Abstract
OBJECTIVE
To isolate the effect of spoken language from financial barriers to care, we examined the relation of language to use of preventive services in a system with universal access.
DESIGN
Cross-sectional survey.
SETTING
Household population of women living in Ontario, Canada, in 1990.
PARTICIPANTS
Subjects were 22,448 women completing the 1990 Ontario Health Survey, a population-based random sample of households.
MEASUREMENTS AND MAIN RESULTS
We defined language as the language spoken in the home and assessed self-reported receipt of breast examination, mammogram and Pap testing. We used logistic regression to calculate odds ratios for each service adjusting for potential sources of confounding: socioeconomic characteristics, contact with the health care system, and measures reflecting culture. Ten percent of the women spoke a non-English language at home (4% French, 6% other). After adjustment, compared with English speakers, French-speaking women were significantly less likely to receive breast exams or mammography, and other language speakers were less likely to receive Pap testing.
CONCLUSIONS
Women whose main spoken language was not English were less likely to receive important preventive services. Improving communication with patients with limited English may enhance participation in screening programs.
Keywords: language, preventive health services, accessibility of health services, communication barriers
As ethnic minority populations grow in developed countries, language may become an increasingly important barrier to health care. Because effective communication is fundamental to the practice of medicine, language differences may have an important impact on patients and providers. The extent to which language affects care, however, is not well known. In English-speaking countries, the data available are limited mostly to comparisons between English and Spanish speakers and suggest that those not speaking English are less likely to have a regular source of care,1 receive fewer eye, dental, or physical examinations,2 and have children with worse reported health status.3
Disentangling the effects of language on medical care from other correlated factors is difficult because language may act in a number of different ways. First, for persons with limited English, language may represent a communication barrier. They may not be able to communicate to the provider that they desire screening, or providers may not be able to discuss or offer screening in an effective way. Second, language may also be a proxy for issues that can affect access to care. For example, in the United States, limited English proficiency is associated with socioeconomic factors known to be related to decreased utilization of care (e.g., lower income, lower educational attainment, and lack of insurance).4–7 Finally, language is closely related to culture (e.g., one’s language denotes functional membership in a particular cultural group).8,9 To the extent that norms vary across cultures, language differences may signal differences in values about health behaviors or use of health care.
In an attempt to understand how one’s spoken language relates to receipt of health care, we used data from the 1990 Ontario Health Survey. We studied use of three preventive services that are widely agreed to be of value to the general population (breast examination, mammography, and Pap test).10,11 The Ontario Health Survey collected detailed sociocultural information including spoken language in a sample of persons representing the entire province, as well as self-reported utilization of health services. Thus, the data allowed us to adjust for socioeconomic factors, contact with the health care system, and measures reflecting culture (ethnicity and immigration status) while assessing use of preventive services across language groups. A key advantage to studying these issues in Canada is the presence of universal and comprehensive insurance coverage for all residents. Thus, insurance cannot confound our analyses.
METHODS
Data Source
The data are from the 1990 Ontario Health Survey, a population-based, multistage random sample of 35,000 households (61,239 persons) in Ontario, a primarily English-speaking province in Canada. The Ontario Health Survey measured demographic, health, and behavioral information on a sample of persons representing the entire household population of Ontario.
Data were collected through in-person interviews with a representative household member in either English or French, and with self-completed questionnaires for all household members over 12 years of age (available in five languages: English, French, Italian, Portuguese, and Chinese). The response rate to the interview was 88%; 2.4% of the eligible sample did not respond because of communication problems including a language barrier. Thus, households otherwise eligible to participate in the survey were excluded if no one spoke either English or French. The response rate to the questionnaire was 77%. The following analyses are based on data from the questionnaires.
Subjects
The study population consisted of the 22,448 women aged 18 to 74 years who completed the 1990 Ontario Health Survey questionnaire with complete information on main language and ethnicity. To conform to the recommendations of the Canadian Task Force on Periodic Health Examinations, women aged 18 years and older were included in our analyses for Pap test, and women aged 50 years and older for breast examination and mammography.10
Measures
Dependent Variables.
The dependent variables were self-reported utilization of three preventive services on the Ontario Health Survey questionnaire: breast examination in the past year and mammogram and Pap test in the past 2 years.
Independent Variable.
