SYNOPSIS
Objectives
To examine multiple dimensions of socioeconomic status and breastfeeding among a large, random sample of ethnically diverse women.
Methods
This study used logistic regression analysis to examine the influence of a range of socioeconomic factors on the chances of ever breastfeeding among a stratified random sample of 10,519 women delivering live births in California for 1999 through 2001. Measures of socioeconomic status included family income as a percentage of the federal poverty level, maternal education, paternal education, maternal occupation, and paternal occupation.
Results
Consistent with previous research, there was a marked socioeconomic gradient in breastfeeding. Women with higher family incomes, those who had or whose partners had higher education levels, and women who had or whose partners had professional or executive occupations were more likely than their counterparts to breastfeed. After adjustment for many potential confounders, maternal and paternal education remained positively associated with breastfeeding, while income and occupation were no longer significant. Compared with other racial or ethnic groups, foreign-born Latina women were the most likely to breastfeed.
Conclusions
The significant association of maternal and paternal education with breastfeeding, even after adjustment for income, occupation, and many other factors, suggests that social policies affecting educational attainment may be important factors in breastfeeding. Breastfeeding rates may be influenced by health education specifically or by more general levels of schooling among mothers and their partners. The continuing importance of racial/ethnic differences after adjustment for socioeconomic factors could reflect unmeasured socioeconomic effects, cultural differences, and/or policies in Latin American countries.
Breastfeeding is the healthiest way to feed an infant;1–4 however, many childbearing women never breastfeed. The Healthy People 2010 goal is for 75% of all U.S. women to breastfeed their infants in the early postpartum period.5 Data from several studies suggest that women of lower socioeconomic status (SES) are less likely to breastfeed their infants, both in the United States and elsewhere.6–19 However, few studies of breastfeeding and SES have used more than one dimension of socioeconomic status to examine more closely the factors most predictive of breastfeeding; some that have used both income and education have sampled primarily or only low-income women.10, 20 One broader study of women in a Boston group practice18 found that maternal education and household income were both significant in predicting breastfeeding initiation, but that education was more important than income. A population-based Canadian study19 found income and education to be approximately equally predictive of breastfeeding initiation.
Reasons for the association between breastfeeding and SES are likely complex. Differing aspects of SES may be associated with knowledge, attitudes, experiences, and beliefs leading a woman to a particular infant feeding choice. Maternal or paternal education may reflect more educated parents being more likely to search out information on the health aspects of infant feeding choices; knowledge of the benefits of breast-feeding has been shown to predict breastfeeding.21 Paternal and maternal income have been shown to affect breastfeeding in opposite directions, perhaps since maternal income is associated with employment, which may detract from breastfeeding.7 In general, income may influence breastfeeding by being a marker of knowledge and attitudes and because women of higher income may be better able to afford feeding supplies. (The ability to afford formula is inversely associated with use of formula; however, public programs such as Women, Infants and Children [WIC] allow poor women to purchase formula, which may serve to blunt any direct effect of income on feeding choice.) Maternal employment has been shown to decrease breastfeeding;22–26 however, in Australia, paternal employment has been positively associated with breastfeeding.12 Employment may be an obstacle because of time away from the baby; Fein and Roe26 found that full-time, but not part-time, employment was negatively associated with breastfeeding initiation. Employment may also decrease breastfeeding because women in lower-status occupations may have more obstacles to expressing breast milk at work, or because women with hazardous occupations might be concerned their exposures might affect breast milk. Higher-SES women may also be more likely to have supportive workplace and/or home environments for breastfeeding. SES is associated with attitudes toward breastfeeding, which may reflect experience with a peer group or a health care provider whose opinions the mother values.27 Racial/ethnic disparities in breastfeeding may reflect unmeasured socioeconomic differences; 28 they may also reflect differing attitudes toward breastfeeding by different racial/ethnic groups. In addition, there may be breastfeeding policies and programs in the U.S. and elsewhere that have affected specific ethnic groups of women. Each of these measures may also be a marker for other components of SES.
Maternal race/ethnicity, which is associated with SES, has also been correlated with breastfeeding. Past studies have generally found that non-Hispanic white women are more likely than women in other racial and ethnic groups to breastfeed. 6, 7, 9 However, race/ethnic studies of breastfeeding have been somewhat limited. For example, breastfeeding rates among Asians and Pacific Islanders have not been examined closely. The impact of race/ethnicity on breastfeeding could reflect unmeasured socioeconomic differences as well as cultural differences or the impacts of policies and programs targeted at specific groups of women in the United States, or elsewhere for immigrant mothers.
