SYNOPSIS
We examined the public health effects of the Northeast blackout of August 2003 and the emergency response to the blackout by the New York City Department of Health and Mental Hygiene (DOHMH). We reviewed departmental documents from the DOHMH Emergency Operations Center and surveyed DOHMH employees to identify deficiencies in the response and elicit suggestions for improvement.
DOHMH deployed its all-hazards, scalable public health Incident Management System to respond to several impacts: (1) failure of multiple hospital emergency generators; (2) patients dependent on electrically powered equipment; (3) loss of electronic data input to the DOHMH syndromic surveillance system from hospital emergency departments; (4) potential for vaccine spoilage due to loss of refrigeration; (5) beach contamination with untreated sewage; (6) heat-related health effects and increase of foodborne disease; and (7) potential for an increased rodent population as a result of increased amounts of discarded perishables. Areas identified for improvement included communications during the event, DOHMH dependence on an external source of electricity, facility management during the response, and lack of readily available and appropriate emergency supplies.
Electrical power failure is not a new phenomenon. Massive power failures have occurred throughout the United States and the world.1–6 The heavy dependence of modern infrastructure on electricity can lead to public health effects when power is lost. Assessment of the public health effects of power failures has been limited to events occurring at hospitals and related emergency medical services. O'Hara and Higgins described events occurring in a cardiothoracic intensive care unit during a blackout in Ireland.3 Hargrove et al. reviewed the health outcomes for patients on cardiopulmonary bypass during three blackouts in Cleveland, Ohio.4 Spivak described the experience of emergency medical services during a citywide blackout in San Francisco.5 Schaffer reported medical staff activities during a blackout that affected a New York City neonatal intensive care unit.6 In this article, we describe the responses of the New York City Department of Health and Mental Hygiene (DOHMH) during the blackout of August 14–17, 2003, to increase awareness of the important public health issues that might arise during a blackout and to share our experiences during the response.
DOHMH EMERGENCY RESPONSE STRUCTURE
During an emergency, individual agencies operate under their own command structure responding to aspects of the emergency that fall under the range of that agency's mandate. However, since multiple agencies are involved, the overall response must be coordinated. This improves communication, allows for pooling of resources, enhances the collaboration between agencies, and improves the efficiency of the response.
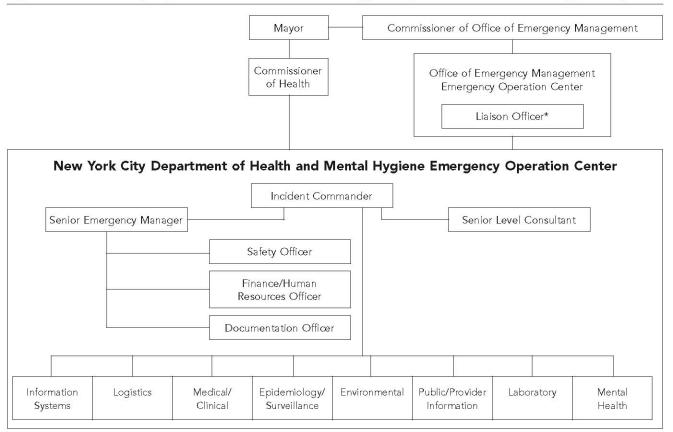
The New York City (NYC) Office of Emergency Management coordinates the citywide response to emergencies (Figure 1). Liaisons for all agencies and organizations involved in the city's response activities are based in the Office of Emergency Management's Emergency Operations Center (EOC) in Brooklyn. In addition, agencies involved in emergency response have their own EOCs.
Figure 1.
New York City Department of Health and Mental Hygiene's public health incident management system
* Department of Health and Mental Hygiene Employee located at the Office of Emergency Management Emergency Operation Center
The DOHMH's EOC is located at DOHMH headquarters in lower Manhattan and employs the Incident Management System, the same predefined chain-of-command system that other emergency response agencies use. The Commissioner of Health, the lead official at DOHMH, determines the need to activate the Incident Management System and to establish an EOC. He appoints the initial incident commander, prioritizes issues, and acts as the public spokesperson for the agency. The incident commander is the operational decision maker for DOHMH during the event. The incident commander's duties also include evaluating the need for outside assistance, responding to interagency requests, and presenting major policy issues to the Commissioner of Health for resolution.
