Abstract
OBJECTIVE
Develop a taxonomy for understanding and classifying goals in the care of persons with dementia.
DESIGN
Qualitative study using open-ended interviews with key informants and the constant comparative method of qualitative data analysis.
SETTING
The geriatric assessment center at a large academic medical center in Connecticut.
PARTICIPANTS
Key informant interviews with 36 subjects: consecutive patients receiving geriatric assessment at the center and their primary family caregivers, case managers, and physicians of patients.
MEASUREMENTS AND MAIN RESULTS
Goals, or desired outcomes, for the patient's care as described by patients, primary family caregivers, case managers, and physicians were the main measurements. Participant interviews were conducted until the point of theoretical saturation, i.e., until further interviews no longer provided new concepts. All participants articulated at least one goal. Specific goals were characterized by a limited number of goal attributes resulting in a taxonomy, or consistent classification system, for reported goals. These attributes include domain (or content), specificity, time frame, and level of challenge.
CONCLUSIONS
The findings suggested that patients, primary family caregivers, and clinicians can articulate goals of care and may bring differing perspectives to the goal-setting process. The research identified a taxonomy that may facilitate negotiation of goals by revealing important, and perhaps overlooked, aspects of goals and the goal-setting process.
Keywords: goals, health care preferences, taxonomy, classification, dementia
An effective clinician must know what she or he is trying to accomplish and would find it difficult to deliver appropriate health care without knowing the goals of care. Similarly, patients and their families may be unable to participate meaningfully in their own health care without understanding the goals of care. Goals are particularly important in the care of persons with dementia for several reasons. As in the care of patients with other chronic conditions, the predominant objective in the care of persons with dementia is adaptation to the condition rather than cure of the disease. Because the meaning of adaptation to dementia and related disability is multifaceted and subjective, goals of care may be less clear and less well articulated than for cases in which curing disease is an option. Further, because dementia deprives many patients of their cognitive ability to participate meaningfully in decision making, family members and clinicians often must develop plans of care without explicit knowledge of the patient's goals. The involvement of multiple caregivers adds complexity and the potential for conflicts in goals. Unless goals are made explicit, caregivers and clinicians may be unable to negotiate shared goals and lack the guidance of specific targets for their actions.
Previous work has demonstrated the theoretical importance of goals as pervasive organizing and motivating forces for human behavior,12–6 and practical work using the specific technique of goal attainment scaling has demonstrated the clinical relevance of goal setting.7––12 Several articles have discussed caregiving goals in the setting of dementia, from the perspective of family caregivers,13, 14 or nurses,15, 16 and one recent article emphasized the central importance of goal setting in the collaborative management of chronic illness.17 Nonetheless, there has been relatively little discussion of theoretical frameworks for describing and classifying goals in clinical medicine or in the specific setting of dementia. The aim of the current study was to examine goals in the care of persons with dementia, with attention to the varying perspectives of patients, caregivers, and clinicians, in order to develop a taxonomy that might help clinicians articulate and communicate goals and establish appropriate plans of care. The article presents the language in which people describe goals and identifies organizing characteristics or attributes of goals. The resulting taxonomy is a system for classifying goals into natural, related groups based on factors common to each.
METHODS
Design
This was a qualitative study using interviews with patients, primary caregivers, case managers, and physicians at the outpatient geriatric assessment center of a major teaching hospital. Given the lack of an existing framework for goals in relation to dementia, we approached the study using qualitative research techniques that rely on in-depth, open-ended interviews and rigorous qualitative analysis. Such techniques are particularly useful in exploring complex and previously unstudied phenomena for which traditional epidemiologic data are not readily obtainable. Patients and primary caregivers were interviewed after the assessment on the day of their initial visit to the center. Case managers and physicians were interviewed within 48 hours of the completed assessment.
