Abstract
The transplantation of neural stem cells (NSCs) offers a new potential therapeutic approach as a cell-based delivery system for gene therapy in brain tumors. This is based on the unique capacity of NSCs to migrate throughout the brain and to target invading tumor cells. However, the signals controlling the targeted migration of transplanted NSCs are poorly defined. We analyzed the in vitro and in vivo effects of angiogenic growth factors and protein extracts from surgical specimens of brain tumor patients on NSC migration. Here, we demonstrate that vascular endothelial growth factor (VEGF) is able to induce a long-range attraction of transplanted human NSCs from distant sites in the adult brain. Our results indicate that tumor-upregulated VEGF and angiogenic-activated microvasculature are relevant guidance signals for NSC tropism toward brain tumors.
Keywords: brain tumor, neural stem cells, migration, cell therapy, angiogenesis
Introduction
More than 17,000 patients are diagnosed yearly with malignant primary brain tumors and more than 170,000 are diagnosed with tumor metastasis to the brain [1]. Despite extensive technical improvements of conventional therapeutic regimens such as surgery, radiation, and chemotherapy, malignant brain tumors remain largely incurable. The highly invasive nature of gliomas or the disseminated presence of brain metastasis limits complete surgical removal, and is one of the major reasons for their dismal prognosis. Direct targeting and eradication of disseminated tumor cells, before they give rise to a recurrent tumor, may be a valuable therapeutic strategy. Neural stem cells (NSCs) have been demonstrated to be effective for directly delivering therapeutic molecules to areas of glioma cell invasion and to increase survival time in experimental glioma models [2–5]. This is based on the enormous capacity of NSCs to migrate throughout the brain and to target single or multifocal areas of pathologic changes while stably expressing a therapeutic transgene. Whether transplanted directly in the parenchyma of the central nervous system (CNS), even at distant sites of a brain tumor or injected intrathecally or intravenously, enrichment of NSCs within the tumor and “tracking” of single glioma cells migrating away from the main tumor mass have been reported [2,6]. Little is known about the mechanisms underlying the brain tumor tropism of NSCs. However, it is essential for future clinical realization of NSC-based therapeutic strategies to find out the relevant signals responsible for directing the migration and fate of transplanted NSCs.
During the embryonic development of the CNS, NSC migration is known to be guided over long distances by gradients of chemotactic and repulsive molecules [7]. It seems reasonable to speculate that soluble factors overexpressed by tumor cells or by cells of the surrounding reactive parenchyma may, in part, be responsible for the brain tumor tropism of NSCs. Active angiogenesis is a major hallmark of malignant brain tumors [8] and is a frequent feature of other neurologic disorders in which NSC tropism has been observed [9,10]. In the present study, we explored the hypothesis that angiogenic growth factors expressed during the malignant progression of different types of brain tumors are able to induce and guide the targeted migration of NSCs.
Materials and Methods
Cell Culture
The clonal human NSC line HB1.F3 [11,12] was maintained as adherent cultures in DMEM supplemented with 10% fetal bovine serum (FBS), 2 mM l-glutamine, 100 U/ml penicillin, and 100 µg/ml streptomycin (Invitrogen, Grand Island, NY). The same culture medium was used for the clonal murine NSC line C17.2 with the addition of 5% horse serum. Porcine aortic endothelial (PAE/KDR) cells stably transfected with KDR (a gift from Dr. Lena Claesson-Welsh; Ludwig Institute, Uppsala, Sweden) and the human glioblastoma cell lines U87 and U251 were cultured using the recommended standard conditions. To obtain conditioned media, the cell lines U87 and U251 were grown on 35-mm plates to 80% confluency. Cultures were rinsed three times with serum-free medium and incubated for another 48 hours in serum-free DMEM supplemented with 2 mM nonessential amino acids (Invitrogen), 2 mM l-glutamine, 100 U/ml penicillin, and 100 µg/ml streptomycin. Conditioned media were collected, cleared by centrifugation for 10 minutes at 600g, and stored at -80°C. Human umbilical vein endothelial cells (HUVECs; Clonetics, Wakersville, MD) were grown on 1% gelatin-coated plasticware in M199 medium (Invitrogen) supplemented with 20% FBS, 90 µg/ml endothelial cell growth supplement (Upstate Biotechnology, Lake Placid, NY), 40 U/ml heparin (Sigma, St. Louis, MO), 100 U/ml penicillin, and 100 µg/ml streptomycin.
