Abstract
OBJECTIVE:
To assess the level of modification by local primary care doctors of key aspects of the National Asthma Education Program (NAEP) Guidelines for the Diagnosis and Management of Asthma.
DESIGN:
A random sample of primary care physicians participating in local asthma guideline development.
SETTING:
Two hospital systems, one based in an urban environment, and a second in a community and rural environment.
PARTICIPANTS:
Primary care physicians.
INTERVENTION:
Design of consensus-based local asthma guidelines using a modified Delphi approach.
MEASUREMENTS AND MAIN RESULTS:
A total of 42 physicians participated in the local guideline development. With few exceptions, the primary care physicians modified in major ways the NAEP Guidelines regarding the role of pulmonary function testing and spirometry. Specifically, the local guidelines did not require peak flow and spirometry measurements as the basis for initiating inhaled steroids as did the national guidelines. All 42 physicians emphasized a clinical diagnosis versus one based on a pulmonary function. Peak flow monitoring was recommended by 35 (83%) of physicians in selected patients only, in contrast to the national guidelines, which emphasized monitoring for all patients routinely and during exacerbations. There was strong agreement with the national guidelines on the role and importance of patient education, and on the indications for the use of inhaled steroids.
CONCLUSIONS:
Disagreement by primary care doctors with parts of the NAEP guideline is a potential cause for poor compliance and lack of influence on patient care. Recognizing the need to modify or customize guidelines through field testing with local primary care physicians will improve acceptance of national guidelines.
Keywords: asthma, guidelines
The National Asthma Education Program (NAEP) published Guidelines for the Diagnosis and Care of Asthma in 1991 as part of an effort to improve quality of care.1 Despite this work and major efforts in publicizing the guidelines, there is little evidence that they have influenced patient care. 2, 3 Why physicians are not following these or other guidelines is unclear. Guidelines for managing patients with chest pain, postmyocardial β-blocker use, cardiac arrest, and hypercholesterolemia have all had poor compliance rates. 4–7 Lack of compliance with the NAEP and other national guidelines have been attributed to incomplete dissemination, and to physicians’ negative attitudes toward guidelines. 8 There has been little attention to the possibility that local primary care physicians are aware of the existence and content of the guidelines and even have positive attitudes toward the guideline content, but that practice context may contribute to the lack of adherence with the national guideline.
We hypothesized that doctors with a primary care perspective might want to modify, on the basis of their practice experience, all or parts of the NAEP Guidelines. As part of a randomized controlled clinical trial designed to test the impact of asthma guidelines on patient health outcomes, 9 we examined the approach of primary care doctors to the care of asthma patients.
METHODS
Of 134 primary care physicians initially recruited for the study, 56 (42%) were associated with the New England Medical Center (NEMC) in Boston, Massachusetts, and 78 (58%) with Baystate Medical Center (BMC) in Springfield, Massachusetts. All 56 physicians at NEMC’s primary care medicine clinics, and all primary care physicians in neighboring areas associated with a single independent provider (IPA) network were included. At BMC, 168 (all associated family practice and general internal medicine physicians and those pediatricians who identified themselves as practicing adolescent medicine) were invited to participate, and 78 (46%) agreed to do so. Of the 134 primary care physicians, 68 were randomized to the experimental group. These physicians were invited to participate in dinner meetings at which local asthma guidelines were formulated.
Three meetings were held at each of the two study sites (BMC in October 1996 and NEMC in May 1996). Thirty-five (51%) of the 68 study doctors participated in a meeting, 14 at NEMC and 21 at BMC. Each meeting included a dinner and lasted approximately 90 minutes. At the outset of each meeting, each participating physician was given four algorithms taken from the Executive Summary of the 1991 Expert Panel Report: Guidelines for the Diagnosis and Management of Asthma. 1 These seed documents consisted of the algorithms for “Management of Asthma in Adults for Chronic Mild Asthma,”“Chronic Moderate Asthma,”“Chronic Severe Asthma,” and “Acute Exacerbations of Asthma in Adults, Home Treatment.” After the participants had reviewed the algorithms, one of the investigators (either SG or HAP) led them through a discussion using a modified Delphi technique. 10, 11 One of the meeting participants acted as a scribe, summarizing the conclusions the group reached on each topic. The discussions were structured to ensure discussions of at least each of the following topics: the role of pulmonary function testing, the role of peak flow meter (PFM) use, indications for inhaled corticosteroids, indications for specialty referral, initial treatment of exacerbations, and patient education.
