Abstract
This paper provides an overview of five key bodies of evidence identifying: 1) Characteristics of depression among older adults - its prevalence, risk factors and illness course, and impact on functional status, mortality, use of health services, and health care costs; 2) Effective Interventions, including pharmacologic, psychotherapies, care management, and combined intervention models; 3) Known Barriers to depression care including patient, provider and service system barriers; 4) Effective Organizational and Educational Strategies to Reduce Barriers to depression care; and 5) Key Factors in Translating Research into Practice. There is strong empirical support for implementing strategies to improve depression care for older adults.
Keywords: Major depression, elderly, evidence-based practice, primary care, home health care, barriers to depression care, collaborative depression care
Introduction
Clinical depression is prevalent among older adults and negatively affects functional status, quality of life and mortality, while increasing health care costs and taking a toll on family caregivers. Unfortunately, despite the availability of effective treatments for depressed elders, the majority remain untreated or undertreated – attributable to well-documented patient, health provider, service system, and social-structural barriers to ensuring that optimal care and services are accessible to elders (Charney, Reynolds, Lewis, Lebowitz, Sunderland, Alexopoulos, et al., 2003; Unützer, 2002).
Defining evidence-based practice solely as “evidence-based treatment” fails to adequately address known barriers to depression care. A more useful and comprehensive definition “empirically supported practice” includes evidence on: patient care seeking and adherence behavior; provider knowledge, clinical decision making and care management skills; health care system design or redesign; and organizational incentives and resources that lead to the implementation of evidence based practice and program guidelines, and empirically derived quality monitoring indicators. This paper provides an overview of five key bodies of evidence identifying: 1) Characteristics of depression among older adults - its prevalence, risk factors and illness course, and impact on functional status, mortality, use of health services, and health care costs; 2) Effective Interventions, including pharmacologic, psychotherapies, care management, and combined intervention models; 3) Known Barriers to depression care including patient, provider and service system barriers; 4) Effective Organizational and Educational Strategies to Reduce Barriers to depression care; and 5) Key Factors in Translating Research into Practice.
Characteristics of Late-life Depression
In community-dwelling older adults, the prevalence of major depression is estimated to be 1%–4% (Mojtabai & Olfson, 2004; Steffens, Skoog, Norton, Hart, Tschanz, Plassman, et al., 2000) and of subsyndromal depression 15 to 30% (Beekman, Deeg, Braam, Smit & VanTilburg, 1997; Lavretsky & Kunar, 2002; Lebowitz, Pearson, Schneider, Reynolds, Alexopoulos, Bruce, et al., 1997; Montgomery, et al., 2000). The latter include elderly with depressive syndromes such as dysthymia, bereavement, adjustment disorder with depressed mood and minor depression along a spectrum of illness severity that results in significant functional morbidity (Flint, 2002; Lyness, 2004; Unützer, 2002). Prevalence of major or clinically significant depression among medically ill elderly ranges from 10 to 43% (Charney, et al., 2003). Depression is the most common late life mental disorder to present in community based primary care. About 1 in 10 primary care patients has major depression, with increasing depression prevalence in home health care (10–26%) (Bruce, et al., 1998; Banerjee & McDonald, 1996; Ell, et al., 2004; Ell & Enguidanos, 2004), and nursing homes (12–30%) (Hendrie, Callahan, Levitt, Hui, Musick, Austrom, et al., 1995; Jongenelis, Pot, Eises, Beekman, Kluiter & Ribbe, 2004; Unützer, Patrick, Simon, Grembowski, Walker, Rutter, et al., 1997). Rates of depression in older adults are higher among women (Blazer, Burchett, Service & George, 1991). Prevalence rates are similar between African-American and White elderly (Bazargan & Hamm-Baugh, 1995), and may be higher among less acculturated Hispanics (González, Haan & Hinton, 2001).
Among the elderly, physical illness and disability are major risk factors for depression (Jorm, 1998; Koenig, et al., 1998; Roberts et al, 1997) as are cognitive deficits, declining functional status, social network losses and low social support, and negative life events (Bruce, 2002; Devanand, Kim, Paykina & Sackeim, 2002; Krasij, Arensman, Spinhover, 2002; Mojtabai & Olfson, 2004; Pennix, Guralnik, Ferrucci, Simonsick, Deeg, D., & Wallace, 1998; Ranga, George, Peiper, Jiang, Arias, Look, et al, 1998; West et al, 1998). Comorbidity of depression with other medical diseases in the elderly is common (Ranga, Krishnan, Delong, Kraemer, Carney, Spiegel et al., 2002) and medical illness increases the risk of suicide in the elderly (Juurlink, Hermann, Szalai, Kopp & Redelmeier, 2004; Suominen, Henriksson, Isometsa, Conwell, Heila & Lonnqvist, 2003).
Higher rates of disability, impaired quality of life and mortality are found among depressed elders (Alexopoulos, Vrontou, Kakuma, Meyers, Young, Klausner & Clarkin, 1996; Cronin-Stubbs, deLeon, Beckett, Field, Glynn & Evans, 2000; Black, Markides & Ray, 2003; Doraiswamy, Khan, Donahue & Richard, 2002; deJonge, Ormel, Slaets, Gertrudis, Kempen, Ranchor, et al., 2004; Lavretsky, Bastani, Gould, Huang, Llorente Maxwell, et al., 2002; Stein & Barrett-Connor, 2002; Pulska, Pahkala, Laippala & Kivela, 1998; Unützer, Patrick, Marmon, Simon & Katon, 2002). The likely multiple pathways that underly the effect of depression on mortality are only beginning to be understood (Alexopoulos & Chester, 1992; Covinsky, Fortinsky, Palmer, Kresevic & Landefeld, 1997; Ariyo, Haan, Tangen, Rutledge, Cushman, Dobs, et al., 2002; Katz, 1996; Mehta, Yaffe, Langa, Sands, Whooley, & Covinsky, 2003; Schulz, Drayer & Rollman, 2002).
For many elderly patients, major depression has a chronic course - persistent, intermittent, and/or recurrent (Beekman, et al., 2002; Cole, 1999; Lyness, Caine, King, Conwell, Duberstein, Cox, 2002; Raue, et al., 2003; Mueller, et al., 2004; Unutzer et al, 1997; 1999). Recent studies of treatment response and illness course among elderly patients find that clinical factors such as history, duration, and severity of depression, comorbid physical illness and disability, and antidepressant treatment as well as psychosocial factors, such as basic and instrumental social support predict depression treatment response, illness course, functional decline and even mortality (Bosworth, McQuoid, George & Steffens, 2002; Hays, Steffens, Flint, Bosworth & George, 2001; Geerlings, Beekman, Deeg, Twisk & Vantilburg, 2002). In the medically ill, improvement or lack of improvement in depression and disability following hospitalization are frequently closed related (Koenig & George, 1998). Depression recovery may be slower in the elderly (Thomas, Mulsant, Solano, Black, Bensai, Flynn, et al., 2002).
Late onset, unipolar depression is particularly characteristic of elderly suicides (Conwell et al, 1996, Dennis & Lindesay, 1995; Henriksson, Marttunen, Isometsä, Heikkinen, Aro, Kuoppasalmi, et al, 1995). For the most part, older suicide victims have had late onset undetected or untreated depressions, although typically they have had contact with their primary care provider prior to their death (Suominen, et al., 2004). And depression may influence end-of-life decision-making as in the case of depressed elderly found to initially decline cardiopulmonary resuscitation, but accept it after recovery from depression (Eggar, Spencer, Anderson & Hiller, 2002).
Not surprising, given its prevalence in medically ill elderly, depression is also associated with increased health service use (Beekman, Deeg, Braam, Smit, & VanTilburg, 1997; Koenig & Kutchibhatla, 1999) and medical costs (Katon, Lin, Russo & Unützer, 2003). Gender differences in depression, service utilization and treatment cost among Medicare elderly raise important questions. In a 5% random sample of 35,673 Medicare beneficiaries, females had a significantly higher incidence of major and other depression and higher outpatient and mental health care costs; whereas total health care costs were higher for men (Burns, Cain, Husaini, 2001). And depression in medically ill elders can result in increased burden on family caregivers (Langa, Valenstein, Fendrick, Kabeto, & Vijan Langa, 2004; Sewitch, McCusker, Dendukuri & Yaffe, 2004).
In summary, the evidence on characteristics of late-life depression supports the need to address depression in the elderly. Routine patient education, screening, and evaluation in older adults with known risk factors are particularly recommended. For example, efforts to improve treatment of depression in primary care have led to lowered suicide rates (Rutz, von Knorring & Wålinder, 1989; Rihmer, Rutz, & Pihlgren, 1995), resulting in recommendations that late-life suicide prevention focus on adequate recognition and treatment of depression (Conwell & Duberstein, 1995; Lish, Zimmerman, Farber, Lush, Kuzma, M.A., & Plescia, 1996; Rihmer, 1996).
Effective Pharmacological and Psychotherapeutic Treatment in the Elderly
Pharmacologic Treatment
Treatment studies document the safety and efficacy of anti-depressant treatment among older adults (Bump, Mulsant, Pollock, Mazumdar, Begley, Dew & Reynolds, 2001; das Gupta, 1998; Salzman, Wong & Wright, 2002), with SSRI’s being generally less toxic than older medications (Charney, et al., 2003; Sheikh, Cassidy, Doraiswamy, Salomon, Hornig, Holland, Mandel, Clary & Burt, et al., 2004). Between 60–80% of patients will respond to medications if prescribed according to recommended guidelines, although full therapeutic benefit may take 8–12 weeks and only about half of patients respond to the first medication prescribed (Sable, Dunn & Zisook, 2002). Response time may be longer among suicidal, more severely depressed and patients with comorbid anxiety (Szanto, Mulsant, Houck, Dew & Reynolds, 2003; Whyte, Dew, Gildengers, Lenze, Bharucha, Mulsant, et al., 2004). Therapy should be continued for at least 6 months, while patients at risk for relapse frequently require therapy for up to 2 years or indefinitely (Sable, et al., 2002). There is some evidence that antidepressants are effective for frail elders, for patients with dysthymia and more severely impaired elders with minor depression (Strein, et al., 2000; Williams, Barrett, Oxman, Frank, Katon, Sullivan, et al., 2000). However, questions remain about the effectiveness of antidepressants for the older adults because few trials have been conducted in the elderly, only a relatively small number of studies address elderly with comorbid conditions, and there is evidence of a significant placebo response rate and a significant number of elders who do not respond or have residual depressive symptoms (Taylor & Doraiswany, 2004).
To reduce inappropriate medication prescribing (Goulding, 2004), pharmacologic guidelines are available to assist primary care physicians in medication management (Dunner, 2003; Serby & You, 2003), however, patients with comorbid illness and accompanying complications and drug-drug interactions may require adapting general guidelines (Sable, et al., 2002). For example, for older adults with pain symptoms, combining antidepressant and pain pharmacotherapy may be indicated (Rao & Cohen, 2004; Unützer, Ferrell, Lin & Marmon, 2004). Poor patient adherence, as well as social factors can negatively affect treatment response (Sable, et al., 2002). To address adherence and social problems that negatively affect treatment response, patient education and sometimes brief counseling is required (Sable, et al., 2002).
Structured Psychosocial Therapies
There is growing consensus that structured psychotherapy, alone or combined with antidepressant treatment, is effective for older adults with depression. (Areán, et al., 2001; Areán & Cook, 2002; Areán, et al.; 1993; Gum & Areán, 2004; Leibowitz, et al, 1997; Unützer et al, 1999). Under some circumstances it is the treatment of choice (i.e., when preferred by individual patients, when pharmacologic treatments are contraindicated, and for elders coping with low social support or environmental stressors), or for maintenance after discontinuation of antidepressant medication (Reynolds, et al., 1999). Clinical benefits from psychotherapy should be evident within 6–8 weeks and are frequently maintained among the elderly for up to a year. Medications should be considered for patients who fail to improve by that time and for those who do not have a full remission after 12 weeks of psychotherapy. Structured psychosocial therapies are as effective as antidepressants for moderate depression and may be more effective in reducing recurrence.
Manualized cognitive behavioral therapies have been shown to be effective in depressed older adults, including elders with comorbid physical illness and disability, cognitive impairment, or comorbid anxiety (Areán & Cook, 2002; Kunik, Braun, Stanley, Wristers, Molinari, Stoebner, et al., 2001; Lenze, 2003; Thompson, Coon, Gallagher-Thompson, Sommer & Koin, 2001). Cognitive-Behavioral Therapy (CBT) challenges pessimistic or self-critical thoughts, emphasizing rewarding activities and decreasing behavior that reinforces depression. Alternative modes of delivery of CBT have been explored, including group CBT and telephone or computer self-help formats (Proudfoot, Goldberg, Mann, Everitt, Marks & Gray, 2003). Problem-Solving Treatment (PST) teaches patients to address current life problems by identifying smaller elements of larger problems and specific steps toward solving these. PST, adapted for primary care (PST-PC) in the multisite IMPACT study (Haverkamp, Areán, Hegel & Unützer, 2003; Kindy, 2003) was found to significantly reduce depressive symptoms among older primary care patients with major depression or dysthymia, including among African-American and Hispanic patients (Unützer, et al., 2002) and among elders with major depression and executive dysfunction (Alexopoulos, Raire & Areán, 2003). PST has also been adapted for older adult home care patients in an ongoing study (Ell & Enguidanos, 2004) and for low-income Latinos with cancer (Dwight-Johnson, Ell & Lee, in press). CBT has been adapted for elderly Chinese Americans (Dai, Zhang, Yamamoto, Ao, Belin, Cheung, et al., 1999).