A senior emergency manager from the DOHMH's Bureau of Emergency Management assists the incident commander in coordinating the administrative and logistical operations of the EOC. The senior emergency manager directs the activities of Bureau of Emergency Management staff members, who include a DOHMH liaison officer assigned to the Office of Emergency Management's EOC, a safety officer, a finance/human resources officer, and a documentation officer. The DOHMH liaison updates the DOHMH incident commander on the activities of other agencies involved in the emergency and transmits information and requests between DOHMH and these agencies. The safety officer monitors the working conditions in the EOC and in the field. The finance officer tracks expenditures during the response. If state or federal agencies can provide the city reimbursement for a response, the finance officer prepares the appropriate documentation regarding the response cost. The documentation officer chronologically records events, responses, and other activities occurring in the EOC and prepares a shift report summarizing the activities of field staff to maintain an adequate flow of information between shifts. Not all of these roles are necessary in every response. During the blackout, only a documentation officer and a liaison to the citywide EOC were needed.
In addition to Bureau of Emergency Management staffing, the expertise of additional consultants may be needed to assist the incident commander. During the blackout, legal counsel was consulted on the health code and assisted the incident commander in its application during the emergency.
Rather than develop individual plans with detailed instructions specific to each type of incident, DOHMH recognizes that certain public health issues are common to most incidents and has adopted an “all-hazards” approach to incident management. Because DOHMH activities during emergencies do not necessarily correspond to its routine operating divisions, eight emergency response sections were created to respond to emergency events: information systems, logistics, medical/clinical, epidemiology/surveillance, environmental, public/provider information, laboratory, and mental health (Figure 1).
Each section has an appointed chief and pre-assigned staff members. Due to DOHMH initiatives to improve preparedness (implemented prior to the blackout), all employees were informed of their section designation in the event of emergency during agency-wide training and orientation on the Incident Management System. During this training, employees were also provided a wallet card with 24-hour contact information and other key Incident Management System information including location and directions to the primary and alternate EOCs. After reporting to their response sections, employees are provided a brief description of their primary role and the duties they are expected to complete (e.g., job action sheet). These duties are prioritized by urgency. In an emergency, employees might not have the same duties they perform routinely; the job action sheets provide direction and clarity by predetermining these duties.
After notification of an incident, the incident commander meets with the section chiefs in the EOC to conduct an initial assessment and determine the response. Actions are identified and then assigned to the appropriate sections. Shifts are established and staff members are assigned, including incident commanders for subsequent shifts. Regular meetings of the incident commander and section chiefs are scheduled for development and prioritization of response activities, updates on pending activities, problem-solving barriers to completion of activities, and identification of prevention activities in anticipation of future public health issues. At the end of each shift, an EOC staff meeting is held to brief incoming staff members on recent events and to identify pending actions. Each employee meets with his or her replacement for the next shift and provides them with specific details regarding duties.
THE BLACKOUT
At 4:15 p.m. on Thursday, August 14, 2003, a cascading electrical power failure across the northeastern United States resulted in power failure in all five New York City boroughs. The Commissioner of Health immediately called for the establishment of an EOC and deployment of the Incident Management System. The DOHMH EOC was located at the central office in Manhattan and a DOHMH liaison was dispatched to the Office of Emergency Management EOC, where the citywide response was coordinated. Twelve-hour shifts were established, and the DOHMH EOC operated with continuous coverage throughout the blackout and for an additional 24 hours after citywide resumption of power. EOC coverage ended at 8:00 a.m. Monday, August 18.
DOHMH RESPONSE
Immediately following the blackout, Bureau of Emergency Management staff distributed fiashlights, provided 800-megahertz radios, and assessed the status of the telephone system at DOHMH. Because the blackout occurred in the afternoon, there was sufficient daylight to work at the EOC without the need for electrical lighting. However, the battery-powered emergency lamps, which were the only source of lighting in hallways and stairwells, ran out within 2 to 3 hours, making traveling between floors hazardous without a flashlight. During the ensuing 90 hours, the DOHMH provided continuous coverage, including critical emergency response functions as well as routine DOHMH operations.