Study Site
The study was a geriatric assessment center affiliated with Yale–New Haven Hospital in New Haven, Connecticut. The center evaluates approximately 50 new patients each month and receives referrals from a wide geographical area, although the majority come from New Haven and Fairfield counties. Currently, approximately 30% of new patients are referred by their physicians, 30% are referred by a community-based agency (such as a home care agency or an adult day care center) or other institution, and 40% come at the direct request of their families. The majority of assessments involve evaluation of cognitive impairment of varying degrees; therefore, the center was an appropriate site for the study of persons with dementia.
Participants
The participants were patients, family caregivers, case managers, and physicians at the assessment center. Consecutive patients presenting to the center for assessment of memory loss or cognitive impairment were enrolled in the study and interviewed. The primary family caregivers, case managers, and physicians for these patients were also enrolled in the study and interviewed. Thus, for every patient enrolled, four interviews (with patient, primary family caregiver, case manager, and clinician) were attempted. The study protocol was approved by the Human Investigation Committee of Yale School of Medicine, and written consent was obtained from the patient or primary caregiver prior to the interviews. In accordance with standard sampling techniques of qualitative methodology, interviews were conducted until no new concepts were elicited, i.e., until the point of theoretical saturation.18 Ten sets of participants (patient, primary family caregivers, case manager, and physician) were enrolled; two patients could not be interviewed owing to the severity of their cognitive impairment, one family caregiver refused interview, and one physician was unavailable for interview. Thus, 36 interviews were completed in total.
Data Collection
Data were collected using open-ended interviews, with two or three investigators present at the interview and subsequent analysis of interview data. The investigators had backgrounds in health services research, medicine, and public health. Interviews generally required 10 to 30 minutes to complete and were audiotaped and transcribed for accuracy. Patient data, including the Folstein Mini-Mental State score and other clinical and demographic information, were abstracted from outpatient medical records.
Interviews included several open-ended questions to elicit goals for each patient's health care. Because little is known about the language that patients, caregivers, and clinicians use to describe goals, a more structured interview might lead or constrain response, limiting the accuracy and depth of the inquiry. An interview guide consisting of three open-ended questions was used. Each interview began with the broad question, “What are your goals for the patient's (or your) care?” If participants appeared to have difficulty understanding the term “goal,” alternative terms were offered, such as, “desired outcomes … what you'd like to achieve.” In addition, participants were asked how such goals were formulated and about their optimism toward achieving the goals. Standardized probes were used to prompt the discussion of both global goals (such as maintenance of independence, enhanced safety, or reduced family burden) and more specific goals (such as homemaker assistance, assessment of driving skills, or use of adult day care). In all cases, participants were encouraged to expand their responses with examples and detailed stories that illustrated their statements. Data concerning body language, tone, and emotional responses were noted by the interviewers to enhance the direct quotations from the audiotape.
Data Analysis
Data were analyzed using the constant comparative method of qualitative data analysis.18 Consistent with qualitative research methodology, interviews were conducted without a priori themes or categories for classifying data. The investigators jointly reviewed each transcript line by line, coding comments and quotations with similar concepts into a list of distinct categories. During the process of coding, new interview data were constantly compared with previous quotations in the same category. Transcripts were reviewed several times to ensure all relevant data were accounted for and properly assembled under defined categories. As is standard in qualitative research, interviews were analyzed soon after each interview was completed and before completing all interviews. As new concepts were identified, probes regarding these concepts were added to future interviews until no new concepts emerged. As the coding and comparison processes continued, the full range of properties and the dimensions of each distinct conceptual category were identified. Categories and their properties were then integrated by the investigators through a series of group meetings to discuss the relation among various categories and their properties. The goal of this process was to reach consensus about how quotations were integrated, what each of the categories meant, and how they were interrelated. This consensual process provided the basis of the taxonomy of goals for persons with dementia.
