Medical education is in the midst of fundamental change, not the least of which is the shift from hospital-based education to the outpatient setting. While outpatient experiences form the basis for education in family practice and many pediatrics rotations, the bulk of students’ and residents’ internal medicine teaching has continued to be within the hospital.1 As internal medicine clerkships and residency programs expand toward office-based education, a number of barriers are making the transition to the outpatient setting difficult. In a 1995 Clerkship Directors in Internal Medicine commentary on outpatient education,2 cost was cited as the greatest practical barrier to the implementation of ambulatory education programs.
In order for educators, health centers, and payers to understand and facilitate this ongoing change in the teaching setting, the cost of ambulatory education must be known more precisely. Since the first studies to measure ambulatory teaching costs published in the late 1970s,3–5 a number of reports have defined, estimated, and measured costs in this setting. We set out to review the methods of estimating and calculating the costs of teaching in the ambulatory setting, and to synthesize the results of those studies that have measured the cost of teaching outpatient medicine.
Methodology
Method of Review
We conducted a MEDLINE search of all English language articles using the key words outpatient, ambulatory, cost, finance, teaching, education, or primary care. In addition, we used the Science Citation Index to cross-reference all articles that cited several of the key authors in the field from 1990 to the present. Articles that were included in our data set met any of the following criteria: (1) calculated or estimated a direct dollar value for any aspect of ambulatory education of either students or residents, (2) measured or estimated the efficiency of a physician while he or she was teaching a student or resident in the office, and (3) measured or estimated any indirect costs associated with the generation, delivery, or maintenance of ambulatory education programs. A total of 26 articles met these criteria and were included in our final cost calculations.
Definition of Costs
Costs have been defined in a number of ways by various investigators. For the purpose of this study, we have defined cost as any of the following: (1) decreasing billing productivity of the teaching physician or teaching site; (2) decreased patient productivity, or fewer numbers of patients seen by the teaching physician; and (3) extra time accounted for by the physician while teaching. We present data that synthesize these reports to describe an overall dollar cost for ambulatory education.
Reporting of Costs
Because the articles in this review reported data in a number of ways, we have standardized the results using a single unit of measure for ease of comparison. For billing productivity, we converted the data into a dollar amount that represents the change in total dollars that would be billed in 1 year by the teaching physician if a student or resident were present in the office for a full year. Patient productivity is reported as a whole number that represents the difference between the number of patients who would be seen by the teaching physician per full day were a student or resident present in the office and the number who would be seen in a full day without a student or resident. Time costs are reported as the number of extra minutes that would be spent in the office by the teaching physician per full day with a student or resident. Finally, we report the net average dollar cost per full day for ambulatory education of students and of residents. We assumed that the average physician sees patients for eight half-day sessions per week, that an average of three patients are seen by a student, and that five patients are seen by a resident per half-day (these assumptions are consistent with the internal medicine literature to date).6–9 Using these assumptions, we then calculated a net dollar cost per day for each study, and we report the average cost of all studies for student teaching sites and resident teaching sites.
Because of the wide variability in the presentation and measurement of these costs, as well as the lack of standardization across sites and programs in this review, we did not attempt to weigh any of the variables we have reported. Dollar values were recalculated using the consumer price index from the U.S. Department of Labor so that all reported dollar figures represent 1996 dollars.
Review Of The Literature
A list of the costs that have been measured is shown in Table 1. We have classified these costs into the following categories: (1) decreased productivity of the teaching physician or teaching site, (2) increased operating costs, (3) direct cost of trainee support, (4) loss of patients, (5) increased time in the office for the purpose of teaching, (6) revenue losses resulting from the types of patients seen in teaching sites, and (7) increased clinical costs (cost of extra medical resources used at a teaching site or resulting from the practice patterns of students or residents).
Table 1.