Most past studies of race/ethnicity and breastfeeding have examined only two or three racial and ethnic groups, typically white, African American, and sometimes Hispanic;7, 8, 18, 27 U.S.-born and foreign-born Hispanics have rarely been examined separately. We used a large, population-based sample of California mothers to examine the simultaneous influence of a number of socioeconomic factors on breastfeeding in a racially and ethnically diverse population. We also adjusted for a number of additional variables (physical problems, pregnancy- and birth-related characteristics, other health-related characteristics, and demographic characteristics) that could potentially confound or mediate the relationships between socioeconomic factors and breastfeeding. We hypothesized that varying measures of SES would have differential effects on breastfeeding; specifically, that maternal variables would be more powerful predictors of breastfeeding than paternal variables, and that because of its role in health knowledge, maternal education would prove to have a greater influence on breastfeeding initiation than income or occupation.
METHODS
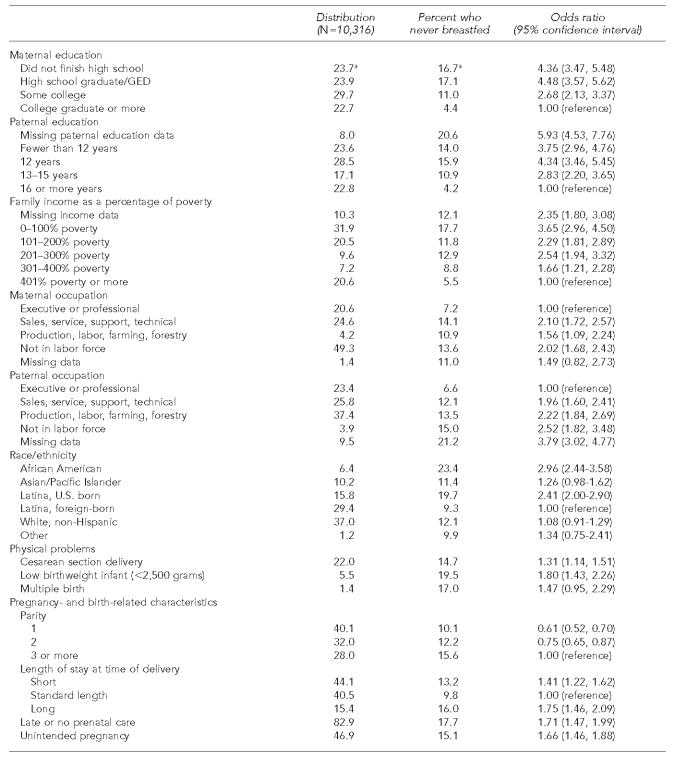
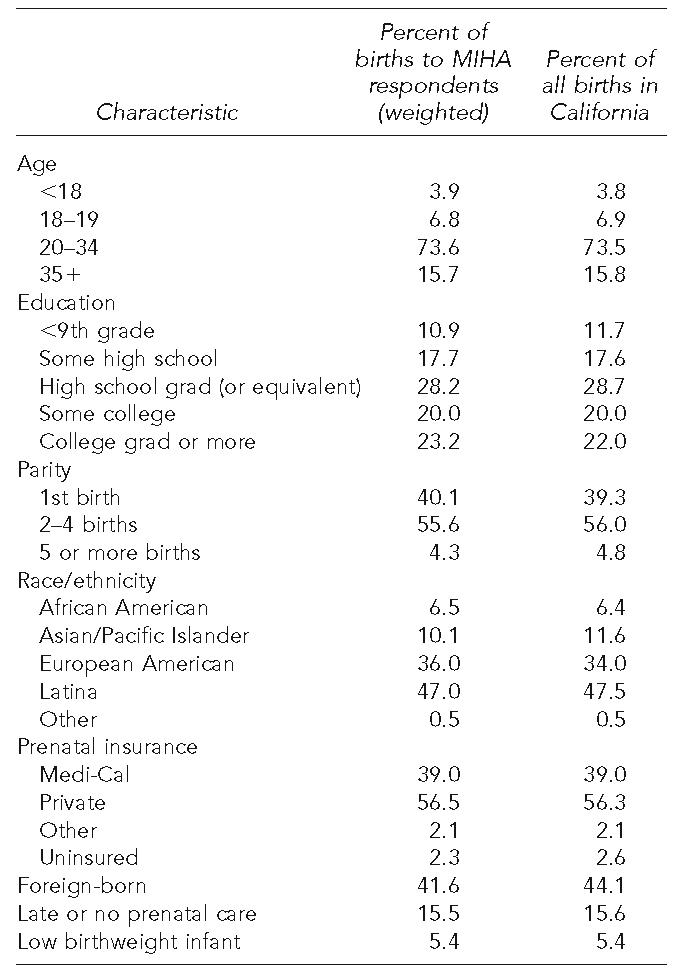
Data for this study were drawn from the California Maternal and Infant Health Assessment (MIHA) for 1999–2001. MIHA, a collaborative effort of the California Department of Health Services, Maternal and Child Health Branch, and researchers at the University of California, San Francisco, is an annual stratified random sample survey of childbearing women in California, similar to the Center for Disease Control and Prevention’s (CDC’s) Pregnancy Risk Assessment Monitoring System (PRAMS) survey.6 MIHA was approved by the Institutional Review Board at the California Department of Health Services, conforming to Declaration of Helsinki principles. MIHA’s purpose is to provide information on a range of issues in maternal and infant health needed to guide state programs and policies, including those affecting breastfeeding. Women are sampled from birth certificate data and are mailed the survey at 10–14 weeks postpartum; surveys were returned up to seven months after birth (median about 3.5 months). The survey excludes women who are not California residents, those under 15 years of age, and those whose names or addresses are missing from the birth certificate. In addition, only women with singletons, twins, or triplets are sampled; those with higher-order multiple births are excluded. MIHA is a mail survey with phone follow-up of nonrespondents, and is conducted in English and Spanish. The sample is stratified by maternal region of residence, race/ethnicity, and education, and African American women are oversampled. For each year, response rates to MIHA were between 70% and 72%, resulting in a sample size of about 3,500 women in each year whose characteristics were similar to those of all women giving birth in California during the same time periods (Table 1). There were 10,519 women in the MIHA samples from 1999–2001. For this study, 103 infants were excluded because questions on breastfeeding were not asked of mothers whose infants had died or who were no longer living with them, leaving 10,316 infants remaining in the survey.