RESULTS
Participant Characteristics
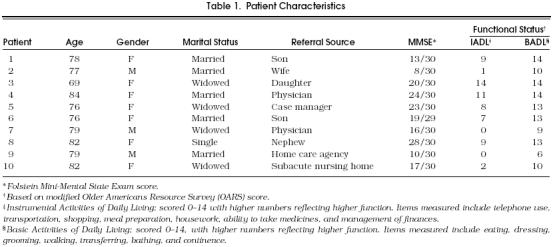
Of nine family interviews (one family caregiver having refused interview), three included two family members, and all nine included the primary family caregiver. The 10 case manager interviews were performed among three geriatric case managers, and the nine physician interviews (one physician having been unavailable for interview) were performed among six geriatric physicians. The clinician respondents included all medical staff at the study site and therefore reflect the scope of geriatric assessment at the study site. The 10 patients displayed a broad range of cognitive and functional status (Table 1).
Table 1.
Patient Characteristics
Taxonomy of Goals
Analysis of the interviews identified four basic axes in the taxonomy of goals (Table 2): goal domain, goal specificity, the time frame of the goal, and goal challenge. Each axis contains various categories; for the axis of goal domain, sample items are provided for the various categories.
Table 2.
Taxonomy of Patient-Centered Goals
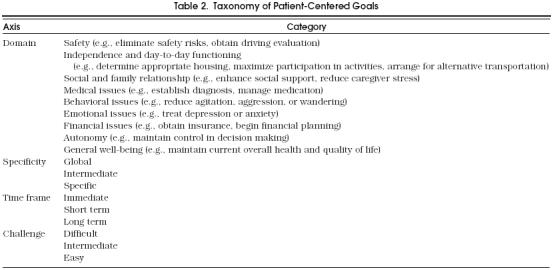
Goal Domain.
Interviews revealed that a limited number of domains broadly characterized goals. By domain, we mean a field or sphere of activity; in other words, domains describe the basic nature and content of the target condition or state. Domains of goals mentioned included safety; independence and day-to-day functioning; social and family relationships; diagnosis and management of medical, behavioral, or emotional issues; financial issues; autonomy; and general well-being. A striking finding was that every participant, including every patient, was able to articulate at least one goal, although in some cases the term “goal” required further definition. The articulated goals of different sets of participants clustered noticeably around a limited set of domains; however, given the qualitative nature of the study, we are unable to estimate the true prevalence of various goals for patients, family caregivers, case managers, or physicians.
The most common goal domain expressed by family members, mentioned by five families, was patient safety. Goals pertaining to patient safety arose from concerns related to either the patient's current living arrangement or ability to perform day-to-day activities fundamental to living independently, such as cooking, shopping, and driving. Referring to her mother-in-law and father-in-law, one daughter-in-law expressed her goals,
I would like to see them safely taken care of. I want someone to be sure they are safe. They are not eating right, not cooking … She couldn't follow a recipe if she had to. They cover for each other… I am just afraid they are going to get lost, but we haven't wanted to limit them, especially their mobility [referring to driving]. (Caregiver 1)
A second domain of goals involved social and family relationships. Goals of this type were mentioned in 9 of the 10 case manager interviews, but by only three physicians, one family member, and no patients. For instance, a case manager described the goals for a patient's care as follows
The goal was to help her [the wife] get some relief or support in relation to her great emotional distress of seeing this guy who she, I think, has had a mad love affair with for 50 years, and she is finding it … incredibly difficult to watch him change. (Case manager 9)
In contrast to the goal domain of safety often expressed by family members and the goal domains of social relationships and caregiver stress often expressed by case managers, physicians in this study typically expressed goals in terms of diagnosing medical or behavioral problems or both. As a representative example of these expressions, one physician stated,
The overall goals for her are to establish whether she has an isolated memory impairment or whether or not she has dementia, to further monitor her to confirm our initial impression that she does not have a depression, and to make sure she doesn't lose any more weight. (Physician 4)
Finally, five of the eight patients who were interviewed expressed the goal of remaining as they were, i.e., maintaining current general well-being. One patient, when asked about goals for her health, chuckled as if she had been asked a very silly question,
Are you kidding? What is there? I'm alive and kicking, and that's that. I would like to continue like this. (Patient 4)
Goal Specificity.
