SYNOPSIS
Objective
Hispanic individuals in the United States have a greater prevalence of diabetes mellitus than non-Hispanic white individuals; however, it is unclear whether Hispanics' risk of diabetes differs based on their level of acculturation. The purpose of our research was to examine acculturation among Hispanic Americans with respect to prevalence and control of diabetes.
Methods
We conducted an analysis of the National Health and Nutrition Examination Survey (NHANES), 1999–2002, a nationally representative sample of the noninstitutionalized U.S. population. We evaluated data on Hispanic adults (≥18 years of age, unweighted n=2,696), analyzing diagnosed diabetes, glycemic blood pressure and lipid control, and diabetes complications according to acculturation as measured by language and birth outside the United States.
Results
Hispanics with low acculturation were more likely to be without a routine place for health care, have no health insurance, and have low levels of education. In adjusted analyses, individuals with low acculturation, measured by language, were more likely to have diabetes (odds ratio [OR] 1.90, 95% confidence interval [CI] 1.02, 3.54). Among individuals with diagnosed diabetes, no significant association was yielded between acculturation and diabetes control. However, individuals with low language acculturation were more likely to have the diabetes complication of peripheral neuropathy (OR 4.01, 95% CI 1.40, 11.48).
Conclusions
Acculturation as measured through language is associated with diabetes and complications among Hispanics even after controlling for a variety of demographic characteristics including health insurance and education. The findings suggest that even within a “single” minority ethnic group, there are differences in disease prevalence and complications and access to health care.
Hispanics persons in the United States have a greater prevalence of diabetes mellitus than non-Hispanic whites.1,2 For example, the 1999–2000 age- and sex-adjusted rate of diagnosed diabetes for Mexican Americans in the United States was more than double that of non-Hispanic whites, 11.7% compared to 4.8%.3 Discussions of ethnic comparisons in research often include debates about whether ethnic populations should be considered as homogeneous groups or if differences within the groups should be considered.4,5 One characteristic that may be particularly useful in planning policy and interventions for ethnic minority groups is acculturation to the majority culture.
Acculturation is a multidimensional process in which individuals whose primary learning has been in one culture change their behaviors to reflect the majority culture. In relation to diabetes, acculturation has had both positive and negative relationships with diabetes risk depending on the ethnic group under study (e.g., Arabs, Hispanics, Japanese).6–9 In one study focusing on Mexican Americans, conducted in 1979–1982 in San Antonio, Texas, greater acculturation to the mainstream culture was associated with a decreased risk of diabetes.8
However, more investigation into the relationship between acculturation and diabetes among Hispanics may be warranted. First, it is unclear whether the relationship between acculturation and diabetes exists in a more contemporary, nationally representative population assessment. Second, since the cultural competency of non-Hispanic providers may also play a role in control and management of risk factors that differ among populations, the management of diabetes among Hispanics may be affected by acculturation.10 The purpose of our study was to examine how acculturation among Hispanics relates to control of diabetes in a nationally representative sample of the U.S. population.
METHODS
Study population and data collection
Data used for this study were derived from the National Health and Nutrition Examination Survey (NHANES), 1999–2002. The NHANES 1999–2002 is a nationally representative sample of the noninstitutionalized U.S. population. The NHANES design includes an oversampling of minorities and an ability to make population estimates. More information on the methodology of the NHANES 1999–2002, including laboratory assessment, can be found at the National Center for Health Statistics (NCHS) website.11
The NHANES contains a series of questions asked to ascertain an individual's race/ethnicity. Race and Hispanic ethnicity were addressed in separate questions. Hispanics were the only group asked questions on language, allowing for assessments of acculturation. Our study was restricted to data on Hispanic adults (≥18 years of age). The number of individuals used in the unweighted sample was 2,696, which represented a weighted population of 26,472,090 Hispanic Americans.
Interviews were conducted in both English and Spanish by trained bilingual interviewers. Respondents were free to switch between languages during the interviews depending on what language he or she was most comfortable with in answering each particular question.