Table 1.
Comparison of Maternal and Infant Health Assessment (MIHA) respondents and California childbearing women, 1999–2001
The MIHA survey asks several questions about breastfeeding, including whether the mother ever breastfed her infant and if so, for how long. For this study, logistic regression was used to examine the relationship between socioeconomic status and ever breastfeeding, adjusting for potential confounders.
SUDAAN29 was used to adjust for the complex sampling design of the MIHA survey. Among the 1999–2001 respondents, a total of 8,977 women said they had breastfed their infants at least once, while 1,339 said they had never breastfed the index child. Variables in the analyses were drawn from the MIHA survey, except for paternal education, maternal and paternal occupation, method of delivery, low birthweight, and maternal age, all of which were drawn from the birth certificate.
Maternal and paternal education, income, and maternal and paternal occupation were simultaneously included as the socioeconomic variables of interest in this study. Maternal education was categorized as did not finish high school, high school graduate/GED, some college, or college graduate or more. Paternal education was categorized as paternal education data missing or fewer than 12 years of education, 12 years, 13–15 years, or 16 or more years. Family income was categorized as no income data, income below or equal to the federal poverty line, 101–200% of the poverty line, 201–300% of poverty, 301–400% of poverty, or >400% of poverty. Maternal and paternal occupation were coded from the text fields of occupation on the birth certificate using SOIC occupational coding software30 and grouped into five categories: executive or professional; sales, service, technical, or support; farming, forestry, production, or construction; not in labor force (homemakers and students); and missing. Missing data were included as separate categories for the income, paternal education, and maternal and paternal occupation variables to maintain an adequate sample size and because previous analyses suggested that women whose partner’s data are missing, and those with missing income data, are likely to be of lower socioeconomic status.28 Correlations among the five socioeconomic measures were all highly statistically significant (p<0.0001). The correlation coefficients varied from 0.3325 for the correlation between maternal and paternal occupation to 0.6418 for the correlation between paternal education and paternal occupation. Maternal and paternal education had a correlation of 0.6144. The coefficient for the correlation between maternal or paternal education and family income was between about 0.56 and 0.58.
Race/ethnicity was categorized as African American/black; Asian/Pacific Islander; foreign-born Latina; U.S.-born Latina; white; and other/unknown. Foreign-born Latinas were used as the reference group for simplicity of presentation, as they had the highest breastfeeding rate.