Goal specificity refers to the degree of detail with which goals are articulated. Data suggested there was a broad range of specificity, even after participants were asked to be as specific about goals as they could be. Responses varied from the most general statements of goals concerning overall well-being to extremely specific goals such as assessing whether adult day care services should be used. Exemplifying the most nonspecific goals, one patient said,
I just want God to keep John [the husband] and I [sic] together as long as possible. (Patient 1)
In contrast, more specificity was apparent in this statement from a clinician,
The grandnephews posed two questions, “Why was she [the patient] so confused?” And “What kind of services would she need in the present and perhaps in the future?” My goals were to answer those questions. (Physician 8)
Time Frame.
A third attribute of goals apparent from the data was the time frame of the goal. Expressed goals could be immediate, short term, or longer term. As an example of immediate goals, one case manager said,
The goal is to deal with his agitated, paranoid, combative behavior tout-de-suite. (Case manager 2)
In contrast, case managers and physicians often focused on longer-term planning; for example,
Our goal was to begin to help the daughter think about what was probably Alzheimer's disease and what's going to happen with her. We did not tell her to stop driving but raised that as an issue that would need to be monitored. (Case manager 3)
Goal Challenge.
A fourth attribute of goals was the perceived level of challenge related to the goal. Goals may be difficult or demanding to achieve, calling for special effort, or they may be easy to achieve; some goals may be unrealistically challenging. Among the informants, some were optimistic about accomplishing goals, while others were clearly pessimistic about accomplishing other goals. One woman expressed her uncertainty about the chances of meeting her goals for her mother-in-law's safety, particularly relating to driving a car, with a frustrated sigh, saying,
I don't know. Ultimately, it comes down to how well my husband can deal with it. (Caregiver 1)
The case manager for the same patient was “mildly optimistic,” again noting that success hinged on the son's cooperation. The physician was more positive about the chances of attaining the defined goal, saying,
Well, the driving will happen because we are going to make it happen by calling the DMV [Department of Motor Vehicles]. (Physician 1)
In another case, the case manager described recommendations to relieve caregiver stress, but then proceeded to indicate that the goals were too challenging,
She is quite extraordinarily reluctant to be relieved of that burden, as burdensome as it seems … She feels that she needs to be there. So that is clearly a rather complicated dance that the two of them do together, and I don't think that at this point in her life we are going to change that much short of his death, and then she might blossom. (Case manager 4)
DISCUSSION
This exploratory study revealed a defined set of attributes that classify goals. Among patients, family caregivers, case managers, and physicians, the attributes of goals described in Table 2 provide a classification system for goals that is organized as a taxonomy, with major axes (goal domain, specificity, time frame, and challenge) and categories (safety, behavior, etc.). All participants were able to articulate goals, suggesting that the concept was comprehensible and relevant to patients, family caregivers, and clinicians, even if the semantic term “goal” required further definition. Furthermore, the data suggested that the taxonomy might provide a useful structure and language for discussing and setting goals in clinical practice.
The research indicated that, although specific goals vary, they can be categorized broadly into goal domains. These goal domains span areas of functioning (including domains of safety, independence, and living arrangements), and psychosocial concerns (such as caregiver relationships, stress, and emotional health), as well as more traditional medical concerns such as diagnosis, medications, and behavior. Although the goal frequently reported by patients of stability appeared to represent a reasonable, positive goal for some, for others it may have reflected lack of insight resulting from the dementia, itself.
The other goal attributes identified in this study are consistent with factors described in other settings and shown to be predictive of goal attainment. For instance, previous research has demonstrated that there is a hierarchy of goals, ranging from global or general to highly specific,2 and that the setting of specific, measurable goals versus more general goals is associated with improved task performance.19 In this study, we found a tendency for patients and family caregivers to describe global goals and clinicians to state more specific goals. The establishment of goals that are specific and measurable may be a critical factor in promoting effective geriatric assessment. Our data suggest that patients and their families may need substantial assistance in formulating specific goals.