Acculturation status
Acculturation is an indication of the cultural change of minority individuals to the majority culture. Acculturation measures vary widely depending on the construct used. Two general constructs available in the NHANES 1999–2002 were used to assess acculturation: language and birth outside the United States. Both of these have been used previously as proxies for acculturation.12–14
The degree of acculturation based on language was assessed using the Short Acculturation Scale (SAS), a five-item Spanish language usage scale with good internal reliability (Cronbach's coefficient alpha ≥0.90) that has been shown to be comparable to longer published acculturation scales. This scale has been validated in several Hispanic populations, with correlations seen between measured acculturation and number of generations living in the U.S., length of time living in the U.S., age of arrival to the U.S., and self report of acculturation.15
The scale consists of the following five questions:
“In general, what language do you read and speak?”
“What was the language(s) you used as a child?”
“What language(s) do you usually speak at home?”
“In which language(s) do you usually think?”
“What language(s) do you usually speak with your friends?”
Each question can be answered as “only Spanish,” “more Spanish than English,” “both equally,” “more English than Spanish,” or “only English.” These responses were scored from 1 to 5 respectively, so that scores ranged from 5–25, with higher scores signifying greater acculturation. The acculturation score was used to define five categories representing a continuum of acculturation from Spanish language only (5), primarily Spanish (6–10), about equal use of Spanish and English (11–15), primarily English (16–20), and nearly all English (21–25). Because of the decreased sample size of the group previously diagnosed with diabetes, we classified individuals within that group as either low acculturation (10 or less) or moderate to high acculturation (≥11).
Birth outside the U.S. was assessed by a single question in the interview regarding the respondent's country of birth. Unfortunately, the assessment of immigration to the U.S. was limited to this question and no assessment of years in the U.S. was available for analysis.
Dependent variables
Diabetes
We assessed previously diagnosed diabetes as well as undetected elevated blood glucose, an indicator of substantial risk for diabetes.
Previously diagnosed diabetes
A diagnosis of diabetes was assessed using responses to a question asking if a doctor has ever told the respondent that he or she has diabetes. This categorization has been used in previous studies.16,17
Undetected elevated blood glucose
Among individuals who had not been previously diagnosed with diabetes, elevated glycosylated hemoglobin (HbA1c) seems to indicate substantial risk for diabetes. Since HbA1c is a function of blood glucose and diabetes is defined as elevated blood glucose, HbA1c is a good indicator of diabetes.18 The use of HbA1c as a population screener for diabetes has shown significant utility and may work as a screener with a conservative estimate of the prevalence of diabetes.19–21 Hanson et al. showed that fasting plasma glucose and HbA1c are similar in predictive ability for the detection of non-insulin-dependent diabetes mellitus (NIDDM) as defined by WHO criteria.21 Further, other studies indicate that HbA1c can be considered as a simple diagnostic test for NIDDM.22 Following Rohlfing's work,18 we defined undetected elevated blood glucose as HbA1C >6.1% among those who denied a previous diagnosis of diabetes.
Diabetes control and complications
Control of diabetes among individuals who had been previously diagnosed was assessed in several ways with the measures available in the NHANES. Measures of control are consistent with standards of care in the U.S. at the time of data collection (e.g., 1998 standards).23 While we acknowledge that these are not the most current recommendations, it would not be useful to judge diabetes care in 1999–2002 by 2004 standards.
