In 1903, the United States took possession of the Isthmus of Panama with the intention of building a canal, a monumental feat that required expertise in both large-scale structural engineering and public health. For the most part, the story of sanitation in the Canal Zone during the era of construction (1904–1914) has focused on the medical arm of the Isthmian Canal Commission (ICC), established by the federal government to oversee the massive task of carving a waterway out of the Central American tropics, and on the activities and personality of William Crawford Gorgas, the army doctor who served as Chief Sanitary Officer.1,2 Yet the Public Health Service (PHS) was integral to American sanitation in Panama. PHS physicians managed quarantine operations, oversaw the eradication of rats and mosquito larvae, superintended hospitals, attended patients, and staffed laboratories. Furthermore, in 1915 the PHS put the lessons learned and techniques developed in the Canal Zone on display at the Panama-Pacific International Exposition (PPIE), mounting an impressive exhibit that was viewed by millions of Americans.3,4
This Public Health Chronicles highlights the forgotten history of the PHS in Panama, paying particular attention to Claude Connor Pierce, who was the first sanitary officer sent to the Canal Zone in January 1904, just in time to observe the lowering and replacement of the French flag with the U.S. flag.5 Born in Tennessee in 1878, Pierce received his degree from Chattanooga Medical College and joined the PHS in the lower ranks in 1900 after serving in the Spanish-American War. He was sent to Panama in 1904, where he worked his way up from assistant to senior surgeon, first acting as a quarantine officer and then, starting in 1913, as the superintendent of Colón Hospital.6,7,8 Afterward, Pierce was transferred to San Francisco, the site of the PPIE, to direct sanitary efforts and organize the PHS display. During his journey from the ports of Panama to the San Francisco embarcadero, Pierce worked alongside many PHS physicians, including Henry Rose Carter, who advanced the understanding of mosquito-borne ailments and strategies for their eradication (and was appointed assistant Surgeon General in 1915), and James C. Perry, long-time quarantine officer who penned some of the first U.S. reports on health conditions in the cities of Panama and Colón. This small yet dedicated group of PHS officers greatly facilitated the construction of the canal. At the same time, they helped to shape the emergent field of tropical medicine on a strategically located isthmus that straddled an expanding U.S. presence in the Caribbean and Pacific.
SHARING THE BURDEN OF PUBLIC HEALTH IN PANAMA
Like France and Britain, the United States was in a mood of colonial expansion at the turn of the nineteenth century, claiming the islands of Puerto Rico, Cuba, and the Philippines in the Spanish-American War of 1898, and also commanding Hawaii, Guam, and Samoa. In 1903, after Panama seceded from Colombia, the United States added the Canal Zone, an area about 10 miles wide and 50 miles long, to its holdings. Like Guam and Samoa, the Canal Zone was an “unorganized possession,” a status that granted the isthmus virtually no political autonomy.2 Indeed, U.S. dominion over the Zone was nearly absolute and extended into the young republic of Panama.
One of the most important aspects of isthmian occupation was sanitary control, which Gorgas had mastered in Havana, Cuba, from 1900 to 1902, first in response to a typhoid, then a yellow fever, outbreak. This experience illustrated that after winning on the battlefield, the maintenance of political order often entailed a sanitary offensive capable of neutralizing an array of disruptive pathogens.9 This lesson was perhaps nowhere more applicable than in Panama, where diseases whose etiologies were not fully grasped in the 1880s—above all, yellow fever and malaria—had decimated the French Canal Company and taken the lives of approximately 20,000 able-bodied workers. Fortunately for Gorgas and the ICC, the United States had timing on its side. The previous 20 years had seen the emergence of tropical medicine, a field that combined bacteriology, microscopy, parasitology, and entomology to elucidate the transmission patterns of diseases prevalent in hot and humid climates, usually via insect and animal vectors.10 Most apposite to the Panama Canal, experiments conducted by European and American scientists had confirmed the mosquito species responsible for yellow fever and malaria (and in the latter case, microscopically identified the pathogenic plasmodium carried in the gut of the Anopheles host). Moreover, these medical men, such as Gorgas and Ronald Ross, the Nobel Prize-winning British physician who performed his laboratory work in India, had devised effective methods of mosquito eradication that revolved around the destruction of larvae and “wrigglers,” and the elimination of any source of standing water.10,11
