Later this year, the US Food and Drug Administration (FDA; Rockville, MD, USA) plans to rewrite its regulations to eliminate any reference to the Declaration of Helsinki (DoH), a document from the World Medical Association (WMA; Ferney-le-Voltaire, France) that many consider to be the hallmark of medical ethics (WMA, 2004). This decision, triggered by the 2000 update to the DoH, is the latest move in an increasingly heated debate over medical research ethics. The FDA is reacting in particular to the addition of two controversial paragraphs, which, if adopted in their own regulations, would limit the use of placebos in drug trials and increase the responsibilities of trial sponsors towards research participants.
Unhappy with revisions made to the DoH between 2000 and 2004, the FDA now refers to the 1989 version of the Declaration, which the WMA itself considers invalid
Since 1975, the FDA, which decides what medicines are marketed in the USA and therefore influences similar decisions elsewhere, had cited the DoH in its rules for new drug applications from studies conducted outside the USA. Unhappy with revisions made to the DoH between 2000 and 2004, the FDA now refers to the 1989 version of the Declaration, which the WMA itself considers invalid. In the future, the FDA plans instead to refer to the Good Clinical Practice: Consolidated Guidance—a joint effort by drug approval agencies from Europe, the USA and Japan, and pharmaceutical trade organizations (ICH, 1996)—which honours the spirit, but not necessarily the wording, of the DoH. The European Commission (EC), which sets the pace on national drug laws and ethical standards in Europe, is also reluctant to adopt the latest version of the DoH and instead refers to the 1996 version in its 2001 clinical trials directive (EC, 2001) and its 2005 directive on good clinical practices (EC, 2005). Birka Lehmann, from the Pharmaceuticals Unit of the EC's Directorate General Enterprise and Industry, said that “no agreement could be reached in respect to an update of the reference to the Declaration of Helsinki in 2005.”
The changes to the DoH that have raised the ire of the FDA are limited to two paragraphs: 29, which states that “The benefits, risks, burdens and effectiveness of a new method should be tested against those of the best current prophylactic, diagnostic, and therapeutic methods. This does not exclude the use of placebo, or no treatment, in studies where no proven prophylactic, diagnostic or therapeutic method exists”; and 30, which states that “At the conclusion of the study, every patient entered into the study should be assured of access to the best proven prophylactic, diagnostic and therapeutic methods identified by the study” (WMA, 2004).
Critics were especially alarmed by paragraph 29, portraying it as an attack on the use of placebos, which would make it more difficult to assess the safety and efficacy of drug candidates. Robert Temple, Director of the Office of Medical Policy at the FDA's Center for Drug Evaluation and Research, said, “We didn't think the World Medical Association understood you really do need placebos to learn something in a lot of cases. Fundamentally, in a lot of symptomatic conditions, it's common for studies that compare a new drug with placebo to fail. If doing the right design, or doing an informative design would mean denying somebody a therapy that would really save their lives, then you just can't do the study at all. Everybody agrees on that. But if it's just a matter of symptoms, having a headache a little longer, being depressed for a few more days, I would say most people and certainly we believe that you could ask a person to participate in a study [using placebos]. But it's not unethical to do a trial like that.” Fearing that these obligations would make it harder to prove the efficacy of a new drug and would drive up the costs of development, drug developers, particularly in the USA, are protesting.
Not surprisingly, the unwillingness of the EC and the FDA to refer to the latest version of the DoH has met with criticism. John Williams, Director of the WMA's Ethics Unit, said, “As far as the WMA is concerned, the current [2004] version of the DoH is the only official one; all previous versions have been replaced and should not be used or cited except for historical purposes.” For Udo Schuklenk, head of the Centre for Ethics in Public Policy & Corporate Governance at Glasgow Caledonian University, UK, and co-editor of Bioethics and Developing World Bioethics, the situation reflects FDA policy. “[The US FDA] never liked the Declaration of Helsinki and worked overtime to get it changed,” he said. “When they failed, they simply decided to ignore it. [It] tells you more about the FDA mentality—do it our way or not at all—than it does about the DoH.”
Notwithstanding these ethical debates, the discrepancy in guidelines could cause dissonance for researchers…
The FDA feels that the WMA has overstepped its mandate with the revised DoH. “What I think has happened to some extent is that the Declaration has moved from a purely ethical document to a document that is increasingly interested in social justice,” said Temple. “For example, [the WMA] clearly are very upset that people in poor countries don't have really good medical care. And I'm upset by that too. But I don't think that determines the ethics of a trial.” Notwithstanding these ethical debates, the discrepancy in guidelines could cause dissonance for researchers, according to Sandy Thomas, Secretariat Director of the Nuffield Council on Bioethics in London, UK. “It's quite clear that some researchers feel perplexed by the disagreement between the guidances and clearly they're under a good deal of pressure to do the right thing. It's very difficult to find a way forward when faced with the contradictions,” she said.