Protein Extracts and ELISAs
Protein extracts were prepared from tumor specimens from brain tumor patients treated at the Department of Neurosurgery (Brigham and Women's Hospital and Children's Hospital, Boston, MA) [13]. Protein concentrations were determined using the bicinchoninic acid protein assay (Pierce, Rockford, IL). All brain tumors were histologically classified by the Department of Neuropathology (Brigham and Women's Hospital) according to the current WHO grading system. Growth factor contents of the protein extracts were determined by using commercially available ELISA kits (R&D Systems, Minneapolis, MN) for VEGF (DVE00), PlGF (DPG00), and SF/HGF (DHG00).
Reverse Transcription Polymerase Chain Reaction (RT-PCR)
Total RNA from HB1.F3 and KDR/PAE cells was prepared using Qiagen RNeasy protocol (Qiagen, Valencia, CA) and treated with DNase prior to further manipulation. Single-stranded cDNA was prepared from 1 µg of total RNA using oligo-p(dT)15 primers following the 1st Strand cDNA Synthesis Kit for RT-PCR protocol (Roche, Indianapolis, IN).
c-met and actin PCR cDNA from the reverse transcription reaction was subject to PCR in the presence of 0.25 µM of each 5′ and 3′ primers, 1.25 U of Taq polymerase (Roche), 2 mM MgCl2, 0.2 mM deoxynucleotide mix, and 1x PCR buffer. PCR was performed in a DNA thermal cycler (MJ Research, Watertown, MA) for 32 cycles, each consisting of 95°C for 1 minute and 55°C for 1 minute, with a 72°C extension for 1 minute. After 32 cycles, there was a final extension at 72°C for 10 minutes. PCR products were visualized by ethidium bromide staining following 1.0% agarose gel electrophoresis. The sense and antisense primers, respectively, and the predicted sizes of the RT-PCR reaction products were as follows:
c-met A: 5′-ACAGTGGCATGTCAACATCGCT-3′
c-met B: 5′-GCTCGGTAGTCTACAGATTC-3′ (655 bp)
β-actin A: 5′-GGCCATCTCTTGCTCGAAGT-3′
β-actin B: 5′-GCCCAGAGCAAGAGAGGCAT-3′(513 bp).
VEGFR-2 PCR cDNA were amplified using VEGFR-2-specific primers A and B for 30 cycles (95°C for 1 minute, 55°C for 1 minute, 72°C for 1 minute, with a final extension at 72°C for 10 minutes). A second round of PCR was carried out using nested VEGFR-2-specific primers C and D for 30 cycles (95°C for 1 minute, 60°C for 1 minute, 72°C for 1 minute, with a final extension at 72°C for 10 minutes). Primers and the predicted sizes of the RT-PCR reaction products were as follows:
VEGFR-2 A: 5′-ACGCTGACATGTACGGTCTAT-3′
VEGFR-2 B: 5′-TTCCCATTTGCTGGCATCATA-3′ (1163 bp)
VEGFR-2 C: 5′-CATCACATCCACTGGTATTGG-3′
VEGFR-2 D: 5′-GCCAAGCTTGTACCATGTGAG-3′ (404 bp).
VEGFR-1 PCR cDNA were amplified using VEGFR-1-specific primers A and B for 30 cycles (95°C for 1 minute, 55°C for 1 minute, 72°C for 1 minute with a final extension at 72°C for 10 minutes). A second round of PCR was carried out using nested VEGFR-1-specific primers C and D for five cycles at (95°C for 1 minute, 48°C for 1 minute, 72°C for 1 minute), five cycles at (95°C for 1 minute, 47°C for 1 minute, 72°C for 1 minute), five cycles at (95°C for 1 minute, 46°C for 1 minute, 72°C for 1 minute), five cycles at (95°C for 1 minute, 45°C for 1 minute, 72°C for 1 minute), five cycles at (95°C for 1 minute, 44°C for 1 minute, 72°C for 1 minute), and 20 cycles at (95°C for 1 minute, 62°C for 1 minute, 72°C for 1 minute, with a final extension at 72°C for 10 minutes). Primers and the predicted sizes of the RT-PCR reaction products were as follows:
VEGFR-1 A: 5′-GCAGGTGTGACTTTTGTTC-3′
VEGFR-1 B: 5′-AGGATTTCTTCCCCTGTGTA-3′ (511 bp)
VEGFR-1 C: 5′-GAGAGCATCACTCAG-3′
VEGFR-1 D: 5′-CCCGCAGTAAAATCCA-3′ (272 bp).