Main language was assessed by the single-item question, “What is the language spoken most often at home,” with response options including 14 languages and “other” language. As Canada is officially bilingual, we divided main language into majority languages, English and French, and all other languages (“other”). The most common “other” languages were Italian, Portuguese, Polish, German, Chinese, Spanish, and Greek.
Control Variables.
Because we wanted to control for characteristics known to be related to the utilization of preventive services, we measured variables in three categories: socioeconomic characteristics, contact with the health care system, and measures reflecting culture.
Sociodemographic information. Sociodemographic variables were included in these analyses as the variables of age (continuous variable), education (some high school, high school graduate, some college, college graduate), family income (measured in categories of Canadian dollars, ≤C$20,000, C$20,000–C$80,000, ≥C$80,000), and family size (1–2, 3–4,> 4). The Papanicolaou model also included sexual activity (reporting a sexual partner within the past year), a known correlate of Pap test use.
Contact with the health care system . The number of doctor visits in the past year was assessed and used as a measure of contact with the health care system. Because visits were not normally distributed (i.e., right skewed), we created two multivariable models, one specifying visits as a continuous variable and the other using visit categories (e.g., 0, 1–4, 5–8,> 8 visits in the past year). Both models yielded almost identical results, and we report the results of the model using visits as a continuous measure.
Measures ref lecting culture. We used ethnic self-identification and immigration status as measures reflecting culture. Reflecting the complexity of ethnic identification, the survey asked respondents their self-reported ethnicity with 19 possible response categories. We categorized ethnicity as Canadian, mixed Canadian (Canadian and a second ethnicity), Western European, Eastern European, Asian, Native American, and other. In addition, subjects were characterized as Canadian-born, long-term immigrant (more than 5 years in Canada), or recent immigrant (5 years or less in Canada). A small proportion of recent immigrants lived in Canada for less than 2 years. Because the outcome of interest was use of preventive services in the past 1 or 2 years, we performed our analyses both on the complete sample and on a restricted sample limited to persons living in Canada for at least 2 years. As the results were almost identical, we report on the analyses for the complete sample.
Analysis
We calculated crude rates of breast examination, mammogram, and Pap test for the three language groups. We used multiple logistic regression to calculate the odds ratio (OR) for use of each of the preventive services by each language group relative to English speakers, using the control variables described above. We found no important second-order interactions and therefore report only main effects.
To account for the sampling design used in the survey, all analyses used analytic weights that account for the probability of selection into the sample, and we used a jackknife repeated replication technique in the calculation of standard errors.12 All models exhibited adequate fit as assessed by the Hosmer-Lemeshow test on unweighted regression models. All analyses were done using STATA (College Station, Tex.).
RESULTS
Characteristics of Language Groups
About 10% of the sample identified a main language other than English: 4% (997) French and 6% (1,377) other. Table 1 shows the demographic characteristics of the main language groups. Compared with English speakers, the French group and other language group reported slightly lower income and were less likely to have completed a high school education. The other language speakers also had the largest family size. Finally, contact with the health care system did not vary importantly across language groups.
Table 1.
Characteristics of Main Language Groups
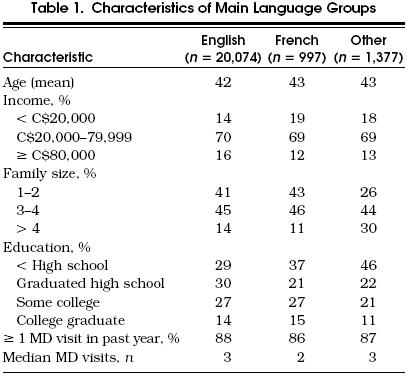
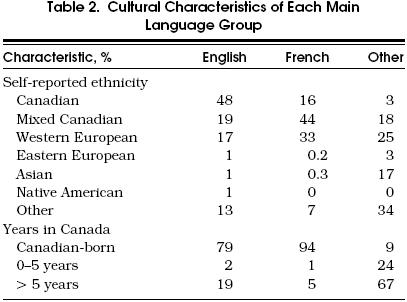
Table 2 shows the relation between main language and the other measures reflecting culture and highlights the fact that language and self-reported ethnicity do not measure the same thing: 33% of English speakers, and 40% of French speakers did not identify themselves as Canadian; conversely, 21% of other language speakers called themselves Canadian even though their main language at home was neither English nor French, the official Canadian languages. As expected, both English and French speakers were predominantly Canadian-born, while most of the other language speakers were immigrants—67% recent (within 5 years) and 24% long-term (immigrated more than 5 years ago).