After the six meetings, one of the investigators together with scribes generated a summary draft of the local guidelines based on the participants’ discussions in algorithm format patterned after the NAEP Guidelines. This summary draft was sent to all meeting participants. Following personal contact by telephone, the draft was also sent to the 33 physicians who did not attend a meeting. This draft presented the synthesized results of the meetings, and asked all physicians to comment on each section of the guideline. They were asked to respond to the question, “Would you modify the above?,” with answers ranging from “Not at all” to “Completely.” They were also asked to comment on what specific changes they would make. Unlike other more formal approaches, there was no attempt to gain consensus.12, 13 Our goal was to focus on those parts of the guidelines in which there was very general agreement or disagreement in order to forge a working document that the physicians would use for continuous quality improvement.
Data analysis was planned to measure level of agreement. Percentage of agreement was recorded as the proportion of doctors completing guideline drafts who agreed completely with the statements within each topic. In our analysis of the returned drafts, we assumed agreement with the local guideline on points differing from the national guideline to represent modification of the national guideline. Analysis of the local physicians’ written agreement with the local draft asthma guideline was planned for each of the six main topics. The number of physicians who agreed on each topic out of the 42 who completed evaluations of the local guideline was taken as an index of agreement with the local guideline.
RESULTS
Of 25 study doctors at NEMC, 14 attended one of the three meetings. Thirteen of these 14 completed reviews of the local guideline, while 2 of the study doctors who did not come to meetings completed a review of the guidelines, resulting in 15 who completed the required steps. Of the 41 physicians at BMC, 21 participated in a meeting. Fourteen of these 21 completed guideline evaluations, while 13 of the study physicians who did not come to meetings completed guideline reviews, for a total of 27 guideline evaluations at BMC, and 42 guideline reviews in total for the study. Over 80% of the BMC and all NEMC physicians were board certified.
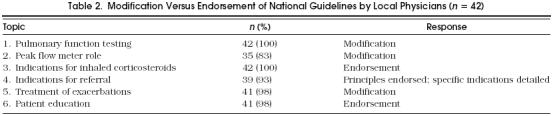
A summary of the local guideline draft components, and a comparison with the NAEP Guidelines is presented in Table 1. Table 2 shows the level of agreement with the guideline draft. With few exceptions, there were no differences between the NEMC and BMC guideline drafts; therefore the six groups were combined for this analysis.
Table 1.
Comparison of Local and National Asthma Guidelines on Decision Points
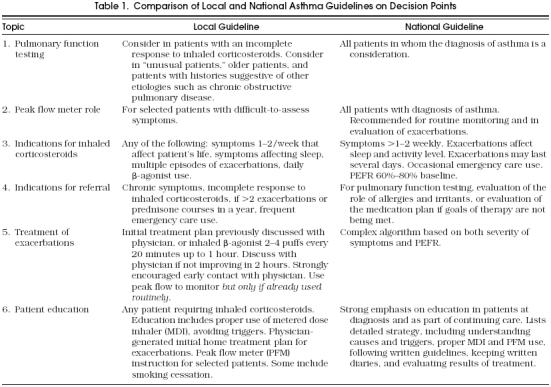
Table 2.
Modification Versus Endorsement of National Guidelines by Local Physicians (n = 42)
Pulmonary Function Testing
The NAEP Guideline recommends full pulmonary function tests (PFTs) in all patients in whom the diagnosis of asthma is entertained. The algorithm for the diagnosis requires definitive demonstration of obstruction for the diagnosis in all patients, including home peak expiratory flow rate (PEFR) monitoring for 2 to 4 weeks in patients with spirometry negative for obstruction, and bronchoprovocation in all patients in whom home PEFR monitoring results are negative as well.
The local guideline emphasizes a clinical diagnosis of asthma (for example, wheezing accompanied by response to inhaled β-agonist by physician examination or PFM in office), without requiring PFTs. The local guideline calls for PFTs only in patients with an incomplete response to inhaled corticosteroids, in “unusual” patients, or in patients in whom an alternative diagnosis is suspected clinically. All 42 physicians endorsed this modification (Table 2
Role for Peak Flow Meters
The NAEP Guideline recommends PFM use in all patients, regardless of severity, and includes PEFR criteria both for the assessment of severity and for monitoring response to therapy.