In Vitro Migration of NSC
NSC migration–in response to recombinant human growth factors VEGF165, PlGF, and SF/HGF (R&D Systems), protein extracts, and glioblastoma cell line-conditioned media was assessed using a modified Boyden chamber assay as previously described [6,13]. Values from at least two independent experiments were expressed as the mean ± standard error (SE) in percentage of the control migration (=100%). The control migration was assessed in response to serum-free DMEM containing 0.1% bovine serum albumin only and reflects the basal migration rate of NSCs in this assay. Tissue extracts, each at a fixed concentration of 400 µg/ml protein, were tested alone and in the presence of neutralizing monoclonal antibodies against VEGF (MAB293; R&D Systems) and SF/HGF (MAB294; R&D Systems) at 20 µg/ml.
Tumor Tropism of NSCs
Tropism of the human NSC HB1.F3 toward orthotopic human glioblastoma xenografts was demonstrated by implantation of tumor cells (U251 or U87) into the brains of 6-week-old nude mice. Animals were anesthetized (100 mg/kg ketamine and 5 mg/kg xylazine) and received stereotactically guided injections of 1x105 tumor cells in 2 µl of PBS through a 30-gauge Hamilton syringe into the right forebrain (∼2 mm lateral and 1 mm anterior to bregma, at a 3-mm depth from the skull surface). Ten days after tumor cell injection, Dil-labeled human NSCs HB1.F3 (5x104 in 2 µl of PBS) were stereotactically injected in the opposite hemisphere using the same coordinates. NSC labeling using the lipophilic tracer Dil (D-282; Molecular Probes, Eugene, OR) was performed immediately prior injection for 30 minutes according to the manufacturer's protocol. After an additional 8 days, animals were perfused with 4% paraformaldehyde, and the brains were removed and cryosectioned coronally at 10-µm intervals. All animal works were carried out in the animal facility at Brigham and Women's Hospital in accordance with federal, local, and institutional guidelines.
In Vivo Migration of NSCs
The in vivo migration of transplanted human NSC HB1.F3 in response to constant intraparenchymal infusions of recombinant human VEGF165 (0.25 ng/h), SF/HGF (0.25 ng/h), or PBS alone was assessed by left frontal implantation of a brain infusion cannula (∼2 mm lateral and 1 mm anterior to bregma, at a 3-mm depth from the skull surface) connected to an osmotic minipump designed to deliver 0.25 µl/hr (Model 2004; Alzet, Cupertino, CA) [14]. To establish a constant flow prior to implantation, the filled pumps were incubated overnight in sterile PBS at 37°C. The pump with sufficient catheter tubing was placed subcutaneously on the back of the anaesthetized mice; the anterior end of the catheter connected to the infusion cannula was tunneled subcutaneously to the site of the burr hole and fixed on the skull with surgical glue. The wounds were carefully sutured. Two days after the pump implantation, Dil-labeled HB1.F3 or HUVECs used as control (5 x 104 in 2 µl of PBS) were stereotactically transplanted in the right hemisphere using the described coordinates. The animals were perfused with 4% paraformaldehyde 5 or 9 days following cell transplantation, and the brains were removed and stored at -80°C until processed for histologic analysis. The correct pump infusion rates during the experiments were confirmed by checking the filling status of the pump reservoirs at the day of animal sacrifice.