Table 2.
Cultural Characteristics of Each Main Language Group
Main Language and Use of Preventive Services
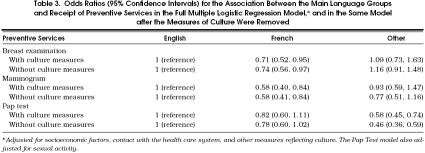
In the unadjusted analysis, use of all three preventive services varied across language groups; in each case, English speakers were most likely to report receipt of the service (Fig. 1). We used multiple logistic regression to examine the association between the use of each preventive service with language using three categories of control variables: socioeconomic factors, contact with the health care system, and measures reflecting culture (Table 3). In the full model, language was significantly related to less receipt of breast examination (OR 0.71; 95% confidence interval [CI] 0.52, 0.95) and mammography (OR 0.58; 95% CI 0.40, 0.84) for French speakers, and to less receipt of Pap testing (OR 0.58; 95% CI 0.45, 0.74) for other language speakers. There was a trend toward less receipt of Pap testing for French speakers. Finally, there was no statistical association between language and receipt of either breast examination or mammogram for the other language speakers. The results of the full model are displayed graphically in Figure 2.
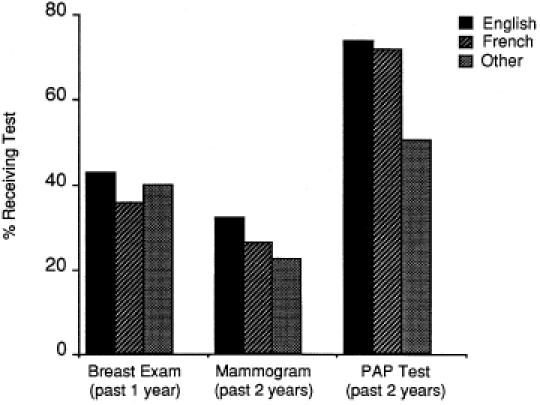
Proportion of each main language group receiving breast examination, mammogram, and Pap test.
Table 3.
Odds Ratios (95% Confidence Intervals) for the Association Between the Main Language Groups and Receipt of Preventive Services in the Full Multiple Logistic Regression Model,* and in the Same Model after the Measures of Culture Were Removed
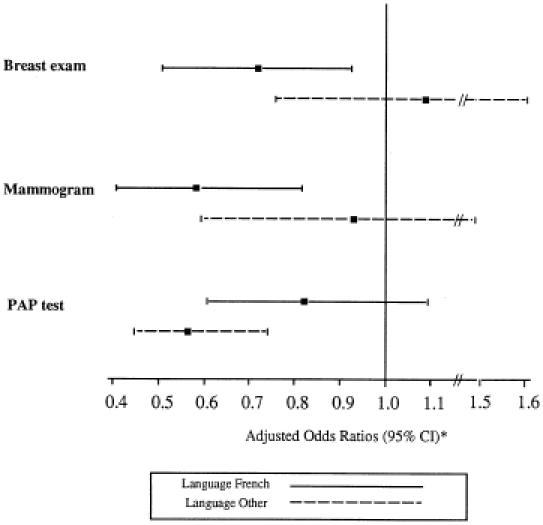
Odds ratios (95% confidence intervals) in the full model for breast examination, mammogram, and Pap test. The Pap Test model also adjusted for sexual activity. *Odds ratio adjusted for socioeconomic factors, contact with the health care system, and other measures reflecting culture.
Table 3 shows how ethnic self-report and immigration status affected the association between language and use of preventive services. For French speakers, ORs for receipt of each of the preventive services were essentially unchanged with the addition of the culture measures to the model. For the other language speakers, however, addition of the culture measures to the model had more of an effect, in each case weakening the association between language and receipt of the service. The largest effect was found in the mammogram model with a change of OR from 0.77 to 0.93 when the measures of culture were added to the model. These findings highlight the fact that both language and other cultural factors affected the receipt of preventive services by members of the other language group.
Finally, we considered whether the measures reflecting culture were themselves related to use of preventive services. Asian ethnicity was the only ethnicity independently related to use of any service (data not shown). In the full model, Asians, compared with those identifying themselves as Canadian, had lower odds of receiving mammography (OR 0.25; 95% CI 0.07, 1.00) and lower odds of receiving Pap testing (OR 0.59; 95% CI 0.40, 0.88). Also in the full model, years in Canada was independently significant only for Pap testing: compared with Canadian-born women, recent immigrants (i.e., in Canada less than 5 years) were less likely to have had a Pap test (OR 0.39; 95% CI 0.22, 0.68).