Interpersonal Therapy (IPT) combines elements of psychodynamic-oriented and cognitive therapies to address interpersonal difficulties, role transitions, and unresolved grief. The majority of studies with older adults have combined IPT with medication or pill-placebo (Areán & Cook, 2002). Combining IPT with antidepressant medication is effective in reducing symptoms in older adults, may prevent relapse and is effective as a maintenance treatment for more severely depressed older adults (Miller, Cornes, Frank, Ehrenpreis, Silberman, Schlernitzaues, et al., 2001; Miller, Frank, Cornes, Houck & Reynolds, 2003; Reynolds, Dew, Frank, Begley, Miller, Cornes, et al, 1998; Reynolds, Frank, Perel, Imber, Cornes, Miller, et al., 1999; Taylor, Reynolds, Cornes, Miller, Stack, Begley, et al., 1999; Scocco & Frank, 2002).
Barriers to Depression Care for the Elderly
Undetected and Inadequately Treated
Although recent evidence indicates that antidepressant use is increasing among Medicare patients (Crystal, Sambamoorthi, Walkup & Akincigil, 2003; Sambamoorthi, Olfson, Walkup & Crystal, 2003), the majority of depressed elderly do not receive antidepressant treatment (Charney, et al., 2003; Luber, Meyers & Williams-Russo, Hollenberg, DiDomenico, Charlson, Alexopoulos, 2001; Unützer, et al., 2000). Few depressed older medical patients receive antidepressants in the hospital and even fewer are treated after discharge (Engberg, Sereika, Weber, Engberg, McDowell & Reynolds, 2001; Koenig, et al, 1997) or in home health care (Bruce, McAvay, Raue, Brown, Meyers, Keohane, et al., 2002). Older suicide victims have had late onset depressions that are not detected or treated, although typically they have had contact with their primary care provider prior to their death (Pfaff & Almeida, 2004). Elderly persons are also less likely to receive an adequate course of psychotherapy compared to younger adults (Harman, Edlund & Fortney, 2004). Older men, patients who prefer counseling or psychotherapy, and racial/ethnic minority elders are less likely to receive any depression care (Brown, et al., 1995; Green-Hennessy & Hennessy, 1999; Areán & Unützer, 2003; Sclar, Robinson, Skaer, et al., 1999; Unützer, Katon, Callahan, Williams, Hunkeler, Harpole, et al., 2003; Virnig, Huang, Lurie, Musgrave, McBean & Dowd, 2004). Poor elderly with Medicaid are also disadvantaged (Crystal, et al., 2003; Melfi, Crogan & Hanna, 1999 Melfi, Crogan & Hanna, 2000). Efforts to increase access to care and to improve the quality of depression care for older adults will need to address important patient, provider, and health system barriers to care (See Figure 1.).
Figure 1.
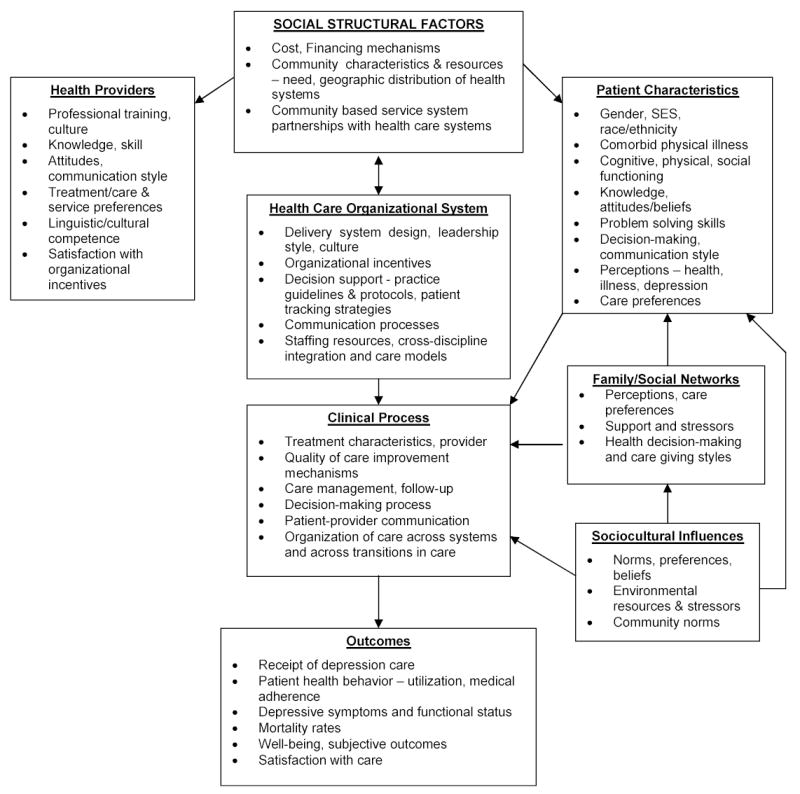
Evidence-based Barriers to Depression Care for Older Adults
Patient Barriers
Patient barriers to depression care influence detection and treatment processes. For example, older patients are less likely to voluntarily report depressive symptoms, may view depression as a moral weakness or character flaw, not an illness, and may be more likely to ascribe symptoms of depression to a physical illness (Heithoff, 1995; Knauper & Wittchen, 1994; Lyness, Cox, Curry, Conwell, King & Caine, 1995). Perceived stigma of depression has been associated with treatment discontinuation among older patients and treatment non-adherence (Sirey, Bruce, Alexopoulos, Perlick, Friedman & Meyers., 2001; Sirey, Bruce, Alexopoulos, Perlick, Raue, Friedman, et al., 2001). Nonadherence to treatment among the elderly is common (Maidment, Livingston & Katona, 2002; Salzman, 1995; Wetherell & Unützer, 2003), perhaps due in part to elders doubts that medication is helpful (Prabhakaran & Butler, 2002). Depressed older adults are less likely to use specialty mental health care, preferring to use the general health care system (Bartels, Coakley, Zubritsky, Ware, Miles, Areán, et al., 2004) and may be reluctant to attend group psychotherapy, but more willing to attend psychoeducational therapy formats (Areán, Alvidrez, Barrera, Robinson & Hicks, 2002).
Culturally based preferences for depression care can become a barrier to care if the preferred mode of care is not available (Cooper-Patrick, et al, 1997). Personal culturally based explanations for depression symptoms may influence symptom expression and patient-provider communication (Gallo et al, 1998; Lin et al, 1995; Marwaha & Livingston, 2002; Melfi et al, 1999; Mills, Alea & Cheong, 2004). Patient perceptions of bias and cultural competence in health care, family perceptions, and practical barriers such as cost and transportation to therapy may impede receipt of care (Johnson, Saha, Arbelaez, Beach & Cooper, 2004).
Provider Barriers
The majority of older adults receive antidepressants from primary care physicians (Harman, Crystal, Walkup & Olfson, 2003). Physician attitudes and experiences may affect depression treatment more than knowledge (Areán, Alvidrez, Feldman, Tong & Shermer, 2003;Poutanen, 1996; Williams, Rost, Dietrich, Ciotti, Zyzanski & Cornell, 1999). Physicians may miss depression because they assume it is a "natural" consequence of aging and associated physical illness, or fail to initiate treatment due to doubts about the efficacy of treatment (Alvidrez & Areán, 2002). Primary care physicians may be more likely to detect depression in older women compared to men, because they are more likely to report affective symptoms and crying spells (Allen-Burge et al, 1994; Brown, et. al., 1995).
Not surprising, physical problems compete with depression for physician attention, thus potentially decreasing the odds that the elderly will receive guideline level pharmacological or psychotherapy treatment (Bartels, Dums, Oxman, Schneider, Areán, Alexopoulos, & Jeste, 2002; Moser, 2002). For example, elderly hospitalized patients who remained depressed and physically disabled following hospitalization do not see mental health specialists any more frequently than elderly without depression or physical impairment (Koenig & Kuchibhatla, 1999). Physicians may fail to distinguish severity levels of depression or depression from social problems. As a result, they may inadequately manage depression, emphasize possible organic pathology, fail to elicit mood or cognitive symptoms, underestimate symptoms in the most severely depressed, including patients at risk of suicide (Fischer, Wei, Solberg, Rush & Heinrich, 2003; Volkers, Nuyen, Verhaak & Schellevis, 2004), and may be less willing to treat suicidal ideation (Uncapher & Areán, 2000). Physicians also report that guidelines are insufficiently flexible for the variety of patients seen in primary care (Smith, Walker & Gilhooly, 2004).
Recent studies find that home health care nurses may also fail to identify late-life depression (Bruce et al., 2002; Bruno & Ahrens, 2003; Raue, Brown & Bruce, 2002; Brown, McAvay, Raue, Moses & Bruce, 2003; Brown, Bruce, McAvay, Raue & Lachs et al., 2004). Sole reliance on home care nurse clinical judgment is reported to be inadequate when compared to the use of structured screening tools (Ell, et al., 2004; Preville, Cote, Boyer, & Hebert, 2004). Nurses may lack specific training in depression and may be uncomfortable with assessing depression (Larson, Chernoff & Sweet-Holp, 2004; McDonald, Passik, Dugan, Rosenfeld & Theobald et al., 1999; Williams & Payne, 2003). Lack of educational support and ease of access to mental health specialists are found to be principal barriers that accounted for nurses’ reluctance to uncover mental health problems (Nolan, Murray & Dallender, 1999).
Health System Barriers
Organizational system barriers may limit implementation of depression guidelines or quality of care improvements. These include lack of coordination and collaboration between providers in primary care, long-term care and specialty mental health providers and shortages of nursing and social service professionals who have training and expertise in geriatric mental health (Bartels, et al., 2002). Economic barriers can interact with organizational barriers. Inadequate or discriminatory financing of mental health services for older adults may defer care (Bartels, et al., 2002). Capitated payment systems that effectively create incentives to provide fewer services or lack of mechanisms to pay for depression care provided by nurses or social workers are examples (Frank, Huskamp & Pincus, 2003). Inadequate drug coverage and the high cost of drugs may deter elders using antidepressants or taking less than recommended doses to reduce costs (Ganguli, 2003; Goldman, Joyce, Escarce, Pace, Solomon, et al., 2004).
Effective Strategies to Improve the Delivery of Depression Care for the Elderly
Depression care quality improvement strategies have been shown to be effective in reducing barriers to depression care (Badamgarav, Weingarten, Henning, Knight, Hasselblad, Gano, et al., 2003; Gilbody, et al., 2003; Mulsant, Whyte, Lenze, Lotrich, Karp, Pollock, et al., 2003) - including among racial/ethnic minorities (Wells, Sherbourne, Schoenbaum, Ettner, Duan, Miranda, et al., 2004). Organizational and educational strategies have been most frequently studied. Modest or mixed results stem from provider education and usually are most effective when combined with more complex interventions that bring additional resources into the health care system (Cherry, Vickrey, Schwankovsky, Heck, Plauchm & Yep, 2004; Gilbody, Whitty, Grimshaw & Thomas, 2003). Aimed at reducing patient barriers to care, patient and sometimes family education seeking their active engagement in depression care management is particularly promising. Organizational strategies (Reuben, 2002) generally include multifaceted quality improvement disease management interventions that change the way depression care is delivered, such as the implementation of routine depression screening, systematic application of evidence-based practice guidelines, clinical decision-making protocols and algorithms, follow-up through remission and maintenance, enhanced roles of nurses or social workers as depression care managers as well as integration between primary care and mental health specialists or service systems.
Effective Screening and Diagnostic Tools and Practice Guidelines
Tools to facilitate routine screening or physician assessment are designed to reduce failure to detect depression. In recent years, the 9-item Patient Health Questionnaire (PHQ-9) (Kroenke, Spitzer & Williams, 2001) has emerged as one of the most reliable depression screening tools in primary care with a demonstrated ability to identify clinically important depression, to make accurate diagnoses of major depression (Kroenke & Spitzer, 2002), to track severity of depression over time (Löwe et al., 2004) and to monitor patient response to therapy (Löwe, Unützer, Callahan, Perkins & Kroenke, in press). The instrument is valid and reliable (Spitzer, Kroenke & Williams, 1999), has specific diagnostic criteria and clinically significant cutoff scores (Kroenke et al., 2001), and has been used with older adults in the IMPACT primary care study where it was found to be sensitive to change in symptom severity when compared with a longer standardized depression severity measure (Löwe, et al., in press), and can be administered in-person or via telephone (Simon, Ludman, Tutty, Operskalski & von Korff, 2004). Other symptom screening tools are available, as are guidelines for brief, but reliable clinical examination by primary care physicians (Williams, Noel, Cordes, Ramirez & Pignone, 2002). Routine screening of patients with known risk factors is particularly likely to improve care (Schulberg, Bruce, Lee, Williams & Dietrich, 2004).
To improve optimal treatment, there are well-established clinical practice guidelines, consensus statements, and decision-making algorithms for managing depression in older adults (Kurlowicz, 2003; Lebowitz, et al., 1997; Sable, et al., 2002; Sommer, Fenn, Pompei, DeBattista, Lembke, Wang & Flores, 2003; Unützer, et al., 2002). Clinical guidelines are available on professional and organizational websites and address depression care by primary care physicians, nurses, and community based clinics (www.depression-primarycare.org/clinicians/; www.guidelines.gov/summary/summary.aspx?doc_id=3512&nbr=2738&string=depression), including important adaptations for home health care practices (Peterson, 2004).
