Abstract
Little is known about the mechanisms converting psychosocial stress into cellular dysfunction. Various genes, up-regulated in atherosclerosis but also by psychosocial stress, are controlled by the transcription factor nuclear factor κB (NF-κB). Therefore, NF-κB is a good candidate to convert psychosocial stress into cellular activation. Volunteers were subjected to a brief laboratory stress test and NF-κB activity was determined in peripheral blood mononuclear cells (PBMC), as a window into the body and because PBMC play a role in diseases such as atherosclerosis. In 17 of 19 volunteers, NF-κB was rapidly induced during stress exposure, in parallel with elevated levels of catecholamines and cortisol, and returned to basal levels within 60 min. To model this response, mice transgenic for a strictly NF-κB-controlled β-globin transgene were stressed by immobilization. Immobilization resulted in increased β-globin expression, which could be reduced in the presence of the α1-adrenergic inhibitor prazosin. To define the role of adrenergic stimulation in the up-regulation of NF-κB, THP-1 cells were induced with physiological amounts of catecholamines for 10 min. Only noradrenaline resulted in a dose- and time-dependent induction of NF-κB and NF-κB-dependent gene expression, which depended on pertussis-toxin-sensitive G protein-mediated phosphophatidylinositol 3-kinase, Ras/Raf, and mitogen-activated protein kinase activation. Induction was reduced by α1- and β-adrenergic inhibitors. Thus, noradrenaline-dependent adrenergic stimulation results in activation of NF-κB in vitro and in vivo. Activation of NF-κB represents a downstream effector for the neuroendocrine response to stressful psychosocial events and links changes in the activity of the neuroendocrine axis to the cellular response.
The cardiovascular system is a target of psychosocial stress associated with exercise-induced myocardial ischemia, increases in blood pressure, heart rate, and arrythmias, development of arteriosclerosis, and death (1–4). Potential toxic elements in the personality construct such as hostility, anger, cynicism, mistrust, and unhealthy lifestyle (1, 5, 6), as well as social isolation (5), lack of social support (6), and work-related stress (7), increase the risk for cardiovascular disease, suggesting a strong causal relationship between chronic stress and the development of atherosclerosis (1). Intervention studies in cynomolgus monkeys support this concept, showing not only activation of these processes by mental stress but also reduction of vascular dysfunction and disease by reducing psychosocial stress through β-adrenergic blockade (8–12). Consistently, behavioral interventions, stress reduction, and stress management demonstrated benefits over and above usual medical care in hypertensive African Americans (13) and in cardiac patients with evidence of myocardial ischemia (14–18).
Recent data have indicated an interplay among hypothalamus, pituitary gland, adrenal medulla, and sympathetic nerve terminals as the neuroendocrine response to stress. Further downstream signals converting psychosocial stress into cellular dysfunction and finally into vascular disease are still largely unknown. One observation pointing to a potential mechanism is the induction of inflammatory reactions and the simultaneous decrease of antiinflammatory reactions leading to enhanced cytokine release and monocytic cell activation (19–23). These changes in mononuclear properties are consistent with the activation of the redox-sensitive transcription factor nuclear factor κB (NF-κB) (24–29).
Indirect evidence for a role of NF-κB in mediating cellular effects in response to psychosocial stress comes from animal studies describing stress-increased NF-κB activation and subsequent NF-κB-dependent gene expression in the brain cortex of rats exposed to immobilization stress (30). Increased NF-κB activation also has been described in blood lymphocytes of women stressed by the experience of breast biopsy (31), an extreme life-threatening stress situation characterized by anxiety and desperation, not comparable to other forms of psychosocial stress. The goal of the present study was to define mechanisms by which more ordinary psychosocial stressors that activate the neuroendocrine axis are converted into mononuclear cell activation in healthy volunteers, animal models, and cultured cells, with implications for a gradual wear and tear on the individual.‡‡
Materials and Methods
Reagents.
Adrenaline (epinephrine), noradrenaline (norepinephrine), prazosin, yohimbine, butoxamine, metoprolol, SB203580, H7, cholera toxin, and pertussis toxin were obtained from Sigma. Wortmannin, ZM 336372, AFC, Sulindaic acid, U0126, PD98059, and the p38-inhibitor were purchased from Calbiochem. Thioctic acid was provided by Asta-Medica (Frankfurt, Germany).
Human Subjects.
Nineteen volunteers (8 men, 11 women; mean age 24.8 ± 4.8 yr) were recruited for this study. All were drug-free nonsmokers and apparently healthy according to a brief medical examination. They were paid for participation.
Laboratory Stressor Test.
For stress-induced stimulation of the hypothalamus-pituitary-adrenal axis, subjects were exposed to the Trier social stress test (TSST; 32). The TSST mainly consists of a free speech and a mental arithmetic task in front of an audience for 15 min, including introduction to the free speech and a preparation phase. Blood samples for peripheral blood mononuclear cells (PBMC) isolation were taken 1 min before (−1 min), immediately after (10 min), and 60 min after stress induction.
Determination of Adrenocorticotropic Hormone (ACTH), Cortisol, and Catecholamine Levels.
ACTH plasma levels were measured with a commercial two-site RIA kit (Nichols Institute, Bad Nauheim, Germany). Salivary cortisol levels were determined by a time-resolved immunoassay with fluorometric detection as described (33). Adrenaline (AD, epinephrine) and noradrenaline (NA, norepinephrine) were assayed by HPLC with electrochemical detection, as described by Smedes et al. (34).
Cell Culture.
Human promonocytic THP-1 cells (cell culture collection of the German Cancer Research Institute, Heidelberg, Germany) were maintained in RPMI medium 1640 containing, 50 μM 1-2-mercaptoethanol, 2 mM l-glutamine, and 100 units/ml penicillin, 100 μg/ml streptomycin (all BioWhittaker) and 5% FCS (Gibco) (35) and seeded 1 d before the experiments.
