Abstract
Adaptation of field isolates of foot-and-mouth disease virus (FMDV) to grow in cells in culture can result in changes in viral properties that include acquisition of the ability to bind to cell surface heparan sulfate (HS). After 13 passages on BHK cells to produce a vaccine, a Cathay topotype isolate of FMDV serotype O from China (O/CHA/90) extended its cell culture host range and bound to heparin-Sepharose, although it did not require cell surface HS as a receptor molecule. To understand these phenomena, we constructed chimeric viruses by using a type A12 infectious cDNA and the capsid protein-coding regions of O/CHA/90 and its cell culture-adapted derivative (vac-O/CHA/90). Using a set of viruses derived from these chimeras by exchanging portions of the capsid-coding regions, we discovered that a group of amino acid residues that surround the fivefold axis of the icosahedral virion determine host range in cell culture and influence pathogenicity in pigs. These residues included aromatic amino acids at positions 108 and 174 and positively charged residues at positions 83 and 172 in protein 1D. To test if these residues participated in non-integrin-dependent cell binding, the integrin-binding RGD sequence in protein 1D was changed to KGE in two different chimeras. Evaluation of these KGE viruses indicated that growth in cell culture was not dependent on HS. One of these viruses was tested in pigs, where it produced a mild disease and maintained its KGE sequence. These results are discussed in terms of receptor utilization and pathogenesis of this important pathogen.
Foot-and-mouth disease (FMD) is a highly contagious viral disease of cloven-hoofed animals, most notably cattle, pigs, and sheep. Although it was the earliest described viral disease of animals, FMD remains one of the most important infectious diseases of animals, as evidenced by costly outbreaks in Taiwan (1997), Japan (2000), the Republic of Korea (2000 and 2002), the United Kingdom (2001), The Netherlands (2001), and France (2001). FMD control in areas of endemicity is implemented by regular vaccination, utilizing an inactivated vaccine product that is produced on an enormous scale from chemically inactivated preparations of FMD virus (FMDV) propagated in baby hamster kidney (BHK) cells. The successful application of this vaccine has contributed to the eradication of FMD from several regions of the world, including the European Union in the 1980s and Uruguay, Argentina, and the south of Brazil in the 1990s. One of the major factors affecting FMD vaccine efficacy is antigenic variation during production of the viral antigen. Specifically, antigenic variants of the virus are readily selected during propagation in cell culture. Thus, it is important for manufacturers to rigorously check vaccine strains in order to maintain vaccine antigen quality.
FMDV exists in seven serotypes (O, A, C, Asia1, SAT1, SAT2, and SAT3) which, along with equine rhinitis A virus, constitute the Aphthovirus genus of the family Picornaviridae. The FMDV virion consists of an icosahedral shell composed of 60 copies each of four structural proteins, 1A to 1D, surrounding a single-stranded, positive-sense RNA. Multiple antigenic sites have been located on the capsid of the virus, and several of these consist of conformational epitopes made up of portions of more than one capsid protein (4, 7, 8, 14, 29, 43, 54). As with other RNA viruses, FMDV isolates exist as quasispecies. Thus, each viral isolate contains a mixture of genomes (16), allowing for the rapid selection of variants upon changes in environment. Selection of variants with more fit genomes from FMDV populations can occur during infection of animals or propagation in cell culture.
The molecular basis of binding of FMDV to its cellular receptor has been elucidated by multiple approaches (5, 20, 35, 42). These studies indicate that naturally occurring isolates of the virus appear to bind to cells via a highly conserved (46), surface-exposed arginine-glycine-aspartic acid (RGD)-containing loop in capsid protein 1D (37). Further, a variety of approaches have indicated that this loop interacts with one or more of the RGD-binding integrins, including integrins αvβ3 (44), αvβ6 (28), and αvβ1 (27). However, FMDV can also enter cells through non-integrin-mediated pathways. For example, antibody-complexed virus can enter cells that express the Fc receptor (6, 40), or it can enter cells through a genetically engineered receptor containing portions of a virus-binding antibody (42). In addition, cell culture-adapted virus can use heparan sulfate (HS), a cell surface glycosaminoglycan (GAG), as a receptor in order to enter cells (26, 48). Furthermore, Domingo and coworkers have reported data showing that derivatives of a type C virus passaged 100 times in cell culture appear to use multiple receptors, which could include molecules that are neither integrins nor HS (2, 3, 39).
Among the seven serotypes of FMDV, serotype O is the most prevalent worldwide (49). Within the serotype O viruses there are multiple topotypes that have had considerable economic impact. One of these, the PanAsian topotype, was responsible for the costly outbreak in the United Kingdom in 2001 (32). Another topotype, the Cathay topotype, includes the virus responsible for the catastrophic outbreak in Taiwan in 1997, which crippled Taiwan's pork industry (55). The 1997 Taiwanese isolate has an interesting host range restriction in that it affects pigs but not cattle (17). It has recently been shown that the molecular basis for this altered host range is the presence of an altered 3A protein in the virus (9). In addition, it has been shown that Cathay topotype isolates with this altered 3A coding region have been circulating in Southeastern Asia for more than 30 years (31).
Here we present studies on a member of the Cathay topotype of FMDV that was isolated in an outbreak on a pig farm of ShenZhen, Guangdong Province, China, in 1990 (referred to as O/CHA/90) (44a). O/CHA/90 was adapted to grow in BHK cells in the early 1990s for use in preparation of an inactivated vaccine to help control FMD along the borders of China. During adaptation, a derivative was obtained (referred to here as vac-O/CHA/90) that was shown to differ from the parental strain by a reduced ability to kill suckling mice, despite high infectivity in BHK cells. As a result of these altered properties, vac-O/CHA/90 was removed from use as a vaccine strain. Genetic and biochemical studies on O/CHA/90 and vac-O/CHA/90 and their genetically engineered derivatives indicate that substitutions surrounding the pore at the fivefold axis of the virus's icosahedral shell allow vac-O/CHA/90 to extend its tissue culture host range. This site included two aromatic amino acid residues and two positively charged residues in viral capsid protein 1D. Interestingly, unlike many previously reported tissue culture-adapted derivatives of FMDV, derivatives of vac-O/CHA/90 appear to replicate in cell culture in a manner that does not appear to require either electrostatic binding to HS or RGD-mediated binding to integrins. Furthermore, a virus engineered to contain KGE substituted for the RGD was able to cause disease in pigs.
MATERIALS AND METHODS
Viruses.
An isolate of FMDV was obtained from a diseased pig in China in 1990 by the Lanzhou Veterinary Research Institute, Gansu, China (44a). Following 1 passage in an experimentally infected pig, this virus was passaged twice in BHK cells at the Plum Island Animal Disease Center as described below. This BHK passage-2 virus is referred to below as O/CHA/90. The same pig-passaged material was also passaged 3 times in suckling mice, 13 times in monolayer cultures of BHK cells at the Lanzhou Institute, and 1 additional time in monolayer cultures of BHK cells at the Plum Island Animal Disease Center. This virus, which represents a virus originally intended for use as an antigen in an inactivated commercial FMD vaccine (see the introduction), is referred to below as vac-O/CHA/90.
Cell lines and plaque assays.
BHK cells, strain 21, clone 13 (passage level 60 to 70), were grown in Eagle's basal medium containing 10% bovine calf serum (HyClone, South Logan, Utah), 10% tryptose phosphate broth, antibiotics and an antimycotic agent (47). Chinese hamster ovary (CHO) cell lines with defined GAG expression patterns (K1, S745, and pgsD-677) (19, 36) were maintained in Ham's F-12 medium supplemented with 10% fetal calf serum (HyClone), antibiotics, and an antimycotic agent as previously described (45). Plaque assays were performed using a tragacanth overlay and crystal violet staining (0.3% in Histochoice; Amresco, Solon, Ohio) by a slight modification of previously described techniques (47). All tissue culture reagents were from Life Technologies, Gaithersburg, Md., unless otherwise noted. Virus titers were determined on BHK cells and are expressed as PFU per milliliter unless otherwise noted. When plaque assays were performed following treatment with peptide-containing solutions, the monolayers were rinsed briefly with phosphate-buffered saline, pH 6.0, to inactivate unadsorbed viral particles prior to overlay and incubation as described above.
RNA isolation, cDNA synthesis, PCR amplification, and sequencing.
RNA was extracted from culture fluids harvested from infected cells or infected animal vesicular fluids by using TRIzol LS (Life Technologies). Long viral cDNAs were then synthesized from these viral RNAs as previously described (41). Briefly, viral cDNAs were synthesized with Superscript II polymerase (Life Technologies) by using random hexamers or specific oligonucleotide primers (P500, GACATGTCCTCCTGCATCTG; P15, GGCGGCCGCTTTTTTTTTTTTTTT;P287, CGTGCCTAGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGGTGAAAGGCGG) and were amplified by a PCR using Herculase polymerase (Stratagene, La Jolla, Calif.). Amplicons containing the 5′ ends of viral cDNAs were obtained by amplification of homopolymer-tailed cDNAs (21). Following amplification, the cDNA fragments were purified from agarose gels with Qiagen columns (Valencia, Calif.) and sequenced by use of selected primers and asymmetric amplification with Big-Dye terminators (Perkin-Elmer Applied Biosystems Inc. [ABI], Foster City, Calif.), followed by resolution on an ABI 3700 or 3100 sequencer.