Effective Health System-Focused Models of Care
Health system-focused depression care models bring new resources into the general health sector or into community agencies, apply clinical guideline care management, activate patient participation in their depression care, and provide patient follow-up and feedback among providers of care. Depression care models that use collaboration between primary care physicians and mental health professionals, where expertise in psychopharmacology in treating depression is provided by a psychiatrist and psychosocial interventions are provided by depression specialist nurses or social workers, are particularly promising approaches to improving depression care for the elderly. Randomized trials have shown collaborative care models to be effective in increasing the motivation of patients to cooperate with treatment, improving the primary care physician’s treatment of depression, and enhancing follow-up care. While further research is needed, there is evidence that collaborative care may be cost-effective (Pyne, Rost, Zhang, Williams, Smith, Fortney, 2003; Simon, Katon, VonKorff, et al., 2001; Schoenbaum, et al., 2001), including for ethnic minority patients (Pirraglia, Rosen, Hermann, Olchanski & Neumann, 2004; Schoenbaum, Miranda, Sherbourne, Duan & Wells, 2004).
In the randomized study Improving Mood-Promoting Access to Collaborative Treatment (IMPACT), collaborative care using a depression care manager to support antidepressant medication treatment was effective in improving depressive symptoms and functional outcomes in adults 60 and older with major depression or dysthymia (Unützer, et al., 2002). A nurse or in some cases a social worker was the designated depression clinical specialist. The depression specialist’s time was primarily devoted to clinical care, including providing PST-PC, much of which was delivered by telephone (Harpole, Stechuchak, Saur, Steffens, Unützer & Oddone, 2003, Haverkamp, et al., 2003).
The Prevention of Suicide in Primary Care Elderly: Collaborative Trial (PROSPECT) randomly tested collaborative care for older adults with either major depression or clinically significant minor depression. Intervention group patients received antidepressant medication or for those declining medication, the offer of brief IPT based on a clinical algorithm, and depression care management by care managers (Bruce, et al., 2004). The intervention substantially reduced suicidal ideation and depression symptom severity.
The Program to Encourage Active, Rewarding Lives for Seniors (PEARLS), a community-integrated model for treating minor depression and dysthymia, tested in a randomized trial, was found to reduce depression symptoms and improve health status in medically ill, low-income, mostly homebound older adults (Ciechanowski, et al., 2004). Patients were recruited through community senior service agencies by social workers who routinely screened elders during scheduled visits or telephone calls and through letters mailed by collaborating agencies to their clients or residents in affiliated public housing.
Two studies have demonstrated improved depression care for home health care patients. Flaherty and colleagues (1998) found that a multifaceted collaborative management home care intervention for depression resulted in lower hospitalization rates (23.5%) compared to a historical control group (40.6%). A randomized controlled trial with blind follow-up six months after recruitment found that care by a psychogeriatric team home care versus usual primary care improved depressive outcomes for 58% versus 25% of people 65 and over (Banerjee, et al, 1996).
The Primary Care Research in Substance Abuse and Mental Health for the Elderly (PRISM-E) randomized study compared integrated behavioral health care with enhanced referral care in primary care settings across the United States (Gallo, Zubritsky, Maxwell, et al., 2004). Integrated care had mental health and substance abuse specialists within the primary care practices; the enhanced referral model included transportation, case management, and other services to engage elderly patients in treatment. Primary care clinicians strongly preferred integrated care.
Collaborative interventions also improve patient adherence and prevent relapse (Lin, Von Korff, Ludman, Rutter, Bush, Simon, et al., 2003). Because depression frequently occurs with other chronic disease, adversely affecting the course of coronary heart disease, cancer, diabetes and arthritis, researchers have begun to examine whether enhancing care for depression improves depression and outcomes of these illnesses (Koike, Unützer & Wells, 2002). The collaborative care model used in the IMPACT study improved affective and functional status, but only minimally affected diabetes outcomes (Williams, Katon, Lin, Noel, Worchel, Cornell, et al., 2004). Among older adults with arthritis, benefits included reduced depression, decreased pain and improved functional status and quality of life (Lin, Katon, VonKorff, Tang, Williams, Kroenke, et al., 2003).
Effective Patient and Provider Educational Strategies
Patient education and activation through peer led educational group formats has been found to be effective in the ongoing management of chronic illness (Lorig & Holman, 2003; Shoor & Lorig, 2002), holding promise for similar programs in depression. Much effort has been expended trying to improve the depression care skills of primary care physicians, but with modest effect (Azocar, Cuffel, Goldman & McCarter, 2003; Callahan, 2001). Grand rounds and simply disseminating guidelines are less effective than academic detailing through brief one-on-one educational sessions (Soumerai, 1998).
Compared to other health professions, there is evidence that nurses are more likely to be willing to participate in geriatric education workshops and have high interest in mental health and dementia training (Larson, Chernoff & Sweet-Holp, 2004; Mayall, Oathamshaw, Lovell & Pusey, 2004). Thus, educational strategies aimed at increasing nurses’ comfort and skill in depression assessment and care management are likely to be successful (Fazi & Wright, 2003; Ell, et al., 2004; Groh & Hoes, 2003; Rosen, Mulsant, Kollar, Kastango, Mazumdar, & Fox, 2002; van Eyk, Diederikas, Kempen, Honig, van de Meer & Brenninkmeijer, 2004).
Translating Research into Practice: Recommendations
Unfortunately, the availability of a strong evidence base does not ensure wide adoption of these practices in existing service systems. Despite mounting evidence that older patients tolerate and respond to treatment with antidepressants or structured psychotherapy, outcomes under real world conditions remain poor (Mulsant, Whyte, Lenze, Lotrich, Kar, Pollock & Reynolds, 2003). Improvement in late-life depression care and outcomes for a larger number of depressed elders depends on success in disseminating and implementing quality of care improvements in diverse settings. Fortunately, researchers have also begun to identify key factors in the dissemination and implementation of evidence based quality of care improvements (Bartels, et al., 2002; Meresman, Hunkeler, Hargreaves, Kirsch, Robinson, Green, et al., 2003; Oishi, Shoai, Katon, Callahan, Unützer, et al., 2003; Pearson, Katz, Soucie, Hunkeler, Meresman, Rooney, et al., 2003).
At the level of the health system, there must be “buy-in” for adopting a chronic care intervention from engaged leaders and administrators who identify the project as important and translate it into clear goals identifiable in policies, procedures, a business plan, and financial plans (ICIC, 2002c). Roles of senior management and strong clinical leaders are particularly important, including the degree to which these key people believe that the evidence responds to significant organizational or clinical needs (Bradley, Webster, Baker, Schlesinger, Inouye, Barth, et al., 2004). Additional important facilitating factors are credible supportive evidence and a health care system infrastructure dedicated to translating the research into practice. Barriers are likely to emerge in relation to the extent to which changes in organizational culture are required, and the amount of coordination needed across departments or disciplines.
The Chronic Care Model (see figure 2) provides a useful framework to guide providers who elect to provide leadership aimed at improving depression care for older adults within their system of care (www.improvingchroniccare.org/change/model/components.html). Developed by Wagner and others based on input from national experts, and extensive pilot work (ICIC, 2002a; Wagner et al., 1996a; Wagner et al., 1996b), this model recommends actions in six specific areas, including 1) the health system, 2) the community, 3) patient self-management support, 4) delivery system design, 5) provider clinical decision support, and 6) clinical information systems (see Figure 2). Intervening at the level of these components is aimed at facilitating productive interactions between patients who take an active part in their care and providers backed by resources and expertise. In turn, these interactions are designed to promote improved health status, higher satisfaction for patients and providers, and lower costs.
Figure 2.
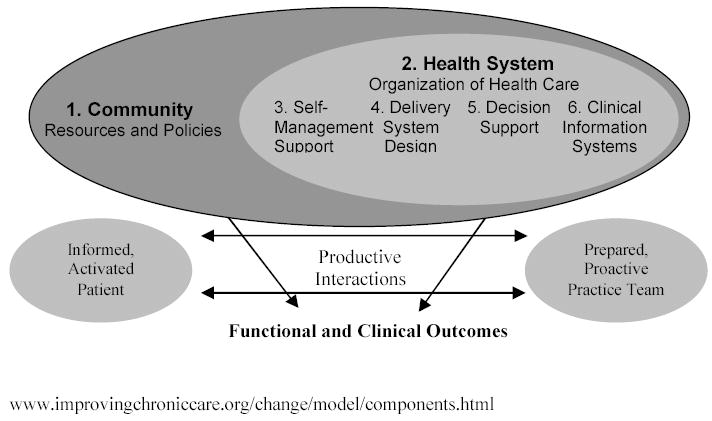
The Chronic Care Model
Personnel must be provided with required resources and support to ensure change, and patients should find services convenient and affordable. Health system level changes may be essential in addressing the attitudes, social norms, and perceived barriers to treatment among providers and lower-level managers. Particularly important, the studies reviewed above emphasize the importance of integrating mental health specialists and strategies within primary care (Oxman, Dietrich & Schulberg, 2003; Sherbourne, Wells, Duan, Miranda, Unützer, Jaycox, et al., 2001).
Delivery system redesign includes using planned interactions to support evidence based care (Sheeran, Brown, Nassisi & Bruce, 2004). Providers need centralized, up-to-date information and active follow-up and outreach must be incorporated into the system, with a designated staff member available for such care. Provider targeted strategies include physician education, application of practice guidelines, physician counseling skill enhancement, application of screening and diagnostic tools, and computer assisted programs to provide management feedback to physicians. Strategies, such as easy to use implementation tool kits and well-described procedures for changing practices are available (Dietrich, et al., 2004; www.depression-primarycare.org; www.Annfammed.org/cgi/content/full/2/4/301/DC1). Routine formal screening for depression in primary care is recommended by the U.S. Preventive Services Task Force. (Pignone, Gaynes, Rushton, Burchell, Orleans, Mulrow, et al., 2002) and tools are available as described above.
Decision support includes delivering care consistent with the scientific evidence and using proven methods to educate providers. At the level of decision support, treatment decisions must be based on explicit, proven guidelines that are discussed with patients (ICIC, 2002f). Providers must have ongoing training to stay up to date, and must remain in the loop when patients are referred for specialty care, through better feedback or joint consultation. These educational interventions can impact provider attitudes, social norms, and perceived barriers to care.
Similarly, clinical information systems provide regular audit and feedback and timely reminders for providers and patients to prompt appropriate care (Smith, et al., 2004). These may be in the form of disease registries that outline recommended care for certain conditions, and check whether individuals’ treatments conform to recommended guidelines (ICIC, 2002g). Outcomes are measured and reminders given for active follow-up. For providers with many competing demands, automated reminders and administrative review may ensure timely depression follow-up care.
At the level of the community, available resources can be identified for supporting or expanding a health system’s care for chronically ill persons (ICIC, 2002b). Partnerships (such as implemented in PEARLS (Ciechanowski, et al., 2004) can be formed with community agencies that provide needed educational, social, legal, or outreach services for the depressed persons, thus expanding service without duplicating efforts. There is evidence that community-based multidisciplinary geriatric mental health treatment teams are effective (Bartels, Dums, oxman, Schneider, Areán, Alexopoulos, et al., 2002; Kohn, Goldsmith & Sedgwick, 2002). In low-income communities, forming linkages among medical, mental health, social service, and community organizations is challenging because existing relationships are often fragmented, and organizations may have scarce resources, however, collaboration and shared responsibility with community agencies may reduce administrator concern about limited resources for new programs (Torrisi & McDaniel, 2003).
At the level of self-management support, patients and family members or caregivers should be given education and information that empowers them to take a central role in their care, so that they may work collaboratively with providers in their ongoing treatment. For depression care, patients need to be taught about available treatment options, symptom monitoring, and engaging effectively with health care providers, family, and friends. Low-income minority patients may require additional education and training in self-empowerment techniques to be active participants in their care, given their often low levels of formal education and often disenfranchised status (Dwight-Johnson, et al., in press). Self-management programs may have to address language or cultural barriers to care and allow families to play a more central role in treatment. Helping patients to communicate more effectively with providers may also help providers overcome linguistic and cultural barriers to providing good care (Johnson, et al., 2004).
Conclusion
The research base underpinning depression care for older adults is comprehensive and encouraging. There is strong evidence of effective methods to identify and evaluate depression in older adults and strong evidence that treatment is effective in reducing depressive symptoms and improving quality of life. There is recent encouraging evidence from Medicare data that older adults (and their caregivers) may be more willing to seek and accept antidepressant treatment. Health care providers are increasingly more likely to detect and treat depression in elderly patients. Unfortunately, critical barriers remain that preclude many older adults from receiving adequate care. Foremost among these are health care system, financing and cost factors. Compelling evidence of elder need, the availability of effective treatments, and the recent evidence of effective strategies to address even some of the more intransigent health system barriers to care demand even greater commitment to and advocacy for evidence-based depression practice in a society whose population of elderly is growing (Bartels, 2003; Lyness, 2004).
Acknowledgments
The work on this manuscript was supported, in part, by NIMH grant 5 R24 MH61700-02 (Dr. Ell, PI).