Preparation of PBMC.
PBMC were separated immediately after venipuncture as described (24, 25), analyzed microscopically, and counted by one investigator (J.W.). The cell number was adjusted to 1 × 106 PBMC per ml.
Electrophoretic Mobility-Shift Assay (EMSA).
Nuclear proteins were prepared and assayed for transcription factor-binding activity by using NF-κB- or Oct-1- consensus oligonucleotides (Promega) as described (24, 25).
Transgenic Mouse Model.
Mice transgenic for an NF-κB-driven β-globin reporter gene (tg14) were provided by T. Wirth (Ulm, Germany) and have been characterized in detail (36). Healthy male mice (8 wk old) were housed in groups of four mice per cage with a 12 h light/12 h dark cycle and free access to food and water. Procedures in this study were approved by the Animal Care and Use Committee at the Regierungspräsidium Karlsruhe, Germany.
Mental Stress Induction by Immobilization.
Mice were divided into three groups and isolated in single cages without any access to food 3 h before the experiment. Control mice were left untreated, whereas mice stressed by immobilization were fixed in a small tube that did not allow further movement during the immobilization period. The third group received 1 mg/kg body weight prazosin (37) 45 min before immobilization. At the end of the immobilization period, mice were killed. Total blood was taken by heart puncture and immediately quick-frozen.
RT-PCR.
RT-PCR for β-globin and β-actin was performed as described (25) by using 1 μg of total RNA as starting material. RT-PCR for human IL-6 was performed by using the following primers and conditions: hIL-6-forward, 5′-AATTCGGTACATCCTCGACG-3′; hIL-6-reverse, 5′-GCGCAGAATGAGATGAGTTG-3′; 1 time at 94°C for 240 s; 30 times at 94°C for 45 s, at 55°C for 45 s, and at 72°C for 45 s; and 1 time at 72°C for 600 s. The PCR products were separated onto 1.5–2% agarose gels and visualized by ethidium bromide staining. Amplification of β-actin served as control for sample loading and integrity. Reactions lacking template RNA or AMV-reverse transcriptase served as internal controls.
Statistical Analysis.
All values are given as mean, with the bars showing the SEM. The means of groups were compared by ANOVA by using the Student's t test to correct for multiple comparisons. P < 0.05 was considered to be statistically significant.
Results
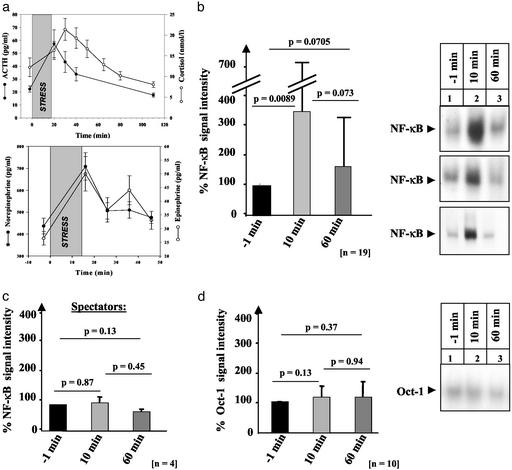
The mechanism by which the neuroendocrine response, activated by psychosocial stress, converts stress into changes of mononuclear cell function was studied in 19 healthy volunteers (mean age 24.8 ± 4.8 yr) monitoring activation of the transcription factor NF-κB (24, 25). Volunteers were exposed to the TSST (32). ACTH and cortisol plasma levels served as markers of the endocrine stress response, demonstrating the expected significant increases in ACTH and cortisol after stress (P < 0.0001; Fig. 1a Upper). The TSST further significantly increased AD and NA levels already 1 min after stress induction. (Fig. 1a Lower). The TSST-mediated induction of NF-κB-binding activity from 100% to 341% (P = 0.0089) observed in PBMC 10 min after stress induction (Fig. 1b) was paralleled by the stress-dependent increase in ACTH, cortisol, and catecholamines, suggesting a rapid NF-κB activation after a brief period (i.e., 10 min) of psychosocial stress.
Figure 1.
Psychosocial stress induces the transcription factor NF-κB in healthy volunteers undergoing the TSST. (a) ACTH, salivary cortisol (Upper) and AD and NA levels (Lower), expressed as mean ± SEM, of healthy volunteers exposed to the TSST (shaded area). (b and c) NF-κB-binding activity was monitored by EMSA in PBMC before (−1 min), immediately after (10 min), and 60 min after stress induction in 19 volunteers (b) and four spectators of the TSST (c) and evaluated by densitometry. The mean ± SEM is reported. (d) Ten occasionally selected nuclear extracts studied in b were assayed for Oct-1-binding activity and evaluated by densitometry. The mean ± SEM is reported.
NF-κB-binding activity consisted of the NF-κB heterodimer NF-κBp50/p65 (data not shown). After mental stress induction (60 min), NF-κB-binding activity had almost completely returned to baseline (166%; P = 0.073) (Fig. 1b). Although the intensity of NF-κB-binding activity decreased in the recovery period, the composition of the NF-κB subunits contributing to the NF-κB-binding activity did not change (data not shown). Two subjects, characterized by the absence of a stress-dependent increase in catecholamines, ACTH, and cortisol, did not induce NF-κB-binding activity, indicating that NF-κB activation depends on the acute response to psychosocial stress.