Histologic Analysis
Frozen sections were counterstained with DAPI or hematoxylin and eosin for histologic evaluation. Blood vessel staining was carried out using standard immunofluorescence techniques with anti-CD31 (1:50; BD Biosciences Pharmingen1, San Jose, CA) as the primary antibody and FITC antirat IgG (1:50; Jackson ImmunoResearch, West Grove, PA) as the secondary antibody. Antibodies for assessing the cellular receptor expression included the primary antibodies anti-VEGFR-2 (1:100; Santa Cruz Biotechnology, Santa Cruz, CA) and anti-cMET (1:100; Santa Cruz Biotechnology) and the secondary antibody FITC anti-rabbit IgG (1:40; DAKO, Carpinteria, CA). Detection of human NSCs by the monoclonal antibody to the nuclear antigen NuMA (Ab-2) (Oncogene NA09L) was carried out using standard techniques with the Vectastain Elite ABC kit (Vector Laboratories, Burlingame, CA).
Statistical Analysis
Correlations between the growth factor content of the protein extracts and their ability to induce NSC migration were assessed by a nonlinear regression analysis. Because the values were not normally distributed we performed a regression on the ranks of the values which is a non parametric regression [15]. Only P < .05 were considered statistically significant.
Results and Discussion
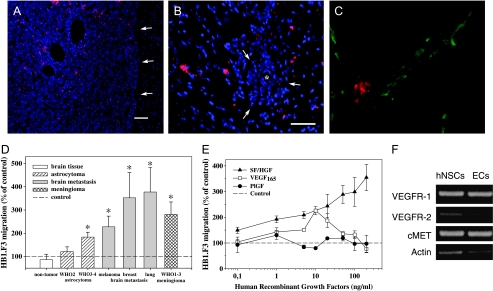
To investigate the signals that are involved in the brain tumor tropism of NSCs, we used the human NSC line HB1.F3 [11,12], which was derived from the ventricular zone of a 14-week-old human fetal brain and the well-characterized murine NSC line C17.2 [2,6,9]. Tumor tropism of the human NSC line HB1.F3 was demonstrated by establishing human U87 or U251 glioblastoma xenografts in the left forebrain of adult nude mice. Ten days later, 5x104 NSCs labeled with the lipophilic cell tracer Dil were stereotactically injected in the forebrain of the contralateral hemisphere. Within 1 week, the NSCs crossed the corpus callosum and enriched in the tumor mass (Figure 1A). Even small tumor satellites distant from the main tumor mass were targeted by NSCs (Figure 1B). In vitro, the conditioned media of U87 and U251 glioblastoma cells stimulated a directed NSC migration in the modified Boyden chamber assay up to two-fold (207 ± 18%, P < .01) and up to three-fold (316 ± 19%, P < .01) compared to the control, respectively. This suggests that soluble chemotactic factors produced by glioma cells may, in part, be responsible for inducing and guiding NSC migration. In vivo, we frequently observed a colocalization of glioma-targeting NSCs with the tumor vasculature (Figure 1C), suggesting that tumor blood vessels provide a vascular niche, possibly allowing survival of the NSCs within the metabolic-deprived tumor environment. Recent reports indicated that the recruitment and differentiation of neural precursors in the adult brain are linked to active angiogenesis [16–18]. Given that angiogenic activity is a frequent feature of many pathologic processes especially of malignant brain tumors, we hypothesized that tumor-expressed angiogenic factors may serve as chemoattractive signals for NSCs in the adult brain.
Figure 1.
Brain tumor tropism of the human neural stem cell line, HB1.F3. (A) Distribution of migrated NSCs (red) within the tumor mass of a U87 human glioblastoma xenograft (arrows = tumor border; blue = cell nuclei; bar = 150 µm). (B) Invaded tumor cells distant from the main tumor mass of a U251 human glioblastoma xenograft coopting a blood vessel were surrounded by human NSCs (* = blood vessel; bar = 100 µm). (C) Colocalization of an NSC (red) with a CD31-positive tumor blood vessel (green) within a U87 human glioblastoma. (D) Effects of protein extracts from different human brain tumor specimens normalized to 400 µg/ml protein on human NSC migration in the modified Boyden chamber assay. Values shown are mean ± SE and are expressed as percentage of the unstimulated basal migratory rate (control = 100%) (*P < .01, Mann-Whitney U test). (E) Recombinant human VEGF165, PlGF, and SF/HGF were tested in a modified 96-well Boyden chamber assay. SF/HGF induced a higher chemotactic response than VEGF. No significant effects were seen for PlGF. (F) Human NSCs expressed the receptor mRNA of VEGFR-2 and VEGFR-1 for VEGF and PlGF, and cMET for SF/HGF. Endothelial cells (PAE/KDR) known to express all three different receptors were used as a positive control.