The local guideline recommends training for in-home PFM use only for “selected patients with difficult to assess symptoms.” There was 83% agreement (35/42) with the local guideline. Only seven physicians evaluating the local guideline felt that routine PEFR monitoring should be mandatory in all patients with moderate or severe asthma (Table 2).
Indications for Inhaled Corticosteroids
The NAEP and local guidelines list similar clinical criteria for the initiation of inhaled corticosteroids (see Table 1, topic 3). The notable difference between the guidelines is the NAEP Guideline’s criterion of PEFR impairment as part of the assessment for need for inhaled corticosteroids. There was 100% agreement (42/42) with the local guideline (Table 2).
Referral
Of the 42 physicians, 39 (93%) recommended referral to a pulmonary or allergy specialist based on either frequency of exacerbations, or incomplete response to therapy. The participants emphasized the value of flexibility in referral criteria; the three dissenters in this area during the protocol review wanted stronger wording emphasizing this flexibility. The NAEP Guideline does not list specific referral criteria.
Treatment of Exacerbations
This component turned out to be a complicated topic with multiple issues. The local guideline emphasized the importance of an individualized treatment plan for each patient, and early communication with the patient’s physician within 2 to 4 hours if no major improvement occurs.
In contrast, the NAEP Guideline provided a detailed algorithm for home management of an exacerbation, with three pathways of treatment and evaluation based on whether a patient partially responds or minimally responds with symptom allevation. An integral part of the evaluation of the response in this algorithm is PEFR monitoring. The local physicians felt strongly that the NAEP Guideline’s detailed home action plan was difficult for a patient in distress to follow, and could discourage the early contact with the patient’s physician that they felt was very important. They felt that the NAEP Guideline relies upon the patient to understand and follow too many detailed instructions in situations in which patients are likely to be uncomfortable, short of breath, and anxious. Forty-one of the 42 suggested major modification of the NAEP Guidelines (see Table 2).
Patient Education
Education was felt to be very important by the local primary care physicians. The less ambitious teaching goals (see Table 1, topic 6) in the local guideline represent the local physicians’ assessment of what was practical for them to achieve with limited or nonexistent ancillary teaching capability. However, 98% endorsed the NAEP Guideline goals for teaching.
DISCUSSION
The sample of primary care doctors in this study suggested major modifications of key parts of the NAEP Guidelines for the Diagnosis and Care of Asthma. The customization was not based on a difference in the interpretation of the evidence, for example, that the use of PEFR monitoring is useful in managing patients with asthma; rather, it was based on the supposition that parts of the guidelines do not appear to apply to the spectrum of disease seen in their practices. Other studies have shown that physicians who were well informed about the NAEP Guidelines and who were using medications in compliance with them (indicating that they did not have overall disregard for the NAEP Guidelines) had a low rate of ordering PFTs. 14, 15 They had an even lower rate of using PFTs in making treatment decisions, even in the acute setting. A survey of members of the American College of Emergency Physicians showed that 98% reported using β-adrenergic agents as first-line therapy in asthma exacerbations, 65% used nebulized agents every 20 to 30 minutes, 48% reported using corticosteroids as part of the initial treatment, and 69% reported always prescribing corticosteroids in patients being discharged from the emergency department—all in close agreement to the NAEP Guidelines recommendations. 14 In contrast, only 53% reported always getting pretreatment and posttreatment spirometry or PEFRs, despite 92% reporting access in their emergency departments to spirometry or PFMs.
A study of primary care practice in the care of patients with asthma found that, in 490 asthma-related patient visits, 68% of visits had neither current nor prior data on spirometry, 55% lacked PEFR data, and 46% had neither, in spite of availability of spirometry and PFMs at 72% of the practice sites. 15 These authors found that older patients had a slightly higher chance of ever having had spirometry or PEFR (odds ratio [OR] 1.04; 95% confidence interval [CI] 1.02, 1.06), while patients who visited the practice more than every 4 months were much more likely to have had either (OR 4.06; 95% CI 2.0, 8.1). While clearly demonstrating a lack of compliance with the NAEP Guidelines by emergency and primary care physicians, these studies did not address causes.