DISCUSSION
In 1990 more than 10% of women in Ontario spoke a language other than English at home. Our study demonstrates that these women were less likely to receive important preventive services than women who spoke English at home.
Use of a language other than English may be related to the receipt of preventive services in four ways: (1) as a proxy for insurance status1 or for low socioeconomic status,5 a factor known to be related to less use of screening 6,7 even in the Canadian system13; (2) as a barrier to contact with the health care system; (3) as a marker for culture differences about the value of screening; or (4) as a communication barrier.
In this study we attempted to isolate the communication aspect of language by adjusting for characteristics reflecting the first three possibilities. In our sample, English speakers had higher income and educational attainment, attributes that, consistent with previous work,5 were associated with increased use of preventive services. However, in our analysis, socioeconomic characteristics did not explain the association between language and use of preventive services. No relation was observed between language and contact with the health care system. Physician contact was high, most likely reflecting Canada’s policy of universal insurance. Thus, although doctor visits were independently related to receipt of preventive services, it is not surprising that controlling for physician visits did not change the effect of language. Finally, although language was related to both self-reported ethnicity and years in Canada, an important independent relation between language and use of preventive services persisted even after adding measures of cultural identification to the model.
The persistent association of language with the preventive services after adjusting for the aforementioned characteristics suggests that the language effect is attributable to a communication barrier. Although there is evidence that beliefs specific to certain ethnic groups (e.g., fatalismo among certain Hispanic groups14) may affect how health care is utilized, communication about the benefits or importance of screening has also been shown to be strongly related to patient compliance with screening recommendations.15,16 In the one study examining cervical cancer screening among Hispanics, most of the reasons cited for noncompliance with Pap testing related to poor provider communication.15 Similarly, Fox and Stein found that the strongest predictor of mammogram use was whether or not the doctor discussed mammography with the patient.17 Spanish-speaking women were significantly less likely to report that the doctor had discussed mammography.
Several aspects of our study merit comment. First, it is reasonable to question the validity of the variables used to measure culture. Self-reported ethnicity and immigration status are only proxies for cultural identification, and failure to adequately measure culture may limit our findings. It could be argued, for example, that language is a more powerful marker of cultural differences than either ethnic identification or immigration status, and that our results simply reflect greater accuracy in identifying the most “culturally” different women in Ontario (i.e., the least acculturated). Such an argument assumes that “less acculturated” uniformly means less interest in prevention. We are unaware of any empirical data to support this assumption. To the contrary, Fox and Stein found that regardless of spoken language, women were equally interested in mammography once the provider discussed the issue.17 It seems more likely that language measures what it implies—communication. Further research is needed, however, to understand when differences in health behaviors are informed (i.e., reflect real differences in values) or are the result of ineffective communication.
Next, we have no information about the extent to which patients and providers shared a common language. Ontario is a predominantly English-speaking province, and most doctors are primary English speakers. If patients and providers are sufficiently fluent in a common language, then language will not be a barrier to communication. Patients, however, may be fluent in English, despite speaking another language at home—or, some doctors may be fluent in languages other than English. Finally, the Ontario Health Survey excluded fully non-English-speaking or non-French-speaking households. About 2.4% of eligible households were excluded on the basis of a language barrier. The excluded households represent the most linguistically isolated persons, a group that is most likely to suffer the consequences of language barriers. Both the extent to which patients and providers shared a common language (i.e., unmeasured language concordance) and the exclusion of the most linguistically isolated persons would tend to minimize differences between language groups—the observed effect would underestimate the true effect.
In conclusion, women in this study who spoke a language other than English at home were less likely to receive important preventive services. The effect of language persisted after adjusting for variables reflecting socioeconomic factors, contact with the health care system, and culture, suggesting that observed differences across language groups may be attributable to a communication barrier. Improving communication with such patients may enhance participation in preventive health programs. Because most other health care involves issues at least as complex, they too are likely to be susceptible to the effects of communication barriers.