Logistics and information systems
The logistics section provided physical security for the building and ensured that the emergency generators at the Public Health Laboratory were operating and had adequate fuel. This section then secured perishable vaccines from DOHMH clinics where refrigeration units had lost power and transferred them to storage at the Public Health Laboratory. Because EOC did not have emergency generators on site, flashlights were the only source of lighting during the evening of August 14. By 2:00 a.m., the logistics section had secured two generators to supply limited power. Floor lamps were moved into the EOC to supply lighting. When the generators arrived, the information systems section equipped EOC with laptop computers, a printer, and wireless Internet connections. The information systems section also played a key role following the return of external power when several network routers failed to reset. This prevented full restoration of the agency's computer network.
Medical/clinical
The medical/clinical section monitored the delivery of health care during the emergency. Despite having emergency generators, four of 75 hospitals in the city were temporarily without electricity when the blackout occurred. The longest interruption was 2 hours and 45 minutes. The medical/clinical section interviewed hospital administrators to determine the extent of the loss and its impact on services. Several hospitals also depend on steam produced by electrically powered systems to sterilize hospital equipment. When the blackout occurred, these systems failed and alternative facilities for sterilizing equipment were needed. The medical/clinical section advised medical providers about the risk of vaccine spoilage that could result from a loss of refrigeration. The Office of Emergency Management opened cooling centers and the medical/clinical section was ready to supply staff members if needed. The medical/clinical section coordinated with the New York City Housing Authority to contact housing facilities for vulnerable populations (e.g., elderly and mentally impaired) and conducted a needs assessment. The Office of Emergency Management coordinated with the New York City Housing Authority to ensure that these facilities had functioning emergency generators to provide adequate cooling for these facilities. Facilities with a history of repeated housing violations were targeted for site visits during the blackout; the remaining facilities were contacted by telephone. The Ofce of Emergency Management provided several facilities with additional fuel for their emergency generators during the blackout.
Persons dependent on medical devices (e.g., home ventilators and medication nebulizers) encountered problems.10 Patients presented to hospital emergency departments to access electricity to power their devices. Emergency medical services and other ambulance services transported patients dependent on electrically powered medical devices, but the large number of patients requiring assistance due to the blackout caused a strain on both emergency medical services and hospitals where these patients were delivered.11 This increased demand was in addition to injuries and deaths attributable to the blackout.12,13 Radio and newspaper announcements were released by the Mayor's Office suggesting that in addition to hospital emergency departments, cooling centers, fire stations, and other facilities were available for this purpose. If they resided on the upper floors of high-rise apartments, homebound persons might not have been able to leave their floors, but there was no way for DOHMH to identify who, where, and what the needs of this group were. Instead, in a press conference, the mayor encouraged New Yorkers to visit older or otherwise vulnerable neighbors and assist them as needed.
Epidemiology/surveillance
The DOHMH's epidemiology/surveillance section maintained syndromic surveillance activities14 to ensure the blackout was not part of a bioterrorist or other attack. This section also monitored potential health-related effects of the blackout (e.g., heat stroke and carbon monoxide poisoning). Typically, hospitals gather these data electronically; however, during the blackout, the same computers that accessed and transmitted the data to DOHMH were not part of the electrical systems supplied by the emergency generators. In response, the epidemiology/surveillance section dispatched staff members to participating hospitals to manually gather the data for an interim emergency department syndromic surveillance system until the restoration of power allowed resumption of the daily transmission of emergency department data. Issues of possible public health concern arising from the tallies were investigated immediately. Of note, three days after the blackout, a robust increase in diarrheal illness was detected. In response, a case-control investigation was conducted to determine risk factors for diarrheal illness after the blackout. The results of this investigation are described by Marx et al.8
Environmental
The DOHMH environmental section contacted the New York City Department of Environmental Protection to determine if the city's drinking water supply was safe for drinking. Because the city's potable water system was constructed such that gravity alone can maintain water pressure, there was no loss of pressure during the blackout, and therefore no additional risk of contamination. DOHMH maintained routine microbial monitoring of potable water during the blackout. Residents of high-rise apartment buildings depend on electrical pumps to raise potable water from street level to their homes. With the loss of power, these residents were left without ready access to potable water for several days. The DOHMH EOC considered plans to determine how to provide potable water to these residents if the blackout continued.