The time frame of goals was found to vary; within a single domain, goals could be immediate, short term, or longer term. In this study, an important facet of the geriatric assessment was redirecting patient and family caregiver time horizons, either to focus them on urgent, immediate goals or to articulate future goals. Longer-term planning was expressed more frequently by clinicians than by patients or their families. Although empirical work testing the effect of goal time frames on task performance is inconclusive,2, 20, 21 clinical judgment suggests that it can be an important determinant of goal achievement.
Yet another attribute of goals was the perceived lack of challenge represented by the goal. The objective degree of challenge posed by a particular goal may be closely linked to the perceived degree of challenge, although other factors, including self-efficacy and innate personality characteristics such as optimism, may also influence the perceived challenge. Previous literature has identified goal challenge as a key attribute determining performance toward goal attainment; goals that are challenging but realistic tend to encourage higher levels of performance than easy goals.2, 22
Multidisciplinary teams representing differing backgrounds and perspectives are the hallmark of geriatric assessment models. This research suggests that those differing perspectives persist even in the fundamental task of goal setting. An advantage of these differing perspectives is the consideration of both global and specific goals, as well as the discussion of goals across a variety of medical, social, and psychological domains. The interviews revealed that different participants often held different goals for care of the same patient. To the extent that these different goals simply reflect the different skills that people bring to a clinical setting, these differences may enhance care. If, however, the different people involved do not share goals for a particular patient, the disagreement could significantly impair the patient's care. Such conflict could be particularly damaging in a “team” setting involving the care of a patient who lacks decision-making capacity. The taxonomy reveals key goal attributes on which disagreement may arise; awareness of these attributes may help clinicians negotiate shared or complementary goals when necessary and appropriate to patient care.
As with most qualitative research, this study was conducted with a relatively small group of select participants at a single clinical site, limiting the generalizability of the results to other clinical (or nonclinical) settings or conditions. It is possible that research with other groups of patients, family caregivers, and clinicians would identify new goal attributes, or new goal domains. As an exploratory qualitative study, however, the research serves primarily to generate hypotheses regarding goals of clinical care. The current results have the strengths of being grounded in clinical experience, possessing strong face validity, and resonating with studies of goals and goal setting in nonclinical research.
We postulate that the goal attributes and taxonomy described here will be broadly applicable in other clinical settings involving dementia, and perhaps also for other clinical conditions. Clinicians might use these results to consider what their goals of care are, when and in what ways their goals are convergent or divergent with the goals of patients and families, whether or not aspects of divergence are problematic, and what they should discuss with patients and families in order to arrive at shared goals.
Acknowledgments
This research was supported by a grant from the Claude D. Pepper Older Americans Independence Center at the Yale School of Medicine.
The authors thank Terri Fried, MD, and Leo Cooney, MD, for reviewing earlier drafts; Grace Shih, Mike Jeong, MD, and Vasum Peiris for research assistance; and the staff of the Dorothy Adler Geriatric Assessment Center at Yale–New Haven Hospital for participating in the research.