Costs of Ambulatory Teaching Cited in the Literature
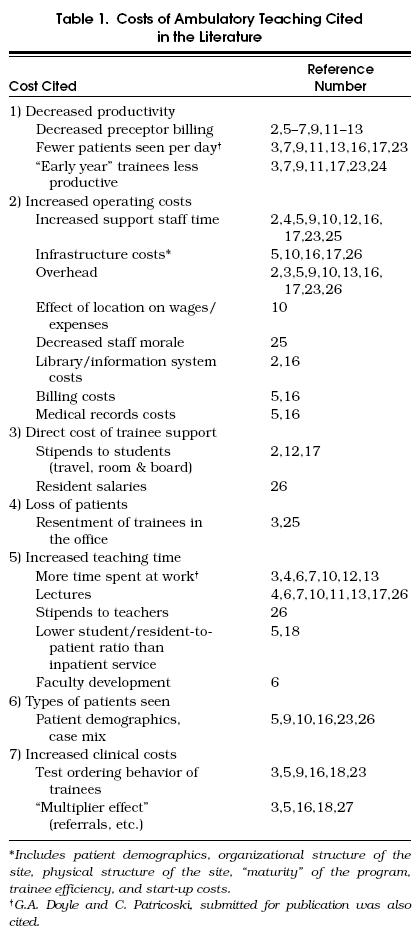
We have not done an extensive evaluation of institutional start-up, operating, or overhead costs. This has been outlined elsewhere,10 in a report that incorporates numerous factors such as site type, location, size of the program, maturity of the program, and other variables into an equation in order to characterize these costs for a particular institution. Rather, we have focused on those costs that the practitioner would incur as a result of teaching a student or resident in the office: billing productivity, patient productivity, and time costs. These three variables are also the most frequently reported outcomes in the literature.
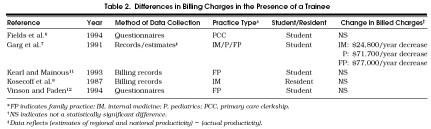
Billing Productivity
Five investigators measured the change in the total charges billed by a practice while a student or resident was present (Table 2). In general, data were obtained by questionnaires or review of the billing records of each practice. Most sites were family practice offices, and all but one were teaching sites for students only.6–8,11,12
Table 2.
Differences in Billing Charges in the Presence of a Trainee
Four of the five studies, including two that used “self controls,”6,11 showed no difference in billed charges when a student was present. The one study that reported a decrease in billed charges did not use practices as their own controls.7 Rather, regional and national billing averages were compared with the actual billing in the practices while a student was present. This study noted significant differences in estimated loss of revenues among family practice, internal medicine, and pediatrics ($52,000 per year greater loss in family practice than internal medicine and $47,000 per year greater loss in pediatrics than internal medicine).
Within each study a few individual offices noted an increase in billed charges while a student was present. Most of these offices were “mature” teaching offices; that is, the offices were long-standing training sites for students with preceptors who frequently taught in the office.
The one report that studied resident costs also showed no significant change in billing charges.8 In this study, as well as most studies we reviewed of resident costs in the outpatient setting, the teaching site was a hospital-based clinic that used full-time faculty as preceptors. These physicians did not see their own patients while precepting residents. We found no study that measured billed charges in a community-based office with residents present.
Overall, it seems that billed charges for most practices do not change considerably when students or residents are present.
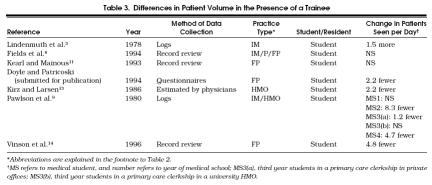
Patient Productivity
Another way investigators have measured productivity is to compare the number of patients seen by physicians while teaching, with the number seen in the absence of a trainee (Table 3). All studies of this type evaluated student sites only (G.A. Doyle and C. Patricoski, submitted for publication).6,9,11,13,14 Six of seven in this group were family practices or combined primary care practices. Results of these studies varied greatly. No significant change in the number of patients seen per day was found in two studies.6,11 Three other studies, one of which used a health maintenance organization (HMO), found that physicians saw fewer patients per day with a student than without one.13,14
Table 3.
Differences in Patient Volume in the Presence of a Trainee
One study showed variable effects on productivity for each medical school class. First-year medical students and third-year clerks in a primary care setting did not cause a significant decrease in patients seen by precepting physicians, while the same program noted decreases of more than eight patients per day when a second-year medical student was in the office.9 Preceptors in this study stated that they decreased their patient number in order to keep up with the educational needs of the clerkship.