Glycemic control
We classified individuals with HbA1c ≥8% as having poor glycemic control, since this level corresponds to the American Diabetes Association's (ADA's) action point for glycemic control.23
Blood pressure control
The NHANES calculated blood pressure by taking three to four systolic and diastolic determinations in the mobile examination center and during home examinations on all eligible individuals using a mercury sphygmomanometer. We considered mean systolic blood pressure greater than 140 mm Hg or diastolic blood pressure greater than 90 mm Hg as elevated.23
Lipid control
The ADA suggests low high density lipoprotein (HDL) as a major risk factor for cardiovascular disease among patients with diabetes. Individuals were considered to have high-risk lipid values if they had HDL <45 mg/dl.23
Peripheral neuropathy
Peripheral neuropathy operationalized as the presence of a loss of protective sensation was ascertained for NHANES participants aged 40 and older using a standard monofilament test.24 Slight pressure with a 5.07 Semmes-Weinstein monofilament was applied three times to each of three areas on the foot (hallux, first, and fifth metatarsal heads). The testing utilized a two alternative forced choice algorithm.25 Insensitivity at any site on more than one occasion constitutes a positive test. Positive 5.07 Semmes-Weinstein monofilament testing in people with diabetes has been shown to be predictive of future diabetic foot ulceration.26,27
Control variables
A variety of variables that might affect the relationship between the diabetes indicators and acculturation were measured in the NHANES. First, ethnicity was assessed among Hispanics, with anyone of Mexican birth or descent classified as a Mexican-American. Hispanics not born in Mexico and not having any Mexican ancestors were classified as Other Hispanics. Second, the NHANES data indicated whether an individual had health insurance. Third, body mass index (BMI) was derived from height and weight measurements (kg/m2) collected in the NHANES physical examination. BMI was classified as <25 for normal or underweight, 25–29.9 for overweight, or ≥30, which corresponds with a classification of obesity. Fourth, having a routine place for care was assessed. Fifth, education was classified in the NHANES as less than a high school education, high school graduate, or at least some college. Gender and age were also used as control variables.
Analysis plan
We used SUDAAN software to allow us to make appropriate estimates from the complex sample design used in the NHANES.28 Our analysis incorporated both the stratification and clustering aspects of the sampling design. The proper weighting procedures include adjustments for the basic probability of selection and adjustments for nonresponse and poststratification. Since minorities were oversampled and a complex sampling design was employed, sampling weights provided by the NHANES were used to compute population estimates based on weighted parameter estimates and standard errors.
Chi-square analyses were used for bivariate comparisons between acculturation variables and diabetes prevalence and other outcomes. Logistic regression models were computed among the entire population to test for an effect of acculturation on diabetes prevalence and undetected elevated blood glucose controlling for ethnicity, age, sex, BMI, education, having a routine place for care, and health insurance. The two measures of acculturation (foreign born, language) were not entered in the same logistic regression, but were used to represent acculturation in separate logistic regression models.
Among individuals with diagnosed diabetes, logistic regression models were computed for acculturation and glycemic control, blood pressure, and presence of neuropathy while controlling for ethnicity, age, sex, BMI, education, having a routine place for care, and health insurance. As with the full population regressions, the two measures of acculturation (foreign born, language) were not entered in the same logistic regression, but were used to represent acculturation in separate logistic regression models.
RESULTS
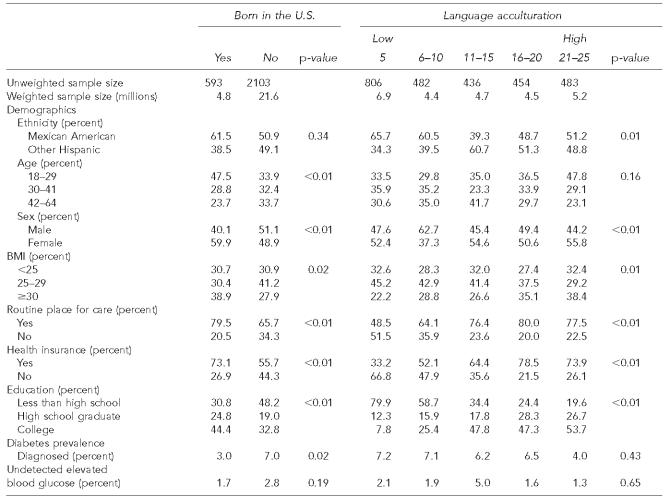
Gender, BMI, routine place for care, health insurance, and education were all related to both measures of acculturation. In addition, whether a person was Mexican American was related to language acculturation (Table 1). A greater proportion of persons with low language acculturation were Mexican American than were individuals whose heritage was from other Latin American countries. Age was also related to whether or not a person was born in the U.S.
Table 1.
Demographics and diabetes prevalence by two measures of acculturation
NOTE: Chi-square tests were used for all comparisons.
