Abstract
OBJECTIVE
To determine whether a computer-assisted reminder would alter prescribing habits for the treatment of hypertension in accordance with current clinical guidelines in a general internal medicine clinic.
DESIGN
A randomized trial.
SETTING
The General Internal Medicine Clinic of the Veterans Affairs Puget Sound Health Care System, Seattle Division.
PATIENTS/PARTICIPANTS
Clinic providers were randomized to a control group (n= 35) or intervention group (n= 36). We targeted the providers of patients being treated for hypertension with calcium channel blockers, a class of drug not recommended for initial therapy.
INTERVENTION
An automated computer query identified eligible patients and their providers. A guideline reminder was placed in the charts of patients of intervention providers; the charts of patients of control providers received no reminder.
MEASUREMENTS AND MAIN RESULTS
During the 5-month study period, 346 patients were seen by the 36 primary care providers (staff physicians, nurse practitioners, residents, and fellows) in the intervention group, and 373 patients were seen by the 35 providers in the control group. Intervention providers changed 39 patients (11.3%) to other medications during the study period, compared with 1 patient (<1.0%) of control providers ( p < .0001). For patients whose therapy was unchanged, providers noted angina in 23.1%, indications other than those for hypertension in 9.5%, intolerable adverse effects with first-line therapy in 13.9%, and inadequate control with first-line therapy in 13.9%. Of those patients without provider-indicated contraindications, 23.6% were switched from calcium channel blockers to first-line agents during the intervention period.
CONCLUSIONS
The use of a computerized, clinic-based intervention increased compliance with guidelines in the treatment of primary hypertension in general, and decreased the use of calcium channel blockers for the treatment of hypertension in particular.
Keywords: guidelines, physician's practice patterns, hypertension, calcium channel blockers
Drug prescribing is a major part of the practice of medicine, yet few randomized, controlled trials examining the effects of interventions have been aimed at improving physician drug-prescribing habits in the primary care setting. Trials have failed to show an impact of printed materials and guidelines alone.1–4 Educational outreach, in the form of face-to-face training, often referred to as “academic detailing,” has been shown to be effective in changing drug-prescribing habits, but suffers from an effect decay over time and a relatively high cost due to time and labor requirements.1,2 Several studies have demonstrated that individualized, computer-generated feedback can influence prescribing patterns.5–7 Generating individual feedback can be time-intensive, thereby limiting practical application. Integrated hospital data management systems make it possible to automate some individualized feedback, with minimal cost and time requirements beyond the establishment of the program.
The Fifth Report of the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure (JNC V) has recommended β blockers and diuretics as first-line therapy in the treatment of uncomplicated hypertension, on the basis of evidence that these drugs can reduce morbidity and mortality.8 More than 80% of patients with essential hypertension can be treated effectively with β blockers, diuretics, or a combination of the two.9 Despite recommendations that they be used only in special clinical circumstances, calcium channel blockers (CCBs) are widely used as first-line therapy for the treatment of essential hypertension. Between 1982 and 1993, the percentage of hypertensive patients treated with CCBs increased from 0.3% to 27%.10 Unlike β blockers and diuretics, there is no evidence that CCBs decrease the mortality or morbidity of hypertension-related disease. There are epidemiologic data,11,12 and some prospective data,13 to suggest that some types of CCBs may increase cardiovascular risk in some populations. An intervention designed to increase the use of first line agents, while decreasing the use of CCBs, would result in neutral or improved clinical outcomes, potentially at a lower cost.
Because of concern about the growing usage of CCBs at our institution, we sought to develop a mechanism to encourage primary care providers in our outpatient clinics to prescribe β blockers and diuretics for the treatment of hypertension. We conducted a randomized, controlled trial to test the hypothesis that a guideline reminder, added to the patient chart at the time of the clinic visit, targeted using an automated computer program, could influence provider prescribing toward recommendations by the JNC V.