Perishables were subject to rapid spoilage with the loss of refrigeration. To ensure that restaurants appropriately discarded these items, DOHMH continued restaurant inspections throughout the city during the daylight hours of the blackout. With the assistance of inspectors from Duchess and Nassau counties and the New York City Department of Agriculture and Markets, approximately 500 inspections were completed. If the increased amount of discarded perishables was not disposed of in a timely manner, the city's rodent population could grow as a result of the increased food supply. Typically, private contractors haul away the waste from retail food service businesses. During the blackout, the contractors had difficulty hauling away the increased volume of refuse at the regularly scheduled intervals. Therefore, DOHMH issued emergency public health orders allowing the Department of Sanitation to cart this waste. As an added measure, routine pest-control services were continued during the blackout; approximately 400 rodent extermination sites were baited during the blackout.
The blackout resulted in the accidental release of 500 million gallons of untreated sewage into the recreational waterways surrounding the city when backup generators powering several treatment facilities failed. This accidental release resulted in an overflow past treatment facilities. Beaches were immediately closed. Because the ambient temperatures during the day were an average of 95° F, reopening the beaches at the earliest possible time when safe was a priority. In coordination with the New York City Department of Environmental Protection, 50 sets of samples from affected New York City beaches were collected for testing, allowing the reopening of beaches at the earliest safe time, three days after the blackout began.
Public/provider information
DOHMH's public/provider information section developed and issued public health alerts for radio or newspaper dissemination regarding the contamination of the recreational waterways and subsequent beach closures. This section addressed the potential threat of heat-related health effects by issuing press releases to educate the public. The public/provider information section also alerted the public of food safety issues during the blackout and encouraged New Yorkers to discard spoiled food.
Laboratory
The Public Health Laboratory, which functions as the laboratory section during emergencies, maintained services despite the blackout, including maintaining refrigeration of the clinical specimens received for immediate testing and millions of specimens archived for investigations and research studies. Ensuring the laboratory refrigeration units continued to function required close monitoring of the laboratory generators' diesel fuel supply. A possible rabies exposure occurred during the blackout. Animal testing was successfully completed at the Public Health Laboratory despite the blackout. The laboratory section conducted fecal coliform testing on 200 beach water specimens collected during 50 sets of sampling by the Department of Environmental Protection. The Public Health Laboratory is also responsible for testing air filters used for environmental surveillance. These units are an early warning system against aerosol releases of hazardous agents by terrorists. Although the laboratory had functioning emergency generators, the protective hoods where the filters could be safely processed were not functioning. As part of the Public Health Laboratory's emergency response plan, agreements to provide backup assistance with predetermined laboratories throughout New York City, the tri-state area, and the country were in place. One of the alternative laboratories in the city was used for processing the filters and results were available on time.
Mental health
The mental health section ensured that LifeNet, the city's 24-hour emergency mental health referral service, continued to function during the blackout. However, contact with the service was reduced to calling the telephone number that was usually devoted to faxing because the digital phone system required supplemental power to function.
Routine DOHMH activities
In addition to blackout-related activities, maintaining routine DOHMH activities was important. The Poison Control Center answered more than 1,000 calls during the blackout. The burial desk issued 400 death certificates. The West Nile Control Program applied larvicide to 16 acres. The Office of the Chief Medical Examiner continued operations despite the blackout, and DOHMH clinics were open Friday, August 15, and offered limited services, although few patients kept appointments that day.
EVALUATION/LESSONS LEARNED
To determine the quality of our response to the blackout event, we conducted a retrospective program evaluation using methods adapted from the Centers for Disease Control and Prevention's Framework for Program Evaluation in Public Health.7 To recount the DOHMH response, we relied on personal experience, the notes of documentation officers, and shift reports prepared during EOC coverage. Notes created by the documentation officers provided a chronological description of events, activities, and responses occurring at the EOC. Shift reports provided a summary of field activities performed by each section. In addition, we reviewed all available reports prepared on specific aspects of the DOHMH response.8,9
To evaluate the DOHMH response, the senior emergency manager asked personnel working in the DOHMH EOC to complete a quality-assessment form. The forms requested a simple listing of activities that achieved their intended goal efficiently and a list of barriers encountered during the response. Respondents were also asked to suggest ways to improve the response. The quality-assessment forms were made available in EOC. Responses were solicited during the blackout to ensure timely and accurate reporting of issues. Responses to the open-ended questions were entered into a spreadsheet and categorized by topic.
