ABSTRACT
Trans-sphenoid anterobasal temporal lobe meningoceles are rare and can be associated with temporal lobe epilepsy or recurrent meningitis. Surgical treatment is described via complicated infratemporal or intracranial approaches with high morbidity. A 32-year-old man presented with an 18-year history of two types of seizures and confirmed epileptic activity in electroencephalogram. A trans-sphenoid meningocele in the left pterygopalatine fossa was found on computed tomography and magnetic resonance imaging. A midfacial degloving was chosen instead of a large neurosurgical approach to remove it and to repair the dura defect with lyophilized dura, collagen, and abdominal fat. The postoperative course was uneventful without visible scars and the patient remains free of seizures without antiepileptic medication 3 years after surgery. Although midfacial degloving is not described yet as a treatment of trans-sphenoid meningoceles, this approach proved to be fast, safe, effective, and reliable and should be considered as the only alternative to large external approaches.
Keywords: Midfacial degloving, trans-sphenoid meningocele, pterygopalatine fossa
Structural anomalies of the central nervous system such as congenital or post-traumatic meningocerebral cicatrix, mesial temporal sclerosis, hamartomas, and indolent neoplasms are frequently associated with epilepsy.1
Congenital meningoencephaloceles of the skull base are commonly classified according to the site of the bone defect2,3,4 and can also result in epileptic disease. Pollock classifies them as follows: (1) sphenopharyngeal or trans-sphenoidal, when they protrude into the epipharynx and/or sphenoid sinus; (2) spheno-orbital, when the protrusion is through the superior orbital fissure into the superior orbit producing unilateral exophthalmus; (3) sphenoethmoidal, when the cerebral mass extends through the sphenoid and ethmoidal bones into the posterior nasal cavity; (4) transethmoidal, when the encephalocele extends into the anterior nasal cavity; and (5) sphenomaxillary, when the meningoencephalocele passes through the superior orbital fissure into the orbit and through the inferior orbital fissure into the pterygopalatine fossa.2
The trans-sphenoidal meningo(encephalo)celes are congenital caused by incomplete embryogenesis of the Ala sphenoidalis major thus protruding in the pterygopalatine fossa.5 They are extremely rare among the meningo(encephalo)celes of the skull base. Their cardinal symptom is temporal lobe epilepsy. The extension of gliosis from the encephalocele in direct continuity to the amygdalohippocampal region, the most active epileptic area, is considered as the pathomechanism of epilepsy.5 Occasionally, this lesion can be discovered during evaluation for recurrent meningitis.6
Computed tomography (CT) usually demonstrates the bony gap and magnetic resonance imaging (MRI) reveals the extent of soft tissue prolapse and allows differentiation between cerebrospinal fluid (CSF) and tissue. Further, MRI detects cases that cannot be diagnosed by CT, which is obligatory in evaluating epilepsy.7
Surgical approach to the middle skull base and pterygopalatine fossa for any kind of benign and malignant processes is a challenge for both neurosurgeons and maxillofacial surgeons and results in sophisticated procedures, such as infratemporal approach, or after anterior subtemporal craniotomy or temporary sagittal mandibulotomy.8,9,10,11,12,13
We report a case of trans-sphenoid meningocele in an adult that resulted in a medically resistant temporal lobe epilepsy. Although not described in the literature, the midfacial degloving was chosen for its surgical management.
CASE REPORT
The subject was a 32-year-old male with a history of two types of seizures for the previous 18 years. The first type began at the age of 14 initially with paresthesias affecting the fingers and feet and dizzy spells lasting several minutes, followed by loss of consciousness and urinary incontinence. The second type, consisting of generalized tonicoclonic seizure (grand mal), first occurred at the age of 27 and continued in 6- to 8-month intervals until presentation.
The patient had an intense lifestyle with alcohol and cigarette abuse and was exposed to professional physical strain as well. He reported that seizures usually occurred during infections of the upper respiratory tract while blowing his nose, or after extreme body fatigue. Antiepileptic treatment for the last 2 years failed to prevent them. There was no history of head injury at birth or later.