A number of variables associated with socioeconomic status and breastfeeding could either confound or be mediators of the breastfeeding/SES relationship. Four primary groups of variables were examined: physical problems that might prevent or deter breastfeeding; pregnancy- and birth-related characteristics; other health-related characteristics; and demographic characteristics. The physical problems included method of delivery (Cesarean section or vaginal); whether the birth was multiple or not; and low birthweight (<2500 grams, 2500 grams or more), used rather than gestational age as birthweight data have greater validity than gestational age data. Pregnancy- and birth-related characteristics included parity (one, two, three, or more total live births); length of hospital stay after delivery (short: fewer than two nights for vaginal delivery or fewer than four nights for a Cesarean; standard: two nights for a vaginal and four nights for a Cesarean delivery; long: more than two nights for a vaginal or more than four nights for a Cesarean delivery); trimester of prenatal care initiation (first trimester or other); and whether the pregnancy was intended or unintended. Other health-related characteristics, all from MIHA, included smoking during pregnancy (any or none); drinking alcohol during pregnancy (any or none); pre-pregnancy body mass index (BMI), (BMI <25, 25.0–29.9, or ≥30); and sense of control (Pearlin mastery scale, 31 with higher values indicating more control; however, results showed that sense of control was unrelated to breastfeeding so was not included in final analyses). Demographic characteristics included maternal age (15–19, 20–24, 25–29, 30–34, 35 years or older); marital status at the time of birth, in mutually exclusive categories (married; living with a partner; single; separated, divorced, or widowed); country of birth (U.S. or elsewhere); usually spoke English at home (yes or no); payment source for delivery (private insurance, Medi-Cal, or other/uninsured); and enrolled in WIC during pregnancy or postpartum (yes or no). Covariates that were not statistically significant in unadjusted analyses were removed from the multivariable logistic regression models.
Sensitivity analyses were performed to examine effects of the potential confounders listed above on SES variables. Adjusted models were constructed by including all SES variables and then gradually adding potential confounders into the model (physical problems, pregnancy- and birth-related behaviors, other health-related characteristics, and demographics).
RESULTS
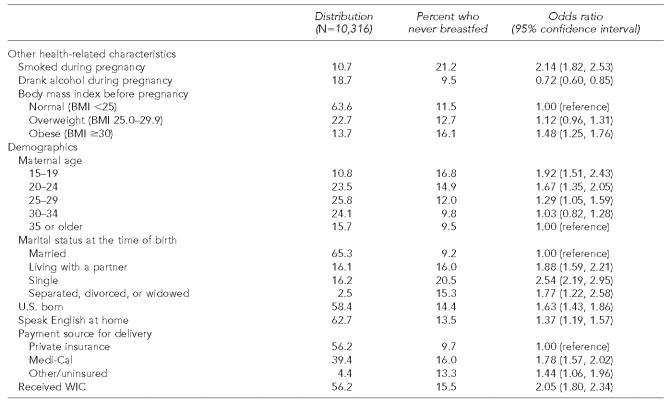
Overall, 87.8% of women had breastfed their infants at least once. This was substantially higher than the most recent reported national rates of 71.4% for 2002.32 Table 2 presents distributions, the percentages who never breastfed, and unadjusted logistic regression models for never breastfeeding. Women with lower education levels and lower incomes were more likely never to breastfeed. Never breastfeeding was also more common among those whose partners had lower education levels, or who had no partner education data reported. For both mothers and their partners, lower-status occupations and not working were associated with never breastfeeding. African Americans and U.S.-born Latinas had an elevated risk of never breastfeeding when compared to foreign-born Latinas.
Table 2.
Distributions, breastfeeding rates, and unadjusted logistic regression models for never breastfeeding, California Maternal and Infant Health Assessment, 1999–2001
All percentages are weighted.
BMI = body mass index
WIC = Special Supplemental Nutrition Program for Women, Infants and Children
Several potential confounders or mediators were also associated with never breastfeeding. Women who had a Cesarean section, a low birthweight infant, or a multiple birth were all more likely never to breastfeed. Women having a third or later child were more likely never to breastfeed than lower-parity women, as were those with an unusually short or long hospital stay, those with late or no prenatal care, and those with an unintended pregnancy. Nonsmokers breastfed more often than smokers, non-obese women more often than obese women, and alcohol drinkers more often than nondrinkers. Younger women and those who were unmarried were more likely never to breastfeed. U.S.-born women and those who spoke English at home had a higher risk of never breastfeeding, as did Medi-Cal and WIC recipients and those who were uninsured.
The adjusted model is presented in Table 3. This model adjusted for confounders or mediators that remained significant after inclusion of other variables (method of delivery, low birthweight, postpartum length of stay, trimester of prenatal care initiation, smoking during pregnancy, drinking alcohol during pregnancy, marital status, and language spoken at home). When all socioeconomic measures and significant confounders were included in the model, family income was no longer predictive of breastfeeding, and neither were maternal or paternal occupation. Maternal and paternal education both remained strongly predictive of breastfeeding, generally along a gradient, although after adjustment there was no difference in breastfeeding between women who did not finish high school and those with a high school diploma or GED. After adjustment, women whose partners had fewer than 12 years of education had about 2.4 times the odds of never breastfeeding as women whose partners had at least 16 years of education; this was similar to the odds ratio of 2.3 for those whose partners’ data were missing.