BMI = body mass index
The unadjusted prevalence of diagnosed diabetes was significantly related to where a person was born, but not to language acculturation (Table 1). Hispanic individuals born in the U.S. had less than half the prevalence of diagnosed diabetes compared to those born outside the U.S. Undetected elevated blood glucose, although showing a pattern similar to diagnosed diabetes, was not statistically significantly related to either acculturation variable. Although the association between language acculturation and undetected elevated blood glucose was not significant, the group with moderate levels of language acculturation had the greatest prevalence of undetected elevated blood glucose. In contrast, Hispanics born in the U.S. or with higher levels of language acculturation were more likely to have a BMI of 30 or more. They were also more likely to have a routine place of care and health insurance.
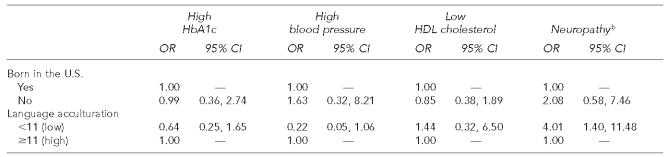
In adjusted logistic regression analyses controlling for ethnicity (Mexican American or Other Hispanic), age, sex, BMI, routine place of care, health insurance, and education, language acculturation had a significant association with diagnosed diabetes (Table 2). Individuals with the lowest level of language acculturation had a higher likelihood of having diagnosed diabetes compared to those with the highest level of acculturation. Although place of birth was related to diagnosed diabetes in an unadjusted relationship, they were not significantly related in a model adjusting for relevant covariates. In adjusted analyses, undetected elevated blood glucose was not related to place of birth or language acculturation.
Table 2.
Adjusted logistic regression analyses predicting occurrence of diabetesa
Controlling for ethnicity, age, sex, body mass index, routine place of care, health insurance, and education.
OR = odds ratio
CI = confidence interval
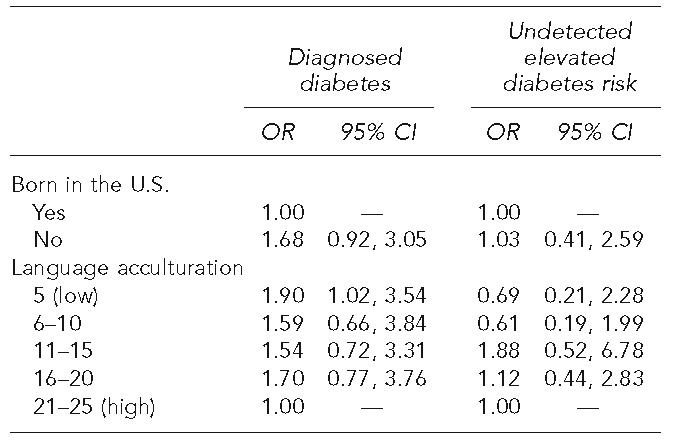
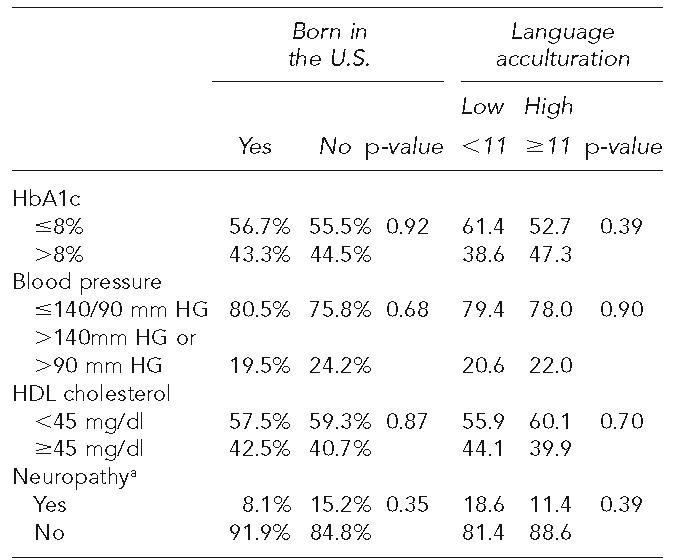
When glycemic control was examined among individuals with diagnosed diabetes, no significant relationships were yielded between the outcomes and either of the acculturation variables (Table 3). Much like with diagnosed diabetes, although no relationship was found in an unadjusted analysis, adjusted analyses showed language acculturation was associated with the presence of peripheral neuropathy (Table 4). Individuals with low language acculturation were more likely to have peripheral neuropathy.