The debate on ethical standards in clinical trials was triggered almost a decade ago by Peter Lurie, Deputy Director of the Public Citizen Health Research Group (HRG; Washington, DC, USA), and Sidney Wolfe, HRG's Director. Long thorns in the side of the FDA, they questioned the ethics of US government-funded research on HIV in developing countries. In an article in the New England Journal of Medicine, they contended that the National Institutes of Health (NIH; Bethesda, MD, USA) had acted unethically by sponsoring studies on the maternal transmission of HIV to newborns involving placebos when effective medication was available and used routinely in the USA (Lurie & Wolf, 1997).
Their article set off a global furore and led to the rewriting of all major ethical guidelines. Although part of the debate focused on the use of placebos, discussions were especially heated over the responsibility of clinical-trial sponsors and researchers to participants and the wider community in developing countries after the research is completed. One of the highest profile debates was at the WMA and led, in 2000, to the fifth revision of the DoH since it was first adopted in 1964.
Discontented with these changes, US interests dug in for a new Battle of Helsinki. Officials from the NIH and the FDA, enlisting colleagues from the developed and developing world, campaigned to marginalize the DoH in a series of articles published in medical, ethics and public health journals, contending that it had been rejected by most global ethics bodies and therefore represented a minority view on research ethics (Lie et al, 2004).
In a discussion paper on the revised DoH, the Pharmaceutical Research and Manufacturers of America (Washington, DC, USA), a trade association representing the country's research-based drug industry, warned that paragraph 30 could have the unintended consequence of establishing “unnecessary barriers to research and treatments for the developing world” and that promising care to study participants amounted to “undue inducement” (PhRMA, 2001). Regarding the limits on placebo use, the document stated “…from a scientific perspective, it is virtually impossible to identify the ‘best' treatments on the basis of a single study.”
Ironically, the current version of the DoH might be the closest to the Nuremburg Code—which established ethical standards for human research subjects after the trials of Nazi physicians (Anonymous, 1949)—that it has ever been, although it was originally adopted to liberalize these standards. “For the last 30 years, [US interests] said they loved the Declaration of Helsinki because it's not as strict as the Nuremburg Code, which says you can't experiment without consent, end of story,” explained George Annas, Chairman of the Health Law Department at Boston University's School of Public Health (Boston, MA, USA). “All of a sudden, Peter Lurie and other people effectively lobbied to make some changes to the DoH after the [AIDS] trials. And now the NIH says, ‘Helsinki? What is that? That doesn't mean anything.' [It's] just totally hypocritical on their part to follow the DoH as long as it says what they want it to say, and as soon as it's changed, say it doesn't mean anything.”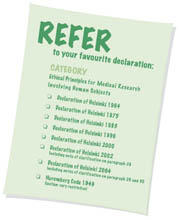
Although critics did not persuade the WMA to throw out paragraphs 29 and 30 completely, they did manage to convince them to add footnotes to the text in 2002 and 2004. The footnote for paragraph 29 states that “a placebo-controlled trial may be ethically acceptable, even if proven therapy is available” under some circumstances, while the footnote for paragraph 30 states that “it is necessary during the study planning process to identify post-trial access by study participants to prophylactic, diagnostic and therapeutic procedures identified as beneficial in the study or access to other appropriate care. Post-trial access arrangements or other care must be described in the study protocol so the ethical review committee may consider such arrangements during its review” (WMA, 2004).
“The footnotes are the result of a backlash by the people in power. Developing countries don't get to do this. Only the rich guys get footnotes. The footnotes muddied the meaning of the Declaration of Helsinki,” Lurie said. The drug industry has a different opinion, however. They are following the 2004 version, although still grumbling about paragraphs 29 and 30. Bruce Innis, Vice-President of Clinical Research and Development at GlaxoSmithKline (GSK; Uxbridge, UK), insists that GSK places a high priority on protecting research subjects. “In clinical trials to establish whether a product has a medical benefit, and whether it has an appropriate safety profile, the questions we struggle with are ‘Are we exploiting anyone? Are we adhering to the principles of autonomy and beneficence and justice that are supposed to undergird the research?' We try to establish trials where no one feels exploited.” He added that GSK “embraces” the amended DoH and has adopted a policy on conducting clinical trials in the developing world that follows both the principles of the DoH and the Good Clinical Practice guidelines (ICH, 1996).
Ironically, the current version of the DoH might be the closest to the Nuremburg Code…that it has ever been, although it was originally adopted to liberalize these standards
In the meantime, the efforts “to undermine the DoH have paid off”, according to Schuklenk. “There's a flurry of other documents on the market now, so one can pick and choose according to what suits one's, or one's sponsor's, needs.” The European Group on Ethics in Science and New Technologies (Brussels, Belgium), which advises the EC, might have gone the farthest, stating that research participants in developing countries should receive beneficial new drugs “even if this implies supplying the drug for a lifetime if necessary. Moreover, there should be an obligation that the clinical trial benefits the community that contributed to the development of the drug” (EGE, 2003).
…charities, governments and drug companies are cautious about being seen as providers of medicine rather than sponsors of medical research
The Council for International Organizations of Medical Sciences (CIOMS; Geneva, Switzerland) took the concept of responsibility beyond the research subject to the wider community, and recommended that every effort is made to ensure that “Any intervention or product developed, or knowledge generated, will be made reasonably available for the benefit of that population or community” (CIOMS, 2002). And the Nuffield Council on Bioethics notes that “Where research studies are on a large scale, the benefits of improved healthcare provided during the research may extend to the whole community, including those not directly involved in the research” (Nuffield Council on Bioethics, 2002).