Table 3.
Adjusteda logistic regression models for never breastfeeding, California Maternal and Infant Health Assessment, 1999–2001
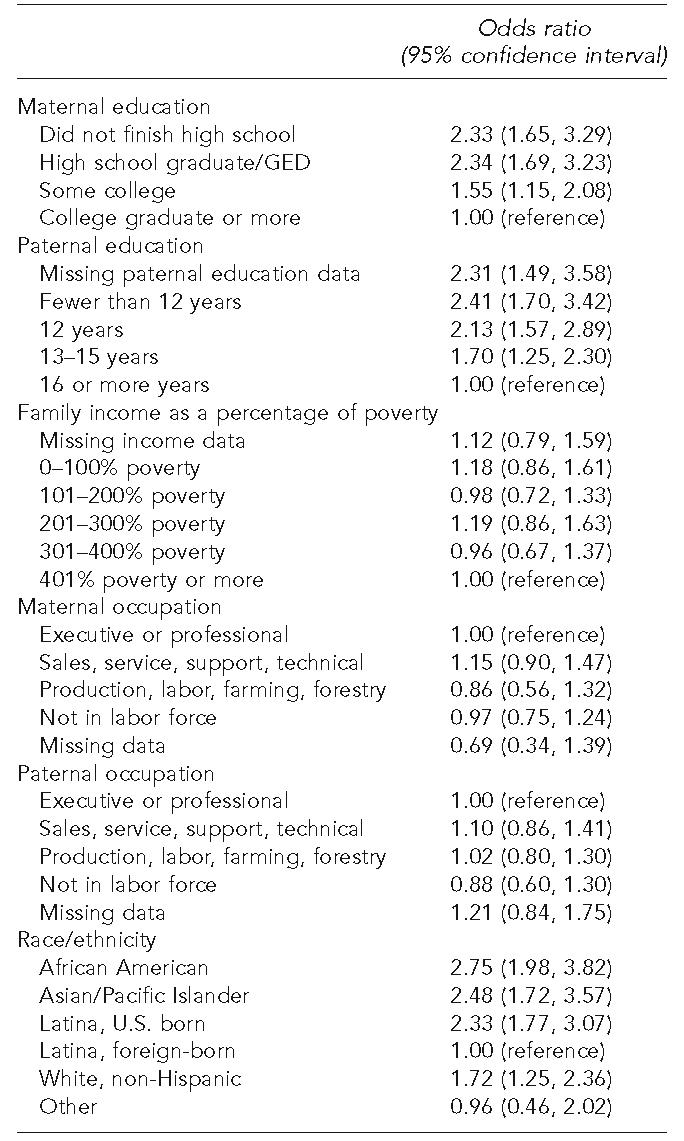
Adjusted for method of delivery, low birthweight, parity, postpartum length of stay, trimester of prenatal care initiation, smoking during pregnancy, drinking alcohol during pregnancy, marital status, and language spoken at home.
Race/ethnicity remained predictive of breastfeeding after adjustment for confounders, with African Americans, Asians/Pacific Islanders, and U.S.-born Latinas all more than twice as likely to never breastfeed as foreign-born Latinas. White women had an odds ratio of 1.7 for never breastfeeding compared with foreign-born Latinas. The odds ratios for African American women and U.S.-born Latinas decreased somewhat with adjustment for socioeconomic status and other factors. However, the odds for Asians/Pacific Islanders and whites increased after adjustment.
Sensitivity analyses indicated that the addition of marital status to the models had a strong effect on the significance of income but not of the maternal or paternal education or occupation variables. Paternal occupation was no longer significant after adjusting for the other four SES variables, while maternal occupation remained marginally significant (p=0.052) with other SES variables in the model, but was not significant once additional confounders or mediators were added. Length of postpartum stay was the covariate with the strongest effect on the association between maternal occupation and breastfeeding. Women with professional and executive occupations were much less likely than other women to have a short hospital stay, and those with a short stay were less likely to breastfeed (data not shown).
MIHA has the ability to look at breastfeeding at several points in time, up to two or three months after birth. We chose ever-breastfeeding as the outcome of interest primarily for simplicity, but additional analyses showed that whether duration or point-in-time data are used, results were essentially identical. Groups most likely to initiate breastfeeding were also those most likely to have breastfed for longer durations.
DISCUSSION
Our hypothesis that maternal education would have a powerful effect on breastfeeding was sustained. However, the hypothesis that maternal variables would outweigh paternal ones was not. This study confirmed previous findings that have shown maternal education to be more powerful than income10, 18, 26 or employment26 in predicting breastfeeding. Our results went beyond previous work in identifying both maternal and paternal education as being more important than family income or occupation of either the mother or the father in predicting breastfeeding. Controlling for all five of those socioeconomic variables did not eliminate racial and ethnic differences observed in breastfeeding, and in some cases strengthened those associations.