To exclude the possibility that factors other than the TSST-mediated psychosocial stress account for the increase in NF-κB-binding activity, PBMC were isolated from four randomly selected spectators watching the TSST and also assayed for NF-κB-binding activity. In none of the spectators, up-regulation of NF-κB could be observed during the assay period (Fig. 1c). This suggests that the rapid NF-κB activation observed in volunteers undergoing the TSST was indeed caused by psychosocial stress. Because psychosocial stress has been described to increase the lymphocyte and monocyte population (21), PBMC had been adjusted to the same cell number before NF-κB-binding activity was determined. To exclude that differences in the quality of the nuclear extracts or nonspecific cell activation account for the induction pattern observed, binding activity of the basal transcription factor OCT-1, known to be in general not activated by stimuli of NF-κB (24, 26), was determined. No changes in OCT-1-binding activity were detected (Fig. 1d Right), as shown for one representative subject (Fig. 1d Left).
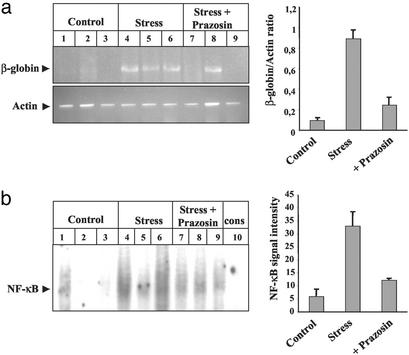
The functional relevance of the stress-induced NF-κB-binding activity was demonstrated in 8-wk-old male transgenic mice carrying a β-globin reporter gene controlled by three consecutive NF-κB sites (36), subjected to immobilization stress for 20 min. Constitutive expression of the β-globin transgene is restricted to lymphoid tissues (36), whereas activation of the NF-κB p50/p65-heterodimer confers inducible transgene activation in all cells (36). Only weak signals for β-globin mRNA could be detected in control mice (Fig. 2a Upper, lanes 1–3). In contrast, blood samples of immobilized mice demonstrated a strong increase in β-globin mRNA (Fig. 2a Upper, lanes 4–6). To define neuroendocrine mediators responsible for NF-κB activation, immobilized mice were pretreated with the α1-antagonist prazosin (1 mg/kg), known to reduce immobilization stress-mediated immediate early gene expression in the mouse brain (37). Stress-induced β-globin transcription was reduced in this group of mice (Fig. 2a Upper, lanes 7–9). IL-6-mRNA, in part regulated by NF-κB, was also induced in response to immobilization and reduced in the presence of prazosin (data not shown). RT-PCR for β-actin served as an internal control and confirmed the comparable RNA-input in each reaction (Fig. 2a Lower). EMSA with nuclear extracts derived from the same blood samples demonstrated a prominent increase in NF-κB-binding activity only in those mice that had been exposed to immobilization (Fig. 2b, lanes 4–6), whereas NF-κB-binding activity in mice pretreated with α1-adrenergic antagonists did not exceed basal activation levels (Fig. 2b, lanes 7–9). These data confirm that mental stress can be converted into functionally significant cellular NF-κB activation.
Figure 2.
Immobilization stress induces NF-κB-dependent gene expression in β-globin transgenic mice. β-globin transgenic mice were left untreated (lanes 1–3) or subjected to immobilization stress for 20 min in the absence (lanes 4–6) or presence (lanes 7–9) of the α1-adrenergic inhibitor prazosin, applied 45 min before immobilization. Three mice were used in each group. (a) Total RNA was prepared from blood and analyzed by RT-PCR for β-globin-transgene (Upper) and β-actin (Lower) transcription. Gel-separated PCR products were quantified by densitometry, and the ratio of β-globin/β-actin was calculated. (b) Nuclear extracts were prepared from the blood investigated above and analyzed for NF-κB-binding activity in EMSA. To confirm NF-κB binding, nuclear extract from an immobilized mouse was competed with a 160-fold molar excess of unlabeled NF-κB consensus oligonucleotides (lane 10). The bar graphs on the right summarize the results obtained in all mice studied. The mean ± SEM is reported.
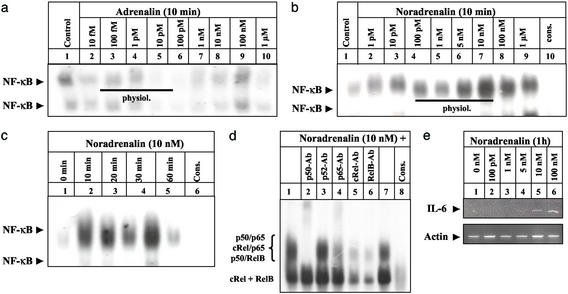
To define the impact of catecholamines on psychosocial stress-dependent NF-κB activation observed in PBMC, we studied whether AD and NA induced NF-κB activation in the human monocyte cell line THP-1. When cultured THP-1 cells were stimulated with 10 fM to 1 μM AD (Fig. 3a) or NA (Fig. 3b), the concentration of AD needed to significantly induce NF-κB-binding activity (Fig. 3a) was 100-fold higher than the concentration determined in volunteers undergoing the TSST. In contrast, physiological concentrations of NA were sufficient to result in a significant increase in NF-κB-binding activity in a dose- (Fig. 3b) and time-dependent manner (Fig. 3c). The NF-κB subunits contributing to the NA-induced NF-κB binding in THP-1 cells were identified as p50, p65, cRel, and Rel B (Fig. 3d). RT-PCR demonstrated that the observed increase in NF-κB-binding activity was functionally significant because NA induced a dose-dependent increase in NF-κB regulated IL-6 transcription in these cells (Fig. 3e).
Figure 3.