There are multiple reasons a primary care physician might not comply with a national guideline. First, a physician might simply be unaware of the guideline. The physicians in our study knew about the NAEP Guidelines; the local guidelines created in the study used algorithms of the NAEP Guidelines as the starting points. Second, a physician might have a negative attitude toward guidelines; our local guidelines showed substantial agreement with the NAEP Guidelines with respect to the importance of inhaled corticosteroids and the importance of patient education. Finally, a physician might agree with a guideline in general, but disagree with parts of it as they apply to the particular subsets of patients seen in their practices. This last reason for doctors not following guidelines raises an important question: Are there fundamental context issues in local clinical practice that are ignored by a national guideline, and importantly, the national guideline generation process itself ?
One of the context issues appearing to operate in this physician sample was a perceived difference in the spectrum of disease severity seen by primary care physicians rendering parts of the national guidelines inapplicable.16Another practice-based issue is that patients might not comply with certain monitoring or treatment regimens; many of the doctors in our study commented on the difficulty of getting patients with mild or moderate asthma to take their medications, much less maintain a PEFR diary. Patients often do not use a PFM correctly when wheezing or anxious, and the results can be misleading. It is also possible that aspects of a guideline are unavailable, too expensive for the patients to carry out, or impractical in some other way. Finally, a proportion of patients may have other major overwhelming diseases (such as cancer or severe heart disease) that make intense asthma monitoring less important.17
Review of the specific points of disagreement between the local and national asthma guidelines, the role of PFTs and PFMs, and parts of the algorithm for treating acute exacerbations shows them to be recommendations based generally on expert opinion, and not completely evidence-based. There is a growing awareness of the problem of grouping, without distinction, recommendations based on different levels of evidence, such as randomized controlled trial data and expert opinion, all under the rubric of a specialty-endorsed national guideline. A more evidence-based approach is thought to result in higher-quality guidelines.18Unfortunately, many of the issues addressed in a national asthma guideline do not have applicable data from randomized controlled trials, especially trials that focus on the kinds of patients seen in a primary care practice. These patients can be different from subspecialty referral populations in terms of compliance rates, comorbidity, and the spectrum of asthma severity.
Some national guidelines are addressing the issue of levels of evidence supporting given recommendations. A recent guideline on the management of idiopathic thrombocytopenic purpura clearly distinguished recommendations based on evidence from expert opinion, and quantified, in detail, the degree of agreement on recommendations based on expert opinion.19This approach implicitly acknowledges that there may be reasonable differences of opinion on aspects of a guideline. It gives guidance to those without specific experience and detailed reading in the area, while leaving others with expertise in the area leeway to follow their own experience and expertise.
The perceived need for “customization” by local primary care physicians of major parts of the NAEP is likely to be one of several reasons for its low impact on patient care. Several changes to the guidelines process could increase their influence. First, the components of the guidelines that are based on well-designed randomized controlled clinical trials and are generalizable to primary care practices should be clearly identified. Aspects that are derived from expert opinion should be identified, and reference made to any contrasting expert opinion, especially when that opinion takes into account the primary care perspective. Second, the format and content of the guideline should be constructed with the acknowledgment that the method by which a guideline is implemented, not to mention its potential impact, depends on multiple aspects of the local setting such as spectrum of disease, anticipated compliance, and physician experience with that disease in that particular community. Rather than ignoring the importance of local factors when trying to improve the care of patients with asthma, the guidelines should act as a road map for the actual process of local adaptation and implementation. Furthermore, primary care doctors should be included, not just in a token manner, in the national guideline process, to add insight into the important issues impacting actual clinical practice. Field testing of guidelines with qualified primary care physicians should be a routine component of national guideline development. Finally, some of the future randomized controlled trials of important therapies for asthma should be done in primary care settings, in order to make their results as readily applicable to this population of patients. Without these changes, it is possible that many important parts of the NAEP Guidelines will fail to disseminate, and never have the opportunity to achieve their potential for improving the care of asthma patients.
Acknowledgments
The authors appreciate the support and financial assistance of Joan Kross, MD, and the New England Medical Center–Tufts IPA, as well as the Shaw Fund at Baystate Medical Center. Dr. Picken was supported by AHCPR Training Grant (T32 HS 00060) to the Division of Clinical Care Research at New England Medical Center.
The authors acknowledge the helpful suggestions of Harry Selker, MD, and the assistance of Barbara Rooney for her editing and preparation of the manuscript.