Once installed in Panama, the ICC knew that the erection of a locks canal across the rocky and mosquito-infested terrain could not proceed without the implementation of a far-reaching and hyper-vigilant brand of sanitation capable of protecting the majority of laborers from deadly scourges. Thus, Gorgas and the ICC assumed total control of all sanitary matters in the Canal Zone. To guarantee that the U.S. jurisdiction would encompass Panama's two coastal cities, in early 1904 Panama's president decreed that the ICC was “hereby authorized to assume charge of all that relates to the sanitation and health in the cities of Colon and Panama.”12 Concurrently, PHS quarantine officers were instructed to “exercise their authority and to dictate the sanitary measures for all ships leaving said ports for the Republic of Panama exactly in the same manner as they are instructed to do for ships bound for the United States.”13
These dicta transformed the Canal Zone and environs into a working laboratory where U.S. health officials had an enormous amount of power to study disease and enforce strategies of containment and eradication. PHS officers took advantage of this arrangement and were the first American representatives to gather data on patterns of health and disease in preparation for the start of dredging and construction. For example, several months before Gorgas had assembled his sanitary corps, Pierce filed a report on Panama City and its surrounding areas. He described the city's shoddy sewage infrastructure of partially exposed underground channels and its nonexistent water system; included demographic and vital statistics drawn from municipal records; and detailed the architecture and capacities of the local hospitals, including the 700-bed Ancón hospital, which was once the clinical centerpiece of the French Canal Company. Pierce bemoaned the lack of a functional quarantine station and sterilization equipment and stressed the urgency to create a station immediately because “Panama is the gateway from the whole world to the west coast of America, from San Francisco to Valparaiso.”14
Several dispatches written by PHS physician James C. Perry followed Pierce's report. Describing Colón's urban districts, Perry evinced dismay with the conditions of the city's poorer neighborhood, which extended over a swampy area: “These habitations are filthy in the extreme, and it is difficult to understand how people can live in such unsanitary surroundings with any semblance of health.”15 Like many of his contemporaries, Perry often saw cleanliness and dirt, health and disease as reflections of racial differences in personal and public hygiene, wherein dark-skinned inhabitants tended to be dirtier and more unkempt than their fairer counterparts. Such prejudices constituted the ugly underside of tropical medicine, which in its initial phases partook of the colonialist belief that it was white man's burden to lift up, civilize, and sanitize the natives.16 For Perry, this mission involved making Colón into a “healthy tropical city” through the two-pronged approach of sanitary engineering and hygienic education.17 In keeping with the combination of hubris and idealism typical among his medical peers, Perry asserted, “Panama offers a fruitful field for the scientific work of the sanitarian” and foresaw that the PHS and ICC's work would “teach a lesson to the world, by showing what can be accomplished in pest-ridden localities in the Tropics by modern preventive medicine.”18
When Gorgas formed his sanitation team in the summer of 1904, he appointed Perry as Chief Quarantine Officer and Pierce as Quarantine Officer at Cristóbal. They remained in Panama for the duration of construction and were joined by additional PHS physicians who collaborated with the ICC. For instance, Henry Rose Carter, who determined the extrinsic incubation period of yellow fever and produced a series of authoritative papers on the epidemiology of and eradication methods for mosquito-borne diseases, served as Director of Hospitals.19,20 About one dozen other PHS physicians served alongside this trio from 1904 to 1914, many fulfilling temporary rotations at the Colón, Cristóbal, and Bocas del Toro quarantine stations.