The information we had did not measure all aspects of the socioeconomic variables we examined. We did not have information on accumulated wealth, past socioeconomic status, or area-level socioeconomic factors. Thus, we cannot rule out additional unmeasured effects of socioeconomic status on breastfeeding.
The power of education, particularly paternal education, in predicting breastfeeding even after adjustment for many potential confounders is a new finding that may be of value in designing breastfeeding promotion programs. Women who have, or whose partners have, low education levels are at particularly high risk of not breastfeeding; paternal knowledge33 and social support34–36 may have been involved in the decision not to breastfeed. These women and their partners may need special interventions designed particularly with the less-educated in mind.
After adjustment for the five socioeconomic variables and the other covariates, maternal race/ethnicity remained a significant predictor of a woman’s likelihood of breastfeeding. Latina women born outside of the 50 U.S. states and Washington, D.C., were more likely than women in any other single racial/ethnic group to breastfeed their infants, despite lower education and lower family incomes. This finding has also been observed in a recent study from Boston, 18 although the Latino population there likely has somewhat different national origins than California’s Latinos. There were concerted efforts in many Latin American countries during the 1980s and 1990s to promote breastfeeding;37–39 the higher rates of breastfeeding among Latina immigrants may reflect those policies. The racial/ethnic disparities observed here may be due at least partly to differences the women perceived in social support for breastfeeding among their peers, 27 which were not measured in our study. However, the findings suggest that there may also be cultural norms that could influence a woman’s likelihood of breastfeeding.
The ability to make estimates for a large, diverse, population-based random sample that included women born in many countries was a strength of this study. Additional strengths included the survey’s response rate, the multiple measures of socioeconomic status available, and the ability to control for a wide range of potential confounders. Weaknesses included lack of detail about SES variables, lack of information on variables such as social support, child health, and breastfeeding education, and possible reporting bias for breastfeeding. However, rates of breastfeeding reported in MIHA were similar to those reported in routine newborn screening data collected by the state.40
CONCLUSIONS
Socioeconomic status, reflected by a range of variables, is an important predictor of a large number of health behaviors and health outcomes.41 Breastfeeding is a healthy practice that improves both maternal and infant well-being; the socioeconomic disparities observed for breastfeeding may be one component contributing to differences in health at various points across the life course. This study suggests that maternal and paternal education are critical factors influencing a woman’s initiation of breastfeeding. The education measured in this study was level of formal education rather than education about breastfeeding; whether such education actually provided any direct health information specific to breastfeeding is unclear. In general, having more formal education may help parents understand the health benefits of breastfeed-ing, and may increase the likelihood of parents to search out information about health practices. Maternal health education is typically provided during prenatal care visits that may or may not involve the mother’s partner, but data from our research suggest that fathers may be equally important in determining whether a woman breastfeeds.
Further research might attempt to discern which aspects of maternal and paternal education play the most important roles in breastfeeding; such information might be used to help target educational programs (whether through schooling or health education). Women who have or whose partners have lower education levels, African Americans, U.S.-born Latinas, and Asians and Pacific Islanders are important groups of concern for improving breastfeeding rates. This study should provide further support for the need to consider fathers’ roles in breastfeeding, and for programs designed to improve breastfeeding rates among the women at highest risk for failing to breastfeed.
