Tobacco (Nicotiana tabacum) is cultivated in more than 100 countries,1 and in 2004, some 5.73 million metric tons dry weight of tobacco were grown worldwide.2 The top five tobacco producers forecast for 2004 are China (2.01 million metric tons; 35.1%), Brazil (757 thousand metric tons; 13.2%), India (598 thousand metric tons; 10.4%), United States (358 thousand metric tons; 6.2%), and Malawi (138 thousand metric tons; 2.4%).2 Together, these five countries account for two-thirds of worldwide tobacco production.
Tobacco farming presents several hazards to those who cultivate and harvest the plant. Although some of these hazards, such as pesticide exposure and musculoskeletal trauma,3 are faced by workers in other types of agricultural production, tobacco production presents some unique hazards, most notably acute nicotine poisoning, a condition also known as green tobacco sickness (GTS).4,5,6 GTS is an occupational poisoning that can affect workers who cultivate and harvest tobacco. It occurs when workers absorb nicotine through the skin as they come into contact with leaves of the mature tobacco plant. GTS is characterized largely by nausea, vomiting, headache, muscle weakness, and dizziness.7,8
Historically, children have played a role in agricultural production in the United States,9,10 and they continue to do so today.11 This includes tobacco farming.12,13 The North American Guidelines for Children’s Agricultural Tasks,14 a set of injury prevention guidelines prepared by the National Children’s Center for Rural and Agricultural Health and Safety, lists GTS as one of several hazards children face when working on tobacco farms.14,15 Children 17 years of age and younger who work on U.S. tobacco farms come from three main groups: members of farm families, migrant youth laborers (primarily Latinos), and other hired local children. All three groups are at risk for GTS. Beyond the U.S., tobacco production using child labor is an emerging topic of concern in developing nations. An international movement, advocated by the Eliminating Child Labor in Tobacco Foundation, is underway to restrict child labor in tobacco production.16
GTS is a unique occupational poisoning associated with tobacco farming. We suspect that many public health practitioners, clinicians, advocates, and researchers are unaware of GTS among children and adolescents. In this article, we provide an overview of GTS among young people who work in tobacco, summarize reports documenting pediatric GTS cases, explain GTS etiology, and present three case studies of pediatric GTS in Kentucky. In addition, we discuss the need for expanded surveillance and prevention of GTS, both in the United States and globally.
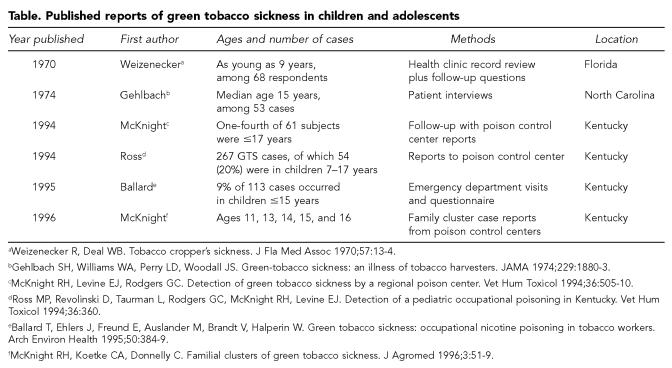
GTS AMONG THE YOUNG IN PUBLISHED REPORTS
In the United States, published reports of GTS among children and adolescents are scant and are derived from two sources: potential GTS cases reported to poison control centers, and records from health care facilities where pediatric patients have presented with symptoms of GTS. We summarize these U.S.-based studies in the Table. Although GTS has been documented among adults in India, Japan, and the United States, we found no reports of this occupational poisoning occurring in children or adolescents outside the United States.
Table.
Published reports of green tobacco sickness in children and adolescents
Weizenecker R, Deal WB. Tobacco cropper's sickness. J Fla Med Assoc 1970;57:13–4.
Gehlbach SH, Williams WA, Perry LD, Woodall JS. Green-tobacco sickness: an illness of tobacco harvesters. JAMA 1974;229:1880–3.
McKnight RH, Levine EJ, Rodgers GC. Detection of green tobacco sickness by a regional poison center. Vet Hum Toxicol 1994;36:505–10.
Ross MP, Revolinski D, Taurman L, Rodgers GC, McKnight RH, Levine EJ. Detection of a pediatric occupational poisoning in Kentucky. Vet Hum Toxicol 1994;36:360.
Ballard T, Ehlers J, Freund E, Auslander M, Brandt V, Halperin W. Green tobacco sickness: occupational nicotine poisoning in tobacco workers. Arch Environ Health 1995;50:384–9.