For PHS physicians, to serve in the Canal Zone was an exciting opportunity to advance the emergent field of tropical medicine and implement effective prophylactic health measures. In addition to quarantine duty, PHS officers pursued clinical studies in the hospital wards, aided urban and rural sanitation campaigns, and participated in the mosquito brigades that marched through Colón, Panama City, and along the cantons that snaked through the Canal Zone.21,22 As uniformed officers, PHS officers were treated as equals by their ICC counterparts and could operate in a fairly unhindered fashion and without the frictions among local, state, and federal public health agencies that were common in the continental United States in the early twentieth century.23
PUTTING THE LESSONS OF PANAMA ON DISPLAY
Convened in San Francisco in 1915, the Panama-Pacific International Exposition (PPIE) triumphantly celebrated the opening of the Panama Canal.24 Much of the fanfare focused on the U.S. sanitary campaign and acclaimed Gorgas for having tamed the tropics and transformed a pesthole into a paradise. Much in the same way that the PHS assisted Gorgas in Panama, the PHS maintained the health infrastructure at the PPIE. From his superintendence at Colón Hospital, Pierce was sent to San Francisco to serve as the PPIE's Chief Sanitary Officer and institute health procedures on the fairgrounds. Not surprisingly, he replicated the hyper-vigilant methods of sanitation he had practiced for more than 10 years in Panama. For example, one of Pierce's first undertakings—realized as the PPIE's grandiose halls, pavilions, and domes were being raised—was a comprehensive medical census of all individuals on the premises according to age, sex, and occupation. In addition, Pierce conducted hookworm and trachoma evaluations and, if needed (as mandated by a recently-passed PHS regulation), smallpox vaccination.25
During the 10-month-long exposition, Pierce and his underlings surveyed the buildings, scrutinized concession stands, hung anti-spitting signs on buildings, and assessed the public bathrooms, all the while searching for vermin, locating pools of standing water, and regularly testing the drinking supply for bacteria. In a typical monthly report, Pierce indicated that he applied borax to fertilized soil to discourage fly breeding; discontinued and oiled water fountains to destroy mosquito larvae; inspected, in total, 244 concessions and structures; and re-inspected the avenues, stockyards, and the fair's rides and booths more than 600 times—ultimately pinpointing 125 problems that needed fixing.26 When Pierce identified sick individuals, he sent them to the Exposition Hospital, which was run by the PHS and operated as a critical care center and an exhibit. It boasted four wards, an operating room, anesthetizing room, waiting room, x-ray machine, a laboratory, electric massage machines, urine and blood analysis kits, two spiffy Cadillac ambulances, and close to 15 personnel, including several attending physicians and nurses, technicians, orderlies, and a maid.27,4 While the PPIE was being built, the Exposition Hospital tended to injured workers, and from the day the first brick was laid to the last day of demolition, more than 7,000 people were treated or hospitalized, sometimes repeatedly, by the PHS.25 The PHS Exposition Hospital also fostered the circulation of modern medical thought at its library, where professionals could peruse a collection of more than 1,000 books or borrow from a stereopticon archive of 8,000 lantern slides, many produced during health campaigns in the field.25
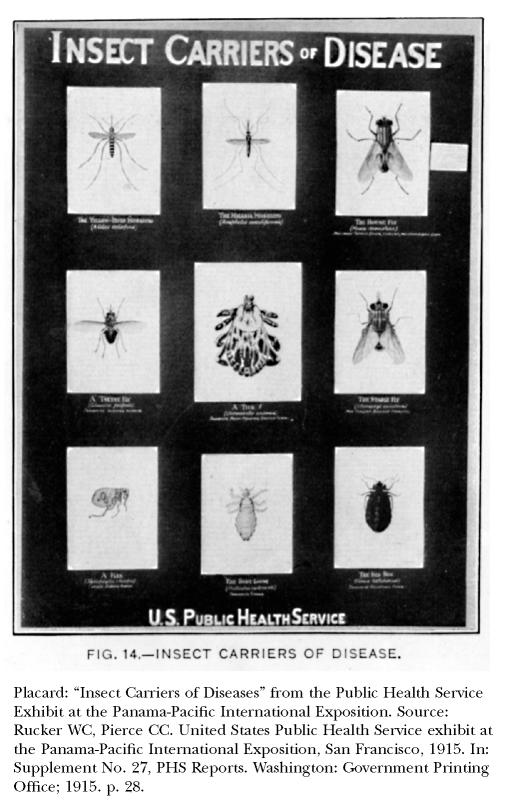
The PHS's crowning achievement at the PPIE was an impressive set of exhibits, six of which won medals, including one gold medal and one grand prize, from the exposition's international jury committee.28 These didactic displays detailed the organization and mission of the PHS, illustrated epidemiological patterns and surveillance techniques, and, recognizing the agency's contribution to tropical medicine, even featured a habitat of living, breeding mosquitoes. Pierce oversaw all of the PHS exhibits, the largest of which covered 5,250 square feet and aimed to present in a “popular and comprehensive way, easily understood by the general public, the latest methods of preventing the common communicable diseases.”3 This exhibit highlighted more than a dozen conditions, including typhoid, tuberculosis, rabies, Rocky Mountain spotted fever, and syphilis, and especially sought to underscore that insects could be dangerous disease carriers. Through negative and positive examples of health prophylaxis, the PHS instructed viewers of the exhibit in the basics of bacteriology and made a hitherto concealed universe of germs visible through magnified drawings of microorganisms and the anthropomorphism of creatures such as the liver fluke and whipworm. The magnified bacilli, larger-than-life insects and helminthes, and placards loaded with mortality and morbidity imparted information about newly identified disease vectors, both common and obscure, and greatly increased the layperson's familiarity with the consolidating field of tropical medicine.