To explore this hypothesis, we tested 56 human protein extracts prepared from surgical specimens of gliomas of different histologic grades, brain metastases, meningiomas, and nontumoral brain tissues for their effects on NSC migration. Extracts normalized for their total protein content from high-grade gliomas WHO III–IV, brain metastases, and meningiomas induced a significant higher HB1.F3 and C17.2 migration in vitro when compared to protein extracts from low-grade gliomas and nontumoral brain tissues derived from patients without any sign of tumor (Figure 1D and Table 1). Whereas the microvasculature of low-grade gliomas resembles that of normal brain, the more malignant variants of brain tumors are highly vascularized and known for the upregulation of positive regulators of angiogenesis including vascular endothelial growth factor (VEGF), placenta growth factor (PlGF), and scatter factor/hepatocyte growth factor (SF/HGF) [8,13,19]. Protein extracts were next determined for their content of VEGF, PlGF, and SF/HGF by ELISA (Table 1). Nonlinear regression analysis revealed a highly significant positive correlation between NSC migration-inducing effects of the protein extracts in vitro and their VEGF content (HB1.F3, P < .0001; C17.2, P < .003) but not for PlGF or SF/HGF. Adding specific neutralizing antibodies against VEGF and SF/HGF to the tumor protein extracts derived from three astrocytomas and three brain metastases inhibited NSC migration up to 80% and 65%, respectively (Figure W1). This demonstrates that the growth factors retained their biologic activity within the complex environment of brain tumors represented by the protein extracts. However, incomplete blocking of NSC migration may point to the presence of other factors influencing NSC migration. This is in agreement with a previous study demonstrating that SDF-1 present in the conditioned media of glioma cell lines induces in vitro migration of NSCs [20]. Recombinant VEGF and SF/HGF were able to stimulate NSC migration in vitro in a dose-dependent manner, thus supporting the functional relevance of VEGF and SF/HGF for NSC migration (Figure 1E). The migratory response to VEGF resembled a typical biphasic dose-response curve most likely due to the downregulation of the respective cellular receptor at higher VEGF concentrations. The cellular expression of VEGFR-2 and cMET was additionally confirmed by immunohistochemistry (data not shown). However, PlGF did not influence NSC migration despite mRNA expression of the corresponding receptor, VEGFR-1 (Figure 1F). Even in combination with VEGF, no effect of PlGF on NSC migration was observed (data not shown), although synergistic effects with VEGF on endothelial cells have been described [19].
Table 1.
Summary of Human Protein Extract-Induced Human Neural Stem Cell (HB1.F3) and Murine NSC (C17.2) Migration in the Modified Boyden Chamber Assay and Growth Factor Content of Protein Extracts as Assessed by ELISA Technique.
| Tissue Type (n) | HB1.F3 Migration | C17.2 Migration (n) | VEGF | PlGF (pg/mg protein) | SF/HGF |
| Brain tissue (no tumor) (7) | 86.3±23.6 | 97.2±24.3 (3) | 1.6±1.2 | 1.1±0.5 | 555.1±102.1 |
| Astrocytoma WHO II (11) | 121.3±20.3 | 144.6±7.2 (4) | 314.6±214.5 | 28.0±9.6 | 546.1±111.1 |
| Astrocytoma WHO III–IV (16) | 183.8±20.8 | 199.8±25.7 (5) | 663.5±193.3 | 30.6±8.0 | 1006.4±170.4 |
| Brain metastasis from | |||||
| Lung adenocarcinoma (8) | 377.6±105.3 | 374.4±142.4 (2) | 935.8±448.5 | 24.4±11.8 | 803.5±202.8 |
| Breast carcinoma (5) | 352.6±109.2 | 204.2 (1) | 283.4±210.9 | 58.7±42.2 | 862.3±224.4 |
| Melanoma (4) | 227.9±46.1 | ND | 306.6±173.9 | 75.1±9.6 | 885.0±284.0 |
| Meningioma WHO I–III (5) | 281.4±53.3 | 173.3±19.4 (3) | 11.5±5.3 | 92.4±35.4 | 281.7±55.0 |
We found a highly significant positive correlation between the NSC migration-inducing effects of the protein extracts in vitro and their VEGF content (HB1.F3, P<.0001; C17.2, P<.003) but not for PlGF or SF/HGF. There was no significant difference between human and murine NSC migration in response to the protein extracts. However, due to the limited amount of protein extracts available, not all extracts could be tested for their effects on C17.2. migration. All values are expressed as mean ± SE (n = number of specimen; ND = not determined).