Physiological concentrations of NA induce functionally significant NF-κB-binding activity in cultured THP-1 monocytic cells. (a and b) THP-1 cells were left untreated (lane 1) or incubated with increasing concentrations of AD (a) and NA (b) for 10 min (lanes 2–9) before NF-κB-binding activity was monitored. NF-κB binding was confirmed by competing with a 160-fold molar excess of unlabeled NF-κB consensus oligonucleotides (b; cons, lane 10). A black line indicates the physiological concentration range of AD and NA. The experiment was repeated two times with identical results and one representative experiment is shown. (c) THP-1 cells were either left untreated (0 h) or stimulated with NA (10 nM) for 10 min to 1 h (lanes 2- 5), and nuclear extracts were assayed for NF-κB-binding activity as above. The experiment was performed twice with identical results and one representative experiment is shown. (d) Characterization of the NF-κB subunits contributing to the NA-induced-binding activity at the NF-κB consensus sequence (lanes 1 and 7) was performed by including 2.5 μg of anti-p50 (lane 2), anti-p52 (lane 3), anti-p65 (lane 4), anti-cRel (lane 5), or anti-relB (lane 6) Abs in the binding reaction. Specificity of NF-κB binding was confirmed as above (lane 10). The position of the different NF-κB complexes formed is indicated at the left. (e) THP-1 cells were either left untreated (0 h) or stimulated with different concentrations of NA (lanes 2–6) for 1 h. Total RNA was prepared and analyzed by RT-PCR with primers specific for human IL-6 and β-actin, respectively.
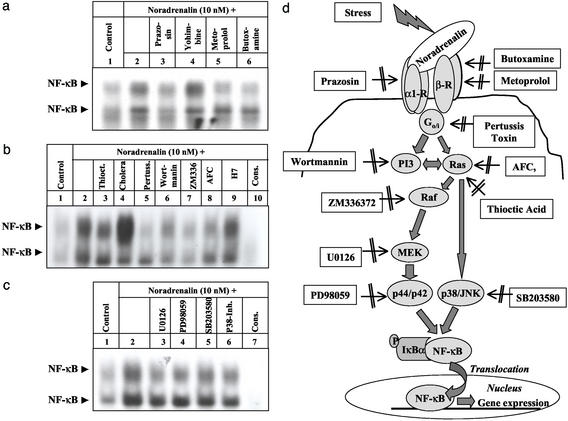
Next, cells were preincubated for 45 min in the presence of α- and β-antagonists before stimulation with 10 nM NA for 10 min (Fig. 4a). Consistent with the observation in immobilized mice (Fig. 2), preincubation with the α1-antagonist prazosin (1 nM) resulted in a significant decrease in NF-κB-binding activity (Fig. 4a, lane 3). The β1-antagonist metoprolol (100 nM) and the β2-antagonist butoxamine (25 nM) also reduced the NA-dependent NF-κB response (Fig. 4a, lanes 5 and 6). The α2-antagonist yohimbine (10 nM) had no effect (Fig. 4a, lane 4), indicating that α1- and β-adrenergic receptors act in concert to mediate NA-dependent NF-κB activation in THP-1 cells.
Figure 4.
Biochemical characterization of the signaling pathways involved in NA-dependent NF-κB activation in cultured THP-1 monocytic cells. THP-1 were left untreated (lane 1) or incubated with NA (10 nM) for 10 min in the absence (lane 2) or presence of either the adrenergic inhibitors prazosin (1 nM, lane 3), yohimbine (10 nM, lane 4), metoprolol (100 nM, lane 5), or butoxamine (25 nM, lane 6) (a), or the pathway inhibitors thioctic acid (2 mM, lane 3), cholera toxin (5 μg/ml, lane 4), Ptx (400 ng/ml, lane 5), wortmannin (100 nM, lane 6), ZM336372 (1 μM, lane 7), AFC (50 μM, lane 8), and H7 (100 μM, lane 9) (b), and the MEK and MAPK inhibitors U0126 (50 μM, lane 3), PD98059 (30 μM, lane 4), SB203580 (20 nM, lane 5), and p38 inhibitor (10 μM, lane 6) (c), respectively. Inhibitors were added to the cells 45 min before NA induction. Nuclear extracts were assayed for NF-κB-binding activity, monitored in EMSA. Specificity of NF-κB binding was confirmed as above (cons). The experiments were repeated three (b and c) to five (a) times with identical results and confirmed by NF-κBp65-specific ELISA. One representative experiment is shown. (d) Schematic representation of the proposed mechanism of psychosocial stress-induced NF-κB activation. Psychosocial stress induces NA that binds to α1- and β-adrenergic receptors, which in turn recruit Ptx-sensitive G proteins. G proteins activate directly or indirectly via PI3-kinase Ras interacting with its effector kinase Raf subsequently. Raf phosphorylates MEK-1 and -2, which activates p44/p42-MAPK. In addition, Ras, which is a target of cellular oxidative stress, can directly induce p38-MAPK activation. Activated MAPKs induce as-yet uncharacterized downstream-located signaling pathways that result in phosphorylation and degradation of the NF-κB-specific cytoplasmic inhibitor IκBα and subsequent activation and nuclear translocation of NF-κB. The inhibitors used to identify different steps in the signaling cascades are given in boxes.