REMEMBERING THE PHS IN PANAMA
The PHS has not received credit for its medical contributions to the building of the canal, whether in the clinic, hospital, laboratory, streets, or the jungle. Undoubtedly, PHS physicians improved the overall health of the canal laborers and tended to those hospitalized. They also gathered epidemiological, entomological, and bacteriological knowledge that helped to refine models for disease eradication, particularly for future campaigns against mosquito-borne ailments in Latin America.29,30 Nevertheless, the status of the Panama Canal as a colonial territory meant that PHS officers operated under the authority of an occupying power, an arrangement that was at odds with the agency's identity as a national body concerned with foreign health insofar as it included immigrant inspection and quarantine regulations. Furthermore, as practitioners of tropical medicine in a colonial setting, PHS physicians in Panama helped to perpetuate a hierarchical health system that was structured starkly by racism. For it was the minority of white laborers, paid in gold, not the diverse majority of black laborers (frequently hailing from Barbados and Jamaica), paid in silver, who received premier clinical care in the Canal Zone and whose homes benefited from mosquito screens.1
Eventually, the strategies employed to protect gold workers from tropical diseases were stripped of their explicit racial conceits and implemented in health campaigns across many regions of the world. Subsequent generations of PHS officers would reject the prejudicial values embedded in U.S. public health activities in Panama. Nevertheless, the history of U.S. sanitation in the Panama Canal reveals how significant medical developments can be intertwined with disturbing—and from today's standards, unethical—approaches to health care delivery. Precisely because of this uneasy combination, it is important to learn from the PHS experience in Panama, which Americans were already beginning to do at the PPIE in 1915.
Portrait of Claude C. Pierce. Source: Jackson FE & Sons. The makers of the Panama Canal. New York: F.E. Jackson & Sons; 1911. p. 91.
Portrait of James C. Perry. Source: Jackson FE & Sons. The makers of the Panama Canal. New York: F.E. Jackson & Sons; 1911. p. 37.
Placard: ”Insect Carriers of Diseases“ from the Public Health Service Exhibit at the Panama-Pacific International Exposition. Source: Rucker WC, Pierce CC. United States Public Health Service exhibit at the Panama-Pacific International Exposition, San Francisco, 1915. In: Supplement No. 27, PHS Repots. Washington: Government Printing Office; 1915. p. 28.
References
- 1.McCullough D. New York: Simon & Schuster; 1977. The path between the seas: the creation of the Panama Canal, 1870–1914. [Google Scholar]
- 2.Major J. New York: Cambridge University Press; 1993. Prize possession: the United States and the Panama Canal, 1903–1979. [Google Scholar]
- 3.Rucker WC, Pierce CC. PHS Reports. Supplement No. 27. Washington: GPO; 1915. United States Public Health Service exhibit at the Panama-Pacific International Exposition, San Francisco, 1915. [Google Scholar]
- 4.Todd FM. 5 vols. New York: G.P. Putnam's Sons; 1921. The story of the exposition: being the official history of the international celebration held at San Francisco in 1915 to commemorate the discovery of the Pacific Ocean and the construction of the Panama Canal. [Google Scholar]
- 5.Jackson FE & Sons. Washington: GPO; 1914. Official list of commissioned and other officers of the United States Public Health Service. The makers of the Panama Canal. New York: F.E. Jackson & Sons; 1911. Public Health Service. [Google Scholar]
- 6.vol. 2. Chicago: The A.N. Marquis Company; 1950. Who was who in America. [Google Scholar]
- 7. “Personal,” Canal Record 7. December 10, 1913. Bancroft Library, University of California at Berkeley.