References
- 1.National Heart, Lung, and Blood Institute. Bethesda, Md: U.S. Department of Health and Human Services: NIH publication; 1991. Executive Summary: Guidelines for the Diagnosis and Management of Asthma; pp. 91–3042. [Google Scholar]
- 2.Hartert TV, Windom HH, Peebles S, et al. Inadequate outpatient medical therapy for patients with asthma admitted to two urban hospitals. Am J Med. 1996;100:386–94. doi: 10.1016/s0002-9343(97)89513-7. [DOI] [PubMed] [Google Scholar]
- 3.Editors, editor. NIH asthma treatment guidelines not being utilized in patient care. W V Med J. 1993;89:292. [PubMed] [Google Scholar]
- 4.Lewis LM, Lasater LC, Ruoff BE. Failure of a chest pain clinical policy to modify physician evaluation and management. Ann Emerg Med. 1995;25:9–14. doi: 10.1016/s0196-0644(95)70348-9. [DOI] [PubMed] [Google Scholar]
- 5.Brand DA, Newcomer LN, Freiburger A, Tian H. Cardiologists’ practices compared with practice guidelines: use of beta-blockade after acute myocardial infarction. J Am Coll Cardiol. 1995;26:1432–6. doi: 10.1016/0735-1097(95)00362-2. [DOI] [PubMed] [Google Scholar]
- 6.Cline DM, Welch KJ, Cline LS, Brown CK. Physician compliance with advanced cardiac support guidelines. Ann Emer Med. 1995;25:52–7. doi: 10.1016/s0196-0644(95)70355-1. [DOI] [PubMed] [Google Scholar]
- 7.Browner WS, Baron RB, Solkowitx S, Adler LJ, Gullion DS. Physician management of hypercholesterolemia. A randomized trial of continuing medical education. West J Med. 1994;161:572–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Tunis S, Hayward RS, Wilson MC, et al. Internists’ attitudes about clinical practice guidelines. Ann Intern Med. 1994;120:956–64. doi: 10.7326/0003-4819-120-11-199406010-00008. [DOI] [PubMed] [Google Scholar]
- 9.Audet AM, Greenfield S, Field M. Medical practice guidelines: current activities and future directions. Ann Intern Med. 1990;113:709–14. doi: 10.7326/0003-4819-113-9-709. [DOI] [PubMed] [Google Scholar]
- 10.Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311:376–80. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fink A, Kosecoff J, Chassin M, Brook RH. Consensus methods: characteristics and guidelines for use. Am J Public Health. 1984;74:979–83. doi: 10.2105/ajph.74.9.979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chassin MR, Kosecoff J, Solomon DH, Brook RH. How coronary angiography is used: clinical determinants of appropriateness. JAMA. 1987;258:2543–7. [PubMed] [Google Scholar]
- 13.Leape LL, Hilborne LH, Park RE, et al. The appropriateness of use of coronary artery bypass graft surgery in New York State. JAMA. 1993;269:753–60. [PubMed] [Google Scholar]
- 14.Emerman CL, Cydulka RK, Skobeloff E. Survey of asthma practice among emergency physicians. Chest. 1996;109:708–12. doi: 10.1378/chest.109.3.708. [DOI] [PubMed] [Google Scholar]
- 15.Fried RA, Miller RS, Green LA, Sherrod P, Nutting PA. The use of objective measures of asthma severity in primary care: a report from ASPN. J Fam Pract. 1995;41:139–43. [PubMed] [Google Scholar]
- 16.Selker HP. Criteria for adoption on practice of medical practice guidelines. Am J Cardiol. 1993;71:339–41. doi: 10.1016/0002-9149(93)90802-j. [DOI] [PubMed] [Google Scholar]
- 17.Kravitz RL, Greenfield S, Rogers W, et al. Differences in the mix of patients among medical specialties and systems of care. JAMA. 1992;267:1617–23. [PubMed] [Google Scholar]
- 18.Woolf SH. Practice guidelines, a new reality in medicine, II: methods of developing guidelines. Arch Intern Med. 1992;152:946–52. [PubMed] [Google Scholar]
- 25.Diagnosis and treatment of idiopathic thrombocytopenic purpura: recommendations of the American Society of Hematology. The American Society of Hematology ITP Practice Guideline Panel. Ann Intern Med. 1997;126:319–26. doi: 10.7326/0003-4819-126-4-199702150-00010. [DOI] [PubMed] [Google Scholar]