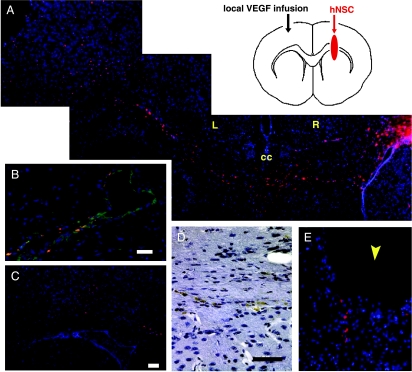
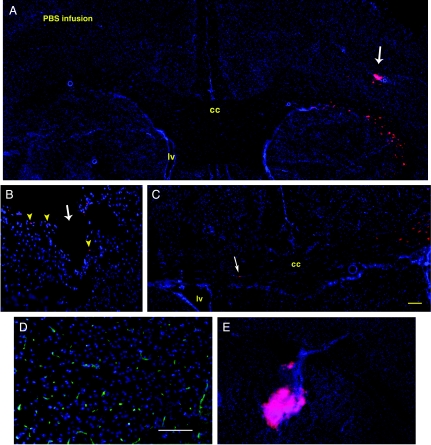
To investigate the relevance of our in vitro findings, studies in vivo were conducted in which a constant local source of growth factors (mimicking the conditions found in brain tumors) was established by local intracerebral infusions of VEGF, SF/HGF, or PBS. A total of 5x104 Dil-labeled NSCs were injected in the contralateral hemisphere and histologic analysis 5 and 9 days later demonstrated an extensive directed migration of the NSCs through the corpus callosum toward the VEGF-infused area where large dilated blood vessels were observed (Figure 2, A–D). This phenomenon is similar as seen in tumors where migrated NSCs were frequently associated with blood vessels (Figure 2B). SF/HGF at the low dosage of 0.25 ng/hr or PBS infusions did not induce a marked change in vascularization near the cannula site, and did not induce a distinct NSC migration (Figures 2E and 3, A–D). However, some NSCs were found locally at the injury site of the brain cannula, indicating that the reaction to the trauma induced by the cannula triggers minor NSC migration. In the absence of a trauma or brain tumor, we never observed any NSC migration toward the contralateral hemisphere (data not shown). Interestingly, the endothelial cells that are known to be highly responsive to VEGF did not display a transhemispheric migration toward the VEGF infused area, but rather stayed at the injection site (Figure 3E). The lack of endothelial cell migration in response to the VEGF infusion and the failure of SF/HGF to induce NSC migration in vivo despite its relevant effects in vitro suggest that VEGF may additionally trigger other signals [10,19] that are possibly relevant for allowing a directed NSC migration.
Figure 2.
Representative sections of VEGF-induced migration of human NSCs HB1.F3 in the brain of adult nude mice (see diagram). (A) Long-range attraction of NSCs (red) from the right hemisphere (R) across the corpus callosum (cc) in response to a local microinfusion of VEGF (0.25 ng/hr) in the left hemisphere (L) (day 9; blue = cell nuclei). (B) Colocalization of NSCs with dilated CD31-positive (green) blood vessels near the VEGF infusion cannula (bar = 50 µm). (C) Already after 5 days, transhemispheric migrated NSCs pool in the area of VEGF infusion (bar = 100 µm). (D) Migrating NSCs (brown) in the corpus callosum as demonstrated by immunohistochemistry using a human-specific antibody (bar = 25 µm). (E) Local microinfusion of SF/HGF (0.25 ng/hr) was not able to induce a long-range attraction. Only directly at the injury site of the cannula (arrowhead) were some NSCs observed.
Figure 3.