References
- Alexopoulos GS, Raue P, Areán P. Problem-solving therapy versus supportive therapy in geriatric major depression with executive dysfunction. American Journal of Geriatric Psychiatry. 2003;11:46–52. [PubMed] [Google Scholar]
- Alexopoulos GS, Vrontou C, Kakuma T, Meyers BS, Young RC, Klausner E, Clarkin J. Disability in geriatric depression. American Journal of Psychiatry. 1996;153:877–885. doi: 10.1176/ajp.153.7.877. [DOI] [PubMed] [Google Scholar]
- Allen-Burge R, Storandt M, Kinscherf DA, Rubin EH. Sex differences in the sensitivity of two self-reported depression scales in older depression inpatients. Psychology and Aging, . 1994;9:443–445. doi: 10.1037//0882-7974.9.3.443. [DOI] [PubMed] [Google Scholar]
- Alvidrez J, Areán PA. Physician willingness to refer older depressed patients for psychotherapy. International Journal of Psychiatry in Medicine. 2002;32(1):21–35. doi: 10.2190/J26T-YQMJ-BF83-M05D. [DOI] [PubMed] [Google Scholar]
- Aparasu R, Mort J, Brandt H. Psychotropic medication expenditures for community-dwelling elderly persons. Psychiatric Services. 2003;54(5):739–42. doi: 10.1176/appi.ps.54.5.739. [DOI] [PubMed] [Google Scholar]
- Areán PA, Cook BL. Psychotherapy and combined psychotherapy/pharmacotherapy for late life depression. Biological Psychiatry. 2002;52:293–303. doi: 10.1016/s0006-3223(02)01371-9. [DOI] [PubMed] [Google Scholar]
- Areán PA, Unützer J. Inequities in depression management in low-income, minority, and old-old adults: a matter of access to preferred treatments? Journal of American Geriatrics Sociology. 2003;51:1808–9. doi: 10.1046/j.1532-5415.2003.51569.x. [DOI] [PubMed] [Google Scholar]
- Areán PA, Alvidrez J, Barrera A, Robinson GS, Hicks S. Would older medical patients use psychological services? Gerontologist. 2002;42(3):392–8. doi: 10.1093/geront/42.3.392. [DOI] [PubMed] [Google Scholar]
- Areán PA, Alvidrez J, Feldman M, Tong L, Shermer R. The role of provider attitudes in prescribing antidepressants to older adults: leverage points for effective provider education. International Journal of Psychiatry Medicine. 2003;33:241–56. doi: 10.2190/R57T-2A9N-NU19-GNTU. [DOI] [PubMed] [Google Scholar]
- Areán PA, Hegel MT, Reynolds CF. Treating depression in older medical patients with psychotherapy. Journal of Clinical Geropsychology. 2001;7:93–104. [Google Scholar]
- Areán PA, Perri MG, Nezu AM, Schein RL, Christopher F, Joseph TX. Comparative effectiveness of social problem-solving therapy and reminiscence therapy as treatments for depression in older adults. Journal of Consulting and Clinical Psychology. 1993;61:1003–1010. doi: 10.1037//0022-006x.61.6.1003. [DOI] [PubMed] [Google Scholar]
- Ariyo AA, Haan M, Tangen CM, Rutledge JC, Cushman M, Dobs A, Furberg CD. Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans. Cardiovascular Health Study Collaborative Research Group. Circulation. 2000;102:1773–9. doi: 10.1161/01.cir.102.15.1773. [DOI] [PubMed] [Google Scholar]
- Azocar F, Cuffel B, Goldman W, McCarter L. The impact of evidence-based guideline dissemination for the assessment and treatment of major depression in a managed behavioral health care organization. Journal of Behavioral Health Services & Research. 2003;30(1):109–18. doi: 10.1007/BF02287816. [DOI] [PubMed] [Google Scholar]
- Banerjee S, Macdonald AJ. Mental disorder in an elderly home care population: associations with health and social service use. British Journal of Psychiatry. 1996;168:750–756. doi: 10.1192/bjp.168.6.750. [DOI] [PubMed] [Google Scholar]
- Banerjee S, Shamash K, Macdonald AJD, Mann AH. Randomized controlled trial of effect of intervention by a psychogeriatric team on depression in frail elderly people at home. British Medical Journal. 1996;13:1058–1061. doi: 10.1136/bmj.313.7064.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels SJ. Improving the system of care for older adults with mental illness in the United States: findings and recommendations for the President’s New Freedom Commission on Mental Health. American Journal of Geriatric Psychiatry. 2003;11:486–497. [PubMed] [Google Scholar]
- Bartels SJ, Coakley EH, Zubritsky C, Ware JH, Miles KM, Areán PA, et al. PRISM-E Investigators. Improving access to geriatric mental health services: a randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. American Journal of Psychiatry. 2004;161(8):1455–62. doi: 10.1176/appi.ajp.161.8.1455. [DOI] [PubMed] [Google Scholar]
- Bartels SJ, Dums AR, Oxman TE, Schneider LS, Areán PA, Alexopoulos GS, Jeste DV. Evidence-based practices in geriatric mental health care. Psychiatric Services. 2002;53(11):1419–31. doi: 10.1176/appi.ps.53.11.1419. [DOI] [PubMed] [Google Scholar]
- Bazargan M, Hamm-Baugh VP. The relationship between chronic illness and depression in a community of urban Black elderly persons. Journal of Gerontology. 1995;50B:S119–S127. doi: 10.1093/geronb/50b.2.s119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beekman AT, Deeg DJ, Braam AW, Smit JH, VanTilburg W. Consequences of major and minor depression in later life: a study of disability, well-being and service utilization. Psychological Medicine. 1997;27:1397–1409. doi: 10.1017/s0033291797005734. [DOI] [PubMed] [Google Scholar]
- Black SA, Markides KS. Depressive symptoms and mortality in older Mexican-Americans. Annals of Epidemiology. 1999;9(1):45–52. doi: 10.1016/s1047-2797(98)00025-8. [DOI] [PubMed] [Google Scholar]
- Blank K, Gruman C, Robinson JT. Case-finding for depression in elderly people: balancing ease of administration with validity in varied treatment settings. Journal of Gerontology: Medical Sciences. 2004;59A:378–384. doi: 10.1093/gerona/59.4.m378. [DOI] [PubMed] [Google Scholar]
- Blazer D, Burchett D, Service C, George LK. The association of age and depression among the elderly: an epidemiologic exploration. Journal of Gerontology: Medical Science. 1991;46:M210–M215. doi: 10.1093/geronj/46.6.m210. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–75. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- Bosworth HB, McQuoid DR, George LK, Steffens DC. Time-to-remission from geriatric depression: psychosocial and clinical factors. American Journal of Geriatric Psychiatry. 2002;10:551–559. [PubMed] [Google Scholar]
- Bradley, E.H., Webster, T.R., Baker, D., Schlesinger, M., Inouye, S.K., Barth, M.C., et al. (2004). Translating research into practice: speeding the adoption of innovative health care programs. Issue Brief, The Commonwealth Fund. www.cmwf.org. [PubMed]
- Brown EL, Bruce ML, McAvay GJ, Raue PJ, Lachs MS, Nassisi P. Recognition of late-life depression in home care: accuracy of the outcome and assessment Information Set. Journal of the American Geriatrics Society. 2004;52:995–999. doi: 10.1111/j.1532-5415.2004.52271.x. [DOI] [PubMed] [Google Scholar]
- Brown EL, Bruce ML, McAvay GJ, Raue PJ, Lachs MS, Nassisi P. Recognition of late-life depression in home care: accuracy of the outcome and assessment Information Set. Journal of the American Geriatrics Society. 2004;52:995–999. doi: 10.1111/j.1532-5415.2004.52271.x. [DOI] [PubMed] [Google Scholar]
- Brown EL, McAvay GJ, Raue PJ, Moses S, Bruce ML. Recognition of depression among elderly recipients of home care services. Psychiatry Services. 2003;54:208–213. doi: 10.1176/appi.ps.54.2.208. [DOI] [PubMed] [Google Scholar]
- Brown EL, McAvay GJ, Raue PJ, Moses S, Bruce ML. Recognition of depression among elderly recipients of home care services. Psychiatry Services. 2003;54:208–213. doi: 10.1176/appi.ps.54.2.208. [DOI] [PubMed] [Google Scholar]
- Bruce ML. Psychosocial risk factors for depressive disorders in late life. Biol Psychiatry. 2002;52:175–184. doi: 10.1016/s0006-3223(02)01410-5. [DOI] [PubMed] [Google Scholar]
- Bruce ML, McAvay GJ, Raue PJ, Brown EL, Meyers BS, Keohane DJ, et al. Major depression in elderly home health care patients. American Journal of Psychiatry. 2002;159:1367–1374. doi: 10.1176/appi.ajp.159.8.1367. [DOI] [PubMed] [Google Scholar]
- Bruce ML, Ten Have TR, Reynolds CF, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- Bruno L, Ahrens J. The importance of screening for depression in home care patients. Caring. 2003;22:54–58. [PubMed] [Google Scholar]
- Bump GM, Mulsant BH, Pollock BG, Mazumdar S, Begley AE, Dew MA, Reynolds CF., 3rd Paroxetine versus nortriptyline in the continuation and maintenance treatment of depression in the elderly. Depression & Anxiety. 2001;13:38–44. doi: 10.1002/1520-6394(2001)13:1<38::aid-da6>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Burns MJ, Cain VA, Husaini BA. Depression, service utilization, and treatment costs among Medicare elderly: gender differences. Home Health Care Services Quarterly. 2001;19:35–44. doi: 10.1300/J027v19n03_03. [DOI] [PubMed] [Google Scholar]
- Callahan CM. Quality improvement research on late life depression in primary care. Medical Care. 2001;39:772–784. doi: 10.1097/00005650-200108000-00004. [DOI] [PubMed] [Google Scholar]
- Charney DS, Reynolds CF, Lewis L, Lebowitz BD, Sunderland T, Alexopoulos GS, et al. Depression and Bipolar Support Alliance consensus statement on the unmet needs in diagnosis and treatment of mood disorders in late life. Archives of General Psychology. 2003;60:664–72. doi: 10.1001/archpsyc.60.7.664. [DOI] [PubMed] [Google Scholar]
- Cherry DL, Vickrey BG, Schwankovsky L, Heck E, Plauchm M, Yep R. Interventions to improve quality of care: the Kaiser Permanente-Alzheimer's Association Dementia Care Project. American Journal of Managed Care. 2004;10(8):553–60. [PubMed] [Google Scholar]
- Chu L, Schnelle JF, Osterweil D. Prescription analgesic and antidepressant utilization and cost among elderly Medicaid beneficiaries before and after nursing home admission. Journal of the American Medical Directors Association. 2004;5(2):75–81. doi: 10.1097/01.JAM.0000113429.87302.2E. [DOI] [PubMed] [Google Scholar]
- Ciechanowski P, Wagner E, Schmaling K, Schwartz S, Williams B, Diehr P, et al. Community-integrated home-based depression treatment in older adults: A randomized controlled trial. JAMA. 2004;29:1569–1577. doi: 10.1001/jama.291.13.1569. [DOI] [PubMed] [Google Scholar]
- Conwell Y, Duberstein PR. Prevention of late life suicide: When, where why and how. Psychiatric Clinical Neurosciences. 1995;49:S79–S83. doi: 10.1111/j.1440-1819.1995.tb01924.x. [DOI] [PubMed] [Google Scholar]
- Cooper LA, et al. The acceptability of treatment for depression among African-American, Hispanic, and White primary care patients. Medical Care. 2003;41:479–489. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- Cooper-Patrick L, et al. Identification of patient attitudes and preferences regarding treatment of depression. JGIM. 1997;12(7):431–438. doi: 10.1046/j.1525-1497.1997.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper-Patrick L, Powe NR, Jenckes MW, Gonzales JJ, Levine DM, Ford DE. Identification of patient attitudes and preferences regarding treatment of depression. Journal of General Internal Medicine. 1997;12:431–438. doi: 10.1046/j.1525-1497.1997.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covinsky KE, Fortinsky RH, Palmer RM, Kresevic DM, Landefeld CS. Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons. Annals of Internal Medicine. 1997;126:417–425. doi: 10.7326/0003-4819-126-6-199703150-00001. [DOI] [PubMed] [Google Scholar]
- Croghan TW, Melfi CA, Dobrez DG, Kniesner TJ. Effect of mental health specialty care on antidepressant length of therapy. Medical Care. 1999;37(4 Suppl Lilly):AS20–3. doi: 10.1097/00005650-199904001-00004. [DOI] [PubMed] [Google Scholar]
- Cronin-Stubbs D, de Leon CF, Beckett LA, Field TS, Glynn RJ, Evans DA. Six-year effect of depressive symptoms on the course of physical disability in community-living older adults. Archives of Internal Medicine. 2000;160:3074–80. doi: 10.1001/archinte.160.20.3074. [DOI] [PubMed] [Google Scholar]
- Crystal S, Sambamoorthi U, Walkup JT, Akincigil A. Diagnosis and treatment of depression in the elderly Medicare population: Predictors, disparities, and trends. Journal of the American Geriatric Society. 2003;51:1718–1728. doi: 10.1046/j.1532-5415.2003.51555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai Y, Zhang S, Yamamoto J, Ao M, Belin TR, Cheung F, Hifumi SS. Cognitive behavioral therapy of minor depressive symptoms in elderly Chinese Americans: a pilot study. Community Mental Health Journal. 1999;35(6):537–42. doi: 10.1023/a:1018763302198. [DOI] [PubMed] [Google Scholar]
- deJonge P, Ormel J, Slaets J, Kempen G, Ranchor A, van Jaarsveld C, et al. Depressive symptoms in elderly patients predict poor adjustment after somatic events. American Journal of Geriatric Psychiatry. 2004;12:57–64. [PubMed] [Google Scholar]
- Dennis MS, Lindesay J. Suicide in the elderly -- The United Kingdom Perspective. International Psychogeriatrics. 1995;7:263–274. doi: 10.1017/s104161029500202x. [DOI] [PubMed] [Google Scholar]
- Devanand DP, Kim MK, Paykina N, Sackeim HA. Adverse life events in elderly patients with major depression or dysthymic disorder and in healthy-control subjects. American Journal of Geriatric Psychiatry. 2002;10(3):265–74. [PubMed] [Google Scholar]
- Dietrich AJ, Oxman TE, Williams JW, Jr, Kroenke K, Schulberg HC, Bruce M, Barry SL. Going to scale: re-engineering systems for primary care treatment of depression. Annals of Family Medicine. 2004;2(4):301–4. doi: 10.1370/afm.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doraiswamy PM, Khan ZM, Donahue RMJ, Richard NE. The spectrum of quality-of-life impairments in recurrent geriatric depression. Journal of Gerontology: Medical Sciences. 2002;57:M134–M137. doi: 10.1093/gerona/57.2.m134. [DOI] [PubMed] [Google Scholar]
- Doraiswamy PM, Krishnan KR, Oxman T, Jenkyn LR, Coffey DJ, Burt T, Clary CM. Does antidepressant therapy improve cognition in elderly depressed patients? Journals of Gerontology Series A-Biological Sciences & Medical Sciences. 2003;58(12):M1137–44. doi: 10.1093/gerona/58.12.m1137. [DOI] [PubMed] [Google Scholar]
- Dunner DL. Treatment considerations for depression in the elderly. CNS Spectrums. 2003;8(Suppl 3):14–9. doi: 10.1017/s1092852900008233. [DOI] [PubMed] [Google Scholar]
- Dwight-Johnson M, et al. Treatment preferences among depressed primary care patients. JGIM. 2000;15:527–534. doi: 10.1046/j.1525-1497.2000.08035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwight-Johnson M, et al. Can quality improvement programs for depression in primary care address patient preferences for treatment? Medical Care. 2001;39(9):934–944. doi: 10.1097/00005650-200109000-00004. [DOI] [PubMed] [Google Scholar]
- Dwight-Johnson M, Lagomasino IT, Aisenberg E, Hay J. Using conjoint analysis to assess depression treatment preferences among low-income Latinos. Psychiatric Services. 2004;55:934–936. doi: 10.1176/appi.ps.55.8.934. [DOI] [PubMed] [Google Scholar]
- Dwight-Johnson, M., Ell, K., & Jiuan-Lee, P. (in press). Can Collaborative Care Address the Needs of Low-income Latinas with Comorbid Depression and Cancer? Results from a Randomized Pilot Study. Psychosomatics. [DOI] [PubMed]
- Engberg S, Sereika S, Weber E, Engberg R, McDowell BJ, Reynolds CF. Prevalence and recognition of depressive symptoms among homebound older adults with urinary incontinence. Journal of Geriatric Psychiatry & Neurology. 2001;14:130–139. doi: 10.1177/089198870101400306. [DOI] [PubMed] [Google Scholar]
- Eggar R, Spencer A, Anderson D, Hiller L. Views of elderly patients on cardiopulmonary resuscitation before and after treatment for depression. International Journal of Geriatric Psychiatry. 2002;17(2):170–4. doi: 10.1002/gps.523. [DOI] [PubMed] [Google Scholar]
- Ell, K., & Enguidanos, S. (2004). Evidence-based Depression Care for Elders in Home Health & Geriatric Care Management. National Gerontological Social Work Conference, Anaheim, CA, March.
- Ell, K., Unützer, J., Aranda, M., Sanchez, K., & Lee, PJ. (in press). Routine PHQ-9 Depression Screening in Home Health Care: Depression Prevalence, Clinical and Treatment Characteristics. Home Health Care Services Quarterly. [DOI] [PMC free article] [PubMed]
- Evans DL, Staab JP, Petitto JM, Morrison MF, Szuba MP, Ward HE, et al. Depression in the medical setting: biopsychological interactions and treatment considerations. Journal of Clinical Psychiatry, 60 Suppl. 1999;4:40–55. [PubMed] [Google Scholar]
- Fazzi RA, Wright K. Improving OASIS accuracy: a national effort. Caring Magazine. 2003;23:52–56. [PubMed] [Google Scholar]
- Fischer LR, Wei F, Solberg LI, Rush WA, Heinrich RL. Treatment of elderly and other adult patients for depression in primary care. Journal of the American Geriatrics Society. 2003;51(11):1554–62. doi: 10.1046/j.1532-5415.2003.51506.x. [DOI] [PubMed] [Google Scholar]
- Flaherty JH, McBride M, Marzouk S, Miller DK, Chien N, Hanchett M, et al. Decreasing hospitalization rates for older home care patients with symptoms of depression. Journal of the American Geriatrics Society. 1998;46:31–38. doi: 10.1111/j.1532-5415.1998.tb01010.x. [DOI] [PubMed] [Google Scholar]
- Flint AJ. The complexity and challenge of non-major depression in late life. American Journal of Geriatric Psychiatry. 2002;10:229–232. [PubMed] [Google Scholar]
- Frank RG, Huskamp HA, Pincus HA. Aligning incentives in the treatment of depression in primary care with evidence-based practice. Psychiatric Services. 2003;54:682–687. doi: 10.1176/appi.ps.54.5.682. [DOI] [PubMed] [Google Scholar]
- Gallo JJ, Cooper-Patrick L, Lesikar S. Depressive symptoms of whites and African Americans aged 60 years and older. Journal of Gerentology: Psychological Sciences & Social Science. 1998;53:277–286. doi: 10.1093/geronb/53b.5.p277. [DOI] [PubMed] [Google Scholar]
- Gallo JJ, Zubritsky C, Maxwell J, Nazar M, Bogner HR, Quijano LM, et al. PRISM-E Investigators. Primary care clinicians evaluate integrated and referral models of behavioral health care for older adults: results from a multisite effectiveness trial (PRISM-e) Annals of Family Medicine. 2004;2:305–9. doi: 10.1370/afm.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganguli G. Consumers Devise Drug Cost-Cutting Measures: Medical and Legal Issues to Consider. Health Care Manager. 2003;22:275–281. doi: 10.1097/00126450-200307000-00013. [DOI] [PubMed] [Google Scholar]
- Geerlings SW, Beekman AT, Deeg DJ, Wwisk JW, Vantilburg W. Duration and severity of depression predict mortality in older adults in the community. Psychological Medicine, 32, 609–618. Geriatric Psychiatry. 2002;11:543–550. doi: 10.1017/s0033291702005585. [DOI] [PubMed] [Google Scholar]
- Gerrity MS, Williams JW, Dietrich AJ, Olson AL. Identifying physicians likely to benefit from depression education: a challenge for health care organizations. Medical Care. 2001;39(8):856–66. doi: 10.1097/00005650-200108000-00011. [DOI] [PubMed] [Google Scholar]
- Goldman B, Balgobin S, Bish R, Lee RH, McCue S, Morrison MH, et al. Nurse educators are key to a best practices implementation program. Geriatric Nursing. 2004;25:171–174. doi: 10.1016/j.gerinurse.2004.04.013. [DOI] [PubMed] [Google Scholar]
- González HM, Haan MN, Hinton L. Acculturation and the prevalence of depression in older Mexican Americans: baseline results of the Sacramento area Latino study on aging. Journal of the American Geriatrics Society. 2001;49:948–953. doi: 10.1046/j.1532-5415.2001.49186.x. [DOI] [PubMed] [Google Scholar]
- Goldman DP, Joyce GF, Escarce JJ, Pace JE, Solomon MD, Laouri M, et al. Pharmacy Benefits and the Use of Drugs by the Chronically Ill. Journal of the American Medical Association. 2004;291:2344–2350. doi: 10.1001/jama.291.19.2344. [DOI] [PubMed] [Google Scholar]
- Goulding MR. Inappropriate medication prescribing for elderly ambulatory care patients. Archives of Internal Medicine. 2004;164:305–12. doi: 10.1001/archinte.164.3.305. [DOI] [PubMed] [Google Scholar]
- Green-Hennessy S, Hennessy KD. Demographic differences in medication use among individuals with self-reported major depression. Psychiatric Services. 1999;50:257–9. doi: 10.1176/ps.50.2.257. [DOI] [PubMed] [Google Scholar]
- Groh CJ, Hoes ML. Practice methods among nurse practitioners treating depressed women. Journal of the American Academy of Nurse Practitioners. 2003;15:130–136. doi: 10.1111/j.1745-7599.2003.tb00269.x. [DOI] [PubMed] [Google Scholar]
- Gum A, Areán PA. Current status of psychotherapy for mental disorders in the elderly. Current Psychological Reports. 2004;6:32–38. doi: 10.1007/s11920-004-0035-7. [DOI] [PubMed] [Google Scholar]
- Harman JS, Crystal S, Walkup J, Olfson M. Trends in elderly patients' office visits for the treatment of depression according to physician specialty: 1985–1999. Journal of Behavioral Health Services & Research. 2003;30(3):332–41. doi: 10.1007/BF02287321. [DOI] [PubMed] [Google Scholar]
- Harman JS, Edlund MJ, Fortney JC. Disparities in the adequacy of depression treatment in the United States. Psychiatric Services. 2004;55:1379–1385. doi: 10.1176/appi.ps.55.12.1379. [DOI] [PubMed] [Google Scholar]
- Harpole LH, Stechuchak KM, Saur CD, Steffens DC, Unützer J, Oddone E. Implementing a disease management intervention for depression in primary care: a random work sampling study. General Hospital Psychiatry. 2003;25(4):238–45. doi: 10.1016/s0163-8343(03)00023-9. [DOI] [PubMed] [Google Scholar]
- Haverkamp R, Areán P, Hegel MT, Unützer J. Problem-solving treatment for complicated depression in late life: a case study in primary care. Perspectives in Psychiatric Care. 2004;40:45–52. doi: 10.1111/j.1744-6163.2004.00045.x. [DOI] [PubMed] [Google Scholar]
- Hayes D. Recent developments in antidepressant therapy in special populations. American Journal of Managed Care. 10. 2004;(6 Suppl):S179–85. [PubMed] [Google Scholar]
- Hays JC, Steffens DC, Flint EP, Bosworth HB, George LK. Does social support buffer functional decline in elderly patients with unipolar depression? American Journal of Psychiatry. 2001;158:1850–1855. doi: 10.1176/appi.ajp.158.11.1850. [DOI] [PubMed] [Google Scholar]
- Hendrie HC, Callahan CM, Levitt EE, Hui SL, Musick B, Austrom MG, et al. Prevalence rates of major depressive disorders: The effects of varying the diagnostic criteria in an older primary care population. American Journal of Geriatric Psychology. 1995;5:119–131. doi: 10.1097/00019442-199500320-00004. [DOI] [PubMed] [Google Scholar]
- Henriksson MM, Marttunen MJ, Isometsä ET, Heikkinen ME, Aro HM, Kuoppasalmi KI, Lönnqvist JK. Mental disorders in elderly suicide. International Psychogeriatrics. 1995;7:275–286. doi: 10.1017/s1041610295002031. [DOI] [PubMed] [Google Scholar]
- Holman H, Lorig K. Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Reports. 2004;119(3):239–43. doi: 10.1016/j.phr.2004.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman GB. Evaluating and treating unintentional weight loss in the elderly. American Family Physician. 2002;65:640–650. [PubMed] [Google Scholar]
- Hunkeler EM, Meresman JF, Hargreaves WA, Fireman B, Berman WH, Kirsch AJ, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Archives of Family Medicine. 2000;9(8):700–8. doi: 10.1001/archfami.9.8.700. [DOI] [PubMed] [Google Scholar]
- Improving Chronic Illness Care ICIC (2002a): The Chronic Care Model: Model Components: Overview of the Chronic Care Model. www.improvingchroniccare.org/change/model/components.html
- Johnson RL, Saha S, Arbelaez JJ, Beach MC, Cooper LA. Racial and ethnic differences in patient perceptions of bias and cultural competence in health care. Journal of General Internal Medicine. 2004;19:101–110. doi: 10.1111/j.1525-1497.2004.30262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jongenelis K, Pot AM, Eises AMH, Beekman ATF, Kluiter H, Ribbe MW. Prevalence and risk indicators of depression in elderly nursing home patients: the AGED study. Journal of Affective disorders. 2004;83:135–142. doi: 10.1016/j.jad.2004.06.001. [DOI] [PubMed] [Google Scholar]
- Jorm AF. Epidemiology of mental disorders in old age. Current Opinion Psychiatry. 1998;11:405–409. [Google Scholar]
- Juurlink DN, Herrmann N, Szalai JP, Kopp A, Redelmeier DA. Medical illness and the risk of suicide in the elderly. Archives of Internal Medicine. 2004;164:1179–1184. doi: 10.1001/archinte.164.11.1179. [DOI] [PubMed] [Google Scholar]
- Katon WJ, Lin E, Russo J, Unützer J. Increased medical costs of a population-based sample of depressed elderly patients. Archives of General Psychiatry. 2003;60:897–903. doi: 10.1001/archpsyc.60.9.897. [DOI] [PubMed] [Google Scholar]
- Katz IR. On the inseparability of mental and physical health in aged persons: Lessons from depression and medical comorbidity. American Journal of Geriatric Psychiatry. 1996;4:1–16. doi: 10.1097/00019442-199624410-00001. [DOI] [PubMed] [Google Scholar]
- Kindy D. Ongoing primary care intervention increased remission and emotional and physical role functioning in major depression. Evidence-Based Nursing. 2003;6:86. doi: 10.1136/ebn.6.3.86. [DOI] [PubMed] [Google Scholar]
- Knauper B, Wittchen HU. Diagnosing major depression in the elderly: Evidence for response bias in standardized diagnostic interviews? Journal of Psychiatric Research. 1994;8:147–164. doi: 10.1016/0022-3956(94)90026-4. [DOI] [PubMed] [Google Scholar]
- Koenig HG, George LK. Depression and physical disability outcomes in depressed medically ill hospitalized older adults. American Journal of Geriatric Psychiatry. 1998;6:230–247. [PubMed] [Google Scholar]
- Koenig HG, Kutchibhatla M. Use of health services by medically ill depressed elderly patients after hospital discharge. American Journal of Geriatric Psychiatry. 1999;7:48–56. [PubMed] [Google Scholar]
- Koenig HG, Kutchibhatla M. Use of health services by medically ill depressed elderly patients after hospital discharge. American Journal of Geriatric Psychiatry. 1999;7:48–56. [PubMed] [Google Scholar]
- Koenig HG, Gittelman D, Branski S, Brown S, Stone P, Ostrow B. Depressive symptoms in elderly medical-surgical patients hospitalized in community settings. American Journal of Geriatric Psychiatry. 1998;6(1):14–23. [PubMed] [Google Scholar]
- Kohn R, Goldsmith E, Sedgwick TW. Treatment of homebound mentally ill elderly patients: the multidisciplinary psychiatric mobile team. American Journal Geriatric Psychiatry. 2002;10:469–475. [PubMed] [Google Scholar]
- Koike AK, Unützer J, Wells KB. Improving the care for depression in patients with comorbid medical illness. American Journal of Psychiatry. 2002;159:1738–1745. doi: 10.1176/appi.ajp.159.10.1738. [DOI] [PubMed] [Google Scholar]
- Kraaij V, Arensman E, Spinhoven P. Negative life events and depression in elderly persons: a meta-analysis. Journals of Gerontology Series B-Psychological Sciences & Social Sciences. 2002;57(1):87–94. doi: 10.1093/geronb/57.1.p87. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annual. 2002;32:509–515. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;169:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunik ME, Braun U, Stanley MA, Wristers K, Molinari V, Stoebner D, Orengo CA. One session cognitive behavioural therapy for elderly patients with chronic obstructive pulmonary disease. Psychological Medicine. 2001;31(4):717–23. doi: 10.1017/s0033291701003890. [DOI] [PubMed] [Google Scholar]
- Kurlowicz LH. (2003). Depression in older adults. In: Mezey M, Fulmer T, Abraham I, Zwicker DA, editor(s). Geriatric nursing protocols for best practice. 2nd ed. New York (NY): Springer Publishing Company, Inc.; p.185–206.
- Langa KM, Valenstein MA, Fendrick AM, Kabeto MU, Vijan S. Extent and cost of informal caregiving for older Americans with symptoms of depression. American Journal of Psychiatry. 2004;161:857–63. doi: 10.1176/appi.ajp.161.5.857. [DOI] [PubMed] [Google Scholar]
- Larson JS, Chernoff R, Sweet-Holp TJ. An evaluation of provider educational needs in geriatric care. Evaluation & the Health Professions. 2004;27:95–103. doi: 10.1177/0163278703261209. [DOI] [PubMed] [Google Scholar]
- Lavretsky H, Kuman A. Clinically significant non-major depression: old concepts, new insights. American Journal of Geriatric Psychiatry. 2002;10:239–255. [PubMed] [Google Scholar]
- Lavretsky H, Bastani R, Gould R, Huang D, Llorente M, Maxwell A, Jarvik L. UPBEAT Collaborative Group. Unified Psychogeriatric Biopsychological Evaluation and Treatment. Predictors of two-year mortality in a prospective "UPBEAT" study of elderly veterans with comorbid medical and psychiatric symptoms. American Journal of Geriatric Psychiatry. 2002;10:458–68. [PubMed] [Google Scholar]
- Lebowitz BD, Pearson JL, Schneider LS, Reynolds CF, Alexopoulow GS, Bruce ML, et al. Diagnosis and treatment of depression in late life: Consensus statement update. JAMA. 1997;278:1186–1190. [PubMed] [Google Scholar]
- Lenze EJ. Comorbidity of depression and anxiety in the elderly. Current Psychiatry Reports. 2003;5:62–67. doi: 10.1007/s11920-003-0011-7. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Mulsant BH, Dew MA, Shear MK, Houck P, Pollock BG, Reynolds CF., 3rd Good treatment outcomes in late-life depression with comorbid anxiety. Journal of Affective Disorders. 2003;77:247–54. doi: 10.1016/s0165-0327(02)00177-5. [DOI] [PubMed] [Google Scholar]
- Lin EH, Katon WJ, Simon GE, VonKorff M, Bush TM, Rutter CM, et al. Achieving guidelines for the treatment of depression in primary care: Is physician education enough? Medical Care. 1997;35:831–842. doi: 10.1097/00005650-199708000-00008. [DOI] [PubMed] [Google Scholar]
- Lin EH, Katon W, Von Korff M, Tan L, Williams JW, Jr, Kroenke K, et al. IMPACT Investigators: Effect of improving depression care on pain and functional outcomes among older adults with arthritis: a randomized controlled trial. JAMA. 2003;290:2428–9. doi: 10.1001/jama.290.18.2428. [DOI] [PubMed] [Google Scholar]
- Lin EH, Von Korff M, Ludman EJ, Rutter C, Bush TM, Simon GE, et al. Enhancing adherence to prevent depression relapse in primary care. General Hospital Psychiatry. 2003;25:303–10. doi: 10.1016/s0163-8343(03)00074-4. [DOI] [PubMed] [Google Scholar]
- Lish JD, Zimmerman M, Farber NJ, Lush DT, Kuzma MA, Plescia G. Suicide screening in a primary care setting at a Veterans Affairs Medical Center. Psychosomatics. 1996;37:413–424. doi: 10.1016/S0033-3182(96)71528-1. [DOI] [PubMed] [Google Scholar]
- Löwe, B., Gräfe, K., Zipfel, S., Witte, S., Loerch B., & Herzog, W. (in press). Diagnosing ICD-10 depressive episodes: Superior criterion validity of the Patient Health Questionnaire. Psychotherapy & Psychosomatics. [DOI] [PubMed]
- Löwe B, Kroenke K, Herzog W, Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9) Journal of Affective Disorders. 2004;81:61–66. doi: 10.1016/S0165-0327(03)00198-8. [DOI] [PubMed] [Google Scholar]
- Löwe B, Spitzer RL, Gräfe K, Kroenke K, Quenter A, Zipfel S, et al. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. Journal of Affective Disorders. 2004;78:131–140. doi: 10.1016/s0165-0327(02)00237-9. [DOI] [PubMed] [Google Scholar]
- Löwe, B., Unützer, J., Callahan, C.M., Perkins, A.J., & Kroenke, K. (in press). Monitoring depression treatment outcomes with the PHQ-9. Medical Care. [DOI] [PubMed]
- Luber MP, Meyers BS, Williams-Russo PG, Hollenberg JP, DiDomenico TN, Charlson ME, Alexopoulos GS. Depression and service utilization in elderly primary care patients. American Journal of Geriatric Psychiatry. 2001;9:169–176. [PubMed] [Google Scholar]
- Lyness JM. Treatment of depressive conditions in later life. JAMA. 2004;291:1626–1627. doi: 10.1001/jama.291.13.1626. [DOI] [PubMed] [Google Scholar]
- Lyness JM, Caine ED, King DA, Conwell Y, Duberstein PR, Cox C. Depressive disorders and symptoms in older primary care patients: one-year outcomes. American Journal of Geriatric Psychiatry. 2002;10:275–282. [PubMed] [Google Scholar]
- Lyness JM, Cox C, Curry J, Conwell Y, King DA, Caine ED. Older age and the underreporting of depressive symptoms. Journal of American Geriatrics Society. 1995;43:216–221. doi: 10.1111/j.1532-5415.1995.tb07325.x. [DOI] [PubMed] [Google Scholar]
- Maidment R, Linvingston G, Katona C. ‘Just keep taking the tablets’: adherence to antidepressant treatment in older people in primary care. International Journal of Geriatric Psychiatry. 2002;17:752–757. doi: 10.1002/gps.688. [DOI] [PubMed] [Google Scholar]
- Marwaha S, Livingston G. Stigma, racism or choice. Why do depressed ethnic elders avoid psychiatrists? Journal of Affective Disorders. 2002;72:257–265. doi: 10.1016/s0165-0327(01)00470-0. [DOI] [PubMed] [Google Scholar]
- Mayall E, Oathamshaw S, Lovell K, Pusey H. Development and piloting of a multidisciplinary training course for detecting and managing depression in the older person. Journal of Psychiatry and Mental Health Nursing. 2004;11:165–171. doi: 10.1111/j.1365-2850.2003.00702.x. [DOI] [PubMed] [Google Scholar]
- McAvay, G.J., Bruce, M.L., Raue, P.J., & Brown, E. (In press). Depression in elderly homecare patients: patient versus informant reports. Psychological Medicine [DOI] [PubMed]
- McDonald MV, Passik SD, Dugan W, Rosenfeld B, Theobald DE, Edgerton S. Nurses’ recognition of depression in their patients with cancer. Oncology Nursing Forum, 26, 593–599. Medical Sciences. 1999;58:M461–7. [PubMed] [Google Scholar]
- Mehta, K.M., Yaffe, K., Langa, K.M., Sands, L., Whooley, M.A., & Covinsky, K.E. (2003). Additive effects of cognitive function and depressive symptoms on mortality in elderly community-living adults. Journal of Gerontology Series A-Biological Sciences & [DOI] [PMC free article] [PubMed]
- Melfi CA, Croghan TW, Hanna MP. Access to treatment for depression in a Medicaid population. Journal of Health Care for the Poor & Underserved. 1999;10:201–15. doi: 10.1353/hpu.2010.0100. [DOI] [PubMed] [Google Scholar]
- Melfi CA, Croghan TW, Hanna MP, Robinson RL. Racial variation in antidepressant treatment in a Medicaid population. Journal of Clinical Psychiatry. 2000;61:16–21. doi: 10.4088/jcp.v61n0105. [DOI] [PubMed] [Google Scholar]
- Meresman JF, Hunkeler EM, Hargreaves WA, Kirsch AJ, Robinson P, Green A, et al. A case report: implementing a nurse telecare program for treating depression in primary care. Psychiatric Quarterly. 2003;74:61–73. doi: 10.1023/a:1021145722959. [DOI] [PubMed] [Google Scholar]
- Miller MD, Cornes C, Frank E, Ehrenpreis L, Silberman R, Schlernitzauer MA, et al. Interpersonal psychotherapy for late-life depression: past, present, and future. Journal of Psychotherapy Practice & Research. 2001;10(4):231–8. [PMC free article] [PubMed] [Google Scholar]
- Miller MD, Cornes C, Frank E, Ehrenpreis L, Silberman R, Schlernitzauer MA, et al. Interpersonal psychotherapy for late-life depression: past, present, and future. Journal of Psychotherapy Practice & Research. 2001;10(4):231–8. [PMC free article] [PubMed] [Google Scholar]
- Miller MD, Frank E, Cornes C, Houck PR, Reynolds CF., 3rd The value of maintenance interpersonal psychotherapy (IPT) in older adults with different IPT foci. American Journal of Geriatric Psychiatry. 2003;11(1):97–102. [PubMed] [Google Scholar]
- Miller MD, Frank E, Cornes C, Houck PR, Reynolds CF., 3rd The value of maintenance interpersonal psychotherapy (IPT) in older adults with different IPT foci. American Journal of Geriatric Psychiatry. 2003;11(1):97–102. [PubMed] [Google Scholar]
- Mills TL, Alea NL, Cheong JA. Differences in the indicators of depressive symptoms among a community sample of African-American and Caucasian older adults. Community Mental Health Journal. 2004;40:309–331. doi: 10.1023/b:comh.0000035227.57576.46. [DOI] [PubMed] [Google Scholar]
- Miranda J, Duan N, Sherbourne C, Schoenbaum M, Lagomasino I, Jackson-Triche M, Wells KB. Improving care for minorities: can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health Services Research. 2003;38:613–30. doi: 10.1111/1475-6773.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda J, et al. Improving care for minorities: Can quality improvement intervention improve care and outcomes for depressed minorities? HSR. 2003;38:613–630. doi: 10.1111/1475-6773.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M. Major depression in community-dwelling middle-aged and older adults: prevalence and 2- and 4-year follow-up symptoms. Psychological Medicine. 2004;34:623–634. doi: 10.1017/S0033291703001764. [DOI] [PubMed] [Google Scholar]
- Moser DK. Psychosocial factors and their association with clinical outcomes in patients with heart failure: why clinicians do not seem to care. European Journal of Cardiovascular Nursing. 2002;1(3):183–8. doi: 10.1016/S1474-5151(02)00033-6. [DOI] [PubMed] [Google Scholar]
- Moser DK. Psychosocial factors and their association with clinical outcomes in patients with heart failure: why clinicians do not seem to care. European Journal of Cardiovascular Nursing. 2002;1:183–188. doi: 10.1016/S1474-5151(02)00033-6. [DOI] [PubMed] [Google Scholar]
- Mueller TI, Kohn R, Leventhal N, Leon AC, Solomon D, Coryell W, et al. The course of depression in elderly patients. American Journal of Geriatric Psychiatry. 2004;12(1):22–9. [PubMed] [Google Scholar]
- Mulsant BH, Whyte E, Lenze EJ, Lotrich F, Karp JF, Pollock BG, Reynolds CF., 3rd Achieving long-term optimal outcomes in geriatric depression and anxiety. CNS Spectrums. 2003;8(12 Suppl 3):27–34. doi: 10.1017/s1092852900008257. [DOI] [PubMed] [Google Scholar]
- Nolan P, Murray E, Dallender J. Practice nurses’ perceptions of services for clients with psychological problems in primary care. International Journal of Nursing Studies. 1999;36:97–104. doi: 10.1016/s0020-7489(99)00015-2. [DOI] [PubMed] [Google Scholar]
- Oishi SM, Shoai R, Katon W, Callahan C, Unützer J, Arean P, et al. Improving Mood: Promoting Access to Collaborative Treatment Investigators. Impacting late life depression: integrating a depression intervention into primary care. Psychiatric Quarterly. 2003;74(1):75–89. doi: 10.1023/a:1021197807029. [DOI] [PubMed] [Google Scholar]
- Oxman TE, et al. A three-component model for reengineering systems for the treatment of depression in primary care. Psychosomatics. 2002;43:441–450. doi: 10.1176/appi.psy.43.6.441. [DOI] [PubMed] [Google Scholar]
- Oxman TE, Dietrich AJ, Schulberg HC. The depression care manager and mental health specialist as collaborators within primary care. American Journal of Geriatric Psychiatry. 2003;11(5):507–16. [PubMed] [Google Scholar]
- Pearson B, Katz SE, Soucie V, Hunkeler E, Meresman J, Rooney T, Amick BC., 3rd Evidence-based care for depression in Maine: dissemination of the Kaiser Permanente Nurse Telecare Program. Psychiatric Quarterly. 2003;74(1):91–102. doi: 10.1023/a:1021149923867. [DOI] [PubMed] [Google Scholar]
- Pearson B, Katz SE, Soucie V, Hunkeler E, Meresman J, Rooney T, Amick BC., 3rd Evidence-based care for depression in Maine: dissemination of the Kaiser Permanente Nurse Telecare Program. Psychiatric Quarterly. 2003;74(1):91–102. doi: 10.1023/a:1021149923867. [DOI] [PubMed] [Google Scholar]
- Penninx BW, Guralnik JM, Ferrucci L, Simonsick EM, Deeg D, Wallace RB. Depressive symptoms and physical decline in community-dwelling older persons. JAMA. 1998;279:1720–1726. doi: 10.1001/jama.279.21.1720. [DOI] [PubMed] [Google Scholar]
- Peterson LE. Strengthening condition-specific evidence-based home health care practice. Journal for Healthcare Quality. 2004;26:10–18. doi: 10.1111/j.1945-1474.2004.tb00490.x. [DOI] [PubMed] [Google Scholar]
- Peterson LE. Strengthening condition-specific evidence-based home healthcare practice. Journal for Healthcare Quality. 2004;26(3):10–8. doi: 10.1111/j.1945-1474.2004.tb00490.x. [DOI] [PubMed] [Google Scholar]
- Pfaff JJ, Almeida OP. Identifying suicidal ideation among older adults in a general practice setting. Journal of Affective Disorders. 2004;83:73–7. doi: 10.1016/j.jad.2004.03.006. [DOI] [PubMed] [Google Scholar]
- Pignone MP, Gaynes BN, Rushton JL, Burchell CM, Orleans CT, Mulrow CD, et al. Screening for depression in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2002;136:765–776. doi: 10.7326/0003-4819-136-10-200205210-00013. [DOI] [PubMed] [Google Scholar]
- Pirraglia PA, Rosen AB, Hermann RC, Olchanski NV, Neumann P. Cost-utility analysis studies of depression management: a systematic review. American Journal of Psychiatry. 2004;161:2155–2162. doi: 10.1176/appi.ajp.161.12.2155. [DOI] [PubMed] [Google Scholar]
- Posternak MA, Zimmerman M. How accurate are patients in are patients in reporting their antidepressant treatment history? Journal of Affective Disorders. 2003;75:115–124. doi: 10.1016/s0165-0327(02)00049-6. [DOI] [PubMed] [Google Scholar]
- Prabhakaran P, Butler R. What are older peoples’ experiences of taking antidepressants? Journal of Affective Disorders. 2002;70:319–322. doi: 10.1016/s0165-0327(01)00315-9. [DOI] [PubMed] [Google Scholar]
- Preville M, Cote G, Boyer R, Hebert R. Detection of depression and anxiety disorders by home care nurses. Aging & Mental Health. 2004;8:400–9. doi: 10.1080/13607860410001725009. [DOI] [PubMed] [Google Scholar]
- Proudfoot J, Goldberg D, Mann A, Everitt B, Marks I, Gray JA. Computerized, interactive, multimedia cognitive-behavioural program for anxiety and depression in general practice. Psychological Medicine. 2003;33(2):217–27. doi: 10.1017/s0033291702007225. [DOI] [PubMed] [Google Scholar]
- Pulska T, Pahkala K, Laippala P, Kivela SL. Survival of elderly Finns suffering from dysthymic disorder: a community study. Social Psychiatry & Psychiatric Epidemiology. 1998;33:319–325. doi: 10.1007/s001270050061. [DOI] [PubMed] [Google Scholar]
- Ranga K, Krishnan R, Delong M, Kraemer H, Carney R, Spiegel D, et al. Comorbidity of depression with other medical diseases in the elderly. Biological Psychiatry. 2002;52:559–588. doi: 10.1016/s0006-3223(02)01472-5. [DOI] [PubMed] [Google Scholar]
- Ranga RK, George LK, Peiper CF, Jiang W, Arias R, Look A, O’Connor C. Depression and social support in elderly patients with cardiac disease. American Heart Journal. 1998;136:491–495. doi: 10.1016/s0002-8703(98)70225-x. [DOI] [PubMed] [Google Scholar]
- Rao A, Cohen JJ. Symptom management in the elderly cancer patient: fatigue, pain, and depression. Journal of National Cancer Institute Monographs. 2004;32:150–157. doi: 10.1093/jncimonographs/lgh031. [DOI] [PubMed] [Google Scholar]
- Raue PJ, Brown EL, Bruce ML. Assessing behavioral health using OASIS: Part 1 Depression and suicidality. Home Healthcare Nurse. 2002;20:154–161. doi: 10.1097/00004045-200203000-00006. [DOI] [PubMed] [Google Scholar]
- Raue, P.J., Meyers, B.S., McAvay, G.J., Brown, E.L., Keohane, D.J., & Bruce, M.E. (2003). One-month stability of depression among elderly home-care patients. American Journal of [PubMed]
- Reuben DB. Organizational interventions to improve health outcomes of older persons. Medical Care. 2002;40:416–428. doi: 10.1097/00005650-200205000-00007. [DOI] [PubMed] [Google Scholar]
- Reynolds CF, 3rd, Frank E, Perel JM, Imber SD, Cornes C, Miller MD, et al. Nortriptyline and interpersonal psychotherapy as maintenance therapies for recurrent major depression: a randomized controlled trial in patients older than 59 years. JAMA. 1999;281:39–45. doi: 10.1001/jama.281.1.39. [DOI] [PubMed] [Google Scholar]
- Reynolds CF, 3rd, Miller MD, Pasternak RE, Frank E, Perel JM, Cornes C, et al. Treatment of bereavement-related major depressive episodes in later life: a controlled study of acute and continuation treatment with nortriptyline and interpersonal psychotherapy. American Journal of Psychiatry. 1999;156:202–208. doi: 10.1176/ajp.156.2.202. [DOI] [PubMed] [Google Scholar]
- Reynolds CF, Dew MA, Frank E, Begley AE, Miller MD, Cornes Cl, et al. Effects of age at onset of first lifetime episode of recurrent major depression on treatment response and illness course in elderly patients. American Journal of Psychiatry. 1998;155:795–799. doi: 10.1176/ajp.155.6.795. [DOI] [PubMed] [Google Scholar]
- Reynolds CF, Frank E, Perel J, et al. Maintenance therapies for late life recurrent major depression: Research and review circa 1995. International Psychogeriatrics. 1995;7(suppl):27–40. doi: 10.1017/s104161029500233x. [DOI] [PubMed] [Google Scholar]
- Rihmer Z. Strategies of suicide prevention: Focus on health care. Journal of Affective Disorders. 1996;39:83–91. doi: 10.1016/0165-0327(96)00007-9. [DOI] [PubMed] [Google Scholar]
- Rihmer Z, Rutz W, Pihlgren H. Depression and suicide on Gotland: An intensive study of all suicides before and after a depression-training program for general practitioners. Journal of Affective Disorders. 1995;35:147–152. doi: 10.1016/0165-0327(95)00055-0. [DOI] [PubMed] [Google Scholar]
- Roeloffs C, Sherbourne C, Unützer J, Fink A, Tang L, Wells KB. Stigma and depression among primary care patients. General Hospital Psychiatry. 2003;25(5):311–5. doi: 10.1016/s0163-8343(03)00066-5. [DOI] [PubMed] [Google Scholar]
- Rosen J, Mulsant BH, Kollar M, Kastango KB, Mazumdar S, Fox D. Mental health training for nursing home staff using computer-based interactive video: a 6-month randomized trial. Journal of the American Medical Directors Association. 2002;3:291–296. doi: 10.1097/01.JAM.0000027201.90817.21. [DOI] [PubMed] [Google Scholar]
- Rost K, Nutting P, Smith J, Werner J, Duan N. Improving depression outcomes in community primary care practice: a randomized trial of the QuEST intervention. JGIM. 2001;16:143–149. doi: 10.1111/j.1525-1497.2001.00537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutz W, von Knorring L, Wålinder J. Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta Psychiatrica Scandinavica. 1989;80:151–154. doi: 10.1111/j.1600-0447.1989.tb01318.x. [DOI] [PubMed] [Google Scholar]
- Sable JA, Dunn LB, Zisook S. Late-life depression: how to identify its symptoms and provide effective treatment. Geriatrics. 2002;57:18–35. [PubMed] [Google Scholar]
- Salzman C. Medication adherence in the elderly. Journal of Clinical Psychiatry. 1995;56:18–22. [PubMed] [Google Scholar]
- Salzman C, Wong E, Wright BC. Drug and ECT treatment of depression in the elderly, 1996–2001: a literature review. Biological Psychiatry. 2002;52:265–284. doi: 10.1016/s0006-3223(02)01337-9. [DOI] [PubMed] [Google Scholar]
- Sambamoorthi U, Olfson M, Walkup JT, Crystal S. Diffusion of new generation antidepressant treatment among elderly diagnosed with depression. Medical Care. 2003;41(1):180–94. doi: 10.1097/00005650-200301000-00019. [DOI] [PubMed] [Google Scholar]
- Sanderson K, Andrews G, Corry J, Lapsley H. Reducing the burden of affective disorders: is evidence-based health care affordable? Journal of Affective Disorders. 2003;77(2):109–25. doi: 10.1016/s0165-0327(03)00134-4. [DOI] [PubMed] [Google Scholar]
- Schoenbaum M, Miranda J, Sherbourne C, Duan N, Wells K. Cost-effectiveness of interventions for depressed Latinos. Journal of Mental Health Policy & Economics. 2004;7:69–76. [PubMed] [Google Scholar]
- Schoenbaum M, Unützer J, Sherbourne C, Duan N, Rubenstein LV, Miranda J, et al. Cost-effectiveness of practice-initiated quality improvement for depression: results of a randomized controlled trial. JAMA. 2001;286(11):1325–30. doi: 10.1001/jama.286.11.1325. [DOI] [PubMed] [Google Scholar]
- Schulberg HC, Bruce ML, Lee PW, Williams JW, Jr, Dietrich AJ. Preventing suicide in primary care patients: the primary care physician's role. General Hospital Psychiatry. 2004;26(5):337–45. doi: 10.1016/j.genhosppsych.2004.06.007. [DOI] [PubMed] [Google Scholar]
- Schulz R, Drayer RA, Rollman BL. Depression as a risk factor for non-suicide mortality in the elderly. Biological Psychiatry. 2002;52:205–225. doi: 10.1016/s0006-3223(02)01423-3. [DOI] [PubMed] [Google Scholar]
- Sclar DA, Robison LM, Skaer TL, Galin RS. Ethnicity and the prescribing of antidepressant pharmacotherapy: 1992–1995. Harvard Review of Psychiatry. 1999;7(1):29–36. doi: 10.1093/hrp/7.1.29. [DOI] [PubMed] [Google Scholar]
- Scocco P, Frank E. Interpersonal psychotherapy as augmentation treatment in depressed elderly responding poorly to antidepressant drugs: a case series. Psychotherapy & Psychosomatics. 2002;71(6):357–61. doi: 10.1159/000065991. [DOI] [PubMed] [Google Scholar]
- Scocco P, Frank E. Interpersonal psychotherapy as augmentation treatment in depressed elderly responding poorly to antidepressant drugs: a case series. Psychotherapy & Psychosomatics. 2002;71:357–361. doi: 10.1159/000065991. [DOI] [PubMed] [Google Scholar]
- Serby M, Yu M. Overview: depression in the elderly. Mount Sinai Journal of Medicine. 2003;70:38–44. [PubMed] [Google Scholar]
- Sewitch MJ, McCusker J, Dendukuri N, Yaffe MJ. Depression in frail elders: impact on family caregivers. International Journal of Geriatric Psychiatry. 2004;19:655–65. doi: 10.1002/gps.1135. [DOI] [PubMed] [Google Scholar]
- Sheeran T, Brown EL, Nassisi P, Bruce ML. Does depression predict falls among home health patients? Using a clinical-research partnership to improve the quality of geriatric care. Home Healthcare Nurse. 2004;22:384–389. doi: 10.1097/00004045-200406000-00007. [DOI] [PubMed] [Google Scholar]
- Sheikh JI, Cassidy EL, Doraiswamy PM, Salomon RM, Hornig M, Holland PJ, et al. Efficacy, safety, and tolerability of sertraline in patients with late-life depression and comorbid medical illness. Journal of American Geriatrics Society. 2004;52:86–92. doi: 10.1111/j.1532-5415.2004.52015.x. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Wells KB, Duan N, Miranda J, Unützer J, Jaycox L, et al. Long-term effectiveness of disseminating quality improvement for depression in primary care. Archives of General Psychiatry. 2001;58(7):696–703. doi: 10.1001/archpsyc.58.7.696. [DOI] [PubMed] [Google Scholar]
- Simon GE, Katon WJ, VonKorff M, Unützer J, Lin EHB, Walker EA, et al. Cost-effectiveness of a collaborative care program for primary care patients with persistent depression. American Journal of Psychiatry. 2001;158:1638–1644. doi: 10.1176/appi.ajp.158.10.1638. [DOI] [PubMed] [Google Scholar]
- Simon GE, Ludman EJ, Tutty S, Operskalski B, Von Korff M. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA. 2004;292:935–42. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- Simon GE, Von Korff M, Ludman EJ, Katon WJ, Rutter C, Unützer J, et al. Cost-effectiveness of a program to prevent depression relapse in primary care. Medical Care. 2002;40(10):941–50. doi: 10.1097/00005650-200210000-00011. [DOI] [PubMed] [Google Scholar]
- Sirey JA, Bruce ML, Alexopoulos GS, Perlick DA, Friedman SJ, Meyers BS. Stigma as a barrier to recovery: Perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatric Services. 2001;52(12):1615–20. doi: 10.1176/appi.ps.52.12.1615. [DOI] [PubMed] [Google Scholar]
- Sirey JA, Bruce ML, Alexopoulos GS, Perlick DA, Raue P, Friedman SJ, Meyers BS. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. American Journal of Psychiatry. 2001;158(3):479–81. doi: 10.1176/appi.ajp.158.3.479. [DOI] [PubMed] [Google Scholar]
- Skaer TL, Sclar DA, Robison LM, Galin RS. Trends in the rate of depressive illness and use of antidepressant pharmacotherapy by ethnicity/race: an assessment of office-based visits in the United States, 1992–1997. Clinical Therapeutics. 2000;22(12):1575–89. doi: 10.1016/s0149-2918(00)83055-6. [DOI] [PubMed] [Google Scholar]
- Smith L, Walker A, Gilhooly K. Clinical guidelines of depression: a qualitative study of GPs' views. Journal of Family Practice. 2004;53(7):556–61. [PubMed] [Google Scholar]
- Sommer BR, Fenn H, Pompei P, DeBattista C, Lembke A, Wang P, Flores B. Safety of antidepressants in the elderly. Expert Opinion on Drug Safety. 2(4):367–83. doi: 10.1517/14740338.2.4.367. [DOI] [PubMed] [Google Scholar]
- Sonnenberg CM, Beekman AT, Deeg DJ, Tilburg V. Drug treatment in depressed elderly in the Dutch community. International Journal of Geriatric Psychiatry. 2003;18(2):99–104. doi: 10.1002/gps.771. [DOI] [PubMed] [Google Scholar]
- Soumerai SB. Principles and uses of academic detailing to improve the management of psychiatric disorders. International Journal of Psychiatry in Medicine. 1998;28:81–86. doi: 10.2190/BTCA-Q06P-MGCQ-R0L5. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Steffens DC, Skoog I, Norton MC, Hart AD, Tschanz JT, Plassman, et al. Prevalence of depression and its treatment in an elderly population: the Cache County study. Archives of General Psychiatry. 2000;57:601–607. doi: 10.1001/archpsyc.57.6.601. [DOI] [PubMed] [Google Scholar]
- Stein MB, Barrett-Connor E. Quality of life in older adults receiving medications for anxiety, depression, or insomnia: findings from a community-based study. American Journal of Geriatric Psychiatry. 2002;10(5):568–74. [PubMed] [Google Scholar]
- Streim JE, Oslin DW, Katz IR, Smith BD, DiFilippo S, Cooper TB, Ten Have T. Drug treatment of depression in frail elderly nursing home residents. American Journal of Geriatric Psychiatry. 2000;8(2):150–9. [PubMed] [Google Scholar]
- Suominen K, Henriksson M, Isometsa E, Conwell Y, Heila H, Lonnqvist J. Nursing home suicides-a psychological autopsy study. International Journal of Geriatric Psychiatry. 2003;18:1095–101. doi: 10.1002/gps.1019. [DOI] [PubMed] [Google Scholar]
- Suominen K, Isometsa E, Lonnqvist J. Elderly suicide attempters with depression are often diagnosed only after the attempt. International Journal of Geriatric Psychiatry. 2004;19:35–40. doi: 10.1002/gps.1031. [DOI] [PubMed] [Google Scholar]
- Symons L, Tylee A, Mann A, Jones R, Plummer S, Walker M, et al. Improving access to depression care: descriptive report of a multidisciplinary primary care pilot service. British Journal of General Practice. 2004;54(506):679–83. [PMC free article] [PubMed] [Google Scholar]
- Szanto K, Mulsant BH, Houck P, Dew MA, Reynolds CF., 3rd Occurrence and course of suicidality during short-term treatment of late-life depression. Archives of General Psychiatry. 2003;60:610–617. doi: 10.1001/archpsyc.60.6.610. [DOI] [PubMed] [Google Scholar]
- Taylor MP, Reynolds CF, 3rd, Frank E, Cornes C, Miller MD, Stack JA. Which elderly patients remain well on maintenance interpersonal psychotherapy alone?: Report from Pittsburgh study of maintenance therapies in late life depression. Depression & Anxiety. 1999;10:55–60. [PubMed] [Google Scholar]
- Taylor WD, Doraiswamy PM. A systematic review of antidepressant placebo-controlled trials for geriatric depression: limitations of current data and directions for the future. Neuropsychopharmacology. 2004;29:2285–99. doi: 10.1038/sj.npp.1300550. [DOI] [PubMed] [Google Scholar]
- Thomas L, Mulsant BH, Solano FX, Black AM, Bensasi S, Flynn T, et al. Response speed and rate of remission in primary and specialty care of elderly patients with depression. American Journal of Geriatric Psychiatry. 2002;10:583–9. [PubMed] [Google Scholar]
- Thomas P, Hazif-Thomas C, Clement JP. Influence of antidepressant therapies on weight and appetite in the elderly. Journal of Nutrition, Health & Aging. 2003;7(3):166–70. [PubMed] [Google Scholar]
- Thompson LW, Coon DW, Gallagher-Thompson D, Sommer BR, Koin D. Comparison of desipramine and cognitive/behavioral therapy in the treatment of elderly outpatients with mild-to-moderate depression. American Journal of Geriatric Psychiatry. 2001;9(3):225–40. [PubMed] [Google Scholar]
- Torrisi D, McDaniel H. Better outcomes for depressed patients. The Nurse Practitioner. 2003;28:32–38. doi: 10.1097/00006205-200308000-00009. [DOI] [PubMed] [Google Scholar]
- Uncapher H, Areán PA. Physicians are less willing to treat suicidal ideation in older patients. Journal of the American Geriatrics Society. 2000;48(2):188–92. doi: 10.1111/j.1532-5415.2000.tb03910.x. [DOI] [PubMed] [Google Scholar]
- Unützer J. Diagnosis and treatment of older adults with depression in primary care. Biological Psychiatry. 2002;52:285–292. doi: 10.1016/s0006-3223(02)01338-0. [DOI] [PubMed] [Google Scholar]
- Unützer J, Ferrell B, Lin EH, Marmon T. Pharmacotherapy of pain in depressed older adults. Journal of American Geriatrics Society. 2004;52:1916–22. doi: 10.1111/j.1532-5415.2004.52519.x. [DOI] [PubMed] [Google Scholar]
- Unützer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting: A randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- Unützer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, et al. Depression treatment in a sample of 1,801 depressed older adults in primary care. Journal of the American Geriatrics Society. 2003;51(4):505–14. doi: 10.1046/j.1532-5415.2003.51159.x. [DOI] [PubMed] [Google Scholar]
- Unützer J, Katon W, Sullivan M, Miranda J. Treating depressed older adults in primary care: narrowing the gap between efficacy and effectiveness. The Millbank quarterly. 1999;77:225–256. doi: 10.1111/1468-0009.00132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unützer J, Patrick DL, Simon G, Grembowski D, Walker E, Rutter C, Katon W. Depressive symptoms and the cost of health services in HMO patients age 65 years and older: A 4-year prospective study. JAMA. 1997;277:1618–1623. doi: 10.1001/jama.1997.03540440052032. [DOI] [PubMed] [Google Scholar]
- Unützer J, Patrick DL, Marmon T, Simon GE, Katon WJ. Depressive symptoms nd mortality in a prospective study of 2,558 older adults. American Journal of Geriatric Psychiatry. 2002;10:521–530. doi: 10.1097/00019442-200209000-00005. [DOI] [PubMed] [Google Scholar]
- Van Eijk J, Diederiks J, Kempen G, Honig A, van der Meer K, Brenninkmeijer W. Development and feasibility of a nurse administered strategy on depression in community-dwelling patients with a chronic physical disease. Patient Education and Counseling. 2004;34:87–94. doi: 10.1016/S0738-3991(03)00201-5. [DOI] [PubMed] [Google Scholar]
- van Eijken M, Wensing M, de Konink M, Vernooy M, Zielhuis G, Lagro T, et al. Health education on self-management and seeking health care in older adults: a randomized trial. Patient Education & Counseling. 2004;55(1):48–54. doi: 10.1016/j.pec.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Virnig B, Huang Z, Lurie N, Musgrave D, McBean AM, Dowd B. Does Medicare managed care provide equal treatment for mental illness across races? Archives of General Psychiatry. 2004;61:201–205. doi: 10.1001/archpsyc.61.2.201. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Quarterly. 1996;7:511–44. [PubMed] [Google Scholar]
- Wells KB, Sherbourne C, Schoenbaum M, Duan N, Meredith L, Unützer J, et al. Impact of disseminating quality improvement programs for depression in managed primary care: A randomized controlled trial. JAMA. 2000;283:212–220. doi: 10.1001/jama.283.2.212. [DOI] [PubMed] [Google Scholar]
- Wells K, Sherbourne C, Schoenbaum M, Ettner S, Duan N, Miranda J, et al. Five-year impact of quality improvement for depression: results of a group-level randomized controlled trial. Archives of General Psychiatry. 2004;61:378–86. doi: 10.1001/archpsyc.61.4.378. [DOI] [PubMed] [Google Scholar]
- West CG, Reed DM, Gildengorin GL. Can money buy happiness? Depressive symptoms in an affluent older population. Journal of American Geriatrics Society. 1998;46:49–57. doi: 10.1111/j.1532-5415.1998.tb01012.x. [DOI] [PubMed] [Google Scholar]
- Wetherell JL, Unützer J. Adherence to treatment for geriatric depression and anxiety. CNS Spectrums. 2003;8(12 Suppl 3):48–59. doi: 10.1017/s1092852900008270. [DOI] [PubMed] [Google Scholar]
- Whyte EM, Dew MA, Gildengers A, Lenze EJ, Bharucha A, Mulsant BH, Reynolds CF. Time course of response to antidepressants in late-life major depression: therapeutic implications. Drugs Aging. 2004;21:531–554. doi: 10.2165/00002512-200421080-00004. [DOI] [PubMed] [Google Scholar]
- Williams JW, Jr, Katon W, Lin EH, Noel PH, Worchel J, Cornell J, et al. The effectiveness of depression care management on diabetes-related outcomes in older patients. Annals of Internal Medicine. 2004;140:1015–24. doi: 10.7326/0003-4819-140-12-200406150-00012. [DOI] [PubMed] [Google Scholar]
- Williams JW, Jr, Noel PH, Cordes JA, Ramirez G, Pignone M. Is this patient clinically depressed? JAMA. 2002;287:1160–1170. doi: 10.1001/jama.287.9.1160. [DOI] [PubMed] [Google Scholar]
- Williams JW, Barrett J, Oxman T, Frank E, Katon W, Sullivan M, et al. Treatment of dysthymia and minor depression in primary care: a randomized controlled trial in older adults. JAMA. 2000;284:1519–1526. doi: 10.1001/jama.284.12.1519. [DOI] [PubMed] [Google Scholar]
- Williams JW, Rost K, Dietrich AJ, Ciotti MC, Zyzanski SJ, Cornell J. Primary care physicians’ approach to depressive disorders: effects of physician specialty and practice structure. Archives of Family Medicine. 1999;8:58–67. doi: 10.1001/archfami.8.1.58. [DOI] [PubMed] [Google Scholar]
- Williams ML, Payne SA. A qualitative study of clinical nurse specialists’ views on depression in palliative care patients. Palliative Medicine. 2003;17:334–338. doi: 10.1191/0269216303pm747oa. [DOI] [PubMed] [Google Scholar]