References
- 1.Heinig MJ. Host defense benefits of breastfeeding for the infant. Effect of breastfeeding duration and exclusivity. Pediatr Clin North Am. 2001;48:105–23. doi: 10.1016/s0031-3955(05)70288-1. ix. [DOI] [PubMed] [Google Scholar]
- 2.Oddy WH. Breastfeeding protects against illness and infection in infants and children: a review of the evidence. Breastfeed Rev. 2001;9:11–8. [PubMed] [Google Scholar]
- 3.Labbok MH. Health sequelae of breastfeeding for the mother. Clin Perinatol. 1999;26:491–503. viii-ix. [PubMed] [Google Scholar]
- 4.Collaborative Group on Hormonal Factors in Breast Cancer. Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease. Lancet. 2002;360:187–95. doi: 10.1016/S0140-6736(02)09454-0. [DOI] [PubMed] [Google Scholar]
- 5.Department of Health and Human Services (US) Healthy People 2010. 2nd ed. 2 vols. Washington: U.S. Government Printing Office; 2000. Nov, [[cited 2005 Jul 15]]. Also available from: URL: http://www.healthy people.gov/Document/html/tracking/THP_Intro.htm) [Google Scholar]
- 6.Beck LF, Morrow B, Lipscomb LE, Johnson CH, Gaffield ME, Rogers M, Gilbert BC. Prevalence of selected maternal behaviors and experiences, Pregnancy Risk Assessment Monitoring System (PRAMS), 1999. MMWR Surveill Summ. 2002;51(SS02):1–27. [PubMed] [Google Scholar]
- 7.Roe B, Whittington LA, Fein SB, Teisl MF. Is there competition between breast-feeding and maternal employment? Demography. 1999;36:157–71. [PubMed] [Google Scholar]
- 8.Hirschman C, Butler M. Trends and differentials in breast feeding: an update. Demography. 1981;18:39–54. [PubMed] [Google Scholar]
- 9.Ryan AS. The resurgence of breastfeeding in the United States. Pediatrics. 1997;99:E12. doi: 10.1542/peds.99.4.e12. [DOI] [PubMed] [Google Scholar]
- 10.Evers S, Doran L, Schellenberg K. Influences on breastfeeding rates in low income communities in Ontario. Can J Pub Health. 1998;89:203–7. doi: 10.1007/BF03404475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nolan L, Goel V. Sociodemographic factors related to breastfeeding in Ontario: results from the Ontario Health Survey. Can J Publ Health. 1995;86:309–12. [PubMed] [Google Scholar]
- 12.Scott JA, Landers MC, Hughes RM, Binns CW. Factors associated with breastfeeding at discharge and duration of breastfeeding. J Paediatr Child Health. 2001;37:254–61. doi: 10.1046/j.1440-1754.2001.00646.x. [DOI] [PubMed] [Google Scholar]
- 13.Rutishauser IH, Carlin JB. Body mass index and duration of breast feeding: a survival analysis during the first six months of life. J Epidemiol Community Health. 1992;46:559–65. doi: 10.1136/jech.46.6.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kocturk T, Zetterstrom R. Thoughts about rates of breastfeeding. Acta Paediatr. 1999;88:356–8. doi: 10.1080/08035259950169666. [DOI] [PubMed] [Google Scholar]
- 15.Riva E, Banderali G, Agostoni C, Silano M, Radaelli G, Giovannini M. Factors associated with initiation and duration of breastfeeding in Italy. Acta Paediatr. 1999;88:411–5. doi: 10.1080/08035259950169792. [DOI] [PubMed] [Google Scholar]
- 16.Byrd TL, Balcazar H, Hummer RA. Acculturation and breast-feeding intention and practice in Hispanic women on the US-Mexico border. Ethn Dis. 2001;11:72–9. [PubMed] [Google Scholar]
- 17.Bick DE, MacArthur C, Lancashire RJ. What influences the uptake and early cessation of breast feeding? Midwifery. 1998;14:242–7. doi: 10.1016/s0266-6138(98)90096-1. [DOI] [PubMed] [Google Scholar]
- 18.Celi AC, Rich-Edwards JW, Richardson MK, Kleinman KP, Gillman MW. Immigration, race/ethnicity, and social and economic factors as predictors of breastfeeding initiation. Arch Pediatr Adolesc Med. 2005;159:255–60. doi: 10.1001/archpedi.159.3.255. [DOI] [PubMed] [Google Scholar]
- 19.Yang Q, Wen SW, Dubois L, Chen Y, Walker MC, Krewski D. Determinants of breast-feeding and weaning in Alberta, Canada. J Obstet Gynaecol Can. 2004;26:975–81. doi: 10.1016/s1701-2163(16)30419-4. [DOI] [PubMed] [Google Scholar]
- 20.Mitra AK, Khoury AJ, Hinton AW, Carothers C. Predictors of breastfeeding intention among low-income women. Matern Child Health J. 2004;8:65–70. doi: 10.1023/b:maci.0000025728.54271.27. [DOI] [PubMed] [Google Scholar]
- 21.Chezem J, Friesen C, Boettcher J. Breastfeeding knowledge, breastfeeding confidence, and infant feeding plans: effects on actual feeding practices. J Obstet Gynecol Neonatal Nurs. 2003;32:40–7. doi: 10.1177/0884217502239799. [DOI] [PubMed] [Google Scholar]