- 8.Cirillo VJ. New Brunswick: Rutgers University Press; 2004. Bullets and bacilli: the Spanish-American war and military medicine. [Google Scholar]
- 9.Worboys M. Tropical diseases. In: Bynum WF, Porter R, editors. Companion encyclopedia of the history of medicine. vol. 1. New York: Routledge; 1993. pp. 512–36. [Google Scholar]
- 10.Ross R. New York: Longmans, Green; 1902. Mosquito brigades and how to organize them. [Google Scholar]
- 11.Washington: GPO; 1915. Feb 20, Report of the Chief Sanitary Officer of the Canal Zone. [Google Scholar]
- 12.Public Health Reports. Washington: GPO; 1904. Mar 4, Public Health Service. [Google Scholar]
- 13.Pierce CC. Public Health Reports. Washington: GPO; 1904. Feb 19, Sanitary report of Panama and vicinity; pp. 273–80. [Google Scholar]
- 14.Perry JC. Public Health Reports. Washington: GPO; 1904. Mar 4, Colon; pp. 351–6. [Google Scholar]
- 15.Anderson W. Immunities of empire: race, disease, and the new tropical medicine, 1900–1920. Bull Hist Med. 1996;70:94–118. doi: 10.1353/bhm.1996.0002. [DOI] [PubMed] [Google Scholar]
- 16.Perry JC. Public Health Reports. Washington: GPO; 1904. Mar 18, A study of the vital statistics as regards prevailing diseases and mortality, of Colon, Republic of Panama, for the year 1903; pp. 467–75. [Google Scholar]
- 17.Perry JC. Public Health Reports. Washington: GPO; 1904. Apr 15, A study of the vital statistics as regards the prevailing diseases and mortality of the city of Panama for the year 1903; pp. 657–64. [Google Scholar]
- 18.Carter HR. Medical Record. Washington: GPO; 1909. Jul 10, Notes on the sanitation of yellow fever and malaria. From Isthmian Experience; pp. 1–14. [Google Scholar]
- 19.Carter HR. Public Health Reports. Supplement No. 19. Washington: GPO; 1914. Yellow fever: its epidemiology, prevention, and control. [Google Scholar]
- 20. Isthmian Canal Commission. Annual reports of the Isthmian Canal Commission. Washington: GPO; 1904–1914.
- 21. Medical Association of the Isthmian Canal Zone. Proceedings, vols. i-ix. Mount Hope: Canal Zone; 1908–1916.
- 22.Marcus Al. Disease prevention in America: from a local to a national outlook, 1880–1910. Bull Hist Med. 1979;53:184–203. [PubMed] [Google Scholar]
- 23.Brechin G. Imperial San Francisco: urban power, earthly ruin. Berkeley: University of California Press; 1999. pp. 245–79. [Google Scholar]
- 24. Annual report of the Surgeon General of the Public Health Service of the United States. Washington: GPO; 1915.
- 25. Pierce CC to Surgeon General, May 8, 1915, Papers of the Panama-Pacific International Exposition, CA 190, carton 86. [Google Scholar]
- 26.Woodward RM. Bancroft Library: University of California at Berkeley; 1913. Jun 4, Letter Re: Hospital service at grounds. Papers of the Panama-Pacific International Exposition, CA 190, carton 23. [Google Scholar]
- 27.Bancroft Library: University of California at Berkeley; 2025. International Jury Awards. Papers of the Panama-Pacific International Exposition, CA 190, carton 51. [Google Scholar]
- 28.Howard LO. A fifty year sketch history of medical entomology and its relation to public health. In: Ravenel MP, editor. A half century of public health. New York: American Public Health Association; 1921. pp. 412–38. [Google Scholar]
- 29.Cueto M. Cycles of eradication: the Rockefeller Foundation and Latin American Public Health, 1918–1940. In: Weindling P, editor. International health organisations and movements, 1918–1939. New York: Cambridge University Press; 1995. pp. 222–43. [Google Scholar]