be distinguished reliably from an organic one by clinical means alone, we prospectively studied 190 consecutive general medical outpatients with abdominal or chest pain.
A clinical judgment based on patient history and physical examination alone correctly predicted final diagnosis at completion of the chart in both abdominal (72%) and chest pain (88%). When a distinction between nonorganic and organic pain, but not a precise diagnosis, was made, accuracy increased to 79% for abdominal pain and remained at 88% for chest pain. These findings match other reports on the pivotal diagnostic contribution of careful history taking and physical examination alone in various patient populations.1,4–8,11–13,22
Medical practitioners often rely on experience and feelings that are described as “probable” or “undoubted.” Here we provide some evidence concerning the adequacy of such terms in the context of nonorganic versus organic abdominal and chest pain. The preliminary diagnosis was almost completely accurate when residents, together with their supervising attending physicians, felt very confident about their preliminary diagnosis. Accuracy of an “undoubted” preliminary diagnosis was 99% compared with the final diagnosis. Conversely, the accuracy of a “probable” preliminary diagnosis of abdominal pain and chest pain compared with the final diagnosis was only 68% and 64%, respectively.
One might argue that patients with an “undoubted” preliminary diagnosis only rarely had additional investigations to dispel their initial diagnosis. However, the follow-up investigation of patients with nonorganic final diagnosis after an average of 29 months (range 18–56 months) did not identify any erroneous judgment in the subset of patients with “undoubted” diagnoses. Diagnostic accuracy for both undoubted and probable nonorganic final diagnoses after completion of the chart (gold standard) in patients with abdominal and chest pain was 93% and 98%, respectively, as compared with the follow-up investigation. This is comparable to a report of 100 patients followed for nonorganic abdominal pain who were assessed with an equally high diagnostic accuracy of 95%.14
Our study did not aim to discern whether patient history or physical examination contributed more to diagnostic accuracy. However, patient history influences diagnostic evaluation more than physical examination does, the latter revealing crucial information in approximately 20% or less of all cases.7,11–13 Our follow-up investigation revealed an improvement of nonorganic abdominal pain in approximately 50% of the patients. Similarly, nonorganic abdominal pain,3 other gastrointestinal complaints,3 and miscellaneous symptoms1 improved in approximately half of all cases after a prolonged observation period. Nonorganic chest pain in our patients improved in 64%. Similar results were reported in patients with atypical chest pain and normal coronary arteries.15 The search for low-cost and high-quality care is ongoing. Patient wishes for interventions have to be considered.23 Yet our data, as well as others’ 24 suggest that lower cost is not necessarily associated with low quality of care. We conclude that only diagnoses of nonorganic pain that are rated as “probable” need further investigations and workup.
Our study has several limitations. First, our consecutive outpatients with abdominal or chest pain are better suited for the study of nonorganic causes of pain than organic ones. The number of our patients with organic diagnoses is relatively small, heterogeneous, and represents a limited number of diseases with a low number of cases in each category of disease. This, and the high prevalence of poorly circumscribed complaints of abdominal and chest pain in daily medical practice,1,8 led us to focus on the reliability of diagnoses for nonorganic causes of pain.
Second, each patient had his or her individual workup; e.g., investigations such as treadmill ergometry or endoscopy were performed only when clinically indicated. Individualization of workup has also been described in other similar studies that reflect conditions of daily medical practice.1,3 Third, a shortcoming of any investigation like ours is the lack of a totally reliable gold standard. In our study the final diagnosis served as a gold standard to measure the quality of the preliminary diagnosis. However, standardized and more aggressive investigations may have somewhat altered the final diagnosis. To assess the gold standard, we performed a follow-up investigation of nonorganic diagnosis. It was possible to reach 71% of the patients. It appeared that our gold standard was very good, 93% for abdominal pain and 98% for chest pain.
Fourth, screening for psychiatric conditions was not performed. A number of nonorganic diagnoses in our patients could have been better circumscribed and defined with questionnaires such as the PRIME–MD patient questionnaire.25 We did not strive to make a specific diagnosis in patients with pain of nonorganic origin. Yet, further psychological workup and care are clearly necessary in these patients.25
With these limitations in mind, our study still indicates that an “undoubted” preliminary nonorganic diagnosis is highly precise and reliable. The specificity of 100% shows that no organic diagnosis was missed. Thus, watchful waiting with little or no additional laboratory or other investigations is appropriate in these cases.
In conclusion, this study demonstrates that the first judgment of experienced physicians based on careful patient history and physical examination alone is reliable in medical outpatients with abdominal or chest pain. Reliability increases with the confidence with which the diagnosis can be made. In patients that have been confidently diagnosed with a nonorganic cause of pain, there does not seem to be a need for additional workup. Avoiding unnecessary workup may contribute to high-quality and low-cost ambulatory medicine. Further studies to evaluate the appropriate investigations are required in ambulatory care patients with nonorganic complaints.
Acknowledgements
The authors thank H.C. Bucher, MD, MPH, and M. Battegay, MD, for discussing and expertly reviewing the manuscript. Mrs. F. Vogel and S. Jaquemet are acknowledged for their outstanding secretarial assistance.