Finally, one internal medicine study found an increase of 1.5 patients per day while a student was present.3 This program used a number of physicians who were experienced in teaching students in the office.
Results varied among similar sites as well. For example, 22 practices in a newly formed primary care clerkship had no decrease in the number of patients seen,6 while a similar clerkship, formed about the same time, had decreases in patient productivity as noted above (G.A. Doyle and C. Patricoski, submitted for publication).
A subgroup analysis of one study 6 reveals interesting findings. Although the overall number of patients seen in this clerkship was not statistically different whether a student was present or not, there were significant differences among the various specialties of the precepting physicians. When a student was present, there was an increase of three patients per day in pediatricians’ offices, no change in internal medicine offices, and a decrease of two patients per day in family practice offices.
Both studies involving HMOs showed decreases in the number of patients seen while a student was present.9,13
In summary, we found that some physicians see fewer patients while teaching students, and there may be significant differences in patient productivity among the primary care specialties. The range of reported decreases was large, but the average is most likely about two patients per day. A student's effect on patient productivity may be magnified in offices in which managed care has a large role.
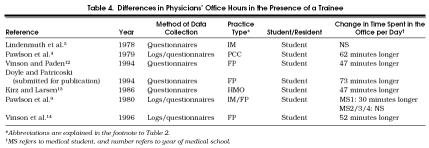
Time Costs
Another important and measurable effect of the presence of a trainee on physicians’ daily schedules is the increase in time spent in the office while teaching (Table 4). Seven studies measured extra time spent in the office when teaching students (G.A. Doyle and C. Patricoski, submitted for publication).3,4,9,12–14 No studies of this type have evaluated residents’ outpatient experiences.
Table 4.
Differences in Physicians’ Office Hours in the Presence of a Trainee
Six of the seven studies showed increases in time spent in the office (range 30 –73 minutes per day). The one study that did not show a significant change in time was based on an aforementioned internal medicine office where more patients were seen in the presence of a student.3
The extra office time was usually added at the end of the day, the beginning of the day, or during lunch. Some physicians also described a work day that was usual in duration, but they taught students during the day at times when they would usually have time to themselves, e.g., reading or “development” time.12–14 Most physicians reported that they did not resent having students despite the increase in effort required; most physicians who have been surveyed continue to teach because they enjoy the experience.13,15
In summary, physicians’ days are generally longer when they are precepting students, but most do not mind the extra time in the office.
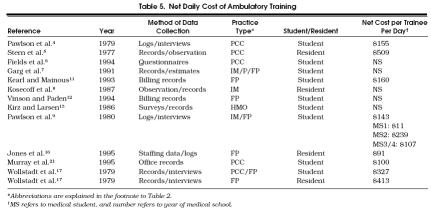
Net Costs
A number of investigators, using various calculations, have attempted to determine a dollar cost for all combined aspects of ambulatory training.6–9,11–13,16–21 Of the 13 studies listed (Table 5), 9 measured student costs alone while 4 measured only resident costs. The practice types vary, but most were family practice or multispecialty primary care offices.
Table 5.
Net Daily Cost of Ambulatory Training
Three recent studies showed no significant net cost to teach a student in the office.6,11,12 A fourth study, which also calculated a zero net cost for resident training,8 took place in an internal medicine practice. All other studies showed significant costs for the training of both students and residents.
After converting each of the three types of cost (decreased billing, decreased patient volume, and increased office hours) into a net dollar cost per day for a physician to teach one student or resident in the office, we found that daily costs ranged from $11 to $509. The study that measured a net cost of $11 daily was based on offices where first-year medical students were present as observers only, and preceptors explained that they did not consciously alter their schedules while the student was present. On the other end of the range, the study that found a cost of $509 described a family practice program with small numbers of residents.
Studies that measured the costs of students who provide meaningful patient care (above the level of an observer) showed costs ranging from $100 to $327 per day, with an average of $113. The range for resident costs was slightly larger, from $91 to $509 per day, with an average of $253. Therefore, there seems to be a real and measurable net cost to a practice to train residents and students in the office.