- 22.Kurinij N, Shiono PH, Ezrine SF, Rhoads GG. Does maternal employment affect breast-feeding? Am J Public Health. 1989;79:1247–50. doi: 10.2105/ajph.79.9.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gielen AC, Faden RR, O’Campo P, Brown CH, Paige DM. Maternal employment during the early postpartum period: effects on initiation and continuation of breast-feeding. Pediatrics. 1991;87:298–305. [PubMed] [Google Scholar]
- 24.Auerbach KG, Guss E. Maternal employment and breastfeeding: a study of 567 women’s experiences. Am J Dis Child. 1984;138:958–60. doi: 10.1001/archpedi.1984.02140480060018. [DOI] [PubMed] [Google Scholar]
- 25.Hills-Bonczyk SG, Avery MD, Savik K, Potter S, Duckett LJ. Women’s experiences with combining breast-feeding and employment. J Nurse Midwifery. 1993;38:257–66. doi: 10.1016/0091-2182(93)90104-o. [DOI] [PubMed] [Google Scholar]
- 26.Fein SB, Roe B. The effect of work status on initiation and duration of breast-feeding. Am J Public Health. 1998;88:1042–6. doi: 10.2105/ajph.88.7.1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Campo P, Faden RR, Gielen AC, Wang MC. Prenatal factors associated with breastfeeding duration: recommendations for prenatal interventions. Birth. 1992;19:195–201. doi: 10.1111/j.1523-536x.1992.tb00402.x. [DOI] [PubMed] [Google Scholar]
- 28.Braveman P, Cubbin C, Marchi K, Egerter S, Chavez G. Measuring socioeconomic status/position in studies of racial/ethnic disparities: maternal and infant health. Public Health Rep. 2001;116:449–63. doi: 10.1093/phr/116.5.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Research Triangle Institute. Release 8.0. Research Triangle Park (NC): Research Triangle Institute; 2001. SUDAAN software for statistical analysis of correlated data. [Google Scholar]
- 30.National Institute for Occupational Safety and Health. The SOIC System User’s Manual, Windows Edition. Morgantown (WV): NIOSH; 1998. [Google Scholar]
- 31.Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. J Health Soc Behav. 1981;22:337–56. [PubMed] [Google Scholar]
- 32.Li R, Darling N, Maurice E, Barker L, Grummer-Strawn LM. Breastfeeding rates in the United States by characteristics of the child, mother, or family: the 2002 National Immunization Survey. Pediatrics. 2005;115:e31–7. doi: 10.1542/peds.2004-0481. [DOI] [PubMed] [Google Scholar]
- 33.Giugliani ER, Bronner Y, Caiaffa WT, Vogelhut J, Witter FR, Perman JA. Are fathers prepared to encourage their partners to breast feed? A study about fathers’ knowledge of breast feeding. Acta Paediatr. 1994;83:1127–31. doi: 10.1111/j.1651-2227.1994.tb18264.x. [DOI] [PubMed] [Google Scholar]
- 34.Gross SM, Caulfield LE, Bentley ME, Bronner Y, Kessler L, Jensen J, et al. Counseling and motivational videotapes increase duration of breast-feeding in African-American WIC participants who initiate breast-feeding. J Am Diet Assoc. 1998;98:143–8. doi: 10.1016/s0002-8223(98)00037-6. [DOI] [PubMed] [Google Scholar]
- 35.Bentley ME, Caulfield LE, Gross SM, Bronner Y, Jensen J, Kessler LA, et al. Sources of influence on intention to breastfeed among African-American women at entry to WIC. J Hum Lact. 1999;15:27–34. doi: 10.1177/089033449901500109. [DOI] [PubMed] [Google Scholar]
- 36.Freed GL, Fraley JK, Schanler RJ. Attitudes of expectant fathers regarding breast-feeding. Pediatrics. 1992;90(2 Pt 1):224–7. [PubMed] [Google Scholar]
- 37.Popkin BM, Canahuati J, Bailey PE, O’Gara C. An evaluation of a national breast-feeding promotion programme in Honduras. J Biosoc Sci. 1991;23:5–21. doi: 10.1017/s0021932000019027. [DOI] [PubMed] [Google Scholar]
- 38.Wilmoth TA, Elder JP. An assessment of research on breastfeeding promotion strategies in developing countries. Soc Sci Med. 1995;41:579–94. doi: 10.1016/0277-9536(94)00363-x. [DOI] [PubMed] [Google Scholar]
- 39.Sandiford P, Morales P, Gorter A, Coyle E, Smith GD. Why do child mortality rates fall? An analysis of the Nicaraguan experience. Am J Public Health. 1991;81:30–7. doi: 10.2105/ajph.81.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McNeill D, Smith AM, Chavez G. In-hospital breastfeeding choices as indicated on the newborn screening form by county of residence and race/ethnicity, 1994–1998. Sacramento (CA): Department of Health Services; 2000. [Google Scholar]
- 41.Pamuk ER, Makuc DM, Heck KE, Lochner K, Reuben C. Health, United States, 1998 Socioeconomic status and health chartbook. Hyattsville (MD): National Center for Health Statistics; 1998. [Google Scholar]