Our data suggest that those who live in developed, English-speaking countries, and who speak a language other than English at home may not receive the same level of care as persons speaking English. As ethnic minority populations grow in these countries, the number of persons with limited English will expand. In the United States, 32 million people speak a language other than English at home.18 Although communication barriers are remediable,19 solutions such as effective interpreter services may be costly. Recent work suggests that simply providing untrained interpreters may do little to improve communication.20 Making rational decisions about how to improve services to minority-language speakers will require understanding the public health costs of communication barriers.
REFERENCES
- 1.Hu DJ, Covell RM. Health care usage by Hispanic outpatients as a function of primary language. West J Med. 1986;144:490–3. [PMC free article] [PubMed] [Google Scholar]
- 2.Solis J, Marks G, Garcia M, Shelton D. Acculturation, access to care, and use of preventive services by Hispanics: findings from HHANES 1982–84. Am J Public Health. 1990;80(8):11–9. doi: 10.2105/ajph.80.suppl.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirkman-Liff B, Mondragon D. Language of interview: relevance for research of Southwest Hispanics. Am J Public Health. 1991;81:1399–404. doi: 10.2105/ajph.81.11.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feinstein J. The relationship between socioeconomic status and health: a review of the literature. Milbank Q. 1993;71:279–322. [PubMed] [Google Scholar]
- 5.Stein J, Fox S. Language preference as an indicator of mammography use among Hispanic women. J Natl Cancer Inst. 1990;82:1715–6. doi: 10.1093/jnci/82.21.1715. [DOI] [PubMed] [Google Scholar]
- 6.Makuc D, Fried V, Kleinman J. National trends in the use of preventive health care by women. Am J Public Health. 1989;79:21–6. doi: 10.2105/ajph.79.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hayward R, Shapiro M, Freeman H, Corey C. Who gets screened for cervical and breast cancer? Arch Intern Med. 1988;148:1177–81. [PubMed] [Google Scholar]
- 8.Marks G, Solis J, Richardson J, Collins L, Birba L, Hisserich J. Health behavior of elderly Hispanic women: does cultural assimilation make a difference? Am J Public Health. 1987;77:1315–9. doi: 10.2105/ajph.77.10.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deyo R, Diehl A, Hazuda H, Stern M. A simple language-based acculturation scale for Mexican-Americans: validation and application to health care research. Am J Public Health. 1985;75:51–5. doi: 10.2105/ajph.75.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Canadian Guide to Clinical Preventive Health Care. Ottawa, Ont: Canada Communication Group; 1994. Canadian Task Force on the Periodic Health Examination. [Google Scholar]
- 11.Guide to Clinical Preventive Services. 2nd ed. Baltimore, Md: Williams & Wilkins; 1996. United States Preventive Services Task Force. [Google Scholar]
- 12.Rust K. Variance estimations for complex estimators in sample surveys. J Off Stat. 1985;4:381–97. [Google Scholar]
- 13.Katz S, Hofer T. Socioeconomic disparities in preventive care persist despite universal coverage: breast and cervical cancer screening in Ontario and the United States. JAMA. 1994;272:530–4. [PubMed] [Google Scholar]
- 14.Perez-Stable E, Sabogal F, Otero-Sabogal R, Hiatt R, McPhee S. Misconceptions about cancer among Latinos and Anglos. JAMA. 1992;268:3219–23. doi: 10.1001/jama.1992.03490220063029. [DOI] [PubMed] [Google Scholar]
- 15.Harlan L, Bernstein A, Kessler L. Cervical cancer screening: who is not screened and why? Am J Public Health. 1991;81:885–91. doi: 10.2105/ajph.81.7.885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kottke T, Trapp M, Fores M, et al. Cancer screening behaviors and attitudes of women in southeastern Minnesota. JAMA. 1995;273:1099–1105. [PubMed] [Google Scholar]
- 17.Fox SA, Stein JA. The effect of physician-patient communication on mammography utilization by different ethnic groups. Med Care. 1991;29:1065–82. doi: 10.1097/00005650-199111000-00001. [DOI] [PubMed] [Google Scholar]
- 18.113th ed. Washington, DC: US Bureau of the Census; 1993. Statistical Abstract of the U.S. 1990 Census. [Google Scholar]
- 19.Woloshin S, Bickell N, Schwartz L, Gany F, Welch H. Language barriers in medicine in the United States. JAMA. 1995;273:724–8. [PubMed] [Google Scholar]
- 20.Baker D, Parker R, Williams M, Coates W, Pitkin K. Use and effectiveness of interpreters in an emergency department. JAMA. 1996;275:783–8. [PubMed] [Google Scholar]