Benefits from Teaching
In order to accurately measure and calculate cost, any possible benefit gained by the teaching site as a result of the presence of a trainee should be added back. Patient screening, performance of simple procedures or phlebotomy, and assistance in documentation are a few of the benefits cited in the literature. Only one study attempted to assign a dollar value for these benefits and included it in the final cost calculation.8
Discussion
This review of selected studies about the cost of ambulatory education suggests that teaching physicians’ billed charges do not change considerably when students or residents are present. Although some physicians do see fewer patients while teaching students, there may be differences among specialties and types of practice. These findings are most likely due to teaching physicians working more hours while precepting. Teaching offers benefits to teaching physicians, most of which are subjective advantages related to job satisfaction and continuing education. The studies evaluating the cost of ambulatory education are not consistent, but suggest true costs of between $100 and $200 per day for a student and between $200 and $300 per day for a resident.
The literature on the net financial cost of outpatient education brings to light a few important points. First, only a limited number of careful studies have measured the costs of ambulatory education in a systematic manner. Most of the studies were done on student sites, only a few of them measured resident costs, and studies done in family practice offices outnumbered studies of internists’ offices. As ambulatory education expands and the use of internal medicine offices as teaching sites for both students and residents becomes more prevalent, there will be a need to study these sites better to determine the financial burden of training there.
Many different types of ambulatory training sites are currently used for outpatient education, and most are included in this review. The sites range from academic hospital-based offices to community hospital clinics to rural solo practitioners’ offices to HMOs. These different types of sites may face widely varying costs, and each of these costs may have a different effect on an overall cost calculation. For instance, a rural office might pay a student a stipend or house a resident for a month, while a teaching hospital might incur more overhead costs such as purchasing extra books for the various sites or setting up library privileges for private physicians.
One approach to incorporating these variables into an overall estimate of the cost of ambulatory education has been proposed by Boex et al.,10 in a report to the Bureau of Health Professions. This model divides costs into direct costs, indirect costs, and infrastructure costs, and delineates how each may differ among institutions and practices, and between student and resident education. To put all of the variables listed in Table 1 into a cost equation would be an even greater undertaking. Some of the earlier studies attempted to calculate overall costs using similar equations.
In contrast, we focused on three basic costs—billing, patient numbers, and time costs—for two reasons. First, most of the studies in this review reported one or more of these variables as the primary outcome of the study. Second, we feel that these three outcomes are good indicators of the overall financial burden to a practice to train a student or resident in the office. As private offices are used more widely, these data may better inform practicing physicians of the actual teaching costs they face.
In terms of resident costs, our findings seem contrary to conventional wisdom concerning the costs of teaching a resident in the office. It is generally felt that, although interns are costly to train in the office setting, third-year residents are efficient enough to at least offset their cost. There may be a number of reasons for our contradictory results. First, we did not delineate cost according to year of residency; thus, the conventional belief may, in fact, hold true, although the literature we reviewed did suggest that residents were more expensive than medical students. Another reason may relate to differences in training between family practice and internal medicine residencies. Although resident sites in some family practice programs continue to break even financially, we found that internal medicine resident sites continue to have an overall net cost. In addition, family practice physicians in this review generally saw their own patients while precepting, but internal medicine physicians teaching residents did not, which may account for more revenue loss by the internal medicine physicians. The new Medicare Teaching Physician Rule requires that supervising faculty not see their own patients while serving as outpatient attending physicians.22
A number of other reasons have been cited for residents’ low billed charges in internal medicine offices. Residents usually see fewer patients than do faculty attending physicians. The Teaching Physician Rule, which governs the interaction of attending physicians in residents’ practices, disallows billing if the teaching physician has not had a significant interaction with the patient for the “key portion” of the encounter with limited exceptions. Finally, there may be differences according to the usual population of a resident's clinic, for example, more uninsured and Medicare or Medicaid patients.21 Although this might not affect billing, there may be an effect on collections, a cost that has not been studied carefully.
The wide billing differences found by Garg et al. among different specialties,7 and the limited number of studies in internal medicine offices throughout this review, underscore the need for more studies of this type, especially in internists’ offices, where costs might not be comparable to those in pediatricians’ or family practitioners’ offices.
Patient productivity was studied only for student sites. Again, this may be in part due to the organization of residents’ outpatient education, namely, that many resident clinics are hospital-based and the precepting physicians do not see their own patients simultaneously.