(A–C) Representative coronal brain sections of different nude mice receiving a constant intraparenchymal PBS infusion in the left hemisphere. (A) No extensive migration toward the PBS-infused left hemisphere was observed 9 days after injection of Dil-labeled human NSCs HB1.F3 (red) in the right forebrain (arrow). (B) However, some NSCs (arrowheads) were found at the lesion site of the brain cannula (arrow) and (C) occasionally single NSCs (arrow) migrating to the opposite infused hemisphere could be detected. This indicates that already the injury induced by the infusion cannula triggers mechanisms causing minor NSC migration (bar = 50 µm). (D) SF/HGF, although known to display angiogenic properties, did not cause a stimulation of angiogenesis near the cannula when infused at the dosage of 0.25 ng/hr (CD31 immunoreactivity = green) (bar = 100 µm). (E) In control experiments, Dil-labeled endothelial cells (red) stayed at the site of injection and did not migrate toward the VEGF infusion site.
In summary, this is the first report directly demonstrating that VEGF is a strong signal for guiding the in vivo migration of NSCs from distant sites in the adult brain. We found a highly significant correlation between the brain tumor-produced VEGF and the induction of NSC attraction in vitro. PlGF was not relevant for NSC migration and low doses of SF/HGF were not able to induce a long-range attraction of transplanted NSCs in vivo. We conclude that upregulated VEGF in brain tumors may serve as a signal for NSC tropism to pathologic sites. Taking into account the expression of factors involved in the survival and guidance of transplanted NSCs during a disease process may allow the optimization of therapeutic transplantation efficiency and the development of rational therapeutic strategies in the future.
Supplementary Material
Acknowledgements
We thank Elizabeth Allred for performing the statistical analysis and Theresa Cargoli and Renna Onario for technical assistance. We are grateful to Evan Snyder for providing the C17.2 cell line.
Abbreviations
- NSC
neural stem cell
- VEGF
vascular endothelial growth factor
- SF/HGF
scatter factor/hepatocyte growth factor
- PlGF
placenta growth factor
Footnotes
This work was supported by Layton BioSciences, Inc., the NIH/NCI, and by a grant from the German Research Foundation (DFG) to N.O.S.
This article refers to supplementary material, which is designated by W (ie, Table W1, Figure W1) and is available online at www.bcdecker.com.
References
- 1.Kleihues P, Cavenee WK. Pathology and Genetics of Tumors of the Central Nervous System International Agency for Research on Cancer Press, Lyon. 2000. [Google Scholar]
- 2.Aboody KS, Brown A, Rainov NG, Bower KA, Liu S, Yang W, Small JE, Herrlinger U, Ourednik V, Black PM, et al. From the cover: neural stem cells display extensive tropism for pathology in adult brain: evidence from intracranial gliomas. Proc Natl Acad Sci USA. 2000;97:12846–12851. doi: 10.1073/pnas.97.23.12846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benedetti S, Pirola B, Pollo B, Magrassi L, Bruzzone MG, Rigamonti D, Galli R, Selleri S, Di Meco F, De Fraja C, et al. Gene therapy of experimental brain tumors using neural progenitor cells. Nat Med. 2000;6:447–450. doi: 10.1038/74710. [DOI] [PubMed] [Google Scholar]
- 4.Ehtesham M, Kabos P, Kabosova A, Neuman T, Black KL, Yu JS. The use of interleukin 12-secreting neural stem cells for the treatment of intracranial glioma. Cancer Res. 2002;62:5657–5663. [PubMed] [Google Scholar]
- 5.Staflin K, Honeth G, Kalliomaki S, Kjellman C, Edvardsen K, Lindvall M. Neural progenitor cell lines inhibit rat tumor growth in vivo. Cancer Res. 2004;64:5347–5354. doi: 10.1158/0008-5472.CAN-03-1246. [DOI] [PubMed] [Google Scholar]