To further identify the cellular signaling cascades involved, THP-1 cells were incubated for 45 min with specific inhibitors of cellular transduction pathways before stimulation with NA (10 nM) for 10 min. NF-κB-binding activity was monitored in EMSA and results were confirmed by using NF-κBp65-specific ELISA (data not shown). Thioctic acid (2 mM), known to inhibit reactive oxygen species-mediated NF-κB activation (38), reduced NA-dependent NF-κB activation by 23% (Fig. 4b, lane 3). Consistent with a linkage of G protein activation to adrenergic signal transduction (39), preincubation with cholera toxin (5 μg/ml), stimulating Gs, increased NA-induced NF-κB activation (Fig. 4b, lane 4) and pertussis toxin (Ptx; 400 ng/ml), inhibiting G(o)/G(i)-dependent signaling, reduced NA-dependent up-regulation of NF-κB by 60% (Fig. 4b, lane 5). A reduction of NF-κB-binding activity was further observed in the presence of wortmannin (100 nM, Fig. 4b, lane 6), an inhibitor of PI3-kinase, ZM336372 (1 μM, Fig. 4b, lane 7), an inhibitor of the serine/threonine kinase Raf and the farnesyl transferase inhibitor AFC (50 μM; Fig. 3b, lane 8), which inhibits Ras activation. In contrast, 1-(5′-isoquinolinesulfonyl)-2-methylpiperazine (H7; 100 μM, Fig. 4b, lane 9), which inhibits both cAMP-dependent protein kinase A and protein kinase C, reduced NA-dependent NF-κB activation <10%. U0126, an inhibitor of the mitogen-activated protein kinase (MAPK)-kinases MEK1 and MEK2 (50 μM; Fig. 4c, lane 3), the extracellular signal-regulated protein-kinases-1 (ERK-1, p44-MAPK) and -2 (ERK-2, p42-MAPK) inhibitor PD98059 (30 μM; Fig. 4c, lane 4), the p38-MAPK/Jun-NH2-kinase (JNK)-inhibitor SB203580 (20 nM, Fig. 4c, lane 5), and a specific p38MAPK-inhibitor (10 μM, Fig. 4c, lane 6) all resulted in partial reduction of NA-induced NF-κB-binding activity. These results strongly suggest that NA-induced adrenergic activation of Ptx-sensitive G proteins results in PI3-kinase, Ras/Raf, and MAPK signaling (Fig. 4d), which seems to be central in stress-dependent NF-κB activation in vitro and in vivo.
Discussion
Atherosclerosis and changes in the immune system are consequences of psychosocial stress (1, 5, 6). Although the endocrine response to psychosocial stress and their impact on the cardiovascular system, including changes in blood pressure and heart rate, have frequently been described (e.g., refs. 1–6 and 14–18), much less is known about the molecular mechanisms converting psychosocial stress into cellular activation. Here we present an adrenergic signaling pathway that explains the rapid increase in activation of the transcription factor NF-κB observed in PBMC shortly after exposure to psychosocial stress, thus linking psychosocial stress to mononuclear cell activation and subsequent changes in the immune system. This extends previous work showing a role of catecholamines in the mechanism for atherosclerosis (8–12). The observation that mental stress in humans and rodents results in nuclear translocation of NF-κB and changes in transcriptional activity thus closes an important gap in understanding the cellular consequences of psychosocial stress. Induction of NF-κB is in part dependent on the interaction of NA with α1- and β-adrenergic receptors. The NA-dependent adrenergic signal transduction is mediated by Ptx-sensitive G proteins inducing PI3-kinase and Ras/Raf signaling that results in MAPK activation and subsequent NF-κB induction (Fig. 4). The observation that binding activity of NF-κB, but not of Oct-1, was altered (Fig. 1 b and d) further confirms that psychosocial stress elicits a receptor-dependent specific signal rather than a nonspecific cell activation. NF-κB activation is supposed to contribute to the pathophysiology of lifestyle-related diseases such as diabetes mellitus, cardiovascular disease, and atherosclerosis (24–29, 38, 40, 57), implicating psychosocial stress-dependent NF-κB activation in the cumulative burden that finally leads to morbidity and mortality.
Identification of Cellular Pathways.
Identification of the NA-induced signaling cascades in mononuclear cells is not only providing a more definite knowledge of a mechanism linking psychosocial stress and catecholamine release to changes in cellular function, but it also provides a tool to directly monitor cellular events caused by such stressors. Consistent with a recently reported linkage of G protein-coupled receptors to MAPK signaling through PI3-kinase γ (41), NA-mediated adrenergic activation of Ptx-sensitive G proteins results in PI3-kinase and Ras activation. On activation, Ras interacts with the serine/threonine kinase Raf, an effector kinase of Ras (42, 43). Subsequently, Raf can phosphorylate MEK1 and MEK2 (44), which in turn phosphorylate and activate ERK-1 and -2 (p44/p42-MAPK) (44). In addition, Ras is supposed to directly participate in p38-MAPK activation (45) and to represent a signaling target for free radicals and cellular redox stress (46). Consistently, NA-dependent activation of NF-κB was inhibited in the presence of PI3-kinase, Ras, Raf, and MAPK inhibitors and by the antioxidant thioctic acid as summarized in Fig. 4d. These findings point to a central role of MAPK in stress-dependent NF-κB activation in vitro and in vivo and are in accordance with a previous report demonstrating NA-dependent ERK-2-phosphorylation in human PBMC (47).
Possible Role of NF-κB Activation as a Pathway Leading to Atherosclerosis.
PBMC are circulating cells playing an important role in vascular disease, inflammation, and immune response. The NA-triggered signaling cascades in mononuclear cells involve PI3-kinase, Ras/Raf, and members of the MAPK family and thus resemble the NA-induced-signaling pathways described in vascular cells (48–54), although NF-κB activation has not yet been studied in these cells. NA-dependent activation of similar signal transduction cascades in various cell types implies that the cellular response to stress uses comparable pathways and suggests that monitoring stress-dependent cellular activation in PBMC might allow estimation of the effect of psychosocial stress on allostasis and its impact on the allostatic load (55). The consistent results obtained in healthy volunteers, animal studies, and studies in vitro provide strong evidence that the mechanism described is not only observed in a single model, but may be applicable to rather different situations with increased NA release as the common denominator. However, it remains unknown whether the changes induced by a brief psychosocial stressor are indeed sufficient to explain the relation of psychosocial stress to cardiovascular disease (1–15). It is more likely that a repeated exposure to adverse, i.e., stressful, life events with failure to habituate biologically to these circumstances will convey the well documented disease outcomes (56). A number of pathophysiologically relevant cellular perturbants such as high glucose, advanced glycation end products, S100-proteins, and amyloid-β peptides have been shown not only to induce NF-κB, but also to perpetuate its activation by engagement of the receptor RAGE (25, 40, 57). In chronic diseases, in which these RAGE ligands are abundantly expressed, psychosocial stress-induced NF-κB activation might not only be amplified, but converted to a constant threat (25, 57). Clinical and experimental studies provide evidence that lowering psychosocial stress by β-adrenergic inhibitors (9, 11, 12) and/or stress management (13–16) lead to reduction of the intima media thickness (13) and the overall cardiovascular mortality (14, 15).