References
- 1.Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: incidence, evaluation, therapy and outcome. Am J Med. 1989;86:262–6. doi: 10.1016/0002-9343(89)90293-3. [DOI] [PubMed] [Google Scholar]
- 2.Martina B. Konsultationsgründe in der ambulanten allgemeinen inneren Medizin. Schweiz Rundsch Med Prax. 1994;83:1–2. [PubMed] [Google Scholar]
- 3.Bleijenberg G, Fennis JFM. Anamnestic and psychological features in diagnosis and prognosis of functional abdominal complaints: a prospective study. Gut. 1989;30:1076–81. doi: 10.1136/gut.30.8.1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kroenke K, Lucas CA, Rosenberg ML, et al. Causes of persistent dizziness. Ann Intern Med. 1992;117:898–904. doi: 10.7326/0003-4819-117-11-898. [DOI] [PubMed] [Google Scholar]
- 5.Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA. 1992;268:760–5. [PubMed] [Google Scholar]
- 6.Schmitt BP, Kushner MS, Wiener SL. The diagnostic usefulness of the history of the patient with dyspnea. J Gen Intern Med. 1986;1:386–93. doi: 10.1007/BF02596424. [DOI] [PubMed] [Google Scholar]
- 7.Hampton JR, Harrison MDG, Mitchell JRA, Prichard JS, Seymour C. Relative contributions of history-taking, physical examination and laboratory investigation to diagnosis and management of medical outpatients. BMJ. 1975;2:486–9. doi: 10.1136/bmj.2.5969.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kroenke K, Arrington ME, Mangelsdorff AD. The prevalence of symptoms in medical outpatients and the adequacy of therapy. Arch Intern Med. 1990;150:1685–9. doi: 10.1001/archinte.150.8.1685. [DOI] [PubMed] [Google Scholar]
- 9.Komaroff AL. Minor illness symptoms. Arch Intern Med. 1990;150:1586–7. doi: 10.1001/archinte.150.8.1586. [DOI] [PubMed] [Google Scholar]
- 10.Katon W, Kleinman A, Rosen G. Depression and somatization—a review. Am J Med. 1982;72:127–35, 241–7. doi: 10.1016/0002-9343(82)90816-6. [DOI] [PubMed] [Google Scholar]
- 11.Rich EC, Crowson TW, Harris IB. The diagnostic value of the medical history. Arch Intern Med. 1987;147:1957–68. [PubMed] [Google Scholar]
- 12.Peterson MC, Holbrook JH, Von Hales DE, Smith NL, Staker LV. Contributions of the history, physical examination and laboratory examination in making medical diagnoses. West J Med. 1992;156:163–5. [PMC free article] [PubMed] [Google Scholar]
- 13.Sandler G. The importance of the history in the medical clinic and the cost of unnecessary tests. Am Heart J. 1980;100:928–31. doi: 10.1016/0002-8703(80)90076-9. [DOI] [PubMed] [Google Scholar]
- 14.Svendsen JH, Munck LK, Andersen JR. Irritable bowel syndrome—prognosis and diagnostic safety. Scand J Gastroenterol. 1985;130:1171–3. doi: 10.3109/00365528509089673. A 5-year follow-up study. [DOI] [PubMed] [Google Scholar]
- 15.Lantiga LJ, Spranfkin RP, McCroskery JH, Baker MT, Warner RA, Hill NE. One-year psychosocial follow-up of patients with chest pain and angiographically normal coronary arteries. Am J Cardiol. 1988;62:209–13. doi: 10.1016/0002-9149(88)90213-5. [DOI] [PubMed] [Google Scholar]
- 16.Holman CDJ. Analysis of interobserver variation on a programmable calculator. Am J Epidemiol. 1984;120:154–60. doi: 10.1093/oxfordjournals.aje.a113864. [DOI] [PubMed] [Google Scholar]
- 17.Koechlin PH, Kulstrunk M, Dubach UC. Vermittelt das Ambulatorium einer Medizinischen Universitäts-Poliklinik genügend praxisbezogene Weiterbildung? Schweiz Aerztezeitung. 1991;72:206–9. [Google Scholar]
- 18.Frymoyer JW. Back pain and sciatica. N Engl J Med. 1988;318:291–300. doi: 10.1056/NEJM198802043180506. [DOI] [PubMed] [Google Scholar]
- 19.Woodhouse CRJ, Brockner S. Chronic abdominal pain: a surgical or psychiatric symptom? Br J Surg. 1979;66:348–9. doi: 10.1002/bjs.1800660515. [DOI] [PubMed] [Google Scholar]
- 20.Manning AP, Thompson WG, Heaton KW, Morris AF. Towards positive diagnosis of the irritable bowel. BMJ. 1978;2:653–4. doi: 10.1136/bmj.2.6138.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Conen D, Frey D. Colon irritabile—ja oder nein? Ist die Anamnese eine Entscheidungshilfe? Schweiz Med Wochenschr. 1982;112:531–4. [PubMed] [Google Scholar]
- 22.Kapoor WN. Diagnostic evaluation of syncope. Am J Med. 1991;90:91–106. doi: 10.1016/0002-9343(91)90511-u. [DOI] [PubMed] [Google Scholar]
- 23.Emanuel L. The search for low-cost-high quality care. J Gen Intern Med. 1995;10:232–3. doi: 10.1007/BF02600261. [DOI] [PubMed] [Google Scholar]
- 24.Starfield B, Power N, Weiner JR, et al. Costs vs quality in different types of primary care settings. JAMA. 1994;24:1903–8. [PubMed] [Google Scholar]
- 25.Kroenke K, Spitzer RL, Williams JBW, et al. Physical symptoms in primary care. Arch Fam Med. 1994;3:774–9. doi: 10.1001/archfami.3.9.774. [DOI] [PubMed] [Google Scholar]