No firm correlation seems to exist between patient volumes and the teaching maturity of the preceptors at similar sites in these reports (G.A. Doyle and C. Patricoski, submitted for publication).6 Also, productivity cannot be compared easily between clerkships that are organized in a block fashion and those that use continuous ambulatory experiences.
We also found that significant differences exist among pediatrics, internal medicine, and family practice in terms of patient volume. The reason is unclear, but the finding suggests that costs measured in other primary care settings may not be valid surrogates of similar costs in internal medicine offices.
Overall, patient volumes varied widely, and the reason for this variation is likely to be multifactorial. The strongest correlation we noted was in non–university-based HMOs. All three clerkships that used these sites showed decreases in patient volumes.9,13 This could be a reflection of time constraints in HMOs, of fewer HMO physicians extending their work days, or a combination of these and other factors.
The primary way in which teaching physicians compensate for expected losses of revenue is by working longer, and this fact is consistent with the findings that they enjoy the experience despite the commitment and possible loss of revenue. Although it is difficult to place a dollar value on this time for any particular physician, the time costs are real and significant, averaging 37 minutes per day in the studies in this review.
Different investigators have used varying methods to produce a “net cost” for outpatient education. Differences in the organization, structure, and size of programs, as well as the duties and role of the teaching physician (e.g., whether the physician is seeing patients independently while teaching, the extent of patient interaction while teaching) have added to the variability in these results.
It is likely that a practice involved in ambulatory education faces a dollar cost per day of between $100 and $200 to teach a student and between $200 and $300 to teach a resident. These numbers do not delineate year of residency, and it has been shown that resident costs per visit decrease after the first year of residency.8 In addition, all resident studies in this review measured cost in a hospital-based clinic, where teaching physicians did not see patients simultaneously. No study was done of residents in private offices, where physicians who teach students also see patients. It is likely that non–hospital-based teaching physicians could generate revenue while they are teaching residents.
The implications of our findings are threefold. From an educational standpoint, there needs to be a reassessment of the value of the office setting for the training of students and residents. Indeed, only a few of the reports we reviewed allude to, and none has studied extensively, the educational implications of expanding into the community. As graduate and undergraduate medical education programs rely more heavily on ambulatory offices for medical education, there needs to be assurance that preceptors do not sacrifice the educational goals of the trainee for the service goals of the practice.
From a policy standpoint, these data suggest that there needs to be a reassessment of the distribution of medical education funds. Namely, Medicare payments for residents, which are currently based principally on inpatient service, should reflect the increasing percentage of time the resident is present in the outpatient setting. Adequate financing of graduate education is critical.
From a research standpoint, the paucity of careful studies of this type and the even greater lack of studies in internists’ offices make it clear that more research is needed in the area of outpatient educational costs. As outpatient medical education changes and expands, the internal medicine community will respond to these changes and evaluate their effect on the finances of teaching in the office.
REFERENCES
- 1.Fallon HJ. Residency reform: a perspective from the association of professors in medicine. Ann Intern Med. 1992;116:1041, 1076–9. doi: 10.7326/0003-4819-116-12-1041. (12 pt 2): [DOI] [PubMed] [Google Scholar]
- 2.Association of Professors in Medicine Ambulatory education: expanding undergraduate experience in medical education—a CDIM commentary. Am J Med. 1995;99:111–5. doi: 10.1016/s0002-9343(99)80128-4. [DOI] [PubMed] [Google Scholar]
- 3.Lindenmuth NW, Stone AW, Donaldson M. The effect of third-year clinical clerks on physician productivity in a primary care practice. J Med Educ. 1978;53:357–9. doi: 10.1097/00001888-197804000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Pawlson LG, Schroeder SA, Donaldson M. Medical student instructional costs in a primary care clerkship. J Med Educ. 1979;54:551–5. doi: 10.1097/00001888-197907000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Stern RS, Jennings M, Delbanco T, et al. Graduate education in primary care. N Engl J Med. 1977;297:638–43. doi: 10.1056/NEJM197709222971205. [DOI] [PubMed] [Google Scholar]
- 6.Fields SA, Toffler WL, Bledsoe NM. Impact of the presence of a third-year medical student on gross charges and patient volumes in 22 rural community practices. Acad Med. 1994;69:S87–9. doi: 10.1097/00001888-199410000-00052. [DOI] [PubMed] [Google Scholar]
- 7.Garg ML, Boero JF, Christiansen RG, Booher CG. Primary care teaching physicians’ losses of productivity and revenue at three ambulatory-care centers. Acad Med. 1991;66:348–53. doi: 10.1097/00001888-199106000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Kosecoff J, Brook RH, Fink A, et al. Providing primary general medical care in university hospitals: efficiency and cost. Ann Intern Med. 1987;107:399–405. doi: 10.7326/0003-4819-107-2-399. [DOI] [PubMed] [Google Scholar]
- 9.Pawlson LG, Watkins R, Donaldson M. The cost of medical student instruction in the practice setting. J Fam Pract. 1980;10:847–52. [PubMed] [Google Scholar]
- 10. Boex JR. Defining the cost structure of ambulatory training. A report to the Bureau of Health Professionals. March 1996.
