Clinical teachers have the challenging and profound responsibility to convey the art and science of current medical practice. Fortunately, over the past four decades, a variety of programs have been developed to help them play this difficult role. Starting with the initial work of Miller and colleagues in the mid 1950s,1 faculty-development programs to enhance instructional skills have been created for the large cadre of clinician-educators in this country. Since 1978, the Department of Health and Human Services and foundations such as the Kaiser Family Foundation, the Macy Foundation, and the Robert Wood Johnson Foundation have supported programs that emphasize teaching. Such initiatives have resulted in a wide variety of faculty-development programs operating at the institutional, regional, and national levels.
The rationale for providing support for clinician-educators can be found in both the task of clinical teaching itself and the empirical studies of faculty-development programs. The task of teaching in general is complex and difficult.2 Clinical teaching can be especially difficult. First, its intended outcome—the effective training of medical practitioners—imposes a ponderous responsibility on the clinical teacher. In the short term, effective clinical teaching is necessary to provide society with excellent care for patients currently in teaching hospitals. Over the long term, effective clinical teaching provides the underpinnings for the high quality of care given patients away from the academic center, who are treated long after physicians finish their formal training. Second, clinical teaching is laden with many educational challenges requiring a breadth of skills. Clinical teachers are expected to address a wide range of educational goals (knowledge, attitudes, and skills); to work with learners who vary greatly in their experience and abilities (students through fellows); to use a variety of teaching methods (lecturing, small–group discussion, and one-on-one teaching); and to teach in different settings (inpatient, outpatient, and lecture hall).3–5 Moreover, clinical teaching is commonly compounded by the simultaneous requirement to deliver patient care. Given this complexity, clinical teachers need to be prepared with as many teaching skills as possible.
Empirical studies provide further evidence for the value of faculty development. First, in evaluating many faculty-development programs, clinical teachers rate the experience as useful, and they recommend their experience to colleagues.6,7 Second, evaluation measures show that such programs can improve teachers’ knowledge, skills, and attitudes. These measures include improvements in the following: self–reported knowledge and the use of educational terms before and after training,8 retrospective ratings of knowledge and skills,9,10 teacher ratings of self-efficacy in teaching specific content,11 teacher behavior during problem-based tutorials,12 teacher beliefs regarding problem-based methods,13 ratings from videotapes of participants’ teaching,3 and attitudes toward collaboration between community faculty and university programs.14 Other unpublished data describe improvements in student ratings,15 participants’ self-report 3 to 6 months after training regarding the concepts and skills taught in the program (T. A. DeWitt and M. Quirk, unpublished results),16 and participants’ ability to use educational concepts when analyzing videotaped teaching scenarios (K. M. Skeff and G. A. Stratos, unpublished results).17 In summary, the difficulty of clinical teaching coupled with the evidence that clinician-educators can improve in this role indicates the value of faculty-development programs.
Although this rationale for using faculty-development methods is forceful, most medical faculty still have not participated in programs to improve teaching skills. Possible reasons include barriers to faculty participation and lack of knowledge about resources. To help more faculty benefit from available methods, we shall discuss potential barriers to participation in faculty-development programs, provide a summary of the types of available programs in primary care fields, describe characteristics of effective teaching-improvement methods, and recommend how to choose among teaching-improvement methods.
BARRIERS TO PARTICIPATION
Several potential barriers can impede participation in teaching-improvement programs. Such barriers include the attitudes and misconceptions of teachers, insufficient support from institutions, and the relative shortage of research on teaching-improvement methods. This discussion is intended to assist faculty in understanding and overcoming these barriers. At least three logical and understandable attitudes of teachers can diminish the likelihood of participation: (1) a tendency to underestimate the need for or potential benefits from a program, (2) a lack of belief in the utility of teaching skills as opposed to clinical skills, and (3) a belief that teacher training is unrelated to teaching excellence.
Need and motivation theories of learning predict that clinical faculty, like other adults, generally require motivation to learn.16,17 Many clinical teachers have a strong motivation to do an excellent job simply because of their commitment to and enjoyment of teaching. However, many faculty do not perceive a need to improve, or do not see their potential for improvement. This attitude may reflect their lack of knowledge that methods can be helpful rather than lack of interest in excellent teaching.
Research has shown that faculty may underestimate both their own potential for improvement and the potential usefulness of programs. In studies involving community and university faculty, participants have rated their training as more beneficial than anticipated, indicating that faculty may underestimate the usefulness of the methods prior to participation.7,14,18 One criticism of these findings is that participants are usually volunteers and, therefore, could be biased toward favorable reviews. However, in one study, essentially all potential participants volunteered, indicating that faculty-development methods may be useful to the faculty at large.3 Research findings also indicate that participants may not be fully aware of their teaching problems and may overestimate their teaching strengths prior to participation in a faculty-development program.9,18 Participation appears to be necessary for a true understanding of program benefits; therefore, we caution faculty not to rule out participation in a program without careful consideration.
Another impediment to participation in teaching-improvement programs is teachers’ beliefs that teaching skills are truly separate from clinical expertise or knowledge, and that clinical skills are sufficient for excellent teaching. Clearly, there is a relationship between the quality of the knowledge base and the ability to teach that knowledge base. Research on medical problem solving indicates that it is easier to solve problems related to knowledge than problems that are totally foreign. Approaches to problems can be learned, but approaches are not isolated from knowledge about the problem.19 There is a similar interaction in teaching. For example, when establishing educational goals for a student, clinical knowledge helps the teacher define the goals. When generating enthusiasm in a student, knowledge about clinical controversy helps. When explaining a concept, evaluating learners, or providing feedback on learner performance, clinical knowledge is essential.
Knowledge alone, however, does not ensure effective teaching, and teachers who lack knowledge can still promote learning. For example, all medical students have experienced knowledgeable teachers who were not able to convey information effectively. These teachers made information boring or confusing, or suppressed students’ enthusiasm. In contrast, teachers who lack knowledge can use teaching skills to promote learning, using gaps in knowledge as stepping stones to new information. This area has become an important topic of discussion in teaching-improvement seminars, in which faculty participants commonly acknowledge the temptation to avoid or cover up gaps in knowledge during teaching. The pressure of being observed as the teacher, the feeling that one “ought to know,” or the challenge of facing the more knowledgeable student or resident can make teachers uncomfortable. However, clinical teachers can use gaps in their knowledge as opportunities for stimulating others to learn. In this manner, the teacher and learner become colearners—colleagues in the educational process—a relationship that should occur frequently between colleagues throughout a person's professional career.
The educational literature contains an extensive discussion of the relationship between knowledge and teaching. Shulman has used the term “pedagogical content knowledge” to describe the knowledge base that a teacher draws on to transform understanding of a particular content area into instruction.20 The most expert teachers of a particular subject matter are aware not only of the content, but also of the ways to make the content understandable to the learner. They are aware of learners’ difficulties with the content as well as of the structure of the content. A master of knowledge can learn new teaching skills. A master of teaching can facilitate the acquisition of new knowledge.
Teachers may also believe that training is unrelated to excellence, arguing that most of the best clinical teachers are untrained, or that training is not necessary. Although it is true that many “untrained” teachers are superb, we believe that it is important to answer the following questions: Are untrained teachers as good as they could be? Is training useful? Faculty-development research has shown that clinical teachers can be more effective and enjoy their teaching more with formal instruction. Thus, even the best clinicians and teachers can benefit from training. Some teachers are excellent without training; however, that fact should not diminish attempts to help all teachers be as effective as possible.
Lack of institutional support for teaching can impede participation in faculty-development programs. Currently, institutions are struggling to respond to the consequences of managed care. Academic institutions, although committed to teaching and research, are being asked to replicate the efficiency of nonteaching institutions—businesses that are themselves under greater productivity requirements in the current health care era. Community physicians, who are increasingly asked to have students and residents in their offices for “real world” learning experiences, are also faced with increased requirements for clinical productivity. These increased demands threaten not only participation in teaching-improvement programs, but even faculty investment in the teaching process itself. Yet, these same constraints on clinicians increase the need for effective teaching skills, given the time restrictions. As institutions position themselves for the new era, an ongoing commitment to quality teaching will be necessary to facilitate participation in teaching-improvement programs. Recent programs have been developed to foster improved teaching, and they have shown their utility for meeting institutional and individual goals.14
Time for faculty development-programs is another critical issue. A faculty member might ask, “Should I devote time to the pursuit of excellence in teaching?” Teaching improvement requires time. Most programs take at least 1 to 2 hours, and more comprehensive ones require a day, a weekend, or even longer; with follow-up sessions to promote continued improvement. Like the practice of medicine, the practice of teaching is never finally mastered. New content, new learners, and new settings all challenge teachers to new growth.
A final barrier to participation may be the relative scarcity of research on teaching-improvement methods. Although evidence supports the usefulness of these methods, there is little research on long-term outcomes,21,22 such as the effects of faculty development on student learning, the timing of follow-up training, the need for different types of training for inpatient versus outpatient teaching, and the comparative effectiveness of different methods.
TYPES OF AVAILABLE PROGRAMS
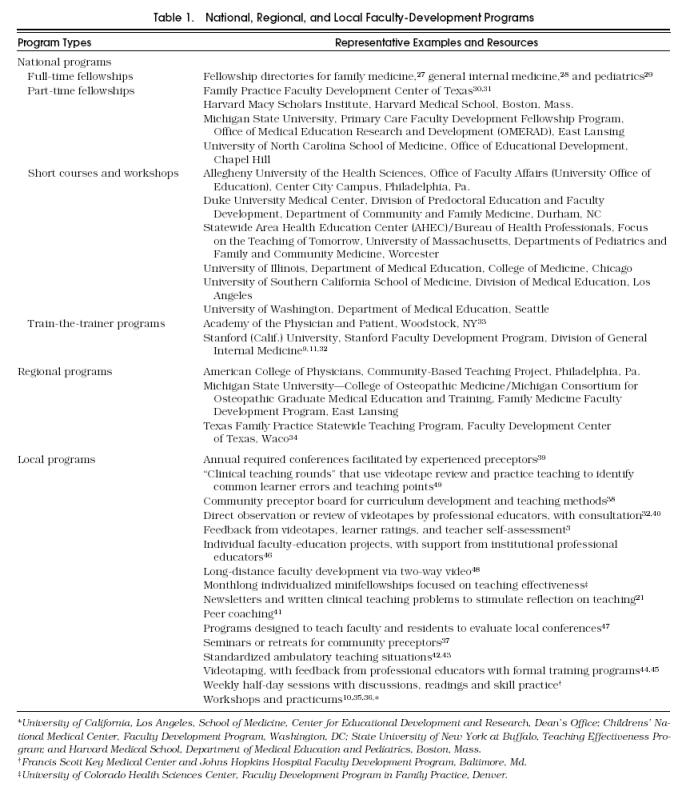
Another possible obstacle to faculty participation is the lack of knowledge about available teaching-improvement programs. In this section, we review the resources currently available. An extensive discussion of teaching-improvement methods for medical faculty can be found in the faculty-development literature.23–25 Teachers can take advantage of several types of approaches, including seminars, workshops, consultation with professional educators, feedback from learners, videotape review, microteaching, and self-evaluation. Capitalizing on such methods, a variety of teaching-improvement approaches have become available in the primary care fields. The following summary is based on a review of the published and unpublished descriptions of the programs, including the medical-education literature, conference proceedings, and executive summaries from the 1993–94 grants in faculty development funded by the Department of Health and Human Services. The extensive work in medical education that has been conducted in other countries is not included in this summary. A list of representative programs of each type is provided in Table 1. To facilitate access to the programs listed, we have categorized them according to whether they are focused on assisting faculty at the national, regional, or local levels. For people who wish to develop their own methods, Bland and colleagues have produced a useful resource: Successful Faculty in Academic Medicine: Essential Skills and How to Acquire Them.26
Table 1.
National, Regional, and Local Faculty-Development Programs
National Approaches to Teaching Improvement
The national approaches to primary care faculty development include full-time and part-time fellowships, train-the-trainer programs, short courses given at several institutions, and brief programs at national meetings (see Table 1) .27–49 Full-time fellowships, usually 2 years in duration, are designed to prepare medical fellows for full-time academic careers. Although these fellowships generally encompass teaching skills, they also emphasize other important faculty roles such as research, administration, and, to a lesser degree, patient care. The fellowship directories for family medicine, general internal medicine, and general pediatrics provide important resources for future academic faculty.28,29,33 In part-time fellowships, current faculty members spend a limited time (from several weeks to several months per year) in formal training at the institution providing these programs, and then conduct projects at their home sites. By combining training at the center with application of important knowledge and skills at the fellow's home institution, these programs teach both the theory and practice of critical faculty skills. A number of centers offer self-contained periodic workshops for faculty from around the country on educational topics related to clinical teaching—for example, teaching improvement and curriculum development. A final type of national program, exemplified by the Stanford Faculty Development Program7 and the American Academy on Physician and Patient,33 uses a train-the-trainer model for teaching improvement to provide more trainers for faculty at individual institutions. These trainers also can serve as regional and national resources.
Finally, there is a growing number of courses on education and teaching being provided at national meetings of each of the primary care societies, including the Society of General Internal Medicine (SGIM), the American Academy of Family Practice (AAFP) in conjunction with the Society of Teachers of Family Medicine (STFM), and the American Academy of Pediatrics (AAP). In addition, other national organizations are examining the issues of teaching in their national meeting, including the Association of Program Directors in Internal Medicine (APDIM), the American College of Physicians (ACP), and the Society for Medical Decision Making (SMDM). The field of internal medicine has sponsored a biannual conference, “Teaching Internal Medicine,” which is a forum for national presentations about all aspects of teaching internal medicine.50 It has broad-based sponsorship, including sponsorship from the Association of Professors of Medicine (APM), APDIM, SGIM, and the Clerkship Directors in Internal Medicine (CDIM). Recently, the American Academy of Pediatrics sponsored a national meeting, “Pediatric Resident Education in Community Settings,” that emphasized faculty development and recruitment.
A final national approach to teaching improvement is the use of stand-alone materials to assist faculty. They include peer-reviewed compendia of materials for medical education, such as those provided by the APDIM clearinghouse; exportable curricula for faculty development; and manuals, kits, and newsletters.51 In addition, readers can use the Internet to access an annotated list of references on faculty development in the health professions (uchsc.edu/CIS). In summary, many national organizations in primary care are focusing on teaching improvement and can be used as resources by faculty from around the country.
Regional Approaches to Teaching Improvement
Other programs assist teachers at the regional level. For example, the American College of Physicians’ community-based teaching project has used groups of facilitators trained by the Stanford Faculty Development Program to conduct regional programs for community-based faculty and their institutional colleagues, such as clerkship and program directors.14 The Texas Statewide Preceptorship Program (TSPP) is organized across eight Texas departments of family medicine, the Texas Academy of Family Physicians, and the state of Texas.34 The Faculty Development Center of Texas organizes and presents annual workshops that are made available to the participating preceptors. The Michigan Consortium for Osteopathic Graduate Medical Education and Training (COGMET) uses a multi-institutional approach to regional training. The consortium is disseminating methods developed previously for use at the Michigan State University College of Osteopathic Medicine to the 16 consortium hospitals.
Institutional Approaches
Many institutions provide local training programs for their own faculty. We list a few of the programs, recognizing that we probably have omitted many excellent programs.
CHOOSING AMONG TEACHING-IMPROVEMENT METHODS
Given the availability of such a variety of methods, individual faculty and institutions need to decide what type of program might be most useful. One teaching-improvement approach is unlikely to meet the needs of all teachers. To maximize the likelihood of a useful experience, we offer a set of questions that a teacher could ask in selecting a teaching-improvement method.
Are the program characteristics consistent with empirical studies on effective faculty-development methods and with educational theory?
Empirical research and educational theory can guide faculty to programs with effective characteristics. Effective faculty-development programs have the following characteristics.52,53
A mission that addresses the needs of the faculty participants
A systematic approach to specific faculty and specific faculty skills
A program that takes into account the workplace of the teachers
An integrated curriculum that emphasizes theory and practice
The opportunity for practice and feedback
A program that builds relationships between program faculty and participants and among partipants
Knlwledgeable and committed program faculty
A balance of MD and non-MD educators as faculty
Participants who are committed to the goals of the programs
A program to train more that one person from a setting
A program that fits the mission and is integrated into the higher organization.
Effective programs focus on the participating teacher, the program's instructors, instructional methods, and characteristics of the participants’ teaching setting. Thus, these programs address not only the learning characteristics of the individual but also the functioning of the individual within the organization. Their emphasis on the organization's mission highlights the importance of a support structure for ongoing teaching improvement. Enthusiastic teachers returning from a faculty-development program can have their enthusiasm stifled and their skills suppressed if their organization does not see teaching as a key mission. Although faculty may participate solely because of their interest, environmental support can enhance their dedication to teaching improvement. Faculty can examine whether the goals of the program are consistent with the goals of their organizations. For the purposes of this article, the major question is whether the teaching skills emphasized by the program will be supported by the institution.
Learning theories both clarify findings of these empirical studies and provide other guidance to potential participating faculty. Skeff, Berman, and Stratos identified several theories that are particularly relevant to evaluating faculty-development programs including need theory, motive-acquisition theory, and social-learning theory.24 Need theory and motive-acquisition theory predict that successful faculty-development programs will address the perceived needs of faculty and will respond to faculty's sources of motivation. Programs that conduct and respond to needs assessments of their participants will be more likely to succeed.
These theories also point out at least two caveats about inherent learning tendencies that can lead faculty to avoid participation. First, faculty, like other adult learners, may not perceive their current level of skills accurately.9,18 Successful programs may have to create a need to learn by assisting faculty to identify unrecognized needs or opportunities to improve. Following a series of teaching courses for university and community physicians, participants estimated that more than 50% of the material presented was new, showing the relatively unknown nature of information on teaching.54 Thus, potential participants should examine a program not only to determine whether it addresses a perceived need, but also to see whether it has the potential of providing insight into yet unidentified areas for improvement.
Second, participation in faculty development may be inhibited by motivational drive. Maslow's theory of motivation predicts that humans take care of their basic needs (e.g., security) first, and, once these needs are met, they deal with their higher-level needs (e.g., intellectual and personal gratification).16 The current climate in medical care makes many faculty respond to immediate needs, such as job security. Yet, community physicians in current faculty-development programs have indicated that they teach because of the personal gratification—a higher-level need. Thus, potential participants may want to evaluate faculty-development programs in terms of their capacity to enhance professional gratification.
Social-learning theories explain the basis for other aspects of successful methods, with special relevance to the mastery of new teaching skills.55 Effective methods provide opportunities for practice. Although clinical teachers may benefit from thinking about and discussing new approaches to teaching, behavioral change requires practice. Bandura points out the usefulness of methods that include symbolic modeling (visualizing new behaviors); vicarious modeling (observing other people perform the behaviors); and especially, participant modeling (practicing the behaviors). Faculty-development programs that incorporate role playing have shown the benefits of modeling, skill practice, and constructive feedback in assisting faculty to acquire new skills. Therefore, to acquire new skills, faculty might look to programs that provide practice and feedback.
Other theories highlight other important elements of successful programs. For example, adult learning theory emphasizes the inclination of adults to base learning on prior experience.56 Clinical teachers have extensive previous experience as students, residents, and faculty that provides the basis for further learning about teaching. Successful programs use these characteristics constructively, building on participants’ experience. Potential participants might ask whether program methods and leaders embody this approach.
Is the program designed to address features of the teaching role most commonly played by the faculty member?
Teaching-improvement methods differ in their relevance to the needs of medical faculty. A faculty member should assess whether the program is oriented to the needs of (1) the front-line, hands-on clinical teacher; (2) the supervising administrator who has more responsibility for educational programs, such as a director of clerkships and residency programs, a dean of education, and a department chair; (3) a teacher trainer, or (4) a faculty member who wants to be involved in the scholarship of education by pursuing an advanced degree. In addition, one can ask whether there is a special focus on teaching in a hospital ward, hospital clinic, community clinic, or rural office practice; on teaching students, fellows, traditional medicine residents, or primary care residents, on a specific content area (patient-physician interactions or medical decision making)20; or on a specific instructional method (lecturing, small-group discussion, problem-based learning, case-based teaching). For an individual teacher, the key question is whether the method focuses on generic teaching skills applicable to a variety of settings or skills oriented to a particular teaching setting. For example, one course for community-based teachers may spend more time on the logistics of setting up an office for teaching, whereas another may emphasize the general teaching skills that the community-based teacher could use with students, residents, colleagues, and patients. Both types of courses can be useful; an individual teacher may prefer one to another at a given time.
Are the instructional approaches likely to lead to new insights?
Teaching-improvement programs may use a wide variety of approaches to assist faculty in improving teaching, including didactic lectures, self-study materials, videotape review, role playing, group discussions, peer coaching, one-on-one consultation, and readings. Teachers may choose among these methods on the basis of their educational goals, their preferred learning approaches, the time available for participation, the availability of resources, or the theoretical or empirical basis for the effectiveness of the method. In choosing among different educational methods, we suggest that faculty consider the method that offers the greatest potential for active learning—that is, the greatest chance to reflect on and practice new approaches. This recommendation comes both from educational theory57 and from our own experience. Powerful changes can occur when faculty have the opportunity to struggle with difficult aspects of teaching. This type of learning can occur in activities such as role playing exercises, in which participants can choose, implement, and reflect on their teaching behaviors, without the usual constraints of actual teaching. Thus, a program that encourages active involvement is most likely to provide the challenge that people need to incorporate the material. Reviews of videotaped role playing may be even more effective because they allow in-depth review of teaching and of the behaviors available to teachers. The greater the opportunities to practice teaching, the more likely the learning experience is to be powerful.
Does the program espouse the use of a particular teaching philosophy?
Some programs deliberately train participants in using a specific teaching philosophy—for example, learner-centered, problem-based learning, or self-directed learning approaches. Others are designed to train faculty in a variety of methods and incorporate multiple teaching philosophies. Faculty can choose courses based on their subscription to a particular philosophy or their desire to be exposed to other approaches. We recommend exposure to as many teaching philosophies as possible, including teacher-centered learning, content-driven learning, learner-centered learning, directed-learning and self-directed learning, didactic lectures and open-ended discussions.
We suggest that, rather than avoid a method with active role playing and videotaping because of concern about potential discomfort, choose such a program. Rather than assume that a professional educator's expertise may not be valuable to clinical teachers, take advantage of programs that offer such a resource. Rather than choose a brief method that may not be challenging, select a program with active involvement, practice, review, and consolidation. In summary, we hope that this article will facilitate participation in faculty development methods to assist clinical teachers in their important role.
JGIM’s E-mail Address
For Letters to the Editor or for information about submitting manuscripts to JGIM: Walklett@mail.med.upenn.edu
REFERENCES
- 1.Miller G. Cambridge, Mass: Harvard University Press; 1980. Educating Medical Teachers. [Google Scholar]
- 2.Wittrock MC, editor. 3rd ed. New York, NY: Macmillan Publishing Co; 1986. Handbook of Research on Teaching. [Google Scholar]
- 3.Skeff KM. Evaluation of a method for improving the teaching performance of attending physicians. Am J Med. 1983;75:465–70. doi: 10.1016/0002-9343(83)90351-0. [DOI] [PubMed] [Google Scholar]
- 4.Skeff KM. Enhancing teaching effectiveness and vitality in the ambulatory setting. J Gen Intern Med. 1988;3(s2):S26–33. doi: 10.1007/BF02600249. [DOI] [PubMed] [Google Scholar]
- 5.Bergen MR, Stratos GA, Berman J, Skeff KM. Comparison of clinical teaching by residents and attending physicians in inpatient and lecture settings. Teach Learn Med. 1993;5:149–57. [Google Scholar]
- 6. Mygdal WK. Participants accept STFM's invitation to excellence. STFM Messenger. February 1994.
- 7.Skeff KM, Stratos GA, Bergen MR, et al. The Stanford Faculty Development Program for Medical Teachers: a dissemination approach to faculty development for medical teachers. Teach Learn Med. 1992;4:180–7. [Google Scholar]
- 8.DeWitt TG, Goldberg RL, Roberts KB. Developing community faculty. Principles, practice, and evaluation. Am J Dis Children. 1993;147:49–53. [PubMed] [Google Scholar]
- 9.Skeff KM, Bergen MR, Stratos GA. Evaluation of a medical faculty development program: a comparison of traditional pre/post and retrospective pre/post self-assessment ratings. Eval Health Prof. 1992;15:350–66. [Google Scholar]
- 10.Keenan JM, Seim HC, Bland CJ, Altemeier TM. A workshop program to train volunteer community preceptors. Acad Med. 1990;65:46–7. [PubMed] [Google Scholar]
- 11.Albright CL, Farquhar JW, Fortmann SP, et al. Impact of a clinical preventive medicine curriculum for primary care faculty: results of dissemination model. Prev Med. 1992;21:419–35. doi: 10.1016/0091-7435(92)90051-i. [DOI] [PubMed] [Google Scholar]
- 12.Benor DE, Mahler S. New Directions for Medical Education: Problem-Based Learning and Community-Oriented Medical Education. In: Schmidt HG, Lipkin M, de Vries MW, Greep JM, editors. New York, NY: Springer-Verlag; 1989. pp. 248–70. Training medical teachers: rationale and outcomes. [Google Scholar]
- 13.Schmidt HG, Bouhuijs PAJ, Khattab T, Makladi F. New Directions for Medical Education: Problem-Based Learning and Community-Oriented Medical Education. In: Schmidt HG, Lipkin M, de Vries MW, Greep JM, editors. New York, NY: Springer-Verlag; 1989. pp. 243–7. Attitude change among medical teachers: effects of a workshop on tutorials. [Google Scholar]
- 14.Skeff KM. Philadelphia, Pa: American College of Physicians; 1996. Proceedings of the American College of Physicians’ National Community-Based Teaching Symposium; pp. 77–99. February 2–3. Setting the research agenda. [Google Scholar]
- 15.Skeff KM, Stratos GA, Bergen MA, Guarino C. Stanford, Calif: Stanford University; 1993. The implementation and evaluation of a teaching improvement method for faculty in the medical school basic sciences. Final Report submitted to Bing Teaching Initiative, School of Humanities and Sciences. [Google Scholar]
- 16.Maslow AH. New York, NY: Harper & Row; 1954. Motivation and Personality. [Google Scholar]
- 17.McClelland DC. Toward a theory of motive acquisition. Am Psychol. 1965;20:321–33. doi: 10.1037/h0022225. [DOI] [PubMed] [Google Scholar]
- 18.Skeff KM, Stratos GA, Berman J, Bergen MR. Improving clinical teaching. Evaluation of a national dissemination program. Arch Intern Med. 1992;152:1156–61. doi: 10.1001/archinte.152.6.1156. [DOI] [PubMed] [Google Scholar]
- 19.Elstein AS, Shulman LS, Sprafka SA. Cambridge, Mass: Harvard University Press; 1978. Medical Problem Solving: An Analysis of Clinical Reasoning. [Google Scholar]
- 20.Shulman L. Knowledge and teaching: foundations of the new reform. Harv Educ Rev. 1987;57(1):1–22. [Google Scholar]
- 21.Harris I, Kvasnicka JH, Ytterberg SR. Faculty development of community primary care preceptors. Acad Med. 1995;70:458–9. doi: 10.1097/00001888-199505000-00065. [DOI] [PubMed] [Google Scholar]
- 22.Irby DM. Teaching and learning in ambulatory care settings: a thematic review of the literature. Acad Med. 1995;70(s2):898–936. doi: 10.1097/00001888-199510000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Stritter FT. Handbook of Health Professions Education. In: McGuire CH, Foley RP, Gorr A, Richards RW, editors. San Francisco, Calif: Jossey-Bass; 1983. pp. 294–318. Faculty evaluation and development. [Google Scholar]
- 24.Skeff KM, Berman J, Stratos G. Clinical Teaching for Medical Residents: Roles, Techniques and Programs. In: Edwards JC, Marier RL, editors. New York, NY: Springer Publishing Company; 1988. pp. 93–121. A review of clinical teaching improvement methods and a theoretical framework for their evaluation. [Google Scholar]
- 25.Dinham SM, Stritter FT. Research on professional education. In: Wittrock MC, editor. 3rd ed. New York, NY: Macmillan Publishing Co; 1986. pp. 952–70. Handbook of Research on Teaching. [Google Scholar]
- 26.Bland CJ, Schmitz CC, Stritter FT, Henry RC, Aluise JJ. New York, NY: Springer Publication; 1990. Successful Faculty in Academic Medicine: Essential Skills and How to Acquire Them. [Google Scholar]
- 27.Fellowship Directory for Family Physicians . Kansas City, MO: 1995. American Academy of Family Physicians/Society of Teachers of Family Medicine. [Google Scholar]
- 28. Fellowship Directory for General Internal Medicine. Washington, DC: Society of General Internal Medicine; 1996.
- 29. General Pediatric Fellowships, within a compendium of all pediatrics fellowships. Pediatr. January 1996.
- 30.Ramsey CN, Hitchcock MA. A statewide model for faculty development in family medicine. J Fam Pract. 1980;11:421–6. [PubMed] [Google Scholar]
- 31.Hitchcock MA, Lamkin BD, Mygdal WK, Clarke CM, O'Connor Clarke S. Affective changes in faculty development fellows in family medicine. J Med Educ. 1986;61:394–403. doi: 10.1097/00001888-198605000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Patridge MI, Harris IB, Petzel RA. Implementation and evaluation of a faculty development program to improve clinical teaching. J Med Educ. 1980;55:711–3. doi: 10.1097/00001888-198008000-00011. [DOI] [PubMed] [Google Scholar]
- 33.Lipkin M, Putman S, Lazare A. The Medical Interview. New York, NY: Springer-Verlag; 1995. [Google Scholar]
- 34.Mygdal WK. The Texas Statewide Preceptorship Program: A decade of service to family medicine in Texas. Texas Fam Phys. 1990;41(s2):8. [Google Scholar]
- 35.Cole DR, Lieberman JA, Fox TG. Developing the private practice physician as a teacher of family medicine. Fam Med. 1983;15:43–6. [Google Scholar]
- 36.Howard DM, Bass EB, Kern DE. Chicago, Ill: 1991. Evaluation of a faculty development program on curricular innovation for academic and practicing internists. Proceedings of the conference: Teaching Internal Medicine. October. [Google Scholar]
- 37.Roberts KB, DeWitt TG. Faculty development of pediatric practitioners: complexities in teaching clinical precepting. Pediatrics. 1996;97:389–93. [PubMed] [Google Scholar]
- 38.Brooks B, Gephart D, Ladd-Brown L. 1995. Eighth Biennial Teaching Internal Medicine Symposium. Engaging community-based preceptors: redefining their role with the academic medical center. September. [Google Scholar]
- 39.Anderson J, Hess G, Rody N, Smith W. Improving a community preceptorship through a clinical faculty development program. Fam Med. 1991;23:387–8. [PubMed] [Google Scholar]
- 40.Hewson M. Washington, DC: 1995. Presented at workshop on Improving Medical Teaching: A Case-based Approach to Effective Teaching Strategies. AAMC Annual Meeting. The Wisconsin Teaching Improvement Program. November. [Google Scholar]
- 41.Flynn SP, Bedinghause J, Snyder C, Heckelman F. Peer coaching in clinical teaching: a case report. Fam Med. 1994;26:569–70. [PubMed] [Google Scholar]
- 42.Lesky LG, Wilkerson L. Using “standardized students” to teach a learner-centered approach to ambulatory precepting. Acad Med. 1994;69:955–7. doi: 10.1097/00001888-199412000-00004. [DOI] [PubMed] [Google Scholar]
- 43.Simpson DE, Lawrence SL, Krogull SR. Using standardized ambulatory teaching situations for faculty development. Teach Learn Med. 1992;4:58–61. [Google Scholar]
- 44.Foley R, Smilansky J, Bughman E, Sajid A. A departmental approach for improving lecture skills of medical teachers. Med Educ. 1976;10:369–73. doi: 10.1111/j.1365-2923.1976.tb01488.x. [DOI] [PubMed] [Google Scholar]
- 45.Bazuin CH, Yonke AM. Improvement of teaching skills in a clinical setting. J Med Educ. 1978;53:377–82. doi: 10.1097/00001888-197805000-00001. [DOI] [PubMed] [Google Scholar]
- 46. Hafler JP. The New Pathway—problem-based faculty development. Presented at workshop on Improving Medical Teaching: A Case-based Approach to Effective Teaching Strategies. AAMC Annual Meeting, Washington, DC, November 1995.
- 47.Rosenblum ND, Nagler J, Lovejoy FH, Jr, Hafler JP. The pedagogic characteristics of a clinical conference for senior residents and faculty. Arch Pediatr Adolesc Med. 1995;149:1023–8. doi: 10.1001/archpedi.1995.02170220089012. [DOI] [PubMed] [Google Scholar]
- 48.Heestand D, Garman K, Fisher D. Faculty development through distance learning. Acad Med. 1996;71:567. doi: 10.1097/00001888-199605000-00100. [DOI] [PubMed] [Google Scholar]
- 49.Lye P, Simpson D, Wendelberger K. Building clinicians’ teacher knowledge. Acad Med. 1996;71:569–70. doi: 10.1097/00001888-199605000-00104. [DOI] [PubMed] [Google Scholar]
- 50. Teaching Internal Medicine, Conference Proceedings. Washington, DC: Association of Professors of Medicine/Association of Program Directors in Internal Medicine.
- 51.Westberg J, Whitman N. Resource materials for faculty development. Fam Med. 1997 In Press. [PubMed] [Google Scholar]
- 52.Bland CJ, Schmitz CC. Enhancing Faculty Careers: Strategies for Renewal. In: Schuster JH, Wheeler DW, editors. San Francisco, Calif: Jossey-Bass; 1988. pp. 41–64. An overview of research on faculty and institutional vitality. [Google Scholar]
- 53.Bland CJ, Stritter FT. Characteristics of effective family medicine faculty development programs. Fam Med. 1988;20:282–8. [PubMed] [Google Scholar]
- 54.Skeff KM, Stratos GA, Bergen MR. Philadelphia, Pa: 1996. Final Report submitted to American College of Physicians. Faculty Development for Community-Based Teachers. [Google Scholar]
- 55.Rosenthal TL, Bandura A. Handbook of Psychotherapy and Behavior Change: An Empirical Analysis. In: Garfield SL, Bergin AE, editors. New York, NY: Wiley; 1978. Psychological modeling: theory and practice. [Google Scholar]
- 56.Knowles M. Houston, Tex: Gulf; 1978. The Adult Learner: A Neglected Species. [Google Scholar]
- 57.Trower P, Bryant B, Argyle M. London, UK: Methuen; 1978. Social Skills and Mental Health. [Google Scholar]