- 6.Brown AB, Yang W, Schmidt NO, Carroll R, Leishear KK, Rainov NG, Black PM, Breakefield XO, Aboody KS. Intravascular delivery of neural stem cell lines to target intracranial and extracranial tumors of neural and non-neural origin. Hum Gene Ther. 2003;14:1777–1785. doi: 10.1089/104303403322611782. [DOI] [PubMed] [Google Scholar]
- 7.Song H, Poo M. The cell biology of neuronal navigation. Nat Cell Biol. 2001;3:E81–E88. doi: 10.1038/35060164. [DOI] [PubMed] [Google Scholar]
- 8.Harrigan MR. Angiogenic factors in the central nervous system. Neurosurgery. 2003;53:639–660. doi: 10.1227/01.neu.0000079575.09923.59. (discussion, 660–631) [DOI] [PubMed] [Google Scholar]
- 9.Park KI, Ourednik J, Ourednik V, Taylor RM, Aboody KS, Auguste KI, Lachyankar MB, Redmond DE, Snyder EY. Global gene and cell replacement strategies via stem cells. Gene Ther. 2002;9:613–624. doi: 10.1038/sj.gt.3301721. [DOI] [PubMed] [Google Scholar]
- 10.Carmeliet P, Storkebaum E. Vascular and neuronal effects of VEGF in the nervous system: implications for neurological disorders. Semin Cell Dev Biol. 2002;13:39–53. doi: 10.1006/scdb.2001.0290. [DOI] [PubMed] [Google Scholar]
- 11.Jeong SW, Chu K, Jung KH, Kim SU, Kim M, Roh JK. Human neural stem cell transplantation promotes functional recovery in rats with experimental intracerebral hemorrhage. Stroke. 2003;34:2258–2263. doi: 10.1161/01.STR.0000083698.20199.1F. [DOI] [PubMed] [Google Scholar]
- 12.Cho T, Bae JH, Choi HB, Kim SS, McLarnon JG, Suh-Kim H, Kim SU, Min CK. Human neural stem cells: electrophysiological properties of voltage-gated ion channels. Neuroreport. 2002;13:1447–1452. doi: 10.1097/00001756-200208070-00020. [DOI] [PubMed] [Google Scholar]
- 13.Schmidt NO, Westphal M, Hagel C, Ergun S, Stavrou D, Rosen EM, Lamszus K. Levels of vascular endothelial growth factor, hepatocyte growth factor/scatter factor and basic fibroblast growth factor in human gliomas and their relation to angiogenesis. Int J Cancer. 1999;84:10–18. doi: 10.1002/(sici)1097-0215(19990219)84:1<10::aid-ijc3>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 14.Schmidt NO, Ziu M, Carrabba G, Giussani C, Bello L, Sun Y, Schmidt K, Albert M, Black PM, Carroll RS. Antiangiogenic therapy by local intracerebral microinfusion improves treatment efficiency and survival in an orthotopic human glioblastoma model. Clin Cancer Res. 2004;10:1255–1262. doi: 10.1158/1078-0432.ccr-03-0052. [DOI] [PubMed] [Google Scholar]
- 15.Iman RL, Conover WJ. Technometrics. 1979;21:499–509. [Google Scholar]
- 16.Louissaint A, Jr, Rao S, Leventhal C, Goldman SA. Coordinated interaction of neurogenesis and angiogenesis in the adult songbird brain. Neuron. 2002;34:945–960. doi: 10.1016/s0896-6273(02)00722-5. [DOI] [PubMed] [Google Scholar]
- 17.Monje ML, Mizumatsu S, Fike JR, Palmer TD. Irradiation induces neural precursor-cell dysfunction. Nat Med. 2002;8:955–962. doi: 10.1038/nm749. [DOI] [PubMed] [Google Scholar]
- 18.Zhang H, Vutskits L, Pepper MS, Kiss JZ. VEGF is a chemoattractant for FGF-2-stimulated neural progenitors. J Cell Biol. 2003;163:1375–1384. doi: 10.1083/jcb.200308040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferrara N, Gerber HP, LeCouter J. The biology of VEGF and its receptors. Nat Med. 2003;9:669–676. doi: 10.1038/nm0603-669. [DOI] [PubMed] [Google Scholar]
- 20.Ehtesham M, Yuan X, Kabos P, Chung NH, Liu G, Akasaki Y, Black KL, Yu JS. Glioma tropic neural stem cells consist of astrocytic precursors and their migratory capacity is mediated by CXCR4. Neoplasia. 2004;6:287–293. doi: 10.1593/neo.3427. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.