Table 3.
Acculturation and outcomes among patients with previously diagnosed diabetes
Neuropathy among diabetics 40 to 64 years of age.
NOTE: Chi-square tests were used for all comparisons.
Table 4.
Adjusted logistic regression analyses predicting high glucose, high blood pressure, low HDL cholesterol, and neuropathy among diabeticsa
Controlling for ethnicity, age, sex, body mass index, routine place of care, health insurance, and education.
Neuropathy among diabetics 40 to 64 years of age
OR = odds ratio
CI = confidence interval
DISCUSSION
These results suggest that within-group differences in ethnic groups may need to be considered in efforts to alleviate health disparities. In this nationally representative survey, acculturation among Hispanics in the U.S., as measured via language, is associated with diabetes even after controlling for a variety of demographic characteristics including health insurance and education. Individuals with low acculturation, measured by language, who have been diagnosed with diabetes are at increased risk for having the complication of peripheral neuropathy. Despite having a higher prevalence of diabetes and a greater risk of complications, they were less likely to have a regular place of care or health insurance. Acculturation was not associated with several other indicators of diabetes control or risk for cardiovascular disease. When acculturation was measured by the crude assessment of being foreign born, no significant relationship was yielded with either diabetes or control among patients with diabetes.
Understanding diabetes, its symptoms, and treatments is particularly important for the patient and conveying this information to the patient is a crucial role for the physician. Poor health literacy is more common among patients with low educational attainment, immigrants, and racial and ethnic minorities.29 Poor health literacy among patients with diabetes has been shown to be associated with worse glycemic control and more frequently reported retinopathy.30 Hispanic patients with low language acculturation may be particularly at risk if their physician has poor Spanish skills and understanding of Hispanic culture.31 Our findings suggest that a substantial portion of Hispanics in the U.S. may be at risk and that focusing on culturally appropriate interventions to increase health literacy among this population may be warranted.
Our nationally representative finding that lower levels of acculturation among Hispanics is associated with diabetes is similar to a previous regional study conducted 20 years earlier.8 Although that study operationalized acculturation differently than the present study, had a more restrictive age range for participation, and included only Mexican Americans, both studies observed a relationship between acculturation and diabetes. However, the regional study did not find a relationship between acculturation and BMI like that found in our analysis. The last 20 years have seen substantial growth of the U.S. Hispanic population to the point where estimates for 2002 indicate that more than one in eight individuals in the U.S., or 37.4 million individuals, is Hispanic.32 The within-group differences found in this nationally representative study illustrate that health care interventions to address disparities should recognize that ethnic groups may need to be seen in more sophisticated ways than simply as homogenous wholes.
We must acknowledge several limitations to this study. First, the data set is cross-sectional, which limits the ability to make inferences about causality. The NHANES data do, however, allow us to make population estimates for conditions for subgroups of the U.S. population. Second, we included everyone who self-identified as Hispanic in our study, then stratified Mexican-Americans vs. Other Hispanics. We believed that in the development of nationally representative population estimates, this clumping would give the best representation of diabetes and acculturation among Hispanics in the U.S, particularly since the primary acculturation measures are based on language or U.S. birth. However, it is possible that differences in health beliefs and behaviors among Hispanic cultural groups may have affected the results when viewing Hispanics as a single culturally unified group.33 Third, the question regarding the assessment of physician-diagnosed diabetes does not discriminate between those told that they had type 1 and type 2 diabetes. Fourth, although the levels of HbA1c and blood pressure and HDL were consistent with recommendations present at the time of data collection, all of these measures had been revised by 2004 to be more stringent.34 Consequently, the findings of this study may not generalize to practice in 2005.
In conclusion, this study points to the importance of within-group differences among Hispanics that need to be understood when considering health care disparities. For ethnic groups that have language and cultural differences from the majority English speaking U.S. population, ensuring cultural competence among providers is warranted.
Acknowledgments
This work was supported in part by grants 1D12HP00023 from the Health Resources and Services Administration; grant 1 P30 AG21677 from the National Institute on Aging; and grants 1 R21 DK067130 and 1R21 DK066066 from the National Institute of Diabetes and Digestive and Kidney Disease.