The patient's physical examination was normal. Neurological evaluation including electroencephalogram confirmed a left temporal lobe dysfunction. Epileptic activity was recorded from the mesial and anterior neocortical surfaces.
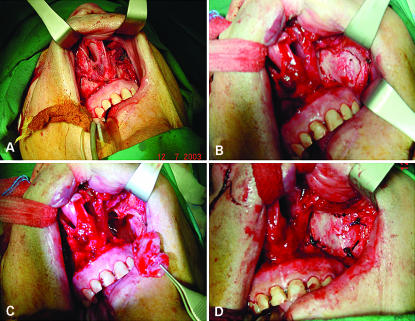
CT of the skull base demonstrated a defect at the left Ala sphenoidalis major and soft tissue protruding into the pterygopalatine fossa as typical trans-sphenoid meningocele (Fig. 1). This location allowed its approach via midfacial degloving.14 Under general anesthesia, the classical four incisions were performed: (l) bilateral sublabial incision in the oral vestibule; (2) complete transfixion between nasal septum and nasal columella; (3) bilateral circumvestibular incision of the piriform aperture extending to the oral vestibule; and (4) bilateral intercartilaginous incision between alar and lateral nasal cartilage (Fig. 2A).
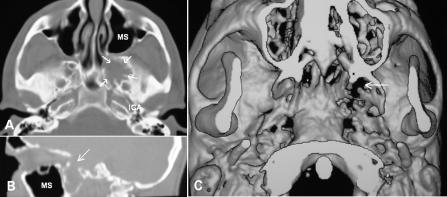
Figure 1.
(A) Preoperative axial CT demonstrating a soft tissue process (arrows) behind the left maxillary sinus (MS), in front of the foramen rotundum and not far from the internal carotid artery (ICA). (B) Sagittal reconstruction of CT at paramedical plane demonstrating the bony gap of the middle fossa skull base (arrow) and soft tissue prolapse (meningocele) in the pterygopalatine fossa behind the healthy maxillary sinus. (C) Three-dimensional reconstruction of the skull base demonstrating the bony gap of the middle fossa skull base at the level of the foramina rotundum et ovale, which are unified (arrow). CT, computed tomography.
Figure 2.
(A) Typical mucosal incisions for midfacial degloving. (B) Elevation of midfacial skin and periosteum and osteoplastic temporary removal of the ventral wall of left maxillary sinus. The infraorbital nerve is preserved. (C) Opening of the left maxillary sinus. (D) Reposition of the maxillary sinus wall and fixation with sutures.
The periosteum of the canine fossae was elevated, preserving the infraorbital nerves. The skin of the lower third of the nose was cranially dislocated toward the glabella by using a wet gauze (Fig. 2B). The ventral wall of the left maxillary sinus, together with the caudal part of the frontal process of the left maxilla, were osteoplastically removed to open the maxillary sinus (Fig. 2C). Its healthy mucosa was preserved and the mucosa of the dorsal sinus wall was elevated as a flap to expose the open posterior antral wall. This was temporarily removed in toto by osteotomy with a fine chisel to access the pterygopalatine fossa. Under the surgical microscope, the internal maxillary artery was dissected and closed by using vasosurgical clips. Further dissection was necessary to expose the thin dura of the meningocele out of the surrounding fat and follow it toward the bony defect. The whole cele was then amputated, resulting in a CSF leak. This was sealed by using lyophilized dura, collagen fleece with fibrin glue, and abdominal fat. Lumbar drain was not necessary. The posterior antral wall was then repositioned and supported by the mucosal flap and fibrin glue. The ventral antral wall was also repositioned and stabilized with slowly resorbable sutures (Fig. 2D) and all incisions were closed with proper material. Endonasal dressing was not implemented and neither supra- nor infraturbinal antrostomy was necessary, since the healthy antral mucosa was completely preserved (Fig. 3). Histological examination confirmed the diagnosis.
Figure 3.
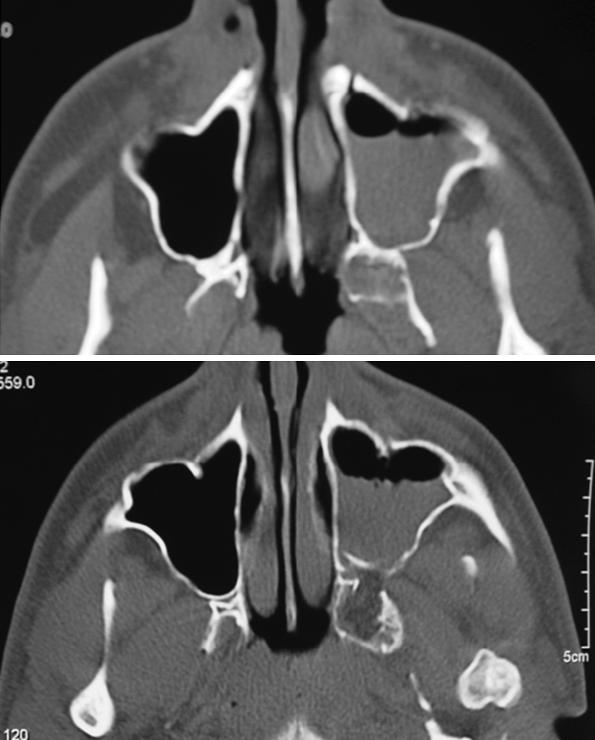
Axial CT 2 days after surgery showing the reposition of the anterior and posterior walls of the left maxillary sinus, the fat obliterating the hole of the removed meningocele, and the postoperative hematosinus. CT, computed tomography.
The postoperative course was uneventful under antibiotic cover with ceftriaxone (Rocephin®) and the patient was discharged 2 days later. He is free of seizures 3 years after surgery without antiepileptic treatment.
DISCUSSION
Trans-sphenoidal meningo(encephalo)celes at the region of the foramen rotundum and pterygoid process protruding in the pterygopalatine fossa are obviously very rare, since only five cases could be found in our literature research. Four of them caused epilepsy5,15 and one patient experienced recurrent meningitis.6 None of these, including our case, fit into the classification system of skull base meningoceles according to Pollock,2 since they did not protrude into the pterygopalatine fossa through the orbit as the described sphenomaxillary ones, but through paramedial dehiscence (see Fig. 1C), and they could be classified as lateral trans-sphenoidal meningo(encephalo)celes. All five cases and also ours were situated on the left side!
Since these meningo(encephalo)celes protrude in the pterygopalatine fossa, they are not apparent during clinical examination and sometimes even the CT scan fails to reveal them. For that reason, the presence of the meningocele was evident intraoperatively during temporal lobectomy for the treatment of temporal lobe epilepsy.5,15 Thus, this disease should be seriously considered in the differential diagnosis of late-onset temporal lobe epilepsy. MRI is recommended for definitive exclusion or confirmation.7
Because surgical access to the region is very demanding, various approaches have been described. Most of them refer to malignant processes, where functional and esthetic compromises can be tolerated to achieve radical tumor resection.8,9,10,11 However, extended facial scars as well as high risk of facial nerve or other cranial nerve palsies after temporary sagittal mandibulotomy are obsolete for treatment of benign processes like the trans-sphenoid meningocele. Anterior subtemporal craniotomy, which requires severe retraction of the brain to access the region (with high morbidity), seems to be over-treatment as well. Recent minimally invasive endoscopic techniques for benign processes of the nose and paranasal sinus are indicated only for minor surgery in the pterygopalatine fossa.12,13
We strongly advocate the transantral endoscopic midfacial degloving approach as a safe, effective, and reliable surgical approach for the treatment of pterygopalatine fossa meningoceles. It allows sufficient exposure for complete resection of the sac. It provides an unobstructed view and space for manipulation to control complications like bleeding of the internal maxillary artery and CSF leak. The only cranial nerve at risk is the second branch of the trigeminal nerve, which should be identified and routinely preserved. Further, all incisions are invisible so that external scars and cosmetic deformities can definitely be avoided. Thus, midfacial degloving should be considered as the only alternative for the treatment of trans-sphenoid meningo(encephalo)celes.
REFERENCES
- Mathienson G. In: Purpura DP, Penry JK, Walter RD eds, editor. Advances in Neurology Volume 8: Neurosurgical Management of the Epilepsies. New York, NY: Raven Press; 1975. Pathologic aspects of epilepsy with special reference to the surgical pathology of focal cerebral seizures. pp. 107–138. [PubMed]
- Pollock J A, Newton T H, Hoyt W F. Transsphenoidal and transethmoidal encephaloceles. A review of clinical and roentgen features in 8 cases. Radiology. 1968;90:442–453. doi: 10.1148/90.3.442. [DOI] [PubMed] [Google Scholar]
- Suwanwela C, Suwanwela N. A morphological classification of sincipital encephalomeningoceles. J Neurosurg. 1972;36:201–211. doi: 10.3171/jns.1972.36.2.0201. [DOI] [PubMed] [Google Scholar]
- David D J, Proudman T W. Cephaloceles: classification, pathology, and management. World J Surg. 1989;13:349–357. doi: 10.1007/BF01660747. [DOI] [PubMed] [Google Scholar]
- Leblanc R, Tampieri D, Robitaille Y, et al. Developmental anterobasal temporal encephalocele and temporal lobe epilepsy. J Neurosurg. 1991;74:933–939. doi: 10.3171/jns.1991.74.6.0933. [DOI] [PubMed] [Google Scholar]
- Chapman P H, Curtin H D, Cunningham M J. An unusual pterygopalatine meningocele associated with neurofibromatosis type 1. Case report. J Neurosurg. 2000;93:480–483. doi: 10.3171/jns.2000.93.3.0480. [DOI] [PubMed] [Google Scholar]
- Kuzniecky R, de la Sayette V, Ethier R, et al. Magnetic resonance imaging in temporal lobe epilepsy: pathological correlations. Ann Neurol. 1987;22:341–347. doi: 10.1002/ana.410220310. [DOI] [PubMed] [Google Scholar]
- Dingman D L, Conley J J. Lateral approach to the pterygomaxillary region. Ann Otol Rhinol Laryngol. 1970;79:967–969. doi: 10.1177/000348947007900515. [DOI] [PubMed] [Google Scholar]
- Attenborough N R. Maxillectomy via a temporal approach. J Laryngol Otol. 1980;94:149–162. doi: 10.1017/s0022215100088617. [DOI] [PubMed] [Google Scholar]
- Pogrel M A, Kaplan M J. Surgical approach to the pterygomaxillary region. J Oral Maxillofac Surg. 1986;44:183–187. doi: 10.1016/0278-2391(86)90105-9. [DOI] [PubMed] [Google Scholar]
- Steinhart H, Schroeder H G, Kleinsasser O. Temporäre sagittale Unterkieferspaltung zur Eröffnung eines Zuganges in die Fossa pterygopalatina, den Parapharyngealraum und den Oropharynx [Temporary sagittal mandibulotomy as an approach to the pterygopalatine fossa, the parapharyngeal space and the oropharynx] Laryngol Rhinol Otol (Stuttg) 1993;72:532–536. doi: 10.1055/s-2007-997951. [DOI] [PubMed] [Google Scholar]
- Pasquini E, Sciarretta V, Farneti G, Ippolito A, Mazzatenta D, Frank G. Endoscopic endonasal approach for the treatment of benign schwannoma of the sinonasal and pterygopalatine fossa. Am J Rhinol. 2002;16:113–118. [PubMed] [Google Scholar]
- DelGaudio J M. Endoscopic transnasal approach to the pterygopalatine fossa. Arch Otolaryngol Head Neck Surg. 2003;129:441–446. doi: 10.1001/archotol.129.4.441. [DOI] [PubMed] [Google Scholar]
- Berghaus A. Midfacial degloving. HNO. 1990;38:7–11. [PubMed] [Google Scholar]
- Ruiz Garcia F. Un caso de epilepsia del lobulo temporal producida por un encefalocele [A case of temporal lobe epilepsy caused by an encephalocele] Rev Esp Otoneurooftalmol. 1971;29:216–220. [PubMed] [Google Scholar]