Construction of chimeric viruses between A12 and O/CHA/90 or vac-O/CHA/90 capsid sequences.
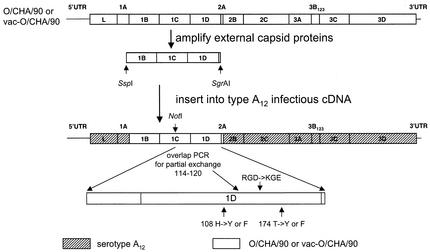
Capsid-encoding regions of O/CHA/90 and vac-O/CHA/90 were amplified by PCRs utilizing oligonucleotide P510 (CCCAAATATTGACTACCCGCAACGGACAC), which had been engineered to add an SspI site by silent mutation at the highly conserved sequence at codons 13 to 15 of protein 1B (amino acid sequence RIL; codons CGa ATa tTg, where lowercased letters represent altered bases), and oligonucleotide P557 (ACGTCACCGGCGAGCTTGAGGAGGTCGAAG), containing an SgrAI site added by silent mutation at the highly conserved sequence at codons 9 to 12 of protein 2A (amino acid sequence LAGD; codons CTc GCc GGt GAC, where lowercased letters represent altered bases) (see Fig. 1). Following digestion with these endonucleases, the amplified fragments were inserted into a serotype A12 cDNA vector derived from the type A12 plasmid pRMC35 as previously described (41). This vector contains a T7 promoter sequence in front of a hammerhead ribozyme at the start of the FMDV genome which terminates with a poly(A) tract of 15 residues followed by a hepatitis delta virus ribozyme (41). Chimeras containing different portions of the capsid regions of the various derivatives were created by routine subcloning procedures utilizing the two sites listed above and a naturally occurring NotI restriction site at codons 138 to 140 (GCG GCC GCA) in the coding regions of 1C (see Fig. 1). Additional chimeras were generated by overlap PCR fusion, carried out by mixing PCR-amplified fragments from different parental clones, reamplifying through the product of the fusion of these two fragments (24), and then digesting and cloning into the sites listed above (see Fig. 1). PCR site-directed substitutions of Y and F codons for H and T codons at 1D codons 108 and 174, respectively, and substitution of codons specifying KGE for the natural RGD codons 145 to 147 of 1D, were accomplished by standard techniques (24) (Fig. 1; Table 4). In all cases, the resulting cDNA clones were sequenced through the entire amplified regions to confirm that they contained the expected modification without any unwanted amplification-associated substitutions.
FIG. 1.
Schematic diagram showing strategy for construction of chimeric viruses used to evaluate the genetic basis of differences between O/CHA/90 and vac-O/CHA/90. The top portion of the figure indicates the position of the amplicon containing proteins 1B, 1C, and 1D on the type O genomes. The bottom portion of the figure shows the general structure of the chimeras generated with serotype A12 virus, including the positions of the NotI restriction endonuclease site and overlap PCR primers used to swap fragments of P1, as well as the positions altered by site-directed mutagenesis (108H→Y or F, 174T→Y or F, 145RGD147→KGE).
TABLE 4.
Comparison of sequences of intra-P1 chimeric cDNA plasmids, sequences of the viruses recovered from these cDNAs, and in vitro properties of these viruses
| Virusa | Residue in protein:
|
Titer (PFU/ml) in the following cell line:
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1B
|
1C
|
1D
|
|||||||||||||
| 78 | 130 | 195 | 30 | 200 | 83 | 108 | 142 | 171 | 172 | 174 | BHK21 | CHOK1 | CHO677 | CHO745 | |
| VpF1 | C | Y | P | F | I | E/Kb | H | N | T | R | T | 5.0 × 107 | <5 | <5 | <5 |
| VpF1YY | C | Y | P | F | I | E/K | Y | N | T | R | Y | 1.7 × 107 | 1.9 × 104 | 1.3 × 105 | 2.1 × 105 |
| VpF1FF | C | Y | P | F | I | E/K | F | N | T | R | F | 2.5 × 108 | 2.0 × 104 | 2.0 × 105 | 1.4 × 105 |
| VpF1B1 | C | Y | P | F | V | K | Y | S | P | R | F | 7.5 × 107 | 1.2 × 105 | 1.9 × 106 | 2.0 × 106 |
| VpF1B2 | C | Y | P | F | V | K | Y | S | T | R | Y | 1.2 × 108 | 6.0 × 105 | 7.6 × 106 | 9.5 × 106 |
| VpB1 | C | Y | L | L | V | K | Y | S | P | R | F | 1.6 × 108 | 5.7 × 104 | 1.2 × 106 | 4.7 × 106 |
| VpB1F1 | C | Y | L | L | I | E/K | H | N | T | R | T | 2.9 × 107 | <5 | <5 | <5 |
| VpB1B2 | C | Y | L | L | V | K | Y | S | T | R | Y | 4.5 × 107 | 7.0 × 104 | 6.0 × 105 | 1.4 × 106 |
| VpB2 | Y | C | P | F | V | K | Y | S | T | R | Y | 1.85 × 108 | 4.2 × 105 | 3.7 × 106 | 1.5 × 107 |
| VpB2F1 | Y | C | P | F | I | E/K | H | N | T | R | T | 2.7 × 107 | <5 | <5 | <5 |
| VpB2B1 | Y | C | P | F | V | K | Y | S | P | R | F | 3.25 × 107 | 1.5 × 105 | 3.5 × 106 | 1.8 × 106 |
| VpB2B2F1 | Y | C | P | F | V | K | Y | N | T | R | T | 1.1 × 108 | <5 | <5 | <5 |
| VpB2F1B2 | Y | C | P | F | I | E | H | S | T | R | Y | 1.3 × 107 | <5 | <5 | <5 |
Virus names are derived from plasmid names, except for plasmids with names including FF and YY, which were produced by site-specific mutagenesis at positions 108 and 174 (see Fig. 1 and the text for construction methodology). Sequence data from the recovered viruses were identical to the sequences of their plasmids of origin, except where indicated at position 83 of protein 1D (see footnote b). Portions of viruses shown in boldface are derived from pF1. Portions of viruses in plain roman type are derived from pB1. Portions of viruses shown in italics are from pB2. Amino acids altered by site-directed mutagenesis are underlined.
E/K, original plasmid encoded an E residue at this position, but the virus recovered from BHK cells displayed a mixture of codons for E and K.
In vitro RNA synthesis and transfection.
Plasmid DNAs containing genome-length cDNAs were linearized at the SwaI site following the poly(A) tract, hepatitis delta ribozyme, and T7 terminator and were used as templates for RNA synthesis by using a MegaScript T7 kit (Ambion, Austin, Tex.) according to the manufacturer's instructions. BHK cells were transfected with these synthetic RNAs by using electroporation (Electrocell Manipulator 600; BTX Corp., San Diego, Calif.) as previously described (41). In some cases, viruses were recovered from BHK cells cotransfected (by using LIPOFECTAMlNE PLUS reagent [Life Technologies]) with a mixture of plasmid DNA containing a genome-length cDNA and a plasmid containing a cytomegalovirus-driven bacteriophage T7 polymerase (41). Viruses were passed two or three times on 35-mm-diameter BHK cell monolayers, by using 1/10 of the harvest of previous passages, prior to amplification on 75- to 175-cm2 BHK cell monolayers. Viruses from the last passage were sequenced through P1 (as described above) to determine if they had maintained the cDNA-encoded sequence.
Heparin-Sepharose binding assays.
Viruses were assayed for their abilities to bind to heparin-Sepharose (Amersham Pharmacia Biotech, Piscataway, N.J.) as previously described (48). Data are expressed in terms of the percentage of virus that was retained by heparin-Sepharose under normal physiological salt and buffering conditions.
Pig inoculations.
Porcine inoculation studies were performed by a modification of the method of Burrows (11). Briefly, following administration of an anesthetic, two 50- to 60-lb pigs were intradermally inoculated at two sites (in the bulb-heel of inner and outer main digits) on each foot with a series of 10-fold dilutions of virus estimated to contain from 102 to 105 PFU/site in 5 μl of tissue culture medium (11). Following inoculation, titers of the dilution series were redetermined, and the aggregate doses for all inoculations are reported in the figure legends. For the next 3 to 7 days, animals were carefully scored for appearance of lesions at inoculation sites and at other sites. Lesion scores were based on the number of sites affected that were distinct from actual injection sites. Scores were calculated as follows: one point for each affected digit, one point for a vesicle(s) on the tongue, one point for a vesicle(s) on the snout, and one point for a vesicle(s) on the lower lip, for a maximum lesion score of 19. The virus in the blood was titered in multiwell plates by standard methods to determine the amount of virus present (expressed as 50% tissue culture infective doses per milliliter), and viral RNA was extracted from vesicular fluid (collected on selected days), reverse transcribed, and sequenced through the entire P1 region as described above.
RESULTS
Genomic sequence analyses of O/CHA/90 and vac-O/CHA/90.
Sequence data were collected from the complete genomes of O/CHA/90 and its derivative developed for use as a vaccine in China (designated vac-O/CHA/90 [see Materials and Methods]). Although these analyses revealed multiple sites where differences were detected between the “majority” populations (Table 1), careful inspection of the electropherograms from the sequencing reactions revealed genetic heterogeneity, as expected from the quasispecies nature of the FMDV genome (see the introduction). Table 1 shows the 22 changes detected at the nucleic acid level, of which 16 resulted in changes in the encoded amino acids (both numerical values include shifts between mixtures and “pure” populations; see Table 1). Evaluation of the changes in the noncoding regions of the genome revealed that none of these changes were expected to alter the secondary structural elements of the viral RNA (data not shown). The six differences detected in the coding regions for the nonstructural proteins also appeared to be unlikely to influence adaptation to cell culture; therefore, we concentrated on changes observed in the capsid-encoding regions (see below). Interestingly, among the 10 differences detected in the capsid-encoding region, 8 were predicted to be on the external surface of the virion based on the three-dimensional structure of O1 BFS (37). Four of these residues were located surrounding the pore at the fivefold axis of the viral particle (residue 83 in protein 1D [1D/83], 1D/108, 1D/171, and 1D/174), and four could be expected to modulate the structure of the RGD-containing G-H loop of protein 1D (1B/78, 1B/130, 1B/132, and 1D/142) (see Table 1).
TABLE 1.
Comparison of the sequences of the complete genomes of O/CHA/90 and vac-O/CHA/90a
| Nucleotide no. | Regionb | O/CHA/90
|
vac-O/CHA/90
|
||||
|---|---|---|---|---|---|---|---|
| Nucleotidec | Codond | Amino acide | Nucleotidec | Codond | Amino acide | ||
| 466 | PK region | R | G | ||||
| 626 | IRES | A | G | ||||
| 1891 | 1A/78 | U | ggU | G | Y | ggY | G |
| 2145 | 1B/78 | G | uGc | C | R | uRc | C/Y |
| 2301 | 1B/130 | R | uRu | Y/C | R | uRu | Y/C |
| 2306 | 1B/132 | R | Ruc | I/V | A | Auc | I |
| 2654 | 1C/30 | U | Uuc | F | Y | Yuc | F/L |
| 3164 | 1C/200 | A | Auu | I | R | Ruu | I/V |
| 3474 | 1D/83 | G | Gag | E | A | Aag | K |
| 3548 | 1D/108 | C | Cac | H | U | Uac | Y |
| 3651 | 1D/142 | R | aRc | N/S | G | aGc | S |
| 3737 | 1D/171 | A | Acc | T | W | Wcc | P/T |
| 3746 | 1D/174 | A | Acu | T | U | Ucu | Y |
| 3747 | 1D/174 | C | aCu | T | W | uWu | F |
| 4301 | 2B/129 | Y | Yug | L | U | Uug | L |
| 4652 | 2C/95 | G | Gcu | A | A | Acu | T |
| 4918 | 2C/185 | G | acG | T | R | acR | T |
| 5211 | 2C/383 | U | aUg | M | A | aAg | K |
| 5326 | 2C/421 | A | aaA | K | R | aaR | K |
| 6119 | 3C/50 | G | Gag | E | C | Cag | Q |
| 8095 | 3′UTR | G | U | ||||
| 8110 | 3′UTR | A | U | ||||
Numbering is based on a complete genome of 8,129 bases, including 15 C residues and 15 A residues inserted for an unknown number of bases in the poly(C) and poly(A) regions.
PK, pseudoknot; IRES, internal ribosomal entry site; UTR, untranslated region.
R = A or G; Y = C or U; W = A or U.
Lowercase letters represent bases shared by the two viruses, and capital letters represent bases that differ between the two viruses.
One-letter code of the encoded amino acid residues. Both amino acids are listed in the case of codons that are mixtures.
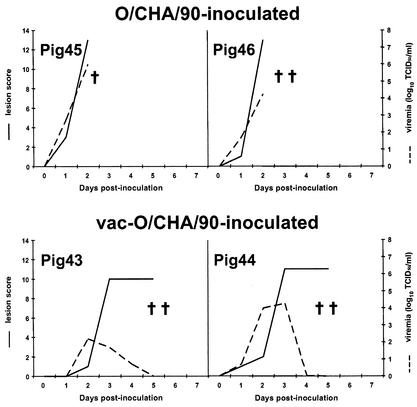
Table 2 shows the biological properties of O/CHA/90, vac-O/CHA/90, and viruses derived from O/CHA/90 and vac-O/CHA/90 by a single passage in pigs. As expected, the cell-adapted virus intended for use as a vaccine exhibited an expanded host range in cell culture and was able to bind to heparin-Sepharose, properties reported several years ago for cell-adapted serotype O1 Campos viruses (45, 48). Interestingly, the tissue culture-adapted Cathay viruses displayed quite different properties from the O1 Campos viruses identified previously (48). Specifically, in the case of the O1 Campos derivatives, adaptation to cell culture was tightly correlated with ability to bind to heparin-Sepharose, and the tissue culture viruses were completely dependent on cell surface HS for infectivity (as evidenced by their inability to grow on CHO cell mutants 677 and 745) (45). However, the cell-adapted Cathay virus, vac-O/CHA/90, was able to bind to heparin-Sepharose but did not require cell surface HS for infectivity, as shown by the ability of this virus to grow in CHO cell lines 677 (36) and 745 (19), in which cell surface GAG expression is defective (Table 2). This discordance is quite striking, and it emphasizes the difference between the heparin-Sepharose binding assay that measures the biophysical properties of the virus and the actual function of cell surface molecules in mediating infection. To ensure that the differences between the Cathay viruses and the O1 Campos derivatives were not a result of the alteration of the cell lines since publication of the earlier work, we confirmed the previously reported phenotype of the cells in culture with the O1 Campos viruses (namely, the ability of heparin-Sepharose-binding viruses to grow in wild-type [WT] but not mutant CHO cells [48]). In addition, the heparin-Sepharose-binding O1 Campos virus (vCRM4 [48]) was routinely incorporated into our experiments to confirm the differences between it and the Chinese viruses described here. In all cases, vCRM4 displayed the expected phenotype, ability to form plaques only in WT, not in mutant, CHO cells. Further, although cell culture adaptation clearly resulted in the acquisition of heparin-Sepharose binding, this binding was not completely reversed when the viruses were passed a single time in pigs (Table 2). Once again, the latter result differed from the results of previous work with O1 Campos, where the virus lost its ability to bind to heparin-Sepharose after a single passage through cattle (48). Interestingly, although vac-O/CHA/90 was able to cause disease in pigs (albeit less severe than the disease caused by O/CHA/90 [Fig. 2 ]), the virus (Vpig43) recovered from one of the pigs inoculated with vac-O/CHA/90 was less able to infect all three types of CHO cells (expressed as a ratio of plaque-forming ability on CHO cells to plaque-forming ability on BHK cells) than the original vac-O/CHA/90 virus (Table 2).
TABLE 2.
P1 amino acid sequences and in vitro properties of O/CHA/90 and vac-O/CHA/90 compared to those of their derivatives recovered from pigs, and sequences of cDNA plasmids created from O/CHA/90 and vac-O/CHA/90
| Virus or plasmid | Residue in protein:
|
Titer (PFU/ml) in the following cell line:
|
% Heparin-Sepharose bindinga | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1B
|
1C
|
1D
|
||||||||||||||
| 78 | 130 | 132 | 195 | 30 | 200 | 83 | 108 | 142 | 171 | 174 | BHK21 | CHOK1 | CHO677 | CHO745 | ||
| O/CHA/90 | C | Y/C | I/V | P | F | I | E | H | N/S | T | T | 2.0 × 107 | <5 | <5 | <5 | 0.2 |
| VPig45b | C | Y/C | I/V | P | F | I | E | H | N/S | T | T | 4.5 × 108 | <5 | <5 | <5 | 0.7 |
| VPig46b | C | Y/C | I/V | P | F | I | E | H | N/S | T | T | 3.5 × 107 | <5 | <5 | <5 | 0.7 |
| pF1c | C | Y | I | P | F | I | E | H | N | T | T | |||||
| vac-O/CHA/90 | C/Y | Y/C | I | P | F/L | I/V | K | Y | S | P/T | Y/F | 7.5 × 107 | 2.6 × 105 | 3.6 × 104 | 4.5 × 105 | 98 |
| VPig43d | C | Y/C | I | P | L | I | K | Y | S | P | F | 4.0 × 107 | 1.6 × 103 | 7.0 × 103 | 1.6 × 104 | 65 |
| VPig44d | C | Y/C | I | P | L | I | K | Y | S | P | F | 6.7 × 107 | 9.2 × 104 | 9.5 × 105 | 5.0 × 105 | 71 |
| pB1e | C | Y | I | P | L | V | K | Y | S | P | F | |||||
| pB2e | Y | C | I | P | F | V | K | Y | S | T | Y | |||||
Percentage of virus that bound to heparin-Sepharose under physiological conditions.
Virus recovered from a vesicular lesion (away from the inoculation site) of an animal inoculated with O/CHA/90.
Sequence data from a single cDNA clone obtained from O/CHA/90.
Virus recovered from a vesicular lesion (away from the inoculation site) of an animal inoculated with vac-O/CHA/90.
Sequence data from two different cDNA clones obtained from vac-O/CHA/90.
FIG. 2.
Comparison of severity of disease induced in pigs by O/CHA/90 (pigs 45 and 46) and vac-O/CHA/90 (pigs 43 and 44). For these experiments, animals 45 and 46 were inoculated intradermally with approximately 140,000 PFU of O/CHA/90 and animals 43 and 44 were inoculated with 140,000 PFU of vac-O/CHA/90 (see Materials and Methods). Solid lines indicate lesion scores, calculated by adding the number of sites away from the inoculation site that were affected by disease (the maximum value achievable was 19 [see Materials and Methods]). Dotted lines indicate the amount of virus detected in the blood. TCID50, 50% tissue culture infective dose. Symbols: †, animal died, apparently due to FMD; ††, animal was euthanized out of humane considerations.
Generation and characterization of genetically engineered FMDVs encoding only the surface-exposed capsid proteins of O/CHA/90 and vac-O/CHA/90.
To help dissect the differences responsible for the altered phenotype of the two viruses, the external portions of the coding region of these viruses were PCR amplified and transferred to the constant genetic background available in our serotype A12 infectious cDNA (see Materials and Methods). For these analyses we selected one cDNA clone (pF1) carrying the capsid coding region of O/CHA/90 and two clones (pB1 and pB2) carrying the capsid coding region of vac-O/CHA/90. Table 2 shows the sequence differences between these two cDNA clones. None of these clones had a nucleic acid sequence that perfectly matched the majority population of the viral isolate it was derived from, although the cDNAs were produced from exactly the same preparation of RNA that was used to sequence the original genomes. These findings are consistent with the quasispecies nature of the FMDV genome (see the introduction) and demonstrate the genetic complexity of the two original isolates (O/CHA/90 and vac-O/CHA/90). Thus, functional analyses of the original isolates at the genetic, biochemical, and biological levels would be severely complicated by this complexity. Therefore, use of cloned viral populations derived either classically (by infection of various substrates with limiting dilutions of the original inoculum) or genetically (by reverse genetic engineering) is required to complete functional genetic analyses.
cDNAs pF1, pB1, and pB2 were used to produce chimeric full-length RNA molecules in vitro, these were introduced into BHK cells, and viruses (designated VpF1, VpB1, and VpB2) were recovered and amplified in BHK cells (see Materials and Methods). Following amplification in BHK cells to produce stocks of virus (passages 3 to 4), the sequences of the P1 regions of these viruses were obtained for comparison to the original cDNAs. Table 3 shows that the viruses derived from cDNAs harboring the P1 region of the vaccine seed virus (VpB1 and VpB2) maintained the sequences encoded by the original chimeric cDNA. On the other hand, the virus recovered from the cDNA molecule obtained directly from the low-passage isolate (VpF1) contained a mixture of codons at position 83 of 1D. This codon, originally encoding a negatively charged E, became a mixture with a codon encoding a positively charged K residue (Table 3). This mixture could be readily separated by binding to heparin-Sepharose. However, the E-containing viruses that remained in the unbound fraction following treatment with heparin-Sepharose readily reverted to an E/K mixture upon a single passage in BHK cells (data not shown), indicating a selective advantage of the positive charge in the BHK cell culture system.
TABLE 3.
Comparison of sequences of P1 chimeric cDNA plasmids, sequences of the viruses recovered from these cDNAs, and the in vitro properties of these viruses as well as the derivatives of these viruses recovered from pigs
| Virus or plasmid | Residue in protein:
|
Titer (PFU/ml) in the following cell line:
|
% Heparin-Sepharose binding | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1B
|
1C
|
1D
|
||||||||||||||
| 78 | 130 | 195 | 30 | 200 | 83 | 108 | 142 | 171 | 172 | 174 | BHK21 | CHOK1 | CHO677 | CHO745 | ||
| pF1 | C | Y | P | F | I | E | H | N | T | R | T | |||||
| VpF1a | C | Y | P | F | I | E/Kb | H | N | T | R | T | 5.0 × 107 | <5 | <5 | <5 | 56 |
| VPig47c | C | Y | P | F | I | E/K | H | N | T | R/Q | T | 4.5 × 107 | <5 | <5 | <5 | 27 |
| VPig48c | C | Y | P | F | I | E/K | H | N | T | R/W | T | 6.5 × 107 | <5 | <5 | <5 | 6 |
| pB1 | C | Y | L | L | V | K | Y | S | P | R | F | |||||
| VpB1 | C | Y | L | L | V | K | Y | S | P | R | F | 1.6 × 108 | 5.7 × 104 | 4.7 × 106 | 1.2 × 106 | 97 |
| VPig470d | C | Y | L | L | V | K | Y | S | P | R | F | 9.0 × 106 | 6.5 × 102 | 2.5 × 105 | 6.5 × 104 | 71 |
| pB2 | Y | C | P | F | V | K | Y | S | T | R | Y | |||||
| VpB2 | Y | C | P | F | V | K | Y | S | T | R | Y | 1.8 × 108 | 4.1 × 105 | 1.5 × 107 | 3.7 × 106 | 82 |
| VPig50e | Y | C | P | F | V | K | Y | S | T | Q | Y | 3.5 × 107 | <5 | <5 | <5 | 4 |
Viruses recovered by transfection of BHK cells with cDNA plasmids are given the designation “V” followed by the plasmid name.
E/K the original plasmid encoded an E residue, but the virus obtained in BHK cells or recovered from pigs displayed a mixture of codons for E and K.
Virus recovered from a vesicular lesion (away from the inoculation site) of an animal inoculated with VpF1.
Virus recovered from a vesicular lesion of an animal that became infected by being placed in contact with an animal inoculated with VpB1.
Virus recovered from a vesicular lesion (away from the inoculation site) of an animal inoculated with VpB2.
Even with this apparent tissue culture adaptation to acquire the K codon at position 83, VpF1 remained unable to infect any of the CHO cells, although it did acquire an ability to bind heparin-Sepharose, a biochemical property that correlated with growth in WT CHO cells (CHO-K1) for tissue culture-adapted O1 Campos viruses (48). VpF1 was also virulent in pigs, although it appeared to be less virulent than the parental virus O/CHA/90 (compare Fig. 2 and 3). Interestingly, upon passage of VpF1 through pigs, additional changes were noted, consisting of the shift from a positively charged R at position 172 of 1D to a mixture of R with noncharged residues and an associated loss of binding to heparin-Sepharose (Table 3).
FIG. 3.
Comparison of severity of disease induced in pigs by chimeric viruses VpF1, VpB1, and VpB2. For these experiments, animals 47 and 48 were inoculated intradermally with approximately 165,000 PFU of VpF1, animals 468 and 469 were inoculated with approximately 385,000 PFU of VpB1, and animal 470 was infected by continuous contact with the two VpB1-inoculated animals. Animals 49 and 50 were inoculated with approximately 775,000 PFU of VpB2. Solid lines indicate lesion scores, calculated by adding the number of sites away from the inoculation site that were affected by disease (the maximum value achievable was 19 [see Materials and Methods]). Dotted lines indicate the amount of virus detected in blood. TCID50, 50% tissue culture infective dose.
As mentioned above, the chimeric viruses derived from vac-O/CHA/90 (VpB1 and VpB2) faithfully maintained the original plasmid cDNA sequences in cell culture (Table 3). In addition, VpB1 and VpB2 appeared to be more attenuated in pigs than VpF1 (which contained the capsid sequences of the pig isolate O/CHA/90) in terms of the disease produced postinoculation (see Fig. 3). Specifically, the data collected postinoculation revealed that VpB2 was particularly avirulent (only one of the inoculated animals displayed any lesions away from the inoculation site or any viremia, and the virus apparently did not spread to the cohoused animal during the 7-day observation period [see Fig. 3]). However, despite this low virulence, we were able to obtain virus from one in-contact animal (VpB1) and one inoculated animal (VpB2). Although one of these recovered viruses (Vpig470) maintained the sequence of the original inoculated virus during passage through the pig, the other (Vpig50) acquired a mutation resulting in the loss of a positively charged R codon at position 172 of 1D. Interestingly, this mutation abolished binding to HS and infection of all three types of CHO cells (Table 3).
To learn more about the requirements of individual capsid residues for acquisition of the ability to infect CHO cells, we undertook construction of a large number of chimeric viruses harboring different portions of the capsids found in cDNAs pF1, pB1, and pB2. Table 4 shows the genetic structures of the viruses obtained for these analyses. Interestingly, for several of these constructs, the recovered viruses differed from the transfected genome-length RNA at position 83 of 1D. Specifically, all viruses derived from chimeric cDNAs that contained the E at position 83 of 1D of plasmid pF1 (derived from the field isolate of O/CHA/90) contained mixtures of the original E codon and a codon for K at this position (Table 4).
Evaluation of cell culture host range data from the chimeric viruses shown in Table 4 indicated that a constellation of amino acids in 1D was required for growth in CHO cells. Interestingly, unlike the previous work on O1 Campos, where one could easily identify a single residue that allowed a tissue culture-adapted O1 Campos virus to grow in CHO cells expressing HS (44), we were unable to find such a mutation in the cell-adapted derivatives of O/CHA/90. Furthermore, unlike the work with O1 Campos, derivatives of O/CHA/90 that grew in HS-expressing CHO cells (CHO-K1) also grew in two GAG mutant cell lines that are known to produce very low levels of HS and chondroitin sulfate (CHO-745) (19) or low levels of HS alone (CHO-677) (36). As mentioned above, following passage of chimeric viruses that expressed an E at position 83, there was a selection of viruses with a positively charged K residue at position 83. However, this K by itself did not determine the ability of the virus to grow in CHO cells. Rather, this K always needed to be accompanied by an R at position 172 in order for growth to be achieved in CHO cells (see Table 3, Vpig50). Further, these two residues together could not mediate growth in CHO cells if the capsid-encoding sequences also encoded an H at 1D/108 and a T at 1D/174 (Table 4; compare VpF1 with VpF1YY and VpF1FF, compare VpB1F1 with VpB1 and VB1B2, and compare VpB2F1 with VpB2 and VpB2B1). Comparisons of VpB2 with VpB2B2F1 and VpB2F1B2 indicate that either an H at 1D/108 or a T at 1D/174 prevents the two charged residues from functioning to facilitate growth in CHO cells (Table 4). Taken together, these data demonstrate that both the two aromatic residues at positions 1D/108 and 1D/174 and the two charged residues at 1D/83 and 1D/172 are required for growth in CHO cells.
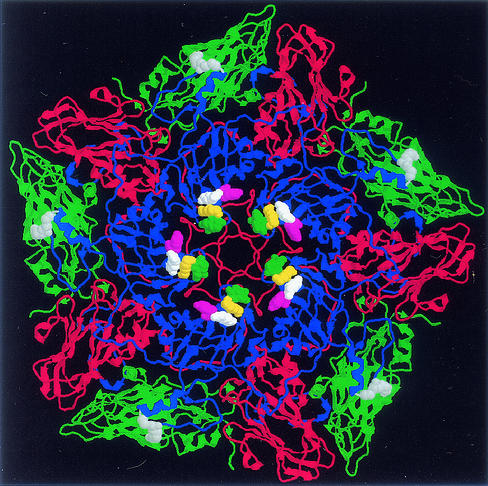
The three-dimensional relationships of these residues are shown in Fig. 4. This figure shows that these residues are clustered around the pore at the fivefold axis of the viral particle, distant from the RGD sequence known to mediate the binding of FMDV to integrins (see the introduction) or sequences at the 1C/1D interface within the biological protomer that have been shown to participate in the binding of heparin and HS to the type O1 Campos capsid (22, 48).
FIG. 4.
Structural representation of 1 of the 12 pentamers that constitute the virion of VpB2, showing the position of residues defining the new receptor specificity of FMDV surrounding the pore at the fivefold axis. Coordinates for the model were obtained by using the SWISS-MODEL program (23), available at http://www.expasy.ch, by modeling the predicted amino acids of VpB2 onto the X-ray crystallography-derived structure of O1 BFS (37) (PDB accession no. 1FOD). This figure shows a view from the outside of the virus particle, looking into the pore at the fivefold axis of a pentameric subunit composed of five copies of protomers comprising proteins 1B, 1C, and 1D; the internally located protein 1A has been removed from the model for clarity. Proteins 1B (green), 1C (red), and 1D (blue) are shown with ribbons representing the β-sheets and α-helices and rods representing the coiled regions of the polypeptide chains. 1D residues 83 (yellow), 108 (green), 172 (white), and 174 (violet), as well as the RGD tripeptide at positions 145 to 147 (gray), are shown in a space-filling representation to facilitate their localization on the capsid structure.
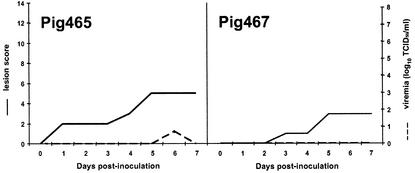
To explore the receptor specificity of viruses with the genotype 1D/83K 1D/108Y 1D/172R 1D/174Y (or F), we produced viruses with these residues that contained a KGE sequence in place of the naturally occurring, integrin-binding RGD (Table 5). It has formerly been shown that the KGE sequence, in the context of either a serotype A12 virus (42) or a type O1 virus (in the absence of HS binding) (45), was incapable of substituting for RGD in allowing the virus to grow in culture. Thus, it was surprising to observe that the KGE derivatives of O/CHA/90 were able to replicate well in cell culture (Table 5), maintaining the KGE sequence during passage (Table 5). Even more surprisingly, upon testing of one of these KGE viruses in animals, we found that it was able to cause a mild disease in pigs (Fig. 5). This disease was characterized by viremia in one of the two inoculated animals, lesions on the tongues of both animals, and vesicles distant from the inoculation sites on the feet. One of these vesicles was used as the source of the virus that was sequenced to reveal that the originally inoculated KGE virus (Table 5) was responsible for the observed disease.
TABLE 5.
Comparison of P1 sequences and in vitro properties of RGD and KGE derivatives of chimeric virus VpB1 and a KGE virus recovered from an animal
| Virusa | Residue in protein:
|
Titer (PFU/ml) on the following cell line:
|
% Heparin-Sepharose binding | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1B
|
1C
|
1D
|
||||||||||||||||
| 78 | 130 | 132 | 195 | 30 | 200 | 83 | 108 | 142 | 145-147 | 171 | 172 | 174 | BHK21 | CHOK1 | CHO677 | CHO745 | ||
| VpB1 | C | Y | I | L | L | V | K | Y | S | RGD | P | R | F | 1.6 × 108 | 5.7 × 104 | 1.2 × 106 | 4.7 × 106 | 97 |
| VpB1-KGE | C | Y | I | L | L | V | K | Y | S | KGE | P | R | F | 6.5 × 107 | 8.7 × 105 | 1.4 × 106 | 1.5 × 107 | 95 |
| VPig465b | C | Y | I | L | L | V | K | Y | S | KGE | P | R | F | 9.5 × 105 | 3.5 × 102 | 1.2 × 104 | 2.5 × 104 | 44 |
| VpB2 | Y | C | I | P | F | V | K | Y | S | RGD | T | R | Y | 1.8 × 108 | 4.1 × 105 | 3.7 × 106 | 1.5 × 107 | 82 |
| VpB2-KGE | Y | C | I | P | F | V | K | Y | S | KGE | T | R | Y | 1.3 × 108 | 5.4 × 105 | 6.3 × 106 | 1.8 × 107 | 74 |
Virus names are derived from plasmid names; see Fig. 1 and the text for construction methodology.
Virus recovered from a vesicular lesion (away from the inoculation site) of an animal inoculated with VpB1-KGE.
FIG. 5.
Evaluation of disease induced by VpB1-KGE. For this experiment, animals 465 and 467 were inoculated intradermally with approximately 175,000 PFU of VpB1-KGE. Solid lines indicate lesion scores, calculated by adding the number of sites away from the inoculation site that were affected by disease (the maximum value achievable was 19 [see Materials and Methods]). Dotted lines indicate the amount of virus detected in the blood.
Evaluation of receptor binding by using synthetic peptides.
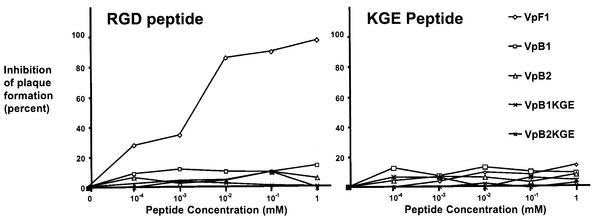
The nature of the binding of VpB1-KGE to cells was further evaluated by utilizing a peptide inhibition of plaque formation protocol similar to that reported by Baranowski et al. (2). The results of these studies, shown in Fig. 6, demonstrate that of the genetically engineered viruses tested, only VpF1 was inhibited from forming plaques on BHK cells by pretreatment with RGD-containing peptides. Further, none of the viruses, including the two containing KGE sequences, were inhibited from forming plaques on BHK cells by KGE-containing peptides (Fig. 6).
FIG. 6.
Inhibition of FMDV infectivity by an RGD peptide (RVSNVRGDLQVLAQK) and a KGE peptide (RVSNVKGELQVLAQK). Monolayers of BHK cells (diameter, 35 mm) were treated with peptides (Sigma-Genosys, The Woodlands, Tex.), diluted at the indicated concentrations in HEPES-buffered medium, for 45 min at 37°C. The indicated viruses were then added to the peptide mixture at concentrations of 25 to 50 PFU per well and were incubated for an additional 45 min. Following low-pH treatment to inactivate unadsorbed virus, the monolayers were overlaid and plaques were revealed by staining 48 h later.
DISCUSSION
Growth of eucaryotic viruses in unnatural hosts has proven invaluable for identification and characterization of pathogens, production of diagnostic reagents, and production of vaccines. However, growth of viruses in cell culture produces selective pressures that are different from those effected by natural transmission and can readily result in the selection of new variants, especially in the case of RNA viruses (see the introduction). Here we describe how adaptation of a field isolate of FMDV to cell culture in the People's Republic of China resulted in selection of variants with altered properties in vitro and in vivo.
Multiple lines of evidence suggest that the normal method of FMDV attachment to cells in vivo is mediated by binding of an RGD sequence in the G-H loop of protein 1D to integrin molecules on the surfaces of susceptible cells (see the introduction). However, in cell culture, other cell surface molecules, including HS, can substitute for integrin molecules in infection (see the introduction). In previous studies it has been shown that adaptation of a type O1 Campos to cell culture selected viruses with an H→R codon shift at position 56 of 1C, which was frequently reported for cell culture-passaged subtype O1 viruses (48). In the present studies on a different subtype of FMDV type O, we did not record any differences in this position; rather, we noted that changes at other sites were selected upon passage in cell culture. Nevertheless, systematic evaluation of these changes, utilizing reverse genetics technology, was able to demonstrate a similarity with the earlier studies. Specifically, passage of virus in cell culture selects viruses with an expanded host range in cell culture and with altered amino acid residues on their capsid surfaces. In the case of the Chinese virus, the changes were clustered around the fivefold axis of the virion, in a region previously shown to be altered by very high level passage of a type C virus in cell culture (2, 3, 18, 39).
Evaluation of the Cathay virus and its derivatives has revealed that a constellation of residues is responsible for acquisition of the ability of Cathay topotype FMDVs to bind to heparin-Sepharose and grow in CHO cells and that these changes also reduce virulence in animals. The latter data were obtained from pathogenicity data in pigs and sequence data obtained from analyses of viruses recovered from vesicles that developed in the infected animals. Although the pathogenicity data were generated from a small number of animals, they suggest that viruses with capsid surface-exposed positive charges are less virulent. Furthermore, sequence data obtained from viruses recovered from animals inoculated with viruses expressing the cell culture-acquired K at position 83 showed that these viruses had, in some cases, lost another positively charged residue (172R), indicating the importance of both of these residues in reducing the ability of the virus to cause vesicles to form. These results can most easily be explained by the supposition that the presence of charged residues at both sites produces a charged patch on the capsid surface (see Fig. 4) that facilitates removal of viruses from the animal's circulation, preventing interaction with the specific cell types needed to produce vesicular disease.
Taken together, our results support an expanding body of literature on the acquisition of HS binding by experimentally propagated viruses and the role of this altered receptor specificity in attenuation (10, 12, 13, 25, 30, 33, 34, 38). In these cases, the ability to bind to HS appears to correlate with the finding that attenuated viruses are rapidly cleared from the circulation, preventing systemic spread and disease. Since acquisition of binding to HS may serve only to prevent a virus from reaching its target tissue, HS does not need to function as a receptor either in vitro or in vivo, and the ability to bind heparin-Sepharose may not always correlate with the ability to utilize HS as a receptor. However, selection of HS-binding variants during in vitro propagation would be most easily explained by utilization of HS as a receptor or coreceptor.
The data on a Cathay topotype virus presented in this paper extend earlier studies on a type O virus from South America (48) by showing that even within the same serotype, different sites can be altered in the acquisition of new cell binding properties. These findings add to the concern that tissue culture propagation can adversely affect vaccine seeds through the selection of viruses that could be altered at multiple sites. Thus, vaccine manufacturers need to be particularly vigilant that propagation does not bias the antigenic profile of their products, especially in light of findings that multiple epitopes are likely to be required to produce highly protective vaccines (1, 51).
Cell culture adaptation of O/CHA/90 was accompanied by selection of viruses that had substitutions of a positively charged amino acid (K) at position 83 of 1D for the negatively charged WT residue (E). As expected from the earlier studies cited above, this alteration in a surface-exposed capsid residue produced viruses with increased abilities to bind to heparin-Sepharose under physiological salt conditions. However, comparison of the growth of these viruses on two CHO cell lines with mutations in GAG biosynthesis failed to conclusively demonstrate that the cell-adapted O/CHA/90 had acquired the ability to utilize HS as an alternative receptor. Although both of these cell lines have been shown to harbor mutations that significantly reduce HS (CHO-677) (36) or HS and chondroitin sulfate (CHO-745) (19) levels, the cell culture-adapted derivatives of the Cathay viruses either might be able to bind very efficiently to low levels of these GAGs synthesized by the mutant cells or might bind to other GAGs expressed on the surfaces of the mutant cells. Although these two mutants clearly produce very low levels of GAGs, it has previously been shown that heparinase could reduce the growth of HS-binding viruses in CHO-745, suggesting a low level of HS synthesis in these cells (44). However, in the present study, we failed to demonstrate that heparinase could reduce the plaque-forming ability of VpB1KGE on a WT or either mutant CHO cell line (data not shown), arguing against a role of HS (but not other GAGs) in the observed growth of the Chinese virus derivatives on the three CHO cell lines used in the present study. The observed difference in GAG binding by these Cathay viruses and the O1 Campos viruses (see above), as well as the type C viruses described by Domingo and coworkers (2, 3, 39), is not surprising, given the report by Spear and coworkers that strains of herpes simplex virus differ in their abilities to bind to subsets of HS molecules depending on their degrees of carbohydrate sulfation (50).
Despite our ability to demonstrate the importance of a constellation of residues on the capsid surface of FMDV for its ability to utilize a new receptor in vitro, we have failed to precisely determine the cell surface molecule utilized by these viruses. As discussed above, the cell surface molecules utilized in reception could consist of one or more GAG molecules (although the binding must be different from that previously determined for cell-adapted O1 viruses; see above). Alternatively, the tissue culture-adapted viruses could bind to a different subset of integrin molecules present on CHO cells (both WT and GAG mutants) that are not able to interact with field viruses such as O/CHA/90 or VpF1. Following this line of reasoning, it is possible that passage of O/CHA/90 in the BHK cells at the Lanzhao Institute selected viruses with an enhanced ability to bind to a subset of integrin molecules that are present on both BHK and CHO cells. A further extension of this line of thought includes the possibility that the selected viruses could have G-H loops in protein 1D that have enhanced affinity for a subset of integrins and that these loops could permit a virus with an “unnatural” (non-RGD) loop to bind to integrins. This could explain the finding that in the context of one of the tissue culture-adapted Cathay viruses, the KGE was apparently able to direct the virus to the sites required to cause disease (even though we have previously been unable to demonstrate integrin-mediated infectivity of type O1 or A12 viruses containing a nonconservative KGE-for-RGD substitution [see Results and the introduction]). This is not the first report of a virus capable of initiating infection in the absence of the highly conserved RGD. Taboga et al. reported the recovery of a type C virus (containing an RGGD sequence) from animals that failed to be protected from disease following vaccination with synthetic peptides (51). In addition, work on another type C virus with an RGG sequence (in this case a genetically engineered derivative of a highly passaged monoclonal antibody escape variant) indicated that it did not utilize either an RGD/integrin or a HS-mediated infection pathway in vitro (2). However, the properties of this type C virus in vivo were not reported (2).
Although none of the residues implicated in the altered receptor binding activities of our panel of mutants are found within the RGD-containing G-H loop of protein 1D, it has been demonstrated that changes elsewhere on the FMDV capsid can alter the conformation of this flexible loop. These include changes on 1B in a patch underlying the 1D G-H loop in the structure of the reduced form of serotype O1 FMDV (37) (1B/78, 1B/130, 1B/132) that is in a region shown to modulate the structure of the loop of serotype A22 virus variants that differ in antigenic and cell binding characteristics (15). Interestingly, the 1B residues that differ among the Cathay virus derivatives include a C residue at position 130 of 1B that can form a disulfide linkage with a C at position 134 of the G-H loop of protein 1D in the type O1 BFS virus particle (37). With respect to this C-C linkage, it is noteworthy that (i) all of the derivatives of O/CHA/90 that we evaluated contained the C at position 134 in 1D, (ii) O/CHA/90 and vac-O/CHA/90 had a mixture of residues (C/Y) at position 130 of 1B, and (iii) one of the two vac-O/CHA/90 derivatives had a C at position 130 in 1B. Interestingly, both O/CHA/90 and vac-O/CHA/90 also showed a mixture of C and Y at position 78 of 1B, but all cloned cDNAs recovered from these viruses had the genotype C78-Y130 or Y78-C130, but never Y78-Y130 or C78-C130. However, our analyses of genetically engineered derivatives revealed that the presence or absence of C residues in these positions in 1B could not explain the ability of a subset of viruses to grow in CHO cells (Table 4). Nevertheless, the ability to form a disulfide cross-link could produce changes in the G-H loop that could permit other subtle interactions, altering the ability of the resulting viruses to bind to integrins that are required for replication in vitro or development of disease in vivo. Taken one step further, this type of modulation of the loop could help to permit the KGE-containing virus to bind to the same class of integrins that are utilized by RGD-expressing FMDVs in the development of disease (see above). Although this hypothesis would seem to be the most reasonable, given the extensive amount of data on RGD-integrin interactions (see the introduction), our findings that the KGE-expressing viruses cause disease raise the possibility that a non-RGD-integrin interaction could be responsible for the generation of FMD in the natural host. Even so, it should be noted that work with an RGD-less coxsackievirus A9 shows that even in the absence of the RGD sequence, the virus can bind to integrin αVβ3 (53), and that other work suggests that although this integrin is required for binding, coreceptors are also required for internalization (52). Finally, the fact that neither RGD nor KGE peptides inhibited plaque formation by the pig-virulent KGE virus we generated suggests that multiple receptors and viral components can be utilized for mediating infection and disease by FMDV.
Acknowledgments
We thank the Swiss Institute of Bioinformatics for making the SWISS-MODEL program freely available (http://www.expasy.ch). We thank S. Curry, Imperial College, London, United Kingdom, for helping to manipulate the structural files to permit viewing of the virus as a pentamer. We thank B. Baxt, PIADC, for helpful discussions and suggestions during the completion of this work and for critical reading of the manuscript.
REFERENCES
- 1.Aggarwal, N., and P. V. Barnett. 2002. Antigenic sites of foot-and-mouth disease virus (FMDV): an analysis of the specificities of anti-FMDV antibodies after vaccination of naturally susceptible host species. J. Gen. Virol. 83:775-782. [DOI] [PubMed] [Google Scholar]
- 2.Baranowski, E., C. M. Ruiz-Jarabo, N. Sevilla, D. Andreu, E. Beck, and E. Domingo. 2000. Cell recognition by foot-and-mouth disease virus that lacks the RGD integrin-binding motif: flexibility in aphthovirus receptor usage. J. Virol. 74:1641-1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baranowski, E., N. Sevilla, N. Verdaguer, C. M. Ruiz-Jarabo, E. Beck, and E. Domingo. 1998. Multiple virulence determinants of foot-and-mouth disease virus in cell culture. J. Virol. 72:6362-6372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnett, P. V., E. J. Ouldridge, D. J. Rowlands, F. Brown, and N. R. Parry. 1989. Neutralizing epitopes of type O foot-and-mouth disease virus. I. Identification and characterization of three functionally independent, conformational sites. J. Gen. Virol. 70:1483-1491. [DOI] [PubMed] [Google Scholar]
- 5.Baxt, B., and Y. Becker. 1990. The effect of peptides containing the arginine-glycine-aspartic acid sequence on the adsorption of foot-and-mouth disease virus to tissue culture cells. Virus Genes 4:73-83. [DOI] [PubMed] [Google Scholar]
- 6.Baxt, B., and P. W. Mason. 1995. Foot-and-mouth disease virus undergoes restricted replication in macrophage cell cultures following Fc receptor-mediated adsorption. Virology 207:503-509. [DOI] [PubMed] [Google Scholar]
- 7.Baxt, B., D. O. Morgan, B. H. Robertson, and C. A. Timpone. 1984. Epitopes on foot-and-mouth disease virus outer capsid protein VP1 involved in neutralization and cell attachment. J. Virol. 51:298-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baxt, B., V. Vakharia, D. M. Moore, A. J. Franke, and D. O. Morgan. 1989. Analysis of neutralizing antigenic sites on the surface of type A12 foot-and-mouth disease virus. J. Virol. 63:2143-2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beard, C. W., and P. W. Mason. 2000. Genetic determinants of altered virulence of Taiwanese foot-and-mouth disease virus. J. Virol. 74:987-991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bernard, K. A., W. B. Klimstra, and R. E. Johnston. 2000. Mutations in the E2 glycoprotein of Venezuelan equine encephalitis virus confer heparan sulfate interaction, low morbidity, and rapid clearance from blood of mice. Virology 276:93-103. [DOI] [PubMed] [Google Scholar]
- 11.Burrows, R. 1966. The infectivity assay of foot-and-mouth disease virus in pigs. J. Hyg. Camb. 64:419-429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Byrnes, A. P., and D. E. Griffin. 1998. Binding of Sindbis virus to cell surface heparan sulfate. J. Virol. 72:7349-7356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Byrnes, A. P., and D. E. Griffin. 2000. Large-plaque mutants of Sindbis virus show reduced binding to heparan sulfate, heightened viremia, and slower clearance from the circulation. J. Virol. 74:644-651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crowther, J. R., S. Farias, W. C. Carpenter, and A. R. Samuel. 1993. Identification of a fifth neutralizable site on type O foot-and-mouth disease virus following characterization of single and quintuple monoclonal antibody escape mutants. J. Gen. Virol. 74:1547-1553. [DOI] [PubMed] [Google Scholar]
- 15.Curry, S., E. Fry, W. Blakemore, R. Abu-Ghazaleh, T. Jackson, A. King, S. Lea, J. Newman, D. Rowlands, and D. Stuart. 1996. Perturbations in the surface structure of A22 Iraq foot-and-mouth disease virus accompanying coupled changes in host cell specificity and antigenicity. Structure 4:135-145. [DOI] [PubMed] [Google Scholar]
- 16.Domingo, E., and J. J. Holland. 1997. RNA virus mutations and fitness for survival. Annu. Rev. Microbiol. 51:151-178. [DOI] [PubMed] [Google Scholar]
- 17.Dunn, C. S., and A. I. Donaldson. 1997. Natural adaption to pigs of a Taiwanese isolate of foot-and-mouth disease virus. Vet. Rec. 141:174-175. [DOI] [PubMed] [Google Scholar]
- 18.Escarmis, C., E. C. Carrillo, M. Ferrer, J. F. Arriaza, N. Lopez, C. Tami, N. Verdaguer, E. Domingo, and M. T. Franze-Fernandez. 1998. Rapid selection in modified BHK-21 cells of a foot-and-mouth disease virus variant showing alterations in cell tropism. J. Virol. 72:10171-10179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Esko, J. D., T. E. Stewart, and W. H. Taylor. 1985. Animal cell mutants defective in glycosaminoglycan biosynthesis. Proc. Natl. Acad. Sci. USA 82:3197-3201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fox, G., N. R. Parry, P. V. Barnett, B. McGinn, D. J. Rowlands, and F. Brown. 1989. The cell attachment site on foot-and-mouth disease virus includes the amino acid sequence RGD (arginine-glycine-aspartic acid). J. Gen. Virol. 70:625-637. [DOI] [PubMed] [Google Scholar]
- 21.Frohman, M. A., M. K. Dush, and G. R. Martin. 1988. Rapid production of full-length cDNAs from rare transcripts: amplification using a single gene-specific oligonucleotide primer. Proc. Natl. Acad. Sci. USA 85:8998-9002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fry, E. E., S. M. Lea, T. Jackson, J. W. Newman, F. M. Ellard, W. E. Blakemore, R. Abu-Ghazaleh, A. Samuel, A. M. King, and D. I. Stuart. 1999. The structure and function of a foot-and-mouth disease virus-oligosaccharide receptor complex. EMBO J. 18:543-554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guex, N., and M. C. Peitsch. 1997. SWISS-MODEL and the Swiss-PdbViewer: an environment for comparative protein modeling. Electrophoresis 18:2714-2723. [DOI] [PubMed] [Google Scholar]
- 24.Higuchi, R., B. Krummel, and R. K. Saiki. 1988. A general method of in vitro preparation and specific mutagenesis of DNA fragments: study of protein and DNA interactions. Nucleic Acids Res. 16:7351-7367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hulst, M. M., H. G. van Gennip, A. C. Vlot, E. Schooten, A. J. de Smit, and R. J. Moormann. 2001. Interaction of classical swine fever virus with membrane-associated heparan sulfate: role for virus replication in vivo and virulence. J. Virol. 75:9585-9595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jackson, T., F. M. Ellard, R. A. Ghazaleh, S. M. Brookes, W. E. Blakemore, A. H. Corteyn, D. I. Stuart, J. W. Newman, and A. M. King. 1996. Efficient infection of cells in culture by type O foot-and-mouth disease virus requires binding to cell surface heparan sulfate. J. Virol. 70:5282-5287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jackson, T., A. P. Mould, D. Sheppard, and A. M. King. 2002. Integrin αvβ1 is a receptor for foot-and-mouth disease virus. J. Virol. 76:935-941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jackson, T., D. Sheppard, M. Denyer, W. Blakemore, and A. M. King. 2000. The epithelial integrin αvβ6 is a receptor for foot-and-mouth disease virus. J. Virol. 74:4949-4956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kitson, J. D., D. McCahon, and G. J. Belsham. 1990. Sequence analysis of monoclonal antibody resistant mutants of type O foot and mouth disease virus: evidence for the involvement of the three surface exposed capsid proteins in four antigenic sites. Virology 179:26-34. [DOI] [PubMed] [Google Scholar]
- 30.Klimstra, W. B., K. D. Ryman, and R. E. Johnston. 1998. Adaptation of Sindbis virus to BHK cells selects for use of heparan sulfate as an attachment receptor. J. Virol. 72:7357-7366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Knowles, N. J., P. R. Davies, T. Henry, V. O'Donnell, J. M. Pacheco, and P. W. Mason. 2001. Emergence in Asia of foot-and-mouth disease viruses with altered host range: characterization of alterations in the 3A protein. J. Virol. 75:1551-1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Knowles, N. J., A. R. Samuel, P. R. Davies, R. P. Kitching, and A. I. Donaldson. 2001. Outbreak of foot-and-mouth disease virus serotype O in the UK caused by a pandemic strain. Vet. Rec. 148:258-259. [PubMed] [Google Scholar]
- 33.Lee, E., and M. Lobigs. 2002. Mechanism of virulence attenuation of glycosaminoglycan-binding variants of Japanese encephalitis virus and Murray Valley encephalitis virus. J. Virol. 76:4901-4911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee, P., R. Knight, J. M. Smit, J. Wilschut, and D. E. Griffin. 2002. A single mutation in the E2 glycoprotein important for neurovirulence influences binding of Sindbis virus to neuroblastoma cells. J. Virol. 76:6302-6310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leippert, M., E. Beck, F. Weiland, and E. Pfaff. 1997. Point mutations within the βG-βH loop of foot-and-mouth disease virus O1K affect virus attachment to target cells. J. Virol. 71:1046-1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lidholt, K., J. L. Weinke, C. S. Kiser, F. N. Lugemwa, K. J. Bame, S. Cheifetz, J. Massague, U. Lindahl, and J. D. Esko. 1992. A single mutation affects both N-acetylglucosaminyltransferase and glucuronosyltransferase activities in a Chinese hamster ovary cell mutant defective in heparan sulfate biosynthesis. Proc. Natl. Acad. Sci. USA 89:2267-2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Logan, D., R. Abu-Ghazaleh, W. Blakemore, S. Curry, T. Jackson, A. King, S. Lea, R. Lewis, J. Newman, N. Parry, et al. 1993. Structure of a major immunogenic site on foot-and-mouth disease virus. Nature 362:566-568. [DOI] [PubMed] [Google Scholar]
- 38.Mandl, C. W., H. Kroschewski, S. L. Allison, R. Kofler, H. Holzmann, T. Meixner, and F. X. Heinz. 2001. Adaptation of tick-borne encephalitis virus to BHK-21 cells results in the formation of multiple heparan sulfate binding sites in the envelope protein and attenuation in vivo. J. Virol. 75:5627-5637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martinez, M. A., N. Verdaguer, M. G. Mateu, and E. Domingo. 1997. Evolution subverting essentiality: dispensability of the cell attachment Arg-Gly-Asp motif in multiply passaged foot-and-mouth disease virus. Proc. Natl. Acad. Sci. USA 94:6798-6802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mason, P. W., B. Baxt, F. Brown, J. Harber, A. Murdin, and E. Wimmer. 1993. Antibody-complexed foot-and-mouth disease virus, but not poliovirus, can infect normally insusceptible cells via the Fc receptor. Virology 192:568-577. [DOI] [PubMed] [Google Scholar]
- 41.Mason, P. W., S. V. Bezborodova, and T. M. Henry. 2002. Identification and characterization of a cis-acting replication element (cre) adjacent to the internal ribosome entry site of foot-and-mouth disease virus. J. Virol. 76:9686-9694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mason, P. W., E. Rieder, and B. Baxt. 1994. RGD sequence of foot-and-mouth disease virus is essential for infecting cells via the natural receptor but can be bypassed by an antibody-dependent enhancement pathway. Proc. Natl. Acad. Sci. USA 91:1932-1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mateu, M. G. 1995. Antibody recognition of picornaviruses and escape from neutralization: a structural view. Virus Res. 38:1-24. [DOI] [PubMed] [Google Scholar]
- 44.Neff, S., P. W. Mason, and B. Baxt. 2000. High-efficiency utilization of the bovine integrin αvβ3 as a receptor for foot-and-mouth disease virus is dependent on the bovine β3 subunit. J. Virol. 74:7298-7306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44a.Office International des Épizooties. 1990. OIE Bull. 102:724.
- 45.Neff, S., D. Sa-Carvalho, E. Rieder, P. W. Mason, S. D. Blystone, E. J. Brown, and B. Baxt. 1998. Foot-and-mouth disease virus virulent for cattle utilizes the integrin αvβ3 as its receptor. J. Virol. 72:3587-3594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pfaff, E., H. J. Thiel, E. Beck, K. Strohmaier, and H. Schaller. 1988. Analysis of neutralizing epitopes on foot-and-mouth disease virus. J. Virol. 62:2033-2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rieder, E., T. Bunch, F. Brown, and P. W. Mason. 1993. Genetically engineered foot-and-mouth disease viruses with poly(C) tracts of two nucleotides are virulent in mice. J. Virol. 67:5139-5145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sa-Carvalho, D., E. Rieder, B. Baxt, R. Rodarte, A. Tanuri, and P. W. Mason. 1997. Tissue culture adaptation of foot-and-mouth disease virus selects viruses that bind to heparin and are attenuated in cattle. J. Virol. 71:5115-5123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Samuel, A. R., and N. J. Knowles. 2001. Foot-and-mouth disease type O viruses exhibit genetically and geographically distinct evolutionary lineages (topotypes). J. Gen. Virol. 82:609-621. [DOI] [PubMed] [Google Scholar]
- 50.Shukla, D., J. Liu, P. Blaiklock, N. W. Shworak, X. Bai, J. D. Esko, G. H. Cohen, R. J. Eisenberg, R. D. Rosenberg, and P. G. Spear. 1999. A novel role for 3-O-sulfated heparan sulfate in herpes simplex virus 1 entry. Cell 99:13-22. [DOI] [PubMed] [Google Scholar]
- 51.Taboga, O., C. Tami, E. Carrillo, J. I. Nunez, A. Rodriguez, J. C. Saiz, E. Blanco, M. L. Valero, X. Roig, J. A. Camarero, D. Andreu, M. G. Mateu, E. Giralt, E. Domingo, F. Sobrino, and E. L. Palma. 1997. A large-scale evaluation of peptide vaccines against foot-and-mouth disease: lack of solid protection in cattle and isolation of escape mutants. J. Virol. 71:2606-2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Triantafilou, K., D. Fradelizi, K. Wilson, and M. Triantafilou. 2002. GRP78, a coreceptor for coxsackievirus A9, interacts with major histocompatibility complex class I molecules which mediate virus internalization. J. Virol. 76:633-643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Triantafilou, M., K. Triantafilou, K. M. Wilson, Y. Takada, and N. Fernandez. 2000. High affinity interactions of Coxsackievirus A9 with integrin αvβ3 (CD51/61) require the CYDMKTTC sequence of β3, but do not require the RGD sequence of the CAV-9 VP1 protein. Hum. Immunol. 61:453-459. [DOI] [PubMed] [Google Scholar]
- 54.Xie, Q. C., D. McCahon, J. R. Crowther, G. J. Belsham, and K. C. McCullough. 1987. Neutralization of foot-and-mouth disease virus can be mediated through any of at least three separate antigenic sites. J. Gen. Virol. 68:1637-1647. [DOI] [PubMed] [Google Scholar]
- 55.Yang, P. C., R. M. Chu, W. B. Chung, and H. T. Sung. 1999. Epidemiological characteristics and financial costs of the 1997 foot-and-mouth disease epidemic in Taiwan. Vet. Rec. 145:731-734. [DOI] [PubMed] [Google Scholar]