Modulation of NF-κB Activation.
The relation of NF-κB activation to cellular dysfunction and vascular disease has been directly established by using genetic approaches to overexpress the NF-κB-specific inhibitor IκBα (28) and by indirect studies looking at the presence of cells with nuclear located NF-κB in vascular disease (24–27, 29). A cooperative action of catecholamines regulating receptor expression and other stress response modifiers might act in concert in controlling cell activation. High concentrations of NA have been described to induce phosphorylation of α1(a)-adrenergic receptors and thereby block receptor action (58). AD release correlates with the extent of NF-κB activation (data not shown), although the AD concentrations achieved in volunteers undergoing the TSST are much to low compared to the concentration of AD required for induction of NF-κB activation in vitro (Figs. 1a and 3a). This implies that low doses of AD might act synergistically with NA and thereby further increase NF-κB activation. A further level of complexity is added by the large differences in the time required to down-regulate NF-κB activation to baseline, which cannot simply be explained by the NF-κB activation inhibiting properties of cortisol (59) because cortisol levels did not significantly differ in the volunteers studied. β-adrenergic agonists exert antiinflammatory effects in monocytic cells by increasing cytoplasmic levels of IκBα (60), implying that the individual proinflammatory responses to psychosocial stress might determine the extent of the antiinflammatory down-regulation. The fact that expression of β2-adrenergic receptors itself is at least in part regulated by NF-κB (61) indicates that the activation of NF-κB might not only be terminating itself by a negative IκBα-dependent feed back loop (27), but that activation of NF-κB by α-adrenergic receptors terminates itself by induction of β2 receptors able to antagonize the proinflammatory challenge (60). Future studies are required to define mechanisms influencing the down-regulation of elevated NF-κB in response to psychosocial stress. The data presented here provide strong evidence for a specific pathway through which psychosocial stress signals are converted into mononuclear cell activation (Fig. 4d). This might open a window to a more profound understanding of the mechanisms linking stress and disease.
Acknowledgments
We thank Dr. T. Wirth (Ulm, Germany) for providing the β-globin-transgenic mice, Dr. H. Tritschler at Asta-Medica (Frankfurt, Germany) for the gift of thioctic acid, and S. Götz and M. Kanitz for technical assistance. This work was in part supported by Deutsche Forschungsgemeinschaft Grants Na 138/5-3 (to P.P.N.) and Ki 537/9-3 (to C.K.), Stiftung Verum (P.P.N.), and Asta-Medica (A.B.).
Abbreviations
- AD
adrenaline
- EMSA
electrophoretic mobility-shift assay
- NA
noradrenaline
- NF-κB
nuclear factor κB
- TSST
Trier social stress test
- Ptx
pertussis toxin
- PI3-kinase
phosphatidylinositol 3-kinase
- MAPK
mitogen-activated protein kinase
- PBMC
peripheral blood mononuclear cell
- AD
adrenaline
- NA
noradrenaline
- ACTH
adrenocorticotropic hormone
Footnotes
This work was presented in part at the 44th meeting of the German Society for Endocrinology, May 31–June 3, 2000, Munich, Germany, the 46th meeting of the German Society for Thrombosis and Hemostasis, Feb. 20–23, 2002, Erfurt, Germany, and the 46th meeting of the German Society for Endocrinology, Feb. 27–March 3, 2002, Göttingen, Germany.
References
- 1.Rozanski A, Blumenthal J A, Kaplan J. Circulation. 2000;99:2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 2.Kaprio J, Koskenvuo M, Rita H. Am J Public Health. 1987;77:283–287. doi: 10.2105/ajph.77.3.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leor J, Poole W K, Kloner R A. N Engl J Med. 1996;334:413–419. doi: 10.1056/NEJM199602153340701. [DOI] [PubMed] [Google Scholar]
- 4.Meisel S R, Kutz I, Dayan K I, Pauzner H, Chetboun I, Arbel Y, David D. Lancet. 1991;338:660–661. doi: 10.1016/0140-6736(91)91234-l. [DOI] [PubMed] [Google Scholar]
- 5.Stansfeld S A, Fuhrer R, Shipley M J, Marmot M G. Int J Epidemiol. 2002;31:248–255. doi: 10.1093/ije/31.1.248. [DOI] [PubMed] [Google Scholar]