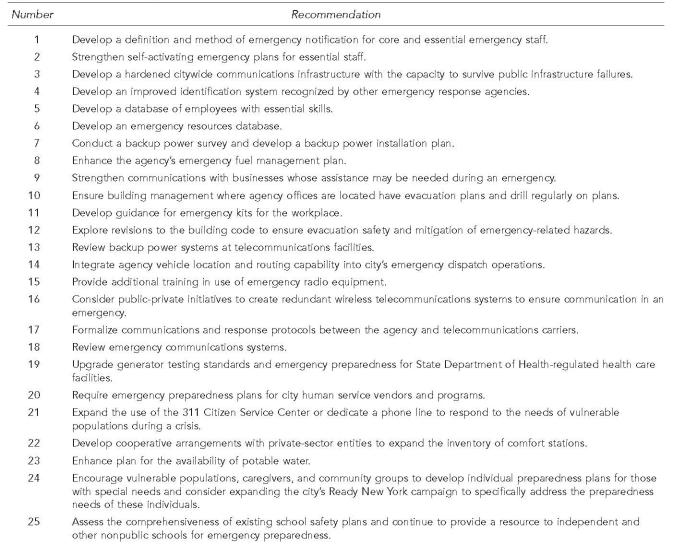
Forty-nine (35%) of the approximately 140 staff members working in the DOHMH EOC during the blackout completed quality-assurance forms. All responses were reviewed by Bureau of Emergency Management staff and subjectively evaluated for practicality, impact, and cost. The responses were then prioritized, assigned to the operating division or section where the change needed to occur, and tracked through regular meetings with the assignee to ensure attainment of the goal.Figure 2 lists the 25 recommendations developed based on the 49 returned quality assurance forms. The recommendations can be summarized in four major categories: (1) communication, (2) EOC dependence on an external source of electricity, (3) facility management during the response, and (4) adequacy of emergency supplies.
Figure 2.
DOHMH employee recommendations for improvement of the blackout response
DOHMH = Department of Health and Mental Hygiene
Communication
All respondents listed at least one item related to problems with communication during the response. During emergencies, employees contact the DOHMH employee call center to obtain information regarding if, when, and where to report for work. However, like other telephones at DOHMH, call center telephones require supplemental electricity to operate. The call center did have a universal power pack, a back-up battery that allowed continued call center operations after the blackout began, but the charge was insufficient to maintain continuous service for the duration of the blackout. In addition, the call center had inadequate telephone lines to respond to the volume of employee calls. Increasing the capabilities of the call center was suggested, but further improvement of protocols could also improve the public health response. The recommended protocols include (1) which, when, and where employees should report during future emergencies; (2) establishing a directory of employees' skills and emergency contact information that would be readily accessible during an emergency; and (3) conducting drills and other training sessions to ensure that employees are aware of these details.
To communicate with key staff members and the citywide EOC, 800-megahertz radios were critical, but their limited battery life eventually resulted in communication difficulties. Extra batteries or emergency power to recharge the radios would improve communications. Although the city's telephone system was on a separate and unaffected power grid, the majority of DOHMH telephones required additional electrical power to function, and therefore did not operate during the blackout. EOC needs telephones that do not require additional power to maintain open lines of communication. Finally, preparing press releases and public health advisories on generic health issues expected during an emergency prior to an event was also suggested because preparing these documents during the emergency without computers caused delays.
EOC dependence on electricity
Fourteen respondents (30%) identified issues related to the EOC's critical dependence on electricity to power lights, computers, printers, and other essential equipment. Although emergency generators were eventually obtained, a lack of power for 10 hours caused delays in completing action plans. Storing battery-operated equipment and emergency generators at DOHMH would improve the efficiency of response in the critical first hours after an event. Key operation plans, contact information, and other documents stored on specific desktop computers were not accessible. Because emergency generators can supply power only to select computers during an emergency, creating a backup, paper library of important documents needed during an emergency would also improve response time.
Facilities management
Eight respondents (17%) commented on problems relating to facilities management during the blackout response. Items mentioned included problems with access to locked offices and buildings and the absence of housekeeping services during the event.