METHODS
Study Subjects
The trial was conducted at the General Internal Medicine Clinic of the Veterans Affairs (VA) Puget Sound Health Care System, Seattle (Wash.) Division, between March and August 1996. The study subjects were all of the 71 full-time and part-time primary care providers, i.e., staff physicians, nurse practitioners, fellows, and residents, who saw patients in the clinic during the 6-month study period. Approximately 5,500 patients were enrolled in the clinic at the time of the study, and more than 20,000 visits were made to the clinic in 1995. In 1995, staff physicians provided 43% of all nonpsychiatric visits; residents and fellows, 41%; and nurse practitioners, 16%.
Study Design
A randomized, controlled design was used. A random number generator was used to randomize providers to either the intervention or the control group, stratified according to whether they were staff physicians, nurse practitioners, or residents or fellows. Providers were assigned numeric codes; study investigators were blinded to the coding identifiers.
Data Collection
The Seattle VA Medical Center maintains comprehensive patient information on a mainframe computer system called the Decentralized Hospital Computer Program (DHCP). Information on patient demographics, comorbidity as assessed by inpatient ICD-9 codes and outpatient diagnosis codes, visit dates, medication profile, and laboratory utilization was obtained from this database. A separate database maintaining pilot data for another ongoing study, the Ambulatory Care Quality Improvement Project (ACQUIP),14 was used to follow blood pressure (BP) and weight. Demographic and practice information on providers was obtained from the hospital Medical Staff Office.
Intervention
The intervention was designed to act at the point of patient contact during the clinic visit. It was targeted at the providers for patients receiving CCBs for hypertension. These patients were identified using a DHCP-based computer program that identified all patients being seen in the General Internal Medicine Clinic on the designated study day who had a prescription for a CCB written or refilled in the past 26 weeks, without having a nitrate prescription written or refilled during the same period. Nitrates were used as a proxy for active ischemic heart disease; eliminating all patients concurrently treated with nitrates and CCBs was expected to eliminate most patients receiving CCBs for angina. Because the pharmacy database records only prescriptions and refills, and cannot guarantee that medications listed are being taken as prescribed, we identified patients with prescriptions filled within 26 weeks of the visit data.
For each clinic visit, for each eligible patient, providers in the intervention group had a 1-page guideline reminder (Appendix A) placed in the patient chart by the clinic pharmacist, attached to the medication refill forms that are given to providers at every patient visit. Providers in the control group received no reminder. The reminder highlighted the prescription and offered alternative drugs and doses. For continued CCB use, the reminder also asked the provider to designate one of four indications: prescription for a diagnosis other than hypertension, concurrent angina and hypertension, failure of other medications to control hypertension, or adverse effects from other medications for hypertension. The reminder was collected by the ward clerk when the patient checked out of clinic, and returned to the study investigators. Response rate by visit for the completion and return of the guideline reminder was 72%, ranging from a return rate of 61% for nurse practitioners to 80% for staff physicians.
Drug changes were recorded for the intervention group when the provider indicated a change on the returned guideline reminder. The pharmacy computer database was reviewed for every patient seen in both the intervention and control groups during the study period. Charts were reviewed for all patients with a drug change to confirm provider intent and medication changes.
The intervention was conducted between March and August 1996. Follow-up to test for persistence of changes was continued through February 1997. The project was approved by the University of Washington Human Subjects Review Committee.
Statistical Analysis
The unit of analysis was the individual provider. Analysis was performed using SPSS for Windows, version 6.0. Continuous variables were analyzed using Student's t test. Because of unequal variances due to different numbers of observations per subject, a randomization test was used to test for significance in rates of change,15 with results reported for p values <.05. Randomization testing, also called permutation testing, is used to test the generic null hypothesis that one variable (randomization group) is unrelated to another (therapy changes). Significance is assessed by shuffling one variable relative to the other. If the variables are related, then the value of the original test statistic of unshuffled data should be extreme relative to the values obtained from shuffling. In this case, the observed statistic was more extreme than any of the 5,000 random samples generated from the data.
Further testing was done weighting by the number of patients seen per provider; none of these tests changed the significance of the results. The results of randomization testing did not differ from independent sample t tests (percentage of patients with therapy changed) or Pearson's χ2 testing (therapy change vs no therapy change).
RESULTS
Study Population at Baseline
The baseline characteristics of providers in the control and intervention groups were not substantially different (Table 1). The majority were board-certified internists or residents or fellows in internal medicine, with fewer nurse practitioners.
Table 1.
Baseline Characteristics
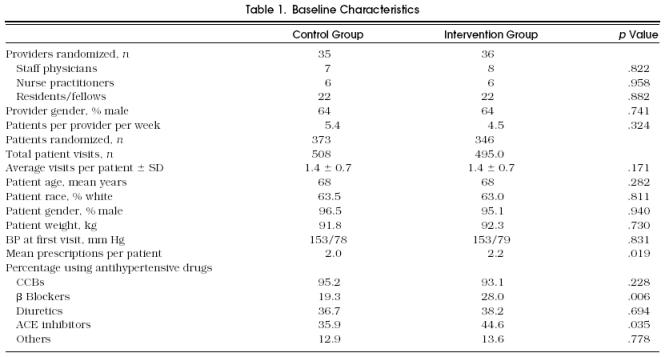
Control and intervention patients were similar in age, gender, and initial BP. Consistent with other VA populations, the patient population for this study consisted primarily of elderly males of European descent, with fewer males of non-European descent and even fewer female patients of all races.
At the initiation of the study, more patients in the intervention group than patients in the control group were receiving a β blocker or an angiotensin-converting enzyme (ACE) inhibitor. Approximately 5% of patients in both groups had past, but not active, prescriptions for CCBs. Control and intervention groups had no significant difference in the type of CCB prescribed at the initiation of the study (Table 2). Outpatient diagnostic codes, available for 87% of patients, showed no significant differences between the control and intervention groups (Figure 1).
Table 2.
Distribution of Calcium Channel Blocker Prescriptions
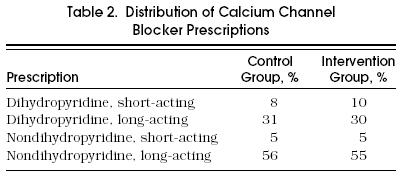
Figure 1.

Outpatient diagnostic codes for intervention and control groups.
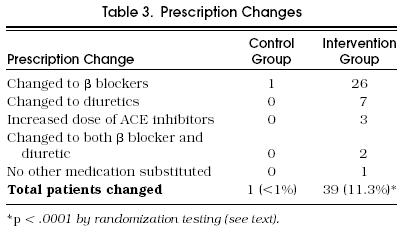
Prescription Changes
Thirty-nine of 346 patients were changed from CCBs to other antihypertensive medications (Table 3). For another 6 patients, providers indicated that changes to medications had been made, but no change could be documented by review of either pharmacy records or patient charts. In 5 patients the change in therapy was later reversed: 2 had inadequate BP control, 1 was changed by the primary provider but had CCBs renewed during an emergency department visit; 1 was changed by the primary provider but had a CCB added by a neurology consultant, and 1 had increasing dyspnea on exertion.
Table 3.
Prescription Changes
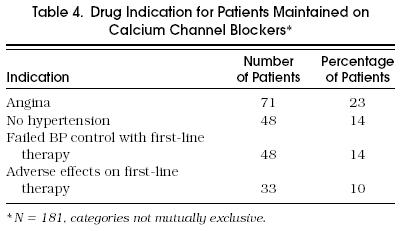
Data on drug indications were available for 181 of 307 patients maintained on CCBs (Table 4). Of the patients not changed, 23% listed that CCBs were prescribed for angina, 48 (14%) indicated that the patient had failed β blockers or diuretics, 48 (14%) indicated that the patient had unacceptable adverse effects on β blockers or diuretics, and 33 (10%) indicated that CCBs were prescribed for indications other than hypertension. In addition, the following contraindications for β-blocker therapy were noted: 18 (10%) indicated chronic obstructive pulmonary disease (COPD) or bronchospasm, 24 (13%) indicated diabetes mellitus, and 6 (3%) indicated a history of depression.
Table 4.
Drug Indication for Patients Maintained on Calcium Channel Blockers*
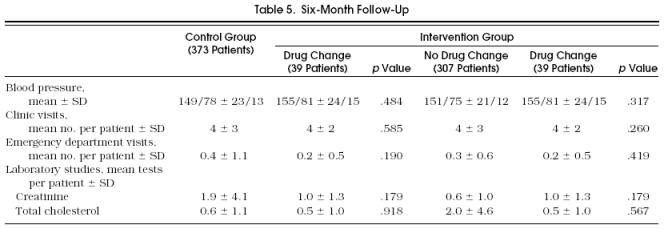
Other Utilization
To evaluate the impact of this intervention on nonpharmacy resources, we examined the follow-up BP, clinic visits, laboratory tests, and admissions according to group, and to whether drug therapy was changed, for the 6 months following the intervention (Table 5). In comparison with control patients, patients whose medication therapy was changed showed no clinically significant change in BP and no significant difference in the number of laboratory tests ordered, follow-up visits, or hospital admissions.
Table 5.
Six-Month Follow-Up
DISCUSSION
Current therapeutic guidelines are based on randomized, controlled clinical trials showing that β blockers and diuretics can decrease the incidence of stroke and myocardial infarction in persons with primary hypertension. Because no such evidence exists for CCBs, they are not considered first-line agents. There is emerging evidence that at least one category of CCB may be harmful. Moreover, CCBs are more costly than β blockers or diuretics. Despite these drawbacks, many providers use CCBs as drugs of choice for hypertension. Attempts to understand and decrease unnecessary variance from evidence-based clinical practice guidelines in medical practice are central to recent initiatives in quality improvement and cost containment.
We demonstrated a significant effect on drug-prescribing habits in a general internal medicine clinic through the use of a simple computerized reminder system. This intervention resulted in 11.3% of intervention patients being changed to first-line antihypertensive agents, without change in control of their hypertension. We believe that this change rate is actually conservative, as the computer program misclassified 23% of patients who were prescribed these drugs for angina. By extending the exclusion for patients on nitrates to 2 years, another 66 patients (19.1%) would have been excluded from the study. None of these patients had their medications changed. Using these criteria, 14% of patients had their medications changed to first-line agents. Excluding patients that had any provider-reported contraindication, 23.6% of patients seen by intervention providers had therapy altered.
We also note that, at baseline, a larger number of patients in the intervention group were already on β blockers and ACE inhibitors, biasing the study against finding a significant effect of the intervention and making regression toward the mean an unlikely explanation of the findings. This study population included many patients with comorbid conditions, such as diabetes mellitus, hyperlipidemia, COPD, and benign prostatic hyperplasia, that might also bias providers against the use of either β blockers or diuretics. In other, healthier populations the rate of change might be expected to be higher because there would be fewer relative contraindications for the use of β blockers and diuretics.
This study also provides information on the reasons CCBs are used in a VA outpatient setting. Almost one quarter of patients were reported to have both hypertension and angina. In almost 10% of patients, CCBs were used for indications other than hypertension or angina, with chronic headache and arrhythmias accounting for most of these cases. Finally, by report of their physicians, almost 25% of patients either failed to obtain adequate BP control or had unacceptable adverse effects using β blockers or diuretics, suggesting failure rates for first-line therapy that are higher than reported in larger drug trials.
Our findings are consistent with past studies in demonstrating that an intervention can change provider prescribing behavior if it is individually targeted and delivered at the point of patient contact. It differs from past studies in showing that successful interventions need not be labor-intensive, as with academic detailing, but rather can rely on computer case finding to identify potentially modifiable prescribing patterns. The ability to design and implement an intervention that changes utilization without requiring extensive infrastructure or personnel makes it particularly attractive.
Though this trial was not designed for a formal cost analysis, we can make crude estimates of the cost of the study and the potential cost savings from drug changes. The computer program was developed in approximately 18 hours of programmer time, which would cost approximately $460. Each study day required approximately 10 minutes of time by the pharmacist to place the study insert in the patient chart. This time totals 16 hours over the 20-week study period, which would cost approximately $400. The total of direct costs was therefore less than $1,000. The total cost savings, calculated by subtracting the cost of the substituted drug from the previously prescribed CCB, was $7,140 for the 6-month period following the study. There was no evidence that providers ordered more laboratory tests or that patients had greater clinic utilization after their medications were changed. Full cost studies have shown that β blockers and diuretics are less expensive than CCBs for the treatment of hypertension, even when the costs of additional follow-up, laboratory testing, and treating any adverse effects are included.16 This intervention did require that the guideline reminder be manually placed in the patient chart after the patient was identified by a case-finding computer program. This protocol was adopted so that information on patients whose drug therapy was not changed could be gathered. If this type of intervention is adopted as an ongoing quality-improvement measure, the guideline reminder could be printed with the individual patient prescription refill forms currently printed in the clinic, thus fully automating the intervention.
Although this study was able to show clear changes in prescribing behavior through a simple intervention, it has several limitations. First, this study in a VA population may not be generalizable because of the relative homogeneity and high acuity of this population. The average patient in this trial was 63 years old and carried eight outpatient diagnoses in addition to hypertension. This may not represent most outpatient populations, but may represent an advantage because therapeutic changes would be more difficult in the setting of greater comorbidity and a larger number of special circumstances that might encourage the use of second-line antihypertensive agents.
Second, this intervention did not test for all areas of quality improvement, and did not examine patient outcomes or quality of life. Adverse drug effects are often cited as reasons for the failure of β blockers and diuretics in the treatment of hypertension. Several studies have concluded that quality of life rises with treatment for all classes of antihypertensive medication, and that no persistent differences in quality of life can be found between different classes of antihypertensive agents.17,18 Although this trial was not designed to test for changes in quality of life, there is no reason to believe that a differential in quality-of-life changes would have been seen.
Third, this trial was not designed to test for persistence of effect. In most settings, interventions that change provider behavior show decay of intervention effect over time. Although we were able to show that providers were willing to change prescribing habits when prompted at the patient-visit level, it is not clear whether this intervention actually changed long-term prescribing habits.
Finally, this trial was conducted in an academic setting. Providers in this setting may be more inclined to consider altering their practice style, particularly when prompted by a colleague. Though this effect cannot be ruled out, providers knew that the investigators were blinded to their identities throughout the trial. Providers in this setting may also be more influenced by recent negative literature on CCBs, though this effect would be seen in both control and intervention providers.
Our study shows that it is possible to use a simple, inexpensive, nonthreatening, computer-driven intervention to encourage treatment of hypertension in accordance with current recommendations. Similar interventions in other areas offer the potential to improve patient care with minimal implementation costs. When treatment according to guidelines can be cost-saving, as with hypertension, such programs could reach the elusive goal of simultaneously improving care while decreasing total health care costs.
Acknowledgments
The authors thank the following individuals at the VA Puget Sound Health Care System for their help and support: Debbie Redman, RPh, and Pharmacy Services for support in placing guideline reminders; Cheryl Canody of Information Resource Services for data extraction; Mary McDonnell, MS, and others at the ACQUIP project for patient data; Don Martin, PhD, for statistical advice and support, and Steve Fihn, MD, MPH, for study design and manuscript advice and review.
Appendix A

REFERENCES
- 1.Avorn J, Soumerai S. Improving drug-therapy decisions through education outreach: a randomized, controlled trial of academically based “detailing.”. N Engl J Med. 1983;308:1457–63. doi: 10.1056/NEJM198306163082406. [DOI] [PubMed] [Google Scholar]
- 2.Schaffner W, Ray WA, Federspiel CF. Improving antibiotic prescribing in office practice: a controlled trial of three education methods. JAMA. 1983;250:1728–32. [PubMed] [Google Scholar]
- 3.Ray WA, Fink R, Schaffner W, Federspiel CF. Improving antibiotic prescribing in outpatient practice: non-association of outcome with prescriber characteristics and measures of receptivity. Med Care. 1985;23:1307–13. doi: 10.1097/00005650-198511000-00009. [DOI] [PubMed] [Google Scholar]
- 4.West SK, Brandon BM, Stevens AM, et al. Drug utilization review in an HMO, I: introduction and examples of methodology. Med Care. 1977;15:505–14. doi: 10.1097/00005650-197706000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Hersey CO, Porter DK, Breslau D, Cohen DI. Influence of simple computerized feedback on prescription changes in an ambulatory clinic: a randomized, clinical trial. Med Care. 1986;24:472–81. doi: 10.1097/00005650-198606000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Gehlback SH, Wilkinson WE, Hammond WE, et al. Improving drug prescribing in a primary care practice. Med Care. 1984;22:193–201. doi: 10.1097/00005650-198403000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Groves R. Therapeutic drug-use review for the Florida Medicaid program. Am J Hosp Pharm. 1985;42:316–9. [PubMed] [Google Scholar]
- 8.Joint National Committee on Detection Evaluation Treatment of High Blood Pressure The Fifth Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V) Arch Intern Med. 1993;153:154–83. [PubMed] [Google Scholar]
- 9.Dahlof B, Lindholm LH, Hansson L, Schersten B, Ekbom T, Wester PO. Morbidity and mortality in the Swedish trial in old patients with hypertension (STOP-Hypertension) Lancet. 1991;338:1281–5. doi: 10.1016/0140-6736(91)92589-t. [DOI] [PubMed] [Google Scholar]
- 10.Maniolio TA, Cutler JA, Furberg CD, Psaty BM, Whelton PK, Applegate WB. Trends in the pharmacologic management of hypertension in the United States. Arch Intern Med. 1995;155:829–37. [PubMed] [Google Scholar]
- 11.Psaty BM, Heckber SR, Koepsell TD, et al. The risk of myocardial infarction associated with antihypertensive drug therapies. JAMA. 1995;274(8):620–5. [PubMed] [Google Scholar]
- 12.Furberg CD, Psaty BM, Meyer JV. Nifedipine: dose-related increase in mortality in patients with coronary heart disease. Circulation. 1995;92(5):1326–31. doi: 10.1161/01.cir.92.5.1326. [DOI] [PubMed] [Google Scholar]
- 13.Borhani NO, Mercuri M, Borhani PA, et al. Final outcome results of the multicenter isradipine diuretic atherosclerosis study (MIDAS) JAMA. 1996;276(10):785–91. [PubMed] [Google Scholar]
- 14.Reiber GE, McDonnell MB, Schleyer AM, et al. A comprehensive system for quality improvement in ambulatory care: assessing quality of diabetes care. Patient Educ Couns. 1995;26:337–41. doi: 10.1016/0738-3991(95)00741-h. [DOI] [PubMed] [Google Scholar]
- 15.Noreen EW. New York, NY: John Wiley & Sons; 1989. Computer Intensive Methods for Testing Hypotheses. [Google Scholar]
- 16.Hilleman DE, Mohiuddin SM, Lucas BD, et al. Cost-minimization analysis of initial antihypertensive therapy in patients with mild-to-moderate essential diastolic hypertension. Clin Ther. 1994;16(1):88–102. [PubMed] [Google Scholar]
- 17.Neaton JD, Grimm RH, Prineas RJ, et al. Treatment of mild hypertension: final results. JAMA. 1993;270(6):713–24. [PubMed] [Google Scholar]
- 18.Boissel JP, Collet JP, Leon L, et al. A randomized comparison of the effect of four antihypertensive monotherapies on the subjective quality of life in previously untreated asymptomatic patients: field trial in general practice. J Hypertens. 1995;13:1059–67. doi: 10.1097/00004872-199509000-00018. [DOI] [PubMed] [Google Scholar]