- 6.Berkman L F, Leo-Summers L, Horwitz R I. Ann Intern Med. 1992;117:1003–1009. doi: 10.7326/0003-4819-117-12-1003. [DOI] [PubMed] [Google Scholar]
- 7.Bosma H, Peter R, Siegrist J, Marmot M. Am J Public Health. 1998;88:68–74. doi: 10.2105/ajph.88.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaplan J R, Manuck S S, Clarkson T B, Lusso F M, Taub D M, Miller E W. Science. 1983;220:733–735. doi: 10.1126/science.6836311. [DOI] [PubMed] [Google Scholar]
- 9.Kaplan J R, Manuck S B, Adams M R, Weingand K W, Clarkson T B. Circulation. 1987;76:1365–1372. doi: 10.1161/01.cir.76.6.1364. [DOI] [PubMed] [Google Scholar]
- 10.Williams J K, Vita J A, Manuck S B, Selwyn A P, Kaplan J R. Circulation. 1991;84:2146–2153. doi: 10.1161/01.cir.84.5.2146. [DOI] [PubMed] [Google Scholar]
- 11.Kaplan J R, Manuck S B. Am Heart J. 1994;128:1316–1328. doi: 10.1016/0002-8703(94)90254-2. [DOI] [PubMed] [Google Scholar]
- 12.Skantze H B, Kaplan J, Petterson K, Manuck S, Blomqvist M, Kyes R, Williams K, Bondjers G. Atherosclerosis. 1998;136:153–161. doi: 10.1016/s0021-9150(97)00202-5. [DOI] [PubMed] [Google Scholar]
- 13.Castillo-Richmond A, Schneider R H, Alexander C N, Cook R, Myers H, Nidich S, Haney C, Rainforth M, Salerno J. Stroke. 2000;31:568–573. doi: 10.1161/01.str.31.3.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blumenthal J A, Babyak M, Wei J, O'Connor C, Waugh R, Eisenstein E, Mark D, Sherwood A, Woodley P S, Irwin R J, et al. Am J Cardiol. 2002;89:164–168. doi: 10.1016/s0002-9149(01)02194-4. [DOI] [PubMed] [Google Scholar]
- 15.Denollet J, Brutsaert D L. Circulation. 2001;104:2018–2023. doi: 10.1161/hc4201.097940. [DOI] [PubMed] [Google Scholar]
- 16.King M S, Carr T, D'Cruz C. Aust Fam Physician. 2002;31:164–168. [PubMed] [Google Scholar]
- 17.Charvat J, Dell P, Folkow B. Cardiologia. 1964;44:121–141. doi: 10.1159/000167892. [DOI] [PubMed] [Google Scholar]
- 18.Cannon W B. Physiol Rev. 1929;9:399–431. [Google Scholar]
- 19.Dobbin J P, Harth M, Mc Cain G A, Martin R A, Cousin K. Brain Behav Immun. 1991;5:339–348. doi: 10.1016/0889-1591(91)90029-a. [DOI] [PubMed] [Google Scholar]
- 20.Song C, Kenis G, van Gastel A, Bosmans E, Lin A, de Jong R, Neels H, Scharpe S, Janca A, Yasukawa K, Maes M. Psychiatry Res. 1999;85:293–303. doi: 10.1016/s0165-1781(99)00012-8. [DOI] [PubMed] [Google Scholar]
- 21.Goebel M U, Mills P J, Irwin M R, Ziegler M G. Psychosom Med. 2000;62:591–598. doi: 10.1097/00006842-200007000-00019. [DOI] [PubMed] [Google Scholar]
- 22.Steptoe A, Willemsen G, Owen N, Flower L, Mohamed-Ali V. Clin Sci. 2001;101:185–192. [PubMed] [Google Scholar]
- 23.Altemus M, Rao B, Dhabhar F S, Ding W, Granstein R D. J Invest Dermatol. 2001;117:309–317. doi: 10.1046/j.1523-1747.2001.01373.x. [DOI] [PubMed] [Google Scholar]
- 24.Hofmann M, Schiekofer S, Isermann B, Kanitz M, Henkels M, Joswig M, Treusch A, Morcos M, Weiss T, Borcea V, et al. Diabetologia. 1999;42:222–232. doi: 10.1007/s001250051142. [DOI] [PubMed] [Google Scholar]
- 25.Bierhaus A, Schiekofer S, Schwaninger M, Andrassy M, Humpert P M, Chen J, Hong M, Luther T, Henle T, Kloting I, et al. Diabetes. 2001;50:2792–2808. doi: 10.2337/diabetes.50.12.2792. [DOI] [PubMed] [Google Scholar]
- 26.Ritchie M E. Circulation. 1998;98:1707–1713. doi: 10.1161/01.cir.98.17.1707. [DOI] [PubMed] [Google Scholar]
- 27.Collins T, Cybulsky M I. J Clin Invest. 2001;107:255–264. doi: 10.1172/JCI10373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Breuss J M, Cejna M, Bergmeister H, Kadl A, Baumgartl G, Steurer S, Xu Z, Koshelnick Y, Lipp J, De Martin R, et al. Circulation. 2002;105:633–638. doi: 10.1161/hc0502.102966. [DOI] [PubMed] [Google Scholar]
- 29.Yoshimura S, Morishita R, Hayashi K, Yamamoto K, Nakagami H, Kaneda Y, Sakai N, Ogihara T. Gene Ther. 2001;8:1635–1642. doi: 10.1038/sj.gt.3301566. [DOI] [PubMed] [Google Scholar]
- 30.Madrigal J L, Hurtado O, Moro M A, Lizasoain I, Lorenzo P, Castrilli A, Bosca L, Leza J C. Neuropsychopharmacology. 2002;26:155–163. doi: 10.1016/S0893-133X(01)00292-5. [DOI] [PubMed] [Google Scholar]
- 31.Nagabhushan M, Mathews H L, Witek-Janusek L. Brain Behav Immun. 2001;15:78–84. doi: 10.1006/brbi.2000.0589. [DOI] [PubMed] [Google Scholar]
- 32.Kirschbaum C, Pirke K M, Hellhammer D H. Neuropsychobiology. 1993;28:76–81. doi: 10.1159/000119004. [DOI] [PubMed] [Google Scholar]