Lack of emergency supplies
Six respondents (13%) listed issues relating to a lack of key emergency items not readily available during the response (e.g., flashlights, food, batteries for laptops, and battery-operated printers). Supplies for EOC should be stored on-site or at a nearby location rather than at a distant agency warehouse. DOHMH plans to stock adequate supplies on-site to provide 48 hours of self-sufficiency for EOC. Additionally, it was suggested that petty cash be made available for emergency purchases.
DISCUSSION
The blackout that occurred on August 14, 2003, affected a substantial area of the Northeast United States, including all five boroughs of New York City. Although power was returned to the majority of the city by the evening of Saturday, August 16, DOHMH encountered several issues during its response to the emergency: failure of hospital emergency generators, large numbers of patients dependent on electrically powered medical equipment, and contamination of recreational waterways. DOHMH anticipated other potential problems, including spoilage of perishable foods, which could potentially result in foodborne disease and pest-control issues and vaccine spoilage. Indeed, syndromic surveillance did detect an increased incidence of gastrointestinal disease in New York City following the blackout.8 While responding to the blackout and resulting public health impacts, DOHMH was also able to maintain important routine functions, such as its burial desk, poison control call center, West Nile pesticide spraying activities, and 24-hour mental health referral hotline.
The events that occurred on September 11, 2001, provided New York City's public agencies with considerable experience in emergency response. For example, following 9/11, the DOHMH adopted the Incident Management System, a scalable, all-hazards approach to incident management used by many emergency response agencies. Our review of DOHMH's response to the blackout revealed that this unified command structure was an efficient means of managing the response. The system allows for easier communication among emergency response agencies during an event due to adoption of a common command structure and familiarity with response-specific language and procedures.
New York City was also affected by citywide blackouts in 1965 and 1977. DOHMH activities during the 1965 blackout were similar to the recent blackout.15,16 DOHMH monitored food wholesalers and retail stores for spoilage of food and monitored hospitals' admissions to detect increases in disease caused by spoiled food and or contaminated water.16 In addition, DOHMH monitored blood banks for the potential spoilage of banked blood because approximately one-third of the blood banks did not have emergency generators.16 In addition, 37% of New York City hospitals did not have emergency generators.16 Among the measures implemented in response to the 1965 blackout was a plan to have standby crews with 55 kW mobile generators to reduce the time required to provide auxiliary power to police and other agencies as needed.16
Communications were also an issue during the 1965 blackout. The DOHMH telephone system was without power, and because of a failure of several networks, citywide radio communications were also interrupted.16 Initial mobilization of personnel was successful during the 1965 blackout because it occurred during the shift change for civil employees. However, subsequent difficulties were encountered in attempts to locate specific personnel and to locate the post from which emergency operations of their respective departments were being directed. As a result of this blackout, a city EOC was established.16
The blackout of July 13–14, 1977, was dominated by criminal activities.17,18 During the 26.5 hours of the blackout, 3,418 persons were arrested, primarily for looting.17 No archived information was available on the activities of DOHMH during this incident.
Because of the events and evaluation of response to the previous blackouts in New York City, the DOHMH was better prepared for the blackout of 2003. However, our employee survey identified areas for further improvement (Figure 2). DOHMH is actively pursuing plans to address these identified needs.