Innis is uncomfortable with the responsibilities to the broader community. “Our first concern is to be sure we have a clear contract with each volunteer in the study,” he said. “This is a balanced discussion between potential volunteers being solicited and investigators who want to conduct the trial, the authorities who authorize the trial and the sponsors, whether they be academic institutions or private parties, developers and manufacturers. The community part is much more nebulous.”
Innis is not alone in his view. Thomas commented that charities, governments and drug companies are cautious about being seen as providers of medicine rather than sponsors of medical research. “The duration aspect is very worrisome since a successful therapy potentially lasts the course of a decade, a lifetime and so on,” she said. “I think the aspiration should be to try and encourage interventions to be provided, but to recognize that many research sponsors are simply not in the position to do that.” Similarly, Julius Ecuru, from the Uganda National Council for Science and Technology in Kampala (Uganda, Africa), commented that the DoH and CIOMS guidelines are important, “but I think they are overly stringent when it comes to the obligation of the sponsors to provide the best proven care and research product to the host communities during and after the research.-I could take that as a desirable standard, but not an absolute moral or ethical requirement without which research would not be allowed to proceed.”
However, Alexander Capron, Director of Ethics, Trade, Human Rights and Health Law at the World Health Organization (WHO; Geneva, Switzerland), said that an obligation to provide subjects with access to the best methods of care identified in studies in which they participate is widely accepted, although not clearly spelled out. “What that means—how much access, what price, and for how long—is still a matter of controversy.” He added that it is easier in theory than in practice to figure out what to do after a trial is over, in particular if the drug has not yet been approved. “[We] haven't resolved that in the ethics community, broadly. The WHO hasn't resolved it either, as a flat rule, because there will be cases where they'll just say ‘We can't pass out this drug. It's not licensed'.”
There is some informal talk about building a new consensus, but Schuklenk is pessimistic. “A consensus conference won't and can't happen. A mix of private organizations, such as the WMA, the Nuffield Council, government regulators or research organizations, don't go together. And if you added the NIH, why not medical research councils in the UK, South Africa or Germany, and so on? It would not really be feasible.”
In view of the lack of consensus and confusion over differing guidelines, Williams from the WMA commented that researchers and trial sponsors must not only follow their national laws and regulations, but also consider whether to go beyond these requirements. In any case, he said “it is probably not a good idea to enshrine the Declaration of Helsinki in national laws and regulations, for two reasons: it is an ethical document and as such incorporates higher standards of behaviour than laws and regulations might require; and it can and does change from time to time and it is unrealistic to expect that countries will change their laws and regulations every time the WMA changes the Declaration of Helsinki. I don't think this undermines it—the Declaration of Helsinki is still a beacon for the research community.”
References
- Anonymous (1949) Trials of War Criminals before the Nuremberg Military Tribunals under Control Council Law No. 10, Vol 2. Washington, DC, USA: Government Printing Office [Google Scholar]
- CIOMS (2002) International Ethical Guidelines for Biomedical Research Involving Human Subjects. Geneva, Switzerland: Council for International Organizations of Medical Sciences [PubMed] [Google Scholar]
- EC (2001) Directive 2001/20/EC of the European Parliament and of the Council of 4 April 2001 on the approximation of the laws, regulations and administrative provisions of the Member States relating to the implementation of good clinical practice in the conduct of clinical trials on medicinal products for human use. Brussels, Belgium: European Commission [PubMed]
- EC (2005) Commission Directive 2005/28/EC of 8 April 2005 laying down principles and detailed guidelines for good clinical practice as regards investigational medicinal products for human use, as well as the requirements for authorisation of the manufacturing or importation of such products. Brussels, Belgium: European Commission
- EGE (2003) Ethical Aspects of Clinical Research in Developing Countries. Brussels, Belgium: European Group on Ethics in Science and New Technologies [Google Scholar]
- ICH (1996) Guidance for Industry. E6 Good Clinical Practice: Consolidated Guidance. Geneva, Switzerland: International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use [Google Scholar]
- Lie RK, Emanuel E, Grady C, Wendler D (2004) The standard of care debate: the Declaration of Helsinki versus the international consensus opinion. J Med Ethics 30: 190–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie P, Wolf SM (1997) Unethical trials of interventions to reduce perinatal transmission of the human immunodeficiency virus in developing countries. N Engl J Med 337: 853–855 [DOI] [PubMed] [Google Scholar]
- Nuffield Council on Bioethics (2002) The Ethics of Research Related to Healthcare in Developing Countries. London, UK: Nuffield Council on Bioethics [Google Scholar]
- PhRMA (2001) PhRMA Discussion Paper on the Declaration of Helsinki as Revised in October 2000. Washington, DC, USA: Pharmaceutical Research and Manufacturers of America [Google Scholar]
- WMA (2004) World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. Ferney-le-Voltaire, France: World Medical Association [Google Scholar]