References
- 1.Austin JT, Vancouver JB. Goal constructs in psychology: structure, process, and content. Psychol Bull. 1996;120:338–75. [Google Scholar]
- 2.Locke EA, Latham GP, editors. Englewood Cliffs NJ:: Prentice Hall;; 1990. A Theory of Goal Setting and Task Performance. [Google Scholar]
- 3.Arvey RD, Dewhirst HD, Brown EM. A longitudinal study of the impact of changes in goal setting on employees satisfaction. Personal Psychol. 1978;31:595–608. [Google Scholar]
- 4.French WL, Bell CH. Englewood Cliffs: NJ: Prentice Hall;; 1984. Organization Development: Behavioral Science Interventions for Organization Improvement. [Google Scholar]
- 5.Gould D. Goal setting for peak performance. In: Williams J, editor. Applied Sport Psychology: Personal Growth to Peak Performance. Palo Alto, Calif:: Mayfield;; 1986. In: ed. [Google Scholar]
- 6.Lee TW, Locke EA, Latham GP. Goal setting theory and job performance. In: Pervin L, editor. Goal Concepts in Personality and Social Psychology. Hillsdale, NJ:: L Erlbaum;; 1989. In: ed. [Google Scholar]
- 7.Kiresuk TJ, Sherman RE. Goal attainment scaling: a general method of evaluating comprehensive mental health programs. Community Ment Health J. 1968;4:443–53. doi: 10.1007/BF01530764. [DOI] [PubMed] [Google Scholar]
- 8.Palisano RJ, Haley SM, Brown DA. Goal attainment scaling as a measure of change in infants with motor delay. Phys Ther. 1992;72:432–7. doi: 10.1093/ptj/72.6.432. [DOI] [PubMed] [Google Scholar]
- 9.Palisano RJ. Validity of goal attainment scaling in infants with motor delays. Phys Ther. 1993;73:651–60. doi: 10.1093/ptj/73.10.651. [DOI] [PubMed] [Google Scholar]
- 10.Greenville J, Lyne P. Patient centered evaluation and rehabilitation care. J Adv Nurs. 1995;22:965–72. doi: 10.1111/j.1365-2648.1995.tb02649.x. [DOI] [PubMed] [Google Scholar]
- 11.Stolee P, Rockwood K, Fox RA, Steiner DL. The use of goal attainment scaling in a geriatric care setting. J Am Geriatr Soc. 1992;40:574–8. doi: 10.1111/j.1532-5415.1992.tb02105.x. [DOI] [PubMed] [Google Scholar]
- 12.Rockwood K, Stolee P, Fox RA. Use of goal attainment scaling in measuring clinically important change in the frail elderly. J Clin Epidemiol. 1993;46:1113–8. doi: 10.1016/0895-4356(93)90110-m. [DOI] [PubMed] [Google Scholar]
- 13.England M. Content domain for care giver planning identified by adult offspring care givers. Image J Nurs Sch. 1996;28(1):17–22. doi: 10.1111/j.1547-5069.1996.tb01172.x. [DOI] [PubMed] [Google Scholar]
- 14.Gignac MAM, Gottlieb BH. Care givers' appraisals of efficacy in coping with dementia. Psychol Aging. 1996;11(2):214–25. doi: 10.1037//0882-7974.11.2.214. [DOI] [PubMed] [Google Scholar]
- 15.Ugarriza DN, Gray T. Alzheimer's disease: nursing interventions for clients and caretakers. J Psychosoc Nurs. 1993;31(10):7–10. doi: 10.3928/0279-3695-19931001-05. [DOI] [PubMed] [Google Scholar]
- 16.Ryden MB, Feldt KS. Goal-directed care: caring for aggressive nursing home residents with dementia. J Gerontol Nurs. 1992;18(1):35–41. doi: 10.3928/0098-9134-19921101-08. [DOI] [PubMed] [Google Scholar]
- 17.Von Korff M, Gruman J, Schaefer J. Collaborative management of chronic illness. Ann Intern Med. 1997;127:1097–102. doi: 10.7326/0003-4819-127-12-199712150-00008. et al. [DOI] [PubMed] [Google Scholar]
- 18.Glaser BG. Strategies for Qualitative Research. New York, NY:: Aldine de Gruyter;; 1967. Strauss AL. The discovery of Grounded Theory: [Google Scholar]
- 19.Locke EA, Chah DC, Harrison S, Lustgarten N. Separating the effects of goal specificity from goal level. Org Behav Hum Decis Processes. 1989;42:270–87. [Google Scholar]
- 20.Kirschenbaum DS. Proximity and specificity of planning: a position paper. Cognitive Ther Res. 1985;9:489–506. [Google Scholar]
- 21.Bandura A, Simon KM. The role of proximal intentions in self regulation of refractory behavior. Cognitive Ther Res. 1977;1:177–93. [Google Scholar]
- 22.Erez M, Zidon I. Effect of goal acceptance on the relationship of goal difficulty to performance. J Appl Psychol. 1984;69:69–79. [Google Scholar]