REFERENCES
- 1.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286:1195–200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 2.Harris MI, Flegal KM, Cowie CC, Eberhardt MS, Goldstein DE, Little RR, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in US adults. The Third National Health and Nutrition Examination Survey, 1988–1994. Diabetes Care. 1998;21:518–24. doi: 10.2337/diacare.21.4.518. [DOI] [PubMed] [Google Scholar]
- 3.Prevalence of diabetes and impaired fasting glucose in adults—United States, 1999–2000. [cited 2006 Aug 16];MMWR Morb Mortal Wkly Rep. 2003 52(35):833–7. Also available from: URL: http://www.cdc.gov/mmwr/PDF/wk/mm5235.pdf. [PubMed] [Google Scholar]
- 4.Goslar PW, Macera CA, Castellanos LG, Hussey JR, Sy FS, Sharpe PA. Blood pressure in Hispanic women: the role of diet, acculturation and physical activity. Ethn Dis. 1997;7:106–13. [PubMed] [Google Scholar]
- 5.Bloche MG. Race-based therapeutics. N Engl J Med. 2004;351:2035–7. doi: 10.1056/NEJMp048271. [DOI] [PubMed] [Google Scholar]
- 6.Jaber LA, Brown MB, Hammad A, Zhu Q, Herman WH. Lack of acculturation is a risk factor for diabetes in Arab immigrants in the US. Diabetes Care. 2003;26:2010–4. doi: 10.2337/diacare.26.7.2010. [DOI] [PubMed] [Google Scholar]
- 7.Huang B, Rodriguez BL, Burchfiel CM, Chyou PH, Curb JD, Yano K. Acculturation and prevalence of diabetes among Japanese-American men in Hawaii. Am J Epidemiol. 1996;144:674–81. doi: 10.1093/oxfordjournals.aje.a008980. [DOI] [PubMed] [Google Scholar]
- 8.Hazuda HP, Haffner SM, Stern MP, Eifler CW. Effects of acculturation and socioeconomic status on obesity and diabetes in Mexican Americans: the San Antonio Heart Study. Am J Epidemiol. 1988;128:1289–301. doi: 10.1093/oxfordjournals.aje.a115082. [DOI] [PubMed] [Google Scholar]
- 9.Tull ES, Ambrose JJ, Chambers E. A preliminary assessment of acculturation and its relationship to body size and glucose intolerance among blacks in the US Virgin Islands. Ethn Dis. 2003;13:15–21. [PubMed] [Google Scholar]
- 10.Game FL, Jones AF. Ethnicity and risk factors for coronary heart disease in diabetes mellitus. Diabetes, Obes Metab. 2000;2:91–7. doi: 10.1046/j.1463-1326.2000.00063.x. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention (US), National Center for Health Statistics National Health and Nutrition Examination Survey. NHANES 1999–2004. [cited 2005 Aug 17]. Available from: URL: http://www.cdc.gov/nchs/about/major/nhanes/nhanes99-02.htm.