Although blackouts affecting large parts of the United States are uncommon, blackouts can occur in association with natural disasters. Improvements in technology and other safeguards might reduce the incidence of future blackouts, but the possibility of blackouts associated with natural disasters will remain. Preparedness for blackouts is therefore of prime importance. DOHMH is improving its preparedness through a review of performance during the blackout. Because the events and responses are specific to New York City, other municipalities should consider the particulars of their own resources and requirements when enhancing their preparedness for blackouts. In an effort to develop more general guidance for blackout preparedness, DOHMH shared its experiences with the Centers for Disease Control and Prevention in the development of a guide to blackout preparedness: Power Outages: Public Health Issues and Recommendations.19
REFERENCES
- 1.Norcross ED, Elliott BM, Adams DB, Crawford FA. Impact of a major hurricane on surgical services in a university hospital. Am Surg. 1993;59:28–33. [PubMed] [Google Scholar]
- 2.Iwamoto S, Isibasi M, Moriyama M, Kobayasi H, Ogino K, Hobara T, et al. Effects of typhoon-caused power failure on medical care facilities [Japanese] Nippon Koshu Eisei Zasºshi. 1993;40(2):115–22. [PubMed] [Google Scholar]
- 3.O'Hara JF, Jr, Higgins TL. Total electrical power failure in a cardiothoracic intensive care unit. Crit Care Med. 1992;20:840–5. doi: 10.1097/00003246-199206000-00023. [DOI] [PubMed] [Google Scholar]
- 4.Hargrove M, Ramish BC, O'Donnell A, Aherne T. Electrical failure during cardiopulmonary bypass: an evaluation of incidence, causes, management and guidelines for preventive measures. Perfusion. 2002;17:369–72. doi: 10.1191/0267659102pf592oa. [DOI] [PubMed] [Google Scholar]
- 5.Spivak M. Bay Area power outage. EMS response to city-wide power outage. Emerg Med Serv. 1999;28:72–3. [PubMed] [Google Scholar]
- 6.Schaeffer HA, Salazar JD. The effect of the New York City power failure on a neonatal intensive care unit. Pediatr Ann. 1978;7:240–2. [PubMed] [Google Scholar]
- 7.Framework for program evaluation in public health. MMWR Morb Mortal Wkly Rep. 1999;48:RR–11. [PubMed] [Google Scholar]
- 8.Investigation of diarrheal illness detected through syndromic surveillance after a massive blackout—New York City August 2003. MMWR Morb Mortal Wkly Rep. 2004;53(Suppl):251. [Google Scholar]
- 9.New York City Emergency Response Task Force (City of New York, Office of the Mayor) Enhancing New York City's emergency preparedness: a report to Mayor Michael R. Bloomberg. 2003. Oct 28,
- 10.Greenwald P, Rutherford A, Green R, Giglio J. Emergency department visits for home medical device failure during the 2003 North America blackout. Acad Emerg Med. 2004;11:786–9. doi: 10.1197/j.aem.2003.12.032. [DOI] [PubMed] [Google Scholar]
- 11.Prezant D, Clair J, Belyaev S, Alleyne D, Banauch G, Davitt M, et al. Effects of the August 2003 blackout on the New York City healthcare delivery system: a lesson for disaster preparedness. Crit Care Med. 2005;33(1 Suppl):S96–101. doi: 10.1097/01.ccm.0000150956.90030.23. [DOI] [PubMed] [Google Scholar]
- 12.Eachempati S, Mick S, Barie P. The impact of the 2003 blackout on a Level 1 trauma center: lessons learned and implications for injury prevention. J Trauma. 2004;57:1127–31. doi: 10.1097/01.ta.0000141891.51102.28. [DOI] [PubMed] [Google Scholar]
- 13.Bureau of Vital Statistics; New York City Department of Health and Mental Hygiene. Summary of the vital statistics 2003. New York: New York City Department of Health and Mental Hygiene; 2004. Deaths caused by the blackout; p. 53. [Google Scholar]
- 14.Heffernan R, Mostashari F, Das D, Karpati A, Kulldorff M, Weiss D. Syndromic surveillance in public health practice, New York City. Emerg Infect Dis. 2004;10:858–64. doi: 10.3201/eid1005.030646. [DOI] [PubMed] [Google Scholar]
- 15.Wagner RF (Office of the Mayor, New York City) New York City Power failure—1965. New York City: Office of the Mayor. 1965 Nov 10; [Google Scholar]
- 16.Emergency Control Board (Office of the Mayor, New York City) Recommended measures to meet emergency conditions caused by a power blackout. New York City: Office of the Mayor. 1965. Dec 21,
- 17.Scoppetta N (Office of the Deputy Mayor for Criminal Justice, New York City) Report concerning the effects of the blackout of July 13–14, 1977 on the criminal justice system in New York City. New York City: Office of the Deputy Mayor for Criminal Justice. 1977 Sep 2; [Google Scholar]
- 18.Department of City Planning (New York City) Blackout commercial damage survey. New York City: Department of City Planning; 1977. Jul, [Google Scholar]
- 19.MMWR Morb Mortal Wkly Rep. 2005. Power outages public health issues and recommendations. In press. [Google Scholar]