- 33.Dressendörfer R A, Kirschbaum C, Rohde W. J Steroid Biochem Mol Biol. 1992;43:683–692. doi: 10.1016/0960-0760(92)90294-s. [DOI] [PubMed] [Google Scholar]
- 34.Smedes F, Kraak J C, Poppe H. J Chromatogr. 1982;231:25–39. doi: 10.1016/s0378-4347(00)80506-x. [DOI] [PubMed] [Google Scholar]
- 35.Takashiba S, Van Dyke T E, Amar S, Murayama Y, Soskolne A W, Shapira L. Infect Immun. 1999;67:5573–5578. doi: 10.1128/iai.67.11.5573-5578.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lernbecher T, Muller U, Wirth T. Nature. 1993;365:767–770. doi: 10.1038/365767a0. [DOI] [PubMed] [Google Scholar]
- 37.Stone E A, Zhang Y. Brain Res. 1995;694:279–286. doi: 10.1016/0006-8993(95)00882-q. [DOI] [PubMed] [Google Scholar]
- 38.Packer L. Drug Metab Rev. 1998;30:245–275. doi: 10.3109/03602539808996311. [DOI] [PubMed] [Google Scholar]
- 39.Williams N G, Zhong H, Minnemann K P. J Biol Chem. 1998;273:24624–24632. doi: 10.1074/jbc.273.38.24624. [DOI] [PubMed] [Google Scholar]
- 40.Evans J L, Goldfine I D, Maddux B A, Grodsky G M. Endocr Rev. 2002;23:599–622. doi: 10.1210/er.2001-0039. [DOI] [PubMed] [Google Scholar]
- 41.Lopez-Ilsaca M, Crespo P, Pellici P G, Gutkind J S, Wetzker R. Science. 1997;275:394–397. doi: 10.1126/science.275.5298.394. [DOI] [PubMed] [Google Scholar]
- 42.Marshall C J. Nature. 1996;383:127–128. doi: 10.1038/383127a0. [DOI] [PubMed] [Google Scholar]
- 43.Baumann B, Weber C K, Troppmaier J, Whiteside S, Israel A, Rapp U R, Wirth T. Proc Natl Acad Sci USA. 2000;97:4515–4620. doi: 10.1073/pnas.080583397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yoshizumi M, Tsuchiya K, Tamaki T. J Med Invest. 2001;48:11–24. [PubMed] [Google Scholar]
- 45.McDermott E P, O'Neill L A. J Biol Chem. 2002;277:7808–7815. doi: 10.1074/jbc.M108133200. [DOI] [PubMed] [Google Scholar]
- 46.Lander H M, Ogiste J S, Teng K K, Novogrodsky A. J Biol Chem. 1995;270:21195–21198. doi: 10.1074/jbc.270.36.21195. [DOI] [PubMed] [Google Scholar]
- 47.Rouppe van der Voort C, Kavelaars A, van de Pol M, Heijnen C J. J Neuroimmunol. 2000;108:82–91. doi: 10.1016/s0165-5728(00)00253-8. [DOI] [PubMed] [Google Scholar]
- 48.Hu Z W, Shi X Y, Lin R Z, Chen J, Hoffman B B. J Pharmacol Exp Ther. 1999;290:28–37. [PubMed] [Google Scholar]
- 49.Muthalif M M, Uddin M R, Fatima S, Parmentier J H, Khandekar Z, Malik K U. Prostaglandins Other Lipid Mediat. 2001;65:33–43. doi: 10.1016/s0090-6980(01)00112-5. [DOI] [PubMed] [Google Scholar]
- 50.Colombo F, Noel J, Mayers P, Mercier I, Calderone A. J Mol Cell Cardiol. 2001;33:1091–1106. doi: 10.1006/jmcc.2001.1381. [DOI] [PubMed] [Google Scholar]
- 51.Xiao L, Pimental D R, Amin J K, Singh K, Sawyer D B, Colucci W S. J Mol Cell Cardiol. 2001;33:779–787. doi: 10.1006/jmcc.2001.1348. [DOI] [PubMed] [Google Scholar]
- 52.Brett J G, Steinberg S F, deGroot P G, Nawroth P P, Stern D M. J Cell Biol. 1988;106:2109–2119. doi: 10.1083/jcb.106.6.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ward D T, Alder A C, Ohanian J, Ohanian V. J Vasc Res. 2002;39:1–11. doi: 10.1159/000048988. [DOI] [PubMed] [Google Scholar]
- 54.Ohanian J, Cunliffe P, Ceppi E, Alder A, Heerkens E, Ohanian V. Arterioscler Thromb Vasc Biol. 2001;21:1921–1927. doi: 10.1161/hq1201.100264. [DOI] [PubMed] [Google Scholar]
- 55.Karlamangla A, Singer B, McEwen B S, Rowe J, Seeman T. J Clin Epidemiol. 2002;55:696–710. doi: 10.1016/s0895-4356(02)00399-2. [DOI] [PubMed] [Google Scholar]
- 56.McEwen B S. N Engl J Med. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 57.Schmidt A M, Stern D. Circ Res. 2000;87:722–724. doi: 10.1161/01.res.87.9.722. [DOI] [PubMed] [Google Scholar]
- 58.Vazquez-Prado J, Medina L C, Romero-Avila M T, Gonzales-Espinosa C, Garcia-Sainz J A. J Biol Chem. 2000;275:6553–6559. doi: 10.1074/jbc.275.9.6553. [DOI] [PubMed] [Google Scholar]
- 59.Auphan N, DiDonato J A, Rosette C, Helmberg A, Karin M. Science. 1995;270:286–290. doi: 10.1126/science.270.5234.286. [DOI] [PubMed] [Google Scholar]
- 60.Farmer P, Pugin J. Am J Physiol. 2000;279:L675–L682. doi: 10.1152/ajplung.2000.279.4.L675. [DOI] [PubMed] [Google Scholar]
- 61.Aksoy M O, Bin W, Yang Y, Yun-You D, Kelsen S G. Am J Physiol. 2001;281:L1271–L1278. doi: 10.1152/ajplung.2001.281.5.L1271. [DOI] [PubMed] [Google Scholar]