- 11.Kearl GW, Mainous AG. Physicians’ productivity and teaching responsibilities. Acad Med. 1993;68:166–7. doi: 10.1097/00001888-199302000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Vinson DC, Paden C. The effect of teaching medical students on private practitioners’ workloads. Acad Med. 1994;69:237–8. doi: 10.1097/00001888-199403000-00020. [DOI] [PubMed] [Google Scholar]
- 13.Kirz HL, Larsen C. Cost and benefits of medical student training to a health maintenance organization. JAMA. 1986;256:734–9. [PubMed] [Google Scholar]
- 14.Vinson DC, Paden C, Devera-Sales A. Impact of medical student teaching on family physicians’ use of time. J Fam Pract. 1996;42(s2):243–9. [PubMed] [Google Scholar]
- 15.Christiansen RG, Wark K, Levenstein JP. Attitudes of part-time community internal medicine faculty about their teaching. Acad Med. 1992;67:863–4. doi: 10.1097/00001888-199212000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Jones TF, Culpepper L, Shea C. Analysis of the cost of training residents in a community health center. Acad Med. 1995;70:523–31. doi: 10.1097/00001888-199506000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Wollstadt LJ, Boyd GE, Gaumer G, et al. Resource requirements for teaching continuity in primary care. J Fam Pract. 1979;9:1065–71. [PubMed] [Google Scholar]
- 18. Institute of Medicine. Report of a Study. Primary care physicians: financing their GME in ambulatory settings, Washington, DC, 1989.
- 19.Diamond HS, Fitzgerald LL, Day R. An analysis of the cost and revenue of an expanded medical residency. J Gen Intern Med. 1993;8:614–8. doi: 10.1007/BF02599717. [DOI] [PubMed] [Google Scholar]
- 20.Gavett JW, Mushlin AI. Calculating the costs of training in primary care. Med Care. 1986;24:301–12. doi: 10.1097/00005650-198604000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Murray E, Jinks V, Modell M. Community-based medical education: feasibility and cost. Med Educ. 1995;29:66–71. doi: 10.1111/j.1365-2923.1995.tb02804.x. [DOI] [PubMed] [Google Scholar]
- 22. Medicare program: revisions to payment policies and adjustments to the relative value units under the physician fee schedule for calendar year 1996. 60 Federal Register—62124. [PubMed]
- 23.Lee D, Nugent G. Costs associated with ambulatory care and education. Acad Med. 1989;64(2):S44–50. doi: 10.1097/00001888-198910000-00025. [DOI] [PubMed] [Google Scholar]
- 24.Xakellis GC, Gjerde CL. Ambulatory medical education: teachers’ activities, teaching cost, and residents’ satisfaction. Acad Med. 1995;70:702–7. doi: 10.1097/00001888-199508000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Roy PJ. Four myths about using med students. Med Econ. 1995:165–6. [PubMed] [Google Scholar]
- 26.Burg FD, Kelley MA, Zervanos NJ. Supporting primary care medical education. J Gen Intern Med. 1994;9(1):S104–14. doi: 10.1007/BF02598125. [DOI] [PubMed] [Google Scholar]
- 27.Schneeweiss R, Ellsbury K, Hart G, et al. The economic impact and multiplier effect of a family practice clinic on an academic medical center. JAMA. 1989;262:370–5. [PubMed] [Google Scholar]