- 12.Mainous AG., 3rd Self-concept as an indicator of acculturation in Mexican Americans. Hispanic J Behav Sci. 1989;11:178–89. [Google Scholar]
- 13.Griffith J. Relationship between acculturation and psychological impairment in adult Mexican Americans. Hispanic J Behav Sci. 1983;5:431–59. [Google Scholar]
- 14.Nesdale D. Acculturation attitudes and the ethnic and host-country identification of immigrants. J Applied Social Psych. 2002;32:1488–507. [Google Scholar]
- 15.Marin G, Sabogal F, Van Oss Marin B, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hispanic J Behav Sci. 1987;9:183–205. [Google Scholar]
- 16.Harris MI, Flegal KM, Cowie CC, Eberhardt MS, Goldstein DE, Little RR, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. The Third National Health Nutrition Examination Survey, 1988–1994. Diabetes Care. 1998;21:518–24. doi: 10.2337/diacare.21.4.518. [DOI] [PubMed] [Google Scholar]
- 17.Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KM. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002;136:565–74. doi: 10.7326/0003-4819-136-8-200204160-00005. [DOI] [PubMed] [Google Scholar]
- 18.Rohlfing CL, Little RR, Wiedmeyer HM, England JD, Madsen R, Harris MI, et al. Use of GHb (HbA1C) in screening for undiagnosed diabetes in the U.S. population. Diabetes Care. 2000;23:187–91. doi: 10.2337/diacare.23.2.187. [DOI] [PubMed] [Google Scholar]
- 19.Peters AL, Davidson MB, Schriger DL, Hasselblad V. A clinical approach for the diagnosis of diabetes mellitus: an analysis using glycosylated hemoglobin levels. Meta-analysis Research Group on the Diagnosis of Diabetes Using Glycated Hemoglobin Levels. JAMA. 1996;276:1246–52. [published erratum appears in JAMA 1997 Apr 9;277:1125] [PubMed] [Google Scholar]
- 20.Davidson MB, Schriger DL, Peters AL, Lorber B. Revisiting the oral glucose tolerance test criterion for the diagnosis of diabetes. J Gen Int Med. 2000;15:551–5. doi: 10.1046/j.1525-1497.2000.08024.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hanson RL, Nelson RG, McCance DR, Beart JA, Charles MA, Petitt DJ, et al. Comparison of screening tests for non-insulin-dependent diabetes mellitus. Arch Intern Med. 1993;153:2133–40. [PubMed] [Google Scholar]
- 22.Diabetes Control and Complications Trial Research Group. The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the Diabetes Control and Complications Trial. Diabetes. 1995;44:968–83. [PubMed] [Google Scholar]
- 23.American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care. 1998;21(Suppl 1):S23–31. [Google Scholar]
- 24.American Diabetes Association. Preventive foot care in people with diabetes. Diabetes Care. 2003;26(Suppl 1):S78–9. doi: 10.2337/diacare.26.2007.s78. [DOI] [PubMed] [Google Scholar]
- 25.Sekuler R, Nash D, Armstrong R. Sensitive objective procedure for evaluating response to light touches. Neurology. 1973;23:1282–91. doi: 10.1212/wnl.23.12.1282. [DOI] [PubMed] [Google Scholar]
- 26.Pham H, Armstrong DG, Harvey C, Harkless LB, Giurini JM, Veves A. Screening techniques to identify people at high risk for diabetic foot ulceration. Diabetes Care. 2000;23:606–11. doi: 10.2337/diacare.23.5.606. [DOI] [PubMed] [Google Scholar]
- 27.Boyko EJ, Ahroni JH, Stensel V, Forsberg RC, Davignon DR, Smith DG. A prospective study of risk factors for diabetic foot ulcer: the Seattle diabetic foot study. Diabetes Care. 1999;22:1036–42. doi: 10.2337/diacare.22.7.1036. [DOI] [PubMed] [Google Scholar]
- 28.Research Triangle Institute. SUDAAN: Version 9.0.1 for SAS Version 9. Research Triangle Park (NC): Research Triangle Institute; 2005. [Google Scholar]
- 29.Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs. Health literacy: a report of the Council on Scientific Affairs. Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. JAMA. 1999;281:552–7. [PubMed] [Google Scholar]
- 30.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–82. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 31.Fernandez A, Schillinger D, Grumbach K, Rosenthal A, Stewart AL, Wang F, et al. Physician language ability and cultural competence. An exploratory study of communication with Spanish-speaking patients. J Gen Intern Med. 2004;19:167–74. doi: 10.1111/j.1525-1497.2004.30266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Census Bureau (US) The Hispanic population in the United States: March 2002. Current population reports, P20-545. Washington: Census Bureau (US); [cited 2005 Jul 23]. Available from: URL: http://www.census.gov/prod/2003pubs/p20-545.pdf. [Google Scholar]
- 33.Pachter LM, Weller SC, Baer RD, de Alba Garcia JE, Trotter RT, 2nd, Glazer M, et al. Variation in asthma beliefs and practices among mainland Puerto Ricans, Mexican-Americans, Mexicans, and Guatemalans. J Asthma. 2002;39:119–34. doi: 10.1081/jas-120002193. [DOI] [PubMed] [Google Scholar]
- 34.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2004;27(Supp 1):S15–35. doi: 10.2337/diacare.27.2007.s15. [DOI] [PubMed] [Google Scholar]