McKnight RH, Koetke CA, Donnelly C. Familial clusters of green tobacco sickness. J Agromed 1996;3:51–9.
GTS EXPOSURE FACTORS
Several factors, some unique to tobacco production, place tobacco workers at risk for GTS. first, the tobacco plant itself is the source of biohazard, unlike other crops where hazards, such as exposure to pesticides, are external to the plant. Comparable situations primarily occur only among those who cultivate illicit crops like coca and opium. Thus, an inherent risk in cultivating tobacco may not be obvious to children or those familiar with other legitimate manually harvested agricultural products like fruits and coffee. Second, residual moisture or water on the surface of the tobacco leaf significantly increases risk of GTS. Moisture on tobacco leaves from dew or rain may contain as much as 9 mg of dissolved nicotine per 100 mL of dew, roughly equivalent to the nicotine content of six average cigarettes.17 On a humid day, especially after a recent rain, the average field worker may be exposed to as much as 600 mL of dew. Gehlbach et al. found that sweat wrung from shirts worn by workers while harvesting tobacco contained up to 98 μg/mL of nicotine.17 Children may not be aware of the substantially increased risk of GTS that a slight rain or heavy dew may cause. Third, tolerance to nicotine, usually by being a long-time cigarette smoker, is believed to develop with chronic exposure.17,18 Since children are less likely to have an established smoking habit than adults, they are less likely to have developed tolerance to nicotine. Some studies are consistent with this assertion. Ballard et al. found an increased risk of GTS with younger age (odds ratio [OR]=3.1; 95% confidence interval [CI]=1.4, 7.0).7 Age was not, however, a risk factor for GTS in a study by Arcury et al.19 But these investigators did find an inverse relationship between years of experience working in tobacco and risk of GTS, with an estimated OR of 2.86 for workers having one year of experience harvesting tobacco compared with those that had five years of experience.19 Finally, some varieties of tobacco are harvested in a way that requires close and prolonged contact between skin and the plant, increasing the risk for GTS.
Tobacco production tasks and GTS
Of the tasks involved in tobacco production, two in particular raise a worker’s risk for GTS: topping and harvesting. In the United States, children frequently perform both tasks. “Topping” involves removing the flower from the growing plant to encourage greater root growth, leaf weight, and nicotine content at harvest. To “top,” workers walk through rows of tobacco plants and snap off the flowers by hand. As one would expect, workers have nearly constant contact with tobacco leaves as they perform this task.
Exposure to mature tobacco leaves varies by the type of tobacco being grown. Flue-cured tobacco, which is dried in a heated room or container, is harvested one leaf at a time over several progressive stages as the leaves ripen. Workers walk through rows of tobacco plants and reach down along the stalks to snap off individual leaves. With this type of harvesting, additional skin contact occurs because, as a worker advances through a row, the picked leaves often are held between the worker’s free arm and chest until no more leaves can be carried. Over a six- to eight-week period, three to 10 “trimmings” are completed for each field.
Burley tobacco, which is naturally air-dried in a barn, is harvested as a whole stalk and requires workers to grasp the stalks of large plants (six to eight feet tall) as they cut them at their bases. Each plant’s stalk is then impaled on a long stake or spear. The sticks are set upright in the field, and the plants are placed upside down to dry for about three days, after which they are transported to a barn for air curing. Normally, tobacco is housed during dry weather, but if it rains during this curing period, workers will load the tobacco onto wagons and house the plants to prevent them from being damaged. If the tobacco is wet, workers are at increased risk of dermal absorption of nicotine.
GTS ETIOLOGY AND PHYSIOLOGY
GTS is caused by dermal absorption of nicotine that has dissolved in water on the surface of the tobacco leaf.6,17,18,20,21 Physical exercise and high ambient temperatures can increase absorption of nicotine, thereby increasing plasma nicotine concentrations by 30% to 45%.22,23 In the United States, tobacco is usually harvested in late August or early September, when the ambient temperature is high. The combination of high ambient temperatures and hard physical labor shunts blood to the skin to help lower body temperature. The resultant increase in surface blood flow also significantly increases dermal absorption of nicotine. One study found about four times as much cotinine (a nicotine metabolite in urine) in tobacco workers as in a non-smoking control group that was given three cigarettes to smoke.17
Compared with adults, children may be especially vulnerable to GTS because their body size is small relative to the dose of nicotine absorbed, they lack tolerance to the effects of nicotine, and they lack knowledge about the risks of harvesting tobacco, especially after a recent rain. Without an awareness of the causes of GTS, children may fail to take effective precautions when handling green tobacco.
CASE HISTORIES OF GTS IN KENTUCKY
Although rarely life-threatening, GTS can be a frightening experience for a child, with sufferers attesting that the sickness made them feel, in their words, “like I was going to die.” We briefly describe three pediatric case histories of GTS reported to the Kentucky Regional Poison Center. Kentucky is the second largest tobacco-producing state in the United States. The Poison Center serves all 120 counties of Kentucky, with its population of 4.1 million residents. Each year the Center manages more than 47,000 human poisoning cases both in children and adults from thousands of toxic substances, including nicotine.
Case one
A 12-year-old boy worked on the family farm harvesting tobacco for 6.5 hours one day in August, along with other family members and another 12-year-old boy. The weather was humid, raining throughout the day, with a temperature of 31° C (88° F). Both boys stopped working and left the fields because of dizziness, nausea, and a feeling of weakness. At home over the next three hours, one boy had multiple episodes of vomiting, increased dizziness, headache, pallor, and muscle weakness. He was given a bath and oral fluids by his mother without relief of symptoms. He was then taken to the hospital emergency department (ED) where he received intravenous fluids and antiemetics. After four hours, he was discharged home. The following morning he was able to tolerate solid food and the muscle weakness had resolved. However, he developed a raised rash on his chest, abdomen, and legs, the locations of greatest contact with the tobacco plant. He was administered an antihistamine, and the rash resolved.
Case two
A 14-year-old boy worked in the fields harvesting tobacco in August. The weather was humid, raining sporadically throughout the day, with a temperature of 34° C (94° F). He left the fields to return home because of nausea, dizziness, and a feeling of weakness. At home, he vomited several times and was put to bed by his mother. While in bed, the boy experienced a grand mal seizure, but later regained consciousness. In the ED, he was treated with an antiemetic and intravenous fluids. A computerized tomography (CAT) scan of the head and electroencephalogram (EEG) were normal. He was observed in the ED for four hours without further seizures and with resolution of other symptoms, and was discharged home.
Case three
Thirteen Latino migrant field workers, including three workers ages 15, 16, and 17, arrived in the ED in August six hours after they stopped working in tobacco fields. The weather was humid, raining sporadically throughout the day, with a temperature of 33° C (91° F). All 13 workers experienced worsening and persistent vomiting, headache, dizziness, and weakness throughout the evening. In the ED, five patients, including two of the young workers, experienced bradycardia, with heart rates between 43 and 54 beats per minute. All were treated with intravenous fluids and antiemetics and discharged after six hours of observation.
DISCUSSION
GTS is an understudied and preventable occupational poisoning in children and adolescents. Our hope is that this short review will raise awareness of the causes of GTS, promote prevention efforts to reduce GTS, and stimulate further surveillance and research on this unique toxic agricultural exposure. GTS was first reported in children in 1970, and the few studies published since then were conducted at least a decade ago in the mid-1990s.7,8,24,25 Renewed efforts are needed to better characterize GTS in children in the United States and, especially, in large tobacco-producing nations in the developing world. We encourage researchers to include pediatric cases in their studies of GTS. One source of GTS data, information collected routinely by U.S. poison control centers, is often readily available.
Almost 95% of worldwide tobacco production occurs outside the United States, so special efforts should be made to document the occurrence of pediatric GTS cases in other countries, especially in China, Brazil, India, and Malawi—countries that collectively produce more than 60% of the world’s tobacco.2 It is likely that the current absence of findings detailing pediatric GTS cases in the developing world is more a function of lack of surveillance and reporting than an absence of cases.
Several questions remain unanswered about pediatric GTS in the developing world, such as the progression of symptoms among affected children; how GTS varies in intensity, frequency, and duration by climate and season; and what treatment options and prevention strategies are in place. Although U.S. children with GTS may have ready access to primary care, emergency, and poison center services, this is not as likely for children in developing nations. Ideally, the best approach to preventing GTS is keeping children out of tobacco production altogether. In the United States, the economics of family-operated tobacco farms makes this goal difficult to achieve. In developing countries, this goal is equally challenging, if not more so. If children are to work in tobacco farming, prevention strategies must include efforts to educate children, parents, farm managers, and farm owners about preventing GTS. One straightforward prevention message that could be promoted is equating working in a field of wet tobacco with working in a field that has recently been sprayed with pesticides—both situations can be hazardous to workers’ health, and both should be avoided until it is safe to enter the fields.
GTS prevention strategies recommended for adults could be adapted for children. Protective clothing such as rain gear and water-tight gloves, measures that have been cited in other studies as precautions adult tobacco workers should adopt,6,26 could also be adopted by child workers. An obvious requirement of wearing such impermeable gear, however, would be evaluating the dangers workers face from heat exhaustion and dehydration in regions with high heat and humidity. Additionally, the U.S. Environmental Protection Agency’s Worker Protection Standard could be revised to address nicotine toxicity in wet tobacco fields.
Clinicians and public health officials and agencies need to become more knowledgeable about the causes of GTS and its signs and symptoms, as the effects of acute nicotine poisoning might be mistaken for those of pesticide poisoning or heat exhaustion.27
Finally, green tobacco sickness is yet another public health issue that arises from using child labor in agriculture.
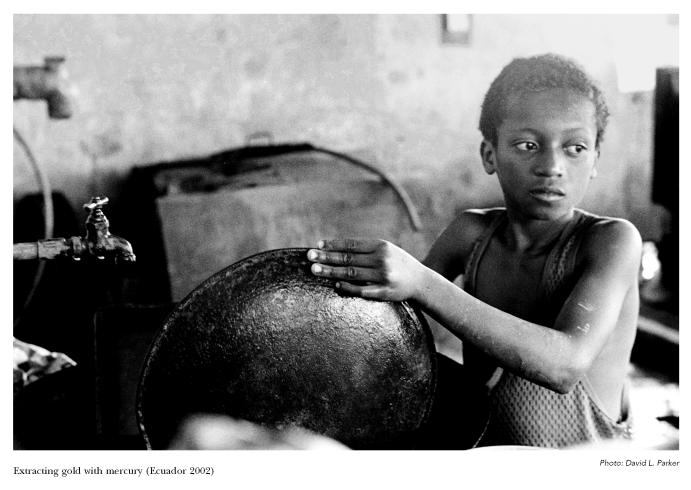
Extracting gold with mercury (Ecuador 2002)
REFERENCES
- 1.Food and Agriculture Organization (UN) Higher world tobacco use expected by 2010—growth rate slowing down. [[cited 2005 July 11]]. Available from: URL: http://www.fao.org/english/newsroom/news/2003/26919-en.html.
- 2.Department of Agriculture (US), Foreign Agricultural Service. World’s leading unmanufactured tobacco producing, trading and consuming countries. [[cited 2005 July 7]]. Available from: URL: http://www.fas.usda.gov/tobacco/circular/2004/082004/TBL1.PDF.
- 3.Pugh KJ, Pienkowski D, Gorczyca JT. Musculoskeletal trauma in tobacco farming. Orthopedics. 2000;23:141–3. doi: 10.3928/0147-7447-20000201-14. [DOI] [PubMed] [Google Scholar]
- 4.Trapé-Cardoso M, Bracker A, Grey M, Kaliszewski M, Oncken C, Ohannessian C, et al. Shade tobacco and green tobacco sickness in Connecticut. J Occup Environ Med. 2003;45:656–61. doi: 10.1097/01.jom.0000071504.96740.ab. [DOI] [PubMed] [Google Scholar]
- 5.Hipke ME. Green tobacco sickness. South Med J. 1993;86:989–92. doi: 10.1097/00007611-199309000-00002. [DOI] [PubMed] [Google Scholar]
- 6.McBride JS, Altman DG, Klein M, White W. Green tobacco sickness. Tob Control. 1998;7:294–8. doi: 10.1136/tc.7.3.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ballard T, Ehlers J, Freund E, Auslander M, Brandt V, Halperin W. Green tobacco sickness: occupational nicotine poisoning in tobacco workers. Arch Environ Health. 1995;50:384–9. doi: 10.1080/00039896.1995.9935972. [DOI] [PubMed] [Google Scholar]
- 8.McKnight RH, Levine EJ, Rodgers GC. Detection of green tobacco sickness by a regional poison center. Vet Hum Toxicol. 1994;36:505–10. [PubMed] [Google Scholar]
- 9.Lyons-Barrett MT. Child labor in commercialized agriculture, 1890–1966 [dissertation] Lincoln (NE): University of Nebraska–Lincoln; 2002. [Google Scholar]
- 10.Department of Labor (US) Child labor in representative tobacco-growing areas. Washington: Government Printing Office; 1926. Children’s Bureau Publication No.: 155. [Google Scholar]
- 11.Wilk VA. Health hazards to children in agriculture. Am J Ind Med. 1993;24:283–90. doi: 10.1002/ajim.4700240305. [DOI] [PubMed] [Google Scholar]
- 12.van Willigen J, Eastwood SC. Tobacco culture: farming Kentucky’s burley belt. Lexington (KY): University Press of Kentucky; 1998. [Google Scholar]
- 13.Browning SR, Westneat SC, Donnelly C, Reed D. Agricultural tasks and injuries among Kentucky farm children: results of the Farm Family Health and Hazard Surveillance Project. South Med J. 2003;96:1203–12. doi: 10.1097/01.SMJ.0000082014.94642.06. [DOI] [PubMed] [Google Scholar]
- 14.National Children’s Center for Rural and Agricultural Health and Safety. North American guidelines for children’s agricultural tasks. [[cited 2005 July 7]]. Available from: URL: http://www.nagcat.org.
- 15.Marlenga B, Pickett W, Berg RL. Evaluation of an enhanced approach to the dissemination of the North American Guidelines for Children’s Agricultural Tasks: a randomized controlled trial. Prev Med. 2002;35:150–9. doi: 10.1006/pmed.2002.1051. [DOI] [PubMed] [Google Scholar]
- 16.Eliminating child labor, ECLT Foundation. [[cited 2005 July 7]]. Available from: URL: http://www.eclt.org.
- 17.Gehlbach SH, Perry LD, Williams WA, Freeman JI, Langone JJ, Peta LV, Van Vunakis H. Nicotine absorption by workers harvesting green tobacco. Lancet. 1975;1:478–80. [PubMed] [Google Scholar]
- 18.Onuki M, Yokoyama K, Kimura K, Sato H, Nordin RB, Naing L, et al. Assessment of urinary cotinine as a marker of nicotine absorption from tobacco leaves: a study on tobacco farmers in Malaysia. J Occup Health. 2003;45:140–5. doi: 10.1539/joh.45.140. [DOI] [PubMed] [Google Scholar]
- 19.Arcury TA, Quandt SA, Preisser JS, Norton D. The incidence of green tobacco sickness among Latino farmworkers. J Occup Environ Med. 2001;43:601–9. doi: 10.1097/00043764-200107000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Gehlbach SH, Williams WA, Freeman JI. Protective clothing as a means of reducing nicotine absorption in tobacco harvesters. Arch Environ Health. 1979;34:111–4. doi: 10.1080/00039896.1979.10667379. [DOI] [PubMed] [Google Scholar]
- 21.Ghosh SK, Parikh JR, Gokani VN, Kashyap SK, Chatterjee SK. Studies on occupational health problems during agricultural operation of Indian tobacco workers: a preliminary report. J Occup Med. 1979;21:45–7. [PubMed] [Google Scholar]
- 22.Homsy W, Yan K, Houle JM, Besner JG, Gossard D, Pierce CH, Caillé G. Plasma levels of nicotine and safety of smokers wearing transdermal delivery systems during multiple simultaneous intake of nicotine and during exercise. J Clin Pharmacol. 1997;37:728–36. doi: 10.1002/j.1552-4604.1997.tb04360.x. [DOI] [PubMed] [Google Scholar]
- 23.Vanakoski J, Seppala T, Sievi E, Lunell E. Exposure to high ambient temperature increases absorption and plasma concentrations of transdermal nicotine. Clin Pharmacol Ther. 1996;60:308–15. doi: 10.1016/S0009-9236(96)90057-0. [DOI] [PubMed] [Google Scholar]
- 24.Ross MP, Revolinski D, Taurman L, Rodgers GC, McKnight RH, Levine EJ. Detection of a pediatric occupational poisoning in Kentucky. Vet Hum Toxicol. 1994;36:360. [Google Scholar]
- 25.McKnight RH, Koetke CA, Donnelly C. Familial clusters of green tobacco sickness. J Agromed. 1996;3:51–9. [Google Scholar]
- 26.Department of Health and Human Services (US) NIOSH issues warning to tobacco harvesters. NIOSH Update. Atlanta: CDC; 1993. July 8. DHHS (NIOSH) Publications No.: 93-115. [Google Scholar]
- 27.Swinker M, Meredith JT. A seizure in the tobacco field: green tobacco sickness. NC Med J. 2000;61:390–2. [PubMed] [Google Scholar]