For teachers of medicine, the outpatient clinic promises many unique educational opportunities including more complete observation of chronic diseases, closer relationships between teachers and learners, and a more appropriate forum for teaching preventive medicine, medical interviewing, and psychosocial aspects of disease.
Despite these educational benefits, teachers face many challenges in the clinics. Not only do most teachers feel there is inadequate time to teach,1 they also have little control over the distribution and organization of this time. Unlike teachers in hospital wards, who often focus on only two or three patients during teaching rounds, outpatient teachers must address the concerns of each patient while the patient is still in the clinic, leaving little or no time for more elaborate instruction (typically 1 minute or less per case).2 Furthermore, teaching about a single well-defined complaint often fails in the ambulatory setting because many problems occur simultaneously, organic findings are intertwined with psychosocial issues, and diagnostic questions are settled more often by observation or empiric treatment than by laboratory testing.
In a recent, comprehensive review of educational research on ambulatory education,3 four important points were made. First, the environmental variables of a particular outpatient clinic—case mix of clinic, pace of workload, structured time for teaching, space for teaching—have little if any impact on the overall ratings of teaching effectiveness.4,5 Second, the behavior of teachers strongly influences the perceived success of the ambulatory experience.6–8 Effective teachers ask questions, show interest, define goals, demonstrate competence, and, most importantly, spend time with the learner.9,10
Third, the definition of effective teaching in most studies is the learners’ perceptions of what is effective, even though this may relate poorly to specific goals of the curriculum. For example, medical students often rank their outpatient experience better than their inpatient one, although formal testing reveals no difference in acquired knowledge between the two areas.10–14
Finally, role modeling clearly influences learners. In one study, there were striking similarities between what teachers wanted to transmit to their students, what these teachers cherished about their own instructors, and what the students admired during the rotation and wanted to emulate subsequently.15 However, when residents were assigned to a teacher who demonstrated deficient charting practices and made fewer psychosocial diagnoses, the residents’ own practices began to suffer from identical deficiencies.16
The challenge for the clinician-educator, therefore, is to create opportunity and space for meaningful dialogue with one or more learners in the midst of a busy outpatient clinic full of vague and indolent patient problems. Based upon the literature just cited and years of experience teaching and observing medical students and house officers in a variety of ambulatory settings, we believe there are several principles that can make outpatient teaching effective, gratifying, and fun. In this article, we address the practical aspects of teaching in the clinic related to preparing the learner for the patient's visit, teaching during the visit, and teaching after the patient has left the clinic.
Preparing For The Visit
To make the teaching efficient and the flow of patients brisk, the teacher should define the learner's specific role in the clinic, especially when teaching medical students. Teachers should outline the following expectations: the number of patients the learner should see, the time to spend with each patient, the parts of the physical examination to perform, the content and form of the written note and case presentation, how to review the medical record efficiently, and when and how to consult the teacher. For example, the teacher could say:
I’d like you to see two patients this morning. I want you to spend about 30 minutes with this patient, and knock on my door when you are through. As you can see from our discussion, the most important parts of the examination are vital signs, thyroid, cardiac, lung, and abdominal examination.
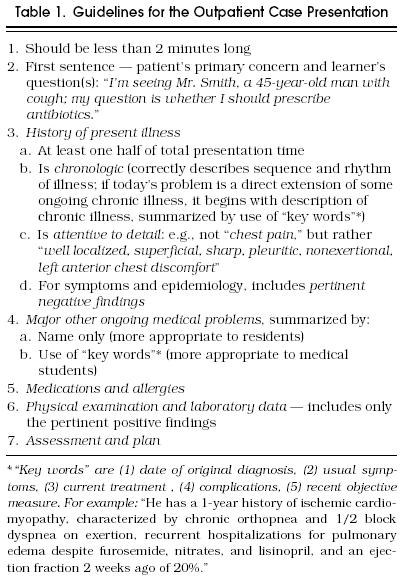
According to most studies of residents’ clinics, only 4 to 7 minutes is available per patient for the case presentation and discussion.2,17 This brief period of time can be consumed by a poorly organized oral case presentation and the teacher's subsequent questions that are necessary to clarify the case.2,18 The teacher can provide learners with guidelines to make oral case presentations more concise, complete, and thoughtful. An example appears in Table 1. Similar guidelines for the written note could contain information about basic content, common abbreviations, and other important details associated with billing and legal issues.
Table 1.
Guidelines for the Outpatient Case Presentation
Teaching During The Visit
Ask Questions
From the learner's perspective, the teacher's questions acknowledge the learner's role in the clinic, show interest in the learner's thoughts, and encourage the learner's clinical reasoning. From the teacher's perspective, questions are a quick way to diagnose the learner's strengths and shortcomings in order to target instruction to the learner's needs. The types of questions used to engage the learner reflect the focus of the clinic, the teacher's interests, the time available, and the learner's abilities. Questions should lead to a specific teaching point or general rule.
The teacher can ask questions after the case presentation, later during the clinic session, or even before the learner sees the patient (see below, Priming). The timing of these questions depends on the learner, the complexity of the patient's problem, and the time available to teach. Effective questions usually begin with a request for the learner's analysis of the case: “What do you think is going on?,” or “What would you like to do?,” followed by a request for supporting evidence: “Why do you think that?,” “What evidence did you obtain to support that approach?”
After asking the question, the teacher should allow enough time for the learner to respond. In most studies, teachers wait for students to respond to their questions for less than 1 second. The lack of adequate wait time often transforms thought-provoking questions into teachers’ monologues.19 If teachers prolong their wait time to at least 3 seconds, the students’ responses become three to seven times longer and contain more logical arguments and speculative thinking.19
Select One Teaching Point: The General Rule
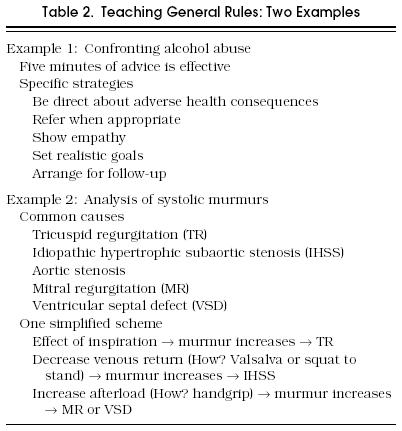
From the learner's answers to these questions, the teacher selects the one most appropriate teaching point, or general rule. Table 2 provides examples of possible general rules that the teacher could select for two different types of patients, one with suspected alcohol abuse and another with an unexplained systolic murmur. Both of these examples demonstrate principles behind selection of a general rule. First, the general rule is brief (i.e., it can be delivered in several minutes) and does not include everything the teacher knows about the subject. Second, it addresses the patient's concerns and the learner's needs, as gleaned largely from the learner's case presentation and analysis. For example, the teacher chose the second general rule in Table 2 not only because the patient had an unexplained systolic murmur, but also because it was clear that the learner's understanding of systolic murmurs could benefit from better information, organization, and review. Third, the general rule minimizes testimonials and emphasizes rational statements or principles that will apply to other clinical cases. When the teacher is trying to select the most appropriate general rule for the learner, one useful technique is to consider the central question: “What one teaching point do I want the learner to leave this patient's encounter with?”
Table 2.
Teaching General Rules: Two Examples
The teacher can deliver general rules even when the patient has no problems and the learner has no questions. Topics for this situation could include a preventive medicine issue, an interviewing technique, a physical diagnosis finding, or one of the patient's inactive problems. For example, a student may evaluate a patient who is new to the teacher's practice and who has no immediate concerns. The student then presents the case including the patient's liver span on physical examination. The teacher could then ask: “What is the normal range for the percussed liver span, and how accurate are clinicians anyway?”
Because the successful general rule does not need to address everything about a case, the teacher can easily transform the bewildering case into a memorable teaching exercise. For example, the learner may be evaluating a patient with depression who complains of back pain. The teacher would like to determine how the pain responds to antidepressant medication before pursuing other radiologic or rheumatologic studies. Even without a clear diagnosis, the teacher could ask the learner: “What are the diagnostic criteria for depression?,” “What antidepressant should we select?,” or “What findings would lead you to suspect spinal stenosis?”
The general rule for medical students usually relates the patient's problem to conditions with similar findings, addressing the question, “Where does this patient's problem, or treatment for that problem, fit into the larger framework of disease?” The teacher often assumes the more sophisticated resident already understands clearly that framework, and thus selects general rules that deal more often with specific aspects of diagnosis or management. For example, for a patient with venous ulcers:
Teacher to medical student: What are the common causes of leg ulcers and how do we distinguish them based on history and physical examination? (The general rule is the differential diagnosis of leg ulcers.)
Teacher to resident: What do we need to think of when venous ulcers fail to respond to treatment? (The general rule emphasizes the recognition of infection, arterial disease, carcinoma, pyoderma gangrenosum, and the normal slow healing of leg ulcers.)
The general rule for the resident would be lost on a learner who could not distinguish a venous ulcer from other causes of leg ulcers, and would risk the learner extrapolating the teacher's comments to the wrong condition.
When faced with many different learners and patients, one technique helpful to the organization of the teacher's thoughts is to make brief notes on an index card during the case presentation, addressing the patient's problem, the learner's analysis, and the general rule to impart (e.g., “how to confront alcoholism,” “systolic murmurs,” “liver span,” “why leg ulcers don’t respond”). The teacher refers to these notes when choosing the general rule, and again at the end of clinic to identify and review those issues only partially addressed earlier during the clinic session.
To help focus and organize the learner's understanding of the general rule, it is also helpful for the teacher to write out the general rule, each point as it is delivered, on a piece of paper for one or two learners or on a blackboard for larger numbers of learners. Table 2 illustrates how the general rule would appear in written form. These notes also provide an efficient way to return to teaching should an interruption occur.
The ability to teach general rules develops over time as teachers ask questions of learners and conceptualize general principles of patient care. With experience, teaching scripts emerge in the memory of teachers.20 These scripts include the purpose or goal of instruction, three to five key teaching points with supporting illustrations, and an understanding of common difficulties learners encounter when mastering the particular knowledge or skill. For example, the teaching script for leg ulcers may have four teaching points (differential diagnosis, general principles of management, why ulcers don’t heal, and the role of antibiotics) and contain two common difficulties (erroneous belief that antibiotics are useful, misdiagnosis of pyoderma gangrenosum). Once teaching scripts are developed, teachers ask questions to determine which teaching point they will use in the context of this case and this learner. These scripts can be developed for the most common problems encountered in ambulatory clinics.
Asking effective questions and teaching one general rule per patient are effective and efficient ways to teach more sophisticated learners, such as house officers. But, when working in a very busy clinic or with learners who are inexperienced, teachers will often use two other teaching techniques, priming and modeling.
Priming
To prime learners means to prepare them immediately before entering the patient's room. Priming is especially important for medical students, who, lacking the experience to recognize diagnostic patterns or set priorities during the visit, may begin to use unproductive and inefficient interviewing techniques, such as an exhaustive review of systems.
There are two different types of priming, one for the patient with a new problem and another for the patient appearing for a follow-up visit. Priming for new problems usually emphasizes differential diagnosis and typically consists of two questions. As an example, if a student is planning to see a patient with slowly progressive dyspnea, the teacher would ask, “What important causes of dyspnea are you thinking of,” followed by “What symptoms, risk factors, and physical signs are associated with each of these diagnoses?” The teacher's goal is to ascertain the student's abilities, and at the same time equip the student with the information necessary to promptly recognize likely diagnoses such as obstructive lung disease, congestive heart failure, chronic pneumonia, angina, or pulmonary emboli.
For the follow-up visit of a patient without a new problem, priming could emphasize questions about health maintenance (“What preventive health measures should we address this visit?”) or different ways to maintain the medical record. For a patient with a chronic disease, the question could focus on the disease's complications. For example, before the student sees a patient with chronic hepatitis C, the teacher may ask, “What complications do we need to think of ?” This empowers the student to recognize the complications of chronic liver disease, such as ascites, encephalopathy, gastrointestinal bleeding, and hepatocellular carcinoma.
Another strategy, especially useful when the teacher is simultaneously seeing patients, is to identify a patient on the schedule and ask the student to prepare for the visit by reading while the teacher sees other patients. The teacher could say: “A patient with congestive heart failure is scheduled for l0:00 AM. I want you to read about this and see the patient when he arrives.”
After the brief priming session, the students should be reminded that the patient's concerns are always the focus of the visit, and that priming does not replace the central role of open-ended questions at the beginning of the patient interview. Priming simply supplies some background and direction for the visit. Even during the rare occasion when the patient's real concern is different from that listed in the nurse's triage note, a lesson from the priming session may easily become the one general rule the teacher will impart for that patient.
Modeling
Another form of teaching in the clinic is modeling, a useful technique when there is insufficient time to ascertain the learner's analysis of the case or when a case is beyond the sophistication of the learner. When modeling, the teacher simply thinks out loud, shares clinical hunches and insights, points out controversial issues, or provides a rationale for what to accomplish during the visit. Modeling helps patients flow through a busy clinic efficiently and quickly. When done with the learner's interest foremost in the teacher's mind, modeling provides a nice balance to the question-asking style and offers the learner conceptual scaffolding for the case and problem. In a complicated case, the teacher often shares the general rule after the modeling session, either immediately after the patient's visit or later during the clinic session.
The most important technique for modeling is for the teacher to identify which specific behavior he or she wants the learner to observe. For example, a patient with a pulmonary nodule arrives for a follow-up visit after a needle biopsy revealed carcinoma, a diagnosis not yet known to the patient. The teacher could say to the learner before entering the room: “I’d like you to observe how I share bad news with a patient.” Or, before seeing a patient with frequent falls, the teacher could say: “Of course, alcohol is really the problem here. I’d like you to watch how I try to confront that issue during the interview.”
In these examples the learner accompanies the teacher during the visit, but modeling can be just as effective after the learner has independently evaluated the patient. As before, the key element is to specifically tell the learner what behavior or technique to observe during modeling. For example, after the learner evaluates and presents a patient with angina and a systolic murmur of uncertain significance, the teacher could say: “The findings you present are a little confusing. Why don’t we go in and repeat the examination together?”
Or, the learner has evaluated a patient with increasing ataxia, more prominent in the legs than arms, but also slightly worse on the right side than on the left side. After the learner's oral case presentation leaves the teacher confused about the patient's diagnosis, the teacher and learner return to the patient's room and review the findings together. The teacher then “models” his or her own analysis of the case outside the patient's room, acknowledging that even the teacher's solution is sometimes imperfect and contains inconsistencies.
The technique of modeling in this example not only efficiently manages a complicated case in a busy clinic, but also shows the student how one expert clinician deals with the ambiguities and uncertainties so common in clinical medicine.
With each of these examples, the teacher may choose to teach general rules when time permits, usually later in the clinic session or after the clinic, formally in a postclinic conference or informally over a cup of coffee. One time-saving device for the teacher working with medical students is to ask the student to begin working on the written note while the teacher continues to see other patients. The student should complete everything up to the point of the assessment and plan, which are added later only after hearing the general rule.
The key to effective modeling is articulation of clinical knowledge and reasoning, demonstration of competent and compassionate care, and active involvement of the learner. During modeling, the teacher actively involves the learner by priming or by subsequently teaching the general rule. These recommendations overcome the common complaints of students who passively shadow a teacher and quickly become bored.
Seeing the Learner's Patients
Teachers typically see most of the medical student's patients. Older studies of residents’ clinics revealed that teachers served only as hallway consultants 86% to 98% of the time,17,21 but in recent years third-party payer and legal considerations often require that all of a resident's patients have contact with an attending physician. Although the extent of this contact varies, the few extra minutes required provide tremendous insights into the learner's skills and new opportunities for improved teaching and patient care. In one study, teachers assigned ratings to the resident's evaluation and the perceived severity of the patient's illness, both immediately after the resident's case presentation and again after directly seeing the patient.22 After seeing the patient personally, the teachers rated the residents’ evaluations less well and the patients as more severely ill. Furthermore, the teachers believed that 80% of the visits with patients had some value to teaching and 85% were helpful to patient management. Consultation time averaged 6.6 minutes for the case presentation and another 8.6 minutes with the direct patient visit included.
Provide Feedback
Effective feedback consists of specific statements about directly observed behaviors that use nonjudgmental language and balance descriptions of learners’ strengths and weaknesses.23,24 For example, after enduring a long case presentation, the teacher may say:
You’ve collected an amazing amount of information, and I admire the way you’ve been able to organize it quickly and thoughtfully. However, I’d like you to work on editing the information and limiting the length to less than 2 minutes. This is what I would have done . . .
Feedback is a powerful tool. In one study, residents were randomly assigned to one group that received feedback from patients and one group that did not. The group receiving feedback performed significantly better over the subsequent 6 months with respect to the art-of-care, technical quality, and total patient satisfaction.25
On many occasions, the teacher can deliver the feedback to the learner in the patient's room, especially when the teacher agrees with the learner's diagnosis (“Yes, I agree, that is a benign intradermal nevus”) or plan (“I agree completely with your doctor's plan to increase your atenolol dose a little”). Even when the teacher disagrees with the learner, feedback is sometimes best delivered in the room if the teaching point could only be made at the bedside and the language used is nonjudgmental and diplomatic. For example: “You know, I think that's actually a seborrheic keratosis because it is slightly raised, contains horn cysts, and appears as if it could be easily picked off.”
To avoid undermining the relationship between learner and patient, and to foster the supportive and nonthreatening environment necessary for effective feedback, extensive discussion about differential diagnosis or management should probably occur outside the patient's room. For example, if a resident is seeing a patient with chest pain but remains confused about whether the discomfort represents angina or some less-serious disorder, the teacher may enter the room, introduce himself or herself, complete the necessary evaluation, and then say: “Your doctor and I are going to step out of the room and put our heads together. Your doctor will be right back to share our thoughts with you.” Outside the room, the teacher and learner can arrive at an assessment and plan. The learner can then return to the patient's room and share the results with the patient.
Teaching After The Visit
The teacher may use the time at the end of the clinic to deliver or review the general rules encountered earlier during the day, or to organize a variety of activities, each designed to address various educational needs (Table 3).
Table 3.
Teaching Rounds: After the Patient Has Left the Clinic
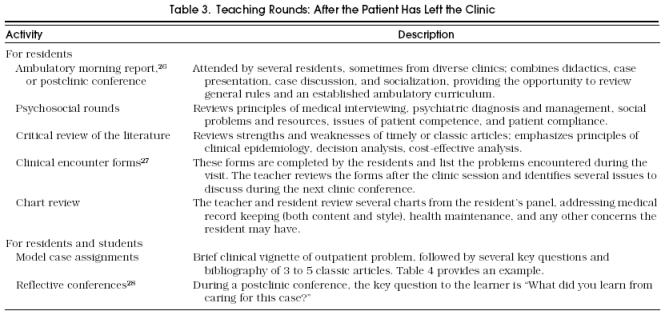
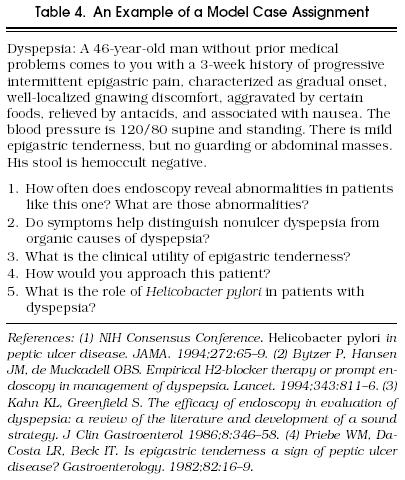
In contrast to learners on inpatient rotations who are usually sleep-deprived, those on outpatient rotations often have no evening and weekend responsibilities. Consequently, teachers can define more rigorous and consistent scholarly expectations for their learners. One excellent way for learners to explore the controversies and science of outpatient medicine is the model case assignment, which presents a clinical vignette followed by several questions and a bibliography of three to five classic articles (Table 4). Medical students usually receive these assignments the week before conference to allow them time to retrieve and review the articles. House officers do not receive these assignments ahead of time but rather use them as handouts for discussion during a preclinic or postclinic conference. Model case assignments provide an excellent way for teachers to cover a curriculum of subjects during a student or resident rotation.
Table 4.
An Example of a Model Case Assignment
Conclusions
One of the strengths of ambulatory education is the opportunity for learners to interact with patients and for teachers to model what they enjoy most about medicine without the intervening technology common to hospital wards. When medical students from the graduating class of 1990 were asked in a national survey what would make the specialty of internal medicine more attractive as a career, the most common suggestion was to increase the ambulatory experience and the connections with patients that such an experience provides.29
More research is necessary to identify which teaching techniques are effective in the clinic.3 Meanwhile, this article makes practical suggestions based on what is known about effective teachers and their behaviors. When teachers ask questions, present general rules, and model interactions, they create brief opportunities for teaching in an otherwise hectic day. Not only do learners recall these general rules, they subsequently want to emulate the teacher's caring attitude toward patients and organized approach to problem solving. Asking questions and modeling interactions help teachers share themselves and their love of medicine with their learners.
REFERENCES
- 1.Feltovich J, Mast TA, Soler NG. Teaching medical students in ambulatory settings in departments of internal medicine. Acad Med. 1989;64:36–41. doi: 10.1097/00001888-198901000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Knudson MP, Lawler FH, Zweig SC, Moreno CA, Hosokawa MC, Blake RL. Analysis of resident and attending physician interactions in family medicine. J Fam Pract. 1989;28:705–9. [PubMed] [Google Scholar]
- 3.Irby DM. Teaching and learning in ambulatory care settings: a thematic review of the literature. Acad Med. 1995;70:898–931. doi: 10.1097/00001888-199510000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Irby DM, Ramsey PG, Gillmore GM, Schaad D. Characteristics of effective clinical teachers of ambulatory care medicine. Acad Med. 1991;66:54–5. doi: 10.1097/00001888-199101000-00017. [DOI] [PubMed] [Google Scholar]
- 5.Little M, Rodnick JE. Evaluating student experiences in a family medicine clerkship. Fam Med. 1988;20:347–51. [PubMed] [Google Scholar]
- 6.Wolverton SE, Bosworth MF. A survey of resident perceptions of effective teaching behaviors. Fam Med. 1985;17:106–8. [PubMed] [Google Scholar]
- 7.Gjerde CL, Coble RJ. Resident and faculty perceptions of effective clinical teaching in family practice. J Fam Pract. 1982;14:323–7. [PubMed] [Google Scholar]
- 8.Stritter FT, Baker RM. Resident preferences for the clinical teaching of ambulatory care. J Med Educ. 1982;57:33–41. doi: 10.1097/00001888-198201000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Irby DM, Gillmore GM, Ramsey PG. Factors affecting ratings of clinical teachers by medical students and residents. J Med Educ. 1987;62:1–7. doi: 10.1097/00001888-198701000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Ramsey PG, Gillmore GM, Irby DM. Evaluating clinical teaching in the medicine clerkship: relationship of instructor experience and training setting to ratings of teaching effectiveness. J Gen Intern Med. 1988;3:351–5. doi: 10.1007/BF02595793. [DOI] [PubMed] [Google Scholar]
- 11.Packman CH, Krackov SK, Groff GD, Cohen J. The Rochester practice-based experience: an experiment in medical education. Arch Intern Med. 1994;154:1253–60. [PubMed] [Google Scholar]
- 12.Butterfield PS, Libertin AG. Learning outcomes of an ambulatory care rotation in internal medicine for junior medical students. J Gen Intern Med. 1993;8:189–92. doi: 10.1007/BF02599265. [DOI] [PubMed] [Google Scholar]
- 13.Papadakis MA, Kagawa MK. A randomized, controlled pilot study of placing third-year medical clerks in a continuity clinic. Acad Med. 1992;68:845–47. [PubMed] [Google Scholar]
- 14.Davis MH, Dent JA. Comparison of student learning in the outpatient clinic and ward rounds. Med Educ. 1994;28:208–l2. doi: 10.1111/j.1365-2923.1994.tb02700.x. [DOI] [PubMed] [Google Scholar]
- 15.Lublin JR. Role-modelling: a case study in general practice. Med Educ. 1992;26:116–22. doi: 10.1111/j.1365-2923.1992.tb00136.x. [DOI] [PubMed] [Google Scholar]
- 16.Quill TE. Medical resident education: a cross-sectional study of the influence of the ambulatory preceptor as a role model. Arch Intern Med. 1987;147:971–3. doi: 10.1001/archinte.147.5.971. [DOI] [PubMed] [Google Scholar]
- 17.Williamson HA, Glenn JK, Spencer DC, Reid JC. The development of clinical independence: resident–attending physician interactions in an ambulatory setting. J Fam Pract. 1988;26:60–64. [PubMed] [Google Scholar]
- 18.Walter LL, Zweig SC, Hosokawa MD. A process evaluation of a required primary care clerkship. Fam Med. 1991;23:547–8. [PubMed] [Google Scholar]
- 19.Rowe MB. Wait time: slowing down may be a way of speeding up! J Teacher Ed. 1986;37:43–50. (Jan–Feb): [Google Scholar]
- 20.Irby DM. What clinical teachers in medicine need to know. Acad Med. 1994;69:333–42. doi: 10.1097/00001888-199405000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Brook RH, Fink A, Kosecoff J, et al. Educating physicians and treating patients in the ambulatory setting: where are we going and how will we know when we arrive? Ann Intern Med. 1987;107:392–8. doi: 10.7326/0003-4819-107-2-392. [DOI] [PubMed] [Google Scholar]
- 22.Gennis VM, Gennis MA. Supervision in the outpatient clinic: effects on teaching and patient care. J Gen Intern Med. 1993;8:378–80. doi: 10.1007/BF02600077. [DOI] [PubMed] [Google Scholar]
- 23.Ende J. Feedback in clinical medical education. JAMA. 1983;250:777–81. [PubMed] [Google Scholar]
- 24.Thomasson C, Levinson W, Acheson K, et al. Teaching tips for clinician-teachers. J Gen Intern Med. 1994;9:349–53. doi: 10.1007/BF02599186. [DOI] [PubMed] [Google Scholar]
- 25.Cope DW, Linn LS, Leake BD, Barrett PA. Modification of residents’ behavior by preceptor feedback of patient satisfaction. J Gen Intern Med. 1986;1:394–8. doi: 10.1007/BF02596425. [DOI] [PubMed] [Google Scholar]
- 26.Malone ML, Jackson TC. Educational characteristics of ambulatory morning report. J Gen Intern Med. 1993;8:512–4. doi: 10.1007/BF02600116. [DOI] [PubMed] [Google Scholar]
- 27.Paccione GA, Cohen E, Schwartz CE. From forms to focus: a new teaching model in ambulatory medicine. Arch Intern Med. 1988;149:2407–11. [PubMed] [Google Scholar]
- 28.Arsenau R. Exit rounds: a reflection exercise. Acad Med. 1995;70:684–7. doi: 10.1097/00001888-199508000-00009. [DOI] [PubMed] [Google Scholar]
- 29.McMurray JE, Schwartz MD, Genero NP, et al. The attractiveness of internal medicine: a qualitative analysis of the experiences of female and male medical students. Ann Intern Med. 1993;119:812–8. doi: 10.7326/0003-4819-119-8-199310150-00007. [DOI] [PubMed